Abstract
Background
Evacuatory dysfunction after distal colorectal resection varies from incontinence to obstructed defaecation and is termed anterior resection syndrome. The aim of this study was to identify risk factors for the development of anterior resection syndrome.
Methods
All anterior resections undertaken at Auckland Hospital from 2002 to 2012 were retrospectively evaluated. An assortment of patient and peri-operative variables were recorded. Cases were stratified by the occurrence of anterior resection syndrome symptoms from 1 to 5 years post-operatively.
Results
A total of 277 patients were identified. Prevalence of anterior resection syndrome decreased progressively from 61 % at 1 year to 43 % at 5 years. Univariate analysis identified anastomotic height, surgeon, pT stage, procedure year and temporary diversion ileostomy as recurring significant correlates (p < 0.05). Logistic regression identified lower anastomotic height (odds ratio (OR) 2.11, 95 % confidence interval (CI) 1.05–4.27; p = 0.04) and obstructive presenting symptoms (OR 6.71, 95 % CI 1.00–44.80; p = 0.05) as independent predictors at 1 and 2 years, respectively. Post-operative chemotherapy was a predictor at 1 year (OR 1.93, 95 % CI 1.04–3.57; p = 0.03). Temporary diverting ileostomy was an independent predictor at 2 (OR 2.49, 95 % CI 1.04–5.95; p = 0.04), 3 (OR 4.17, 95 % CI 1.04–16.78; p = 0.04), 4 (OR 8.05, 95 % CI 1.21–53.6; p = 0.03), and 5 years (OR 49.60, 95 % CI 2.17–1134.71; p = 0.02) after adjusting for anastomotic height.
Conclusions
Anastomotic height, post-operative chemotherapy and obstructive presenting symptoms were independent predictors at 1 and 2 years. Temporary diversion ileostomy was an independent predictor for the occurrence of anterior resection syndrome at 2, 3, 4 and 5 years even after correcting for anastomotic height. Prospective assessment is required to facilitate more accurate risk factor analysis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oncological outcomes following rectal cancer surgery have improved significantly over recent decades through superior surgical technique and the use of adjuvant therapy.1, 2 However, these survival advantages have greatly overshadowed functional outcomes of surgery, which are poor for many patients and consistently under-reported.3 The term ‘anterior resection syndrome’ (ARS) has been used to describe the diverse and interchangeable evacuatory symptoms that may occur following distal colorectal resection. Symptoms range from obstructed defaecation to urgency to incontinence and have been quoted as occurring in between 0 and 74 % of patients.3 This wide variation in purported incidence has led to a poor understanding of its natural history and may be attributed to the lack of a standardised definition for ARS or validated tool assessing its severity.
ARS has a major impact on quality of life (QoL), with many patients describing debilitating social limitations and developing psychiatric disorders.4–6 It has been postulated that its effect on QoL and body image are similar to patients with a stoma.7 Indeed, a recent Cochrane review found no significant difference in QoL between patients who had undergone low anterior resection with primary anastomosis and those with permanent colostomy following abdominoperineal resection.8
It is hoped that identification of clinical risk factors that predispose to the occurrence of ARS will facilitate insight into its pathogenesis and perhaps serve as a platform for the design and execution of future research. The aims of this retrospective cohort study were to characterise the natural history of ARS after distal colorectal resection over a 5-year follow-up period and to determine patient and peri-operative factors associated with its development.
Methods
Ethical approval was obtained from the National Ethics Committee and the appropriate institutional committee prior to data retrieval.
A prospectively maintained register of all anterior resections performed by the Colorectal Unit at Auckland City Hospital (ACH) was retrospectively accessed. Anterior resection was defined as any large-bowel resection involving the rectum with primary colorectal or coloanal anastomosis. Consecutive procedures between 1 January 2002 and 31 December 2012 (inclusive) were identified via the acquisition of unique patient National Health Index (NHI) numbers. Patient NHI numbers were used to extract information for an assortment of patient characteristics and peri-operative variables with data then entered into an electronic spreadsheet.
Patient characteristics recorded included age at surgery, gender, ethnicity, previous abdominal surgery, gastrointestinal comorbidities, presenting bowel symptoms, ASA grade and BMI. For patients with confirmed primary rectal cancer, the height of the tumour from the anorectal junction was assessed by digital rectal examination (DRE) and rigid sigmoidoscopy for low rectal tumours and colonoscopy for more proximal lesions. Presenting bowel symptoms were recorded as nil, per rectal (PR) bleeding alone, incontinence symptoms, obstructive symptoms, mixed symptoms or any of these symptom clusters combined with PR bleeding. Pre-operative variables recorded were the use of neo-adjuvant chemotherapy or radiotherapy, year of diagnosis, time from diagnosis to surgery and elective vs. acute presentation. Intra-operative variables recorded were surgeon, indication, procedure duration, year of procedure, open vs. laparoscopic vs. converted approach, formation of a neo-reservoir, stapled vs. hand-sewn anastomosis, height of the anastomosis and formation of a stoma. Stoma formation was further qualified relative to the index procedure as being created before (ileostomy or colostomy in the case of distal obstruction), during (temporary ileostomy for the diversion of faeces) or after (end colostomy for anastomotic leak). Height of the anastomosis was recorded as high (anastomosis to the intraperitoneal rectum), low (anastomosis to the extraperitoneal rectum) or ultralow (coloanal anastomosis).9 Post-operative variables extracted were length of post-operative stay, time defunctioned with a stoma, anastomotic leak, pelvic abscess, post-operative ileus and anastomotic stricture. The presence of other complications was also recorded and graded according to the Clavien-Dindo classification for severity.10 For patients with primary colorectal cancer, the pathological TNM stage and use of adjuvant chemotherapy and/or radiotherapy were noted.
The primary outcome for this study was the occurrence of ARS at yearly time points from 1 to 5 years post-operatively. These time points coincide with the New Zealand National Colorectal Cancer Guidelines which mandate clinic follow-up at 6 months, 12 months and then yearly until 5 years post-operatively.11 Six symptoms were used in the definition of ARS: faecal incontinence, urgency, increased frequency (defined as four or more bowel motions/day), constipation, sensation of incomplete evacuation or changes to stool consistency (classified as ‘loose’, ‘hard’ or ‘fluctuating’). This information was retrieved by manually searching through all surgical follow-up clinic letters. Description of specific symptoms within the text of the clinic letter was used to record each as ‘present’ or ‘not present’; if not reported, this was recorded as ‘not specified’. ARS was broadly defined as the presence of any one or more of the above six symptoms. Patients therefore required at least one of the above six symptoms to be explicitly identified in order to be classified as having ARS at a given time point. Patients who were temporarily defunctioned were followed starting from the time of stoma reversal, and symptoms recorded yearly from this point onwards.
Statistical analysis was performed using SPSS for Windows (Version 19; SPSS, Chicago, IL, USA). Analysed variables were then stratified according to the presence or absence of ARS at each of the five yearly post-operative time points. Missing data were excluded in a listwise fashion from all further analyses. Parametricity was determined using the Shapiro-Wilk test, with normally distributed data being expressed as mean ± standard deviation (SD) and nonparametric data as median ± interquartile range (IQR). Univariate analysis was carried out for each time period using the χ 2 test for categorical variables and the Spearman’s Rho test for nonparametric continuous variables. All variables which were significant or near-significant (p < 0.15) were entered into a logistic regression model. Multiple regression models for each time point were created if two or more input variables were related, thereby avoiding erroneous correction. Results were considered statistically significant if p < 0.05.
Results
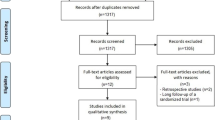
In total, 495 anterior resections were undertaken by the Colorectal Unit at ACH over the study period. Of these, 218 were excluded from analysis as there was no reporting of evacuatory function at or beyond 1 year post-operatively. This was most commonly due to patients undergoing surgery for non-malignant indications such as diverticulitis (n = 73), other pelvic cancers (n = 15) or early discharge from colorectal follow-up due to advanced age (n = 20) or metastatic disease (n = 17). Patients defunctioned with a loop ileostomy at the time of index surgery who had not subsequently undergone reversal were also excluded (n = 20). A total of 277 cases had post-operative reporting of evacuatory function and were included in the current study. If patients died or were discharged from the clinic during the study period, data was included until they were lost to follow-up. Of these, 202 patients (72.9 %) were recorded as having ARS at some point post-operatively. Increased frequency (29 %) was the most commonly reported symptom of ARS (Fig. 1). ARS prevalence decreased progressively from 61.1 % at 1 year to 43.4 % at 5 years (Table 2). The mean duration of post-operative follow-up was 2.71 years (range 1–5 years). Data extraction for the final database was >99 % complete for recorded patient and peri-operative variables.
Baseline characteristics can be found in Table 1. Basic descriptive statistics showing significant correlates of ARS occurrence over the post-operative period are listed in Table 2. Given that ARS occurrence was investigated across five discrete time points, it was decided for clarity and brevity to only display significant correlates on univariate analysis in Table 2. Univariate analysis showed year of diagnosis, year of procedure, lower tumour and anastomotic heights, temporary stoma formation, pT stage and operative surgeon as recurring correlates of ARS over the post-operative period. Pelvic irradiation was significantly associated with the occurrence of ARS at any time point following surgery (Table 1) and approached significance at the 1- (p = 0.054), 2- (p = 0.053) and 3-year (p = 0.055) marks.
There was no significant difference (p < 0.05) between ARS and non-ARS populations at any time point for gender, previous abdominal surgery, GI comorbidities, pre-operative chemotherapy or radiotherapy, acute vs. elective presentation, weight, height, BMI, ASA grade, surgical approach, neo-reservoir formation, stapled vs. hand-sewn anastomosis, length of post-operative stay, post-operative ileus and post-operative chemotherapy and radiotherapy. Anastomotic leak was not a significant correlate at any time point, although anastomotic stricture was at 1 and 3 years. Complication grade and pelvic abscess formation were also significant at 3 and 4 years, respectively.
Logistic regression analysis revealed a number of independent predictors for ARS occurrence at the yearly time points (Table 3). Care was taken to avoid erroneous correction of related variables on regression analysis by creating multiple models for each time point. Variables independently substituted into separate regression models were anastomotic height vs. ileostomy formation at index procedure; pelvic abscess vs. stricture vs. complication grade vs. time with stoma; weight vs. BMI; and pre-operative chemotherapy vs. pre-operative radiotherapy. Tumour height and year of diagnosis were similarly excluded from regression as they would speciously correct for the also significant and more clinically relevant variables of anastomotic height and year of procedure, respectively.
At 1 year, regression showed both low (odds ratio (OR) 2.11, 95 % confidence interval (CI) 1.05–4.27; p = 0.04) and ultralow (OR 4.34, 95 % CI 1.05–18.04; p = 0.01) anastomoses to be independent predictors of ARS occurrence, with only ultralow anastomoses persisting as a predictor at 2 years (OR 4.50, 95 % CI 1.17–17.28; p = 0.03). Post-operative chemotherapy was a significant independent predictor of ARS at 1 year only (OR 1.93, 95 % CI 1.04–3.57; p = 0.03). Presenting symptoms of an obstructive nature alone or combined with PR bleeding, ileostomy formation both before and at the time of the index procedure and year of procedure were also predictors of ARS at 2 years.
Temporary ileostomy formation at procedure was the only significant independent predictor of ARS occurrence at 3 (OR 4.17, 95 % CI 1.04–16.78; p = 0.04), 4 (OR 8.05, 95 % CI 1.21–53.60; p = 0.03) and 5 years (OR 49.60, 95 % CI 2.17–1134.71; p = 0.02) even with correction for anastomotic height. To ensure that the strong relation between ultralow anastomosis and temporary ileostomy formation did not bias this result, sub-analyses were undertaken excluding all ultralow procedures from regression models. Temporary ileostomy formation at procedure persisted as a significant predictor of ARS at 3 (OR 4.87, 95 % CI 1.06–22.42; p = 0.04), 4 (OR 13.80, 95 % CI 1.34–142.21; p = 0.03) and 5 years (OR 69.68, 95 % CI 1.41–3441.86; p = 0.03) post-operatively.
Discussion
Evacuatory dysfunction is a common sequela of distal colorectal resection and has been reported to affect up to 90 % of patients following surgery.4 Symptoms were initially believed to be due to mucosal irritability related to post-operative tissue healing and therefore short-lived. This is corroborated by the observation that evacuatory dysfunction is generally most prominent in the first 1–2 years post-operatively.3 However, recent studies have observed that ARS may persist for over a decade post-operatively,12 suggesting that the pathogenesis is more likely the result of permanent changes in colonic and rectal physiology.3 Indeed, it has been shown in the present study that 43 % of the anterior resection cohort was symptomatic 5 years after surgery. The lack of a uniform reporting tool for ARS coupled with its propensity to be ‘eclipsed’ by mortality-dependent oncologic outcomes has led to an underestimation of the true burden and functional impact of this condition.
The absence of an internationally accepted and validated definition for ARS has led to huge variation in reporting of its incidence and has also hindered the ability to delineate risk factors. This has also conferred a poor understanding of the post-surgical physiologic changes which underpin ARS. There appears to be a general consensus in the literature that a practical definition for ARS is a change in post-operative bowel function causing an altered QoL.3, 13–16 Difficulty translating these subjective features into tangible endpoints is likely to have contributed to impaired internal and external validity of studies investigating ARS. Recent work has led to the development and validation of scoring systems specifically for ARS.14, 17 However, these tools were designed for prospective work and were therefore not appropriate to utilise in the present study. Nonetheless, an attempt was made in the present retrospective review to conform to the above definition by manually evaluating all clinic letters. It was assumed that patients with troubling bowel symptoms impacting QoL would raise these during surgical follow-up, especially when prompted by the examining clinician. If any one or more of the six recorded evacuatory symptoms was reported in the clinic letter, the patient was deemed to have ARS at that particular time point. This broad definition of ARS was decided on to attempt to capture all patients with post-operative evacuatory dysfunction. Despite the strong association between urinary/sexual symptoms and the ARS complex,15, 18, 19 we elected to not evaluate these symptoms as they are not routinely recorded during colorectal follow-up and detract from the primary outcome of preservation or absence of ‘normal’ bowel function.
The pathophysiologic mechanisms which underpin the development of sustained post-operative evacuatory dysfunction remain unclear but are believed to be related principally to iatrogenic damage of pelvic nerves or disruption of neuromuscular continuity within the rectal wall.20 This in turn is believed to lead to abnormalities of rectal sensation and compliance and, perhaps also, to interfere with the wholly intramural recto-anal reflex.21 It has also been suggested that the reduced capacity of a neo-rectum following formation of a lower anastomosis may contribute to the ARS symptoms of clustering and increased frequency.3 Progressively lower anastomoses will necessarily lead to a shorter length of rectal remnant and hence may be expected to be correlated with poorer post-operative functional outcomes. This has been the finding of previous studies and indeed the present cohort, which identified lower rectal anastomoses as independent predictors for the development of ARS at the 1- and 2-year time points.20, 22–25 However, it is interesting to note that this association did not persist on regression analysis beyond 2 years post-operatively. This finding echoes that of other studies and suggests that the neo-rectum is endowed with the capacity to adapt over time.22, 26 Previous studies have detailed the relationship between anastomotic leak or pelvic abscess formation and subsequent anastomotic stricture with ARS.27 Anastomotic stricture, pelvic abscess and Clavien-Dindo complication grade were associated with ARS at various time points but did not persist on multivariate analysis. Similarly, the effect of a neo-reservoir on post-operative function has been well reported in the literature.28 These relationships were not present in our analysis, which may reflect a limitation of the retrospective nature of this study. Pelvic radiation was a significant correlate in our study when comparing patients with ARS at any time point against those who did not have ARS at any stage. This was not repeated at any of the individual time points, which may reflect the broad definition of ARS used in our study, or alternatively smaller patient numbers at the individual time points compared to the whole cohort.
Post-operative chemotherapy was a significant predictor of ARS occurrence at 1 year post-operatively. Both diarrhoea and constipation are known side effects of chemotherapy, likely stemming from alimentary mucositis.29 This relationship did not persist beyond the 1-year time point, thus is unlikely to represent a meaningful factor in the aetiology of ARS. It is more likely attributable to chemotherapy-induced evacuatory dysfunction, which is short-lived in comparison to ARS.30
Presenting symptoms of an obstructive nature, alone or combined with PR bleeding, were a significant independent predictor of ARS occurrence at 2 years post-operatively. The reason for this is unclear and may be a spurious finding given its appearance at a single time point.
It has been shown that diverting loop ileostomy can cause structural and functional changes to the distal bowel segment. These include atrophy of the gut wall and anal sphincter musculature, villus atrophy, mucosal inflammation (leading to ‘diversion colitis’) and impaired absorptive and secretory function.31–33 It is postulated that these changes may contribute to the symptoms of ARS upon restoration of intestinal continuity. However, this effect is likely to be short-lived as it has been demonstrated that muscle strength and normal mucosal function are rapidly regained after stoma reversal.31, 33, 34
The present study has shown that formation of temporary ileostomy at the time of index surgery was an independent predictor of ARS occurrence at 2, 3, 4 and 5 years post-operatively, both with and without correction for anastomotic height. This finding suggests that the effect of faecal diversion on downstream function may be more permanent than was previously thought and could ostensibly be related to changes in the submucosal and myenteric plexi of the enteric nervous system (ENS) rather than those observed in the mucosa or muscularis propria. Indeed, this hypothesis is corroborated by rodent models which have shown that a period of faecal diversion is accompanied by extensive remodelling of the ENS, often involving neuronal loss, and the reversibility of these changes remains unknown.35–37
A second hypothesis relates to mechanical disruption of intestinal continuity at the level of the ileum. The distal ileum is functionally unique in that it patterns upstream and downstream gut motility via an array of complex neural and motor reflexes believed to be largely regulated by the ENS.38–40 These reflexes have yet to be accurately characterised, but their disruption has been implicated in functional gastrointestinal disease. Some symptoms of irritable bowel syndrome (IBS) are similar to those of ARS sufferers, and it has been shown that aberrations of distal ileal function, potentially effected by ENS remodelling, may be an important pathophysiologic step in the development of IBS for patients with a tendency to both constipation and diarrhoea.39, 41
A further consideration at this level is the method in which ileal continuity is re-established. Several recent reviews comparing sutured and stapled techniques for ileostomy closure report a significant reduction in post-operative small-bowel obstruction in patients with stapled anastomoses.42–44 Stapled anastomoses provide a larger lumen than sutured and are therefore less prone to further constriction by post-operative oedema.42, 44 It has also been postulated that fibrosis may later occur at this site resulting in a clinically significant stricture,42 particularly in patients with sutured anastomoses; this may in turn lead to obstructive symptoms that could reflect those seen in ARS. However, studies with sufficient follow-up to investigate this theory are yet to be performed.
Although the degree of functional and mechanical compromise that occurs as a result of disruption of intestinal continuity and ENS remodelling is unclear, it provides a plausible mechanism to explain the persistence of ARS symptoms in those who had an ileostomy. However, it is also possible that the aetiology of ARS in these patients is multifactorial involving muscular, mucosal and neuronal changes in both diverted ileum and colon, and this may indeed explain the wide variability in clinical symptoms. Further investigation is required to determine the effect a defunctioning loop ileostomy has on changes in upstream and downstream human bowel morphology and motility.
The prevalence of ARS in our cohort decreased progressively over the 5-year follow-up period. This may be related to a greater proportion of patients experiencing functional recovery; successful use of anti-diarrhoeal, laxative or bulking medication; or an improved ability of patients to cope with ARS symptoms over time and hence not perceive them as troublesome. The use of bowel-altering medication and dietary modifications have been linked to improved post-operative evacuatory function in some patients.45, 46 However, changes in bowel function as a result of these interventions are likely to be more rigorously trialled and adopted in ARS patients early on in their post-operative course and are increasingly unlikely to play a role in reduced incidence past the first post-operative year. The decline in ARS prevalence over the observed post-operative time points is therefore more likely related to functional recovery than patients suddenly identifying a new intervention to control their evacuatory dysfunction.
An important limitation of this study is its retrospective nature. Although this meant that missing data could not be reconciled, the final dataset was >99 % complete for patient and peri-operative variables. This also impacted on the definition of ARS that could be applied, as previously discussed. While far from optimal, such a limitation of retrospective investigation cannot be easily overcome. Secondly, it was observed that some confidence intervals in the regression model were relatively broad, and this may be attributed to the relatively small number of patients being followed up. The strength of association between the reported risk factors and the development of ARS is therefore unclear. However, the consistency of results across contiguous time points strongly suggests that temporary diverting ileostomy and anastomotic height are independent risk factors for ARS development and warrant further investigation. A final consideration is the 12-year period over which data was included. Changes in chemoradiotherapy regimens and surgical technique (for example, the wider utilisation of laparoscopic surgery) have occurred over this period that were not readily identifiable on retrospective evaluation. However, this would have been corrected to some degree by the input of ‘procedure year’ in all regression analyses.
Future research should involve prospective analysis of clinical risk factors, with the use of a consistent and validated approach to recording ARS occurrence and severity. Further risk factor analysis may not only facilitate the development of a predictive stratification tool for ARS following surgery but stand to provide insight into the aetiology of this condition and inform preventive and management strategies.
Conclusions
The prevalence of ARS in our study population decreased progressively from 61 % at 1 year to 43 % at 5 years post-operatively. Low and ultralow anastomotic heights and post-operative chemotherapy were independent clinical predictors for ARS occurrence at 1 year. Obstructive presenting symptoms and ultralow anastomoses were independent predictors at 2 years. Temporary diversion ileostomy was a recurring independent predictor of ARS occurrence at the 2–5-year time points even after correcting for anastomotic height. It appears that defunctioning the colon may have long-term effects on evacuatory function following anterior resection. Further prospective assessment is required to facilitate more accurate risk factor assessment and to evaluate the long-term effect of defunctioning ileostomy.
References
Kapiteijn E, Marijnen CAM, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJT, Pahlman L, Glimelius B, Van Krieken JHJM, Leer JWH, Van De Velde CJH. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001;345(9):638-646.
Law WL, Chu KW. Anterior resection for rectal cancer with mesorectal excision: A prospective evaluation of 622 patients. Ann Surg. 2004;240(2):260-268.
Bryant CLC, Lunniss PJ, Knowles CH, Thaha MA, Chan CLH. Anterior resection syndrome. The Lancet Oncology. 2012;13(9):e403-e408.
Desnoo L, Faithfull S. A qualitative study of anterior resection syndrome: The experiences of cancer survivors who have undergone resection surgery. European Journal of Cancer Care. 2006;15(3):244-251.
Landers M, McCarthy G, Savage E. Bowel symptom experiences and management following sphincter saving surgery for rectal cancer: A qualitative perspective. European Journal of Oncology Nursing. 2012;16(3):293-300.
Coco C, Valentini V, Manno A, Rizzo G, Gambacorta MA, Mattana C, Verbo A, Picciocchi A. Functional results after radiochemotherapy and total mesorectal excision for rectal cancer. Int J Colorectal Dis. 2007;22(8):903-910.
Cornish JA, Tilney HS, Heriot AG, Lavery IC, Fazio VW, Tekkis PP. A meta-analysis of quality of life for abdominoperineal excision of rectum versus anterior resection for rectal cancer. Annals of Surgical Oncology. 2007;14(7):2056-2068.
Pachler J, Wille-Jørgensen P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane database of systematic reviews (Online). 2012;12.
Lowry AC, Simmang CL, Boulos P, Farmer KC, Finan PJ, Hyman N, Killingback M, Lubowski DZ, Moore R, Penfold C. Consensus statement of definitions for anorectal physiology and rectal cancer*. Colorectal Disease. 2001;3(4):272-275.
Dindo D, Demartines N, Clavien P-. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205-213.
New Zealand Guidelines Group. Management of early colorectal cancer - evidence-based best practice guidelines. Wellington: New Zealand Guidelines Group; 2011.
Lundby L, Krogh K, Jensen VJ, Gandrup P, Qvist N, Overgaard J, Laurberg S. Long-term anorectal dysfunction after postoperative radiotherapy for rectal cancer. Dis Colon Rectum. 2005;48(7):1343-1349.
Rickert A, Kienle P. Incontinence and bowel disorders after colorectal resection. Journal fur Gastroenterologische und Hepatologische Erkrankungen. 2013;11(4):14-22.
Emmertsen KJ, Laurberg S. Low anterior resection syndrome score: Development and validation of a symptom-based scoring system for bowel dysfunction after low anterior resection for rectal cancer. Ann Surg. 2012;255(5):922-928.
Hassan I, Cima RR. Quality of life after rectal resection and multimodality therapy. J Surg Oncol. 2007;96(8):684-692.
Chen TY, Emmertsen KJ, Laurberg S. What are the best questionnaires to capture anorectal function after surgery in rectal cancer? Current Colorectal Cancer Reports. 2014:1-7.
Temple LK, Bacik J, Savatta SG, Gottesman L, Paty PB, Weiser MR, Guillem JG, Minsky BD, Kalman M, Thaler HT. The development of a validated instrument to evaluate bowel function after sphincter-preserving surgery for rectal cancer. Diseases of the colon & rectum. 2005;48(7):1353-1365.
Keating JP. Sexual function after rectal excision. ANZ J Surg. 2004;74(4):248-259.
Vironen JH, Kairaluoma M, Aalto A-, Kellokumpu IH. Impact of functional results on quality of life after rectal cancer surgery. Dis Colon Rectum. 2006;49(5):568-578.
Pucciani F. A review on functional results of sphincter-saving surgery for rectal cancer: The anterior resection syndrome. Updates in Surgery. 2013;65(4):257-263.
Efthimiadis C, Basdanis G, Zatagias A, Tzeveleki I, Kosmidis C, Karamanlis E, Harlaftis N. Manometric and clinical evaluation of patients after low anterior resection for rectal cancer. Techniques in coloproctology. 2004;8(1):s205-s207.
Ziv Y, Gimelfarb Y, Igov I. Post anterior rectal resection syndrome - a retrospective multicentre study. Colorectal Disease. 2013;15(6):e317-e322.
Welsh FKS, McFall M, Mitchell G, Miles WFA, Woods WGA. Pre-operative short-course radiotherapy is associated with faecal incontinence after anterior resection. Colorectal Disease. 2003;5(6):563-568.
Bretagnol F, Troubat H, Laurent C, Zerbib F, Saric J, Rullier E. Long-term functional results after sphincter-saving resection for rectal cancer. Gastroenterol Clin Biol. 2004;28(2):155-159.
Lewis WG, Martin IG, Williamson ME, Stephenson BM, Holdsworth PJ, Finan PJ, Johnston D. Why do some patients experience poor functional results after anterior resection of the rectum for carcinoma? Diseases of the colon & rectum. 1995;38(3):259-263.
Harris G, Lavery I, Fazio V. Function of a colonic J pouch continues to improve with time. Br J Surg. 2001;88(12):1623-1627.
Nesbakken A, Nygaard K, Lunde O. Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancer. Br J Surg. 2001;88(3):400-404.
Brown CJ, Fenech D, McLeod RS. Reconstructive techniques after rectal resection for rectal cancer. Cochrane Database Syst Rev. 2008;2.
Gibson RJ, Keefe DM. Cancer chemotherapy-induced diarrhoea and constipation: Mechanisms of damage and prevention strategies. Supportive Care in Cancer. 2006;14(9):890-900.
Mitchell EP. Gastrointestinal toxicity of chemotherapeutic agents. . 2006;33(1):106-120.
Sailer M, Fein M, Fuchs K-, Bussen D, Grun C, Thiede A. Morphologic changes of the anal sphincter musculature during and after temporary stool deviation. Langenbeck's Archives of Surgery. 2001;386(3):183-187.
Williams L, Armstrong M, Finan P, Sagar P, Burke D. The effect of faecal diversion on human ileum. Gut. 2007;56(6):796-801.
Geraghty JM, Talbot IC. Diversion colitis: Histological features in colon and rectum after defunctioning colostomy. Gut. 1991;32(9):1020-1023.
Deruyter L, Delvaux G, Willems G. Restoration of colorectal continuity reverses atrophy in human rectal mucosa. Dig Dis Sci. 1990;35(4):488-494.
Braganca De Vasconcellos Fontes R, Froes LB, Omar ED, Liberti EA. The myenteric plexus of the rat colon after fecal stream diversion: A morpho-quantitative study. Autonomic Neuroscience: Basic and Clinical. 2004;114(1-2):39-46.
Ekclund KM, Ekblad E. Structural, neuronal, and functional adaptive changes in atrophic rat ileum. Gut. 1999;45(2):236-245.
Chaudhury A, Shariff A, Srinivas M, Sabherwal U. Changes in nitrergic innervation of defunctionalized rat colon after diversion colostomy. Neurogastroenterology & Motility. 2004;16(4):475-487.
Spiller RC, Trotman IF, Higgins BE, Ghatei MA, Grimble GK, Lee YC, Bloom SR, Misiewicz JJ, Silk DB. The ileal brake–inhibition of jejunal motility after ileal fat perfusion in man. Gut. 1984;25(4):365-374.
Husebye E. The patterns of small bowel motility: Physiology and implications in organic disease and functional disorders. Neurogastroenterology and Motility. 1999;11(3):141-162.
Phillips SF, Quigley EM, Kumar D, Kamath PS. Motility of the ileocolonic junction. Gut. 1988;29(3):390-406.
Kellow JE, Phillips SF, Miller LJ, Zinsmeister AR. Dysmotility of the small intestine in irritable bowel syndrome. Gut. 1988;29(9):1236-1243.
Gong J, Guo Z, Li Y, Gu L, Zhu W, Li J, Li N. Stapled vs hand suture closure of loop ileostomy: A meta‐analysis. Colorectal Disease. 2013;15(10):e561-e568.
Sajid M, Craciunas L, Baig M, Sains P. Systematic review and meta-analysis of published, randomized, controlled trials comparing suture anastomosis to stapled anastomosis for ileostomy closure. Techniques in coloproctology. 2013;17(6):631-639.
Markides GA, Wijetunga IU, Brown SR, Anwar S. Meta-analysis of handsewn versus stapled reversal of loop ileostomy. ANZ J Surg. 2014.
Nikoletti S, Young J, Levitt M, King M, Chidlow C, Hollingsworth S. Bowel problems, self-care practices, and information needs of colorectal cancer survivors at 6 to 24 months after sphincter-saving surgery. Cancer Nurs. 2008;31(5):389-398.
Sloots K, Bartlett L. Practical strategies for treating postsurgical bowel dysfunction. J Wound Ostomy Continence Nurs. 2009;36(5):522-527.
Conflict of Interest
The authors have no conflicts of interest or sources of funding to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was previously presented at the Royal Australasian College of Surgeons Annual Scientific Congress, Singapore, 5–9 May 2014.
Rights and permissions
About this article
Cite this article
Wells, C.I., Vather, R., Chu, M.J.J. et al. Anterior Resection Syndrome—A Risk Factor Analysis. J Gastrointest Surg 19, 350–359 (2015). https://doi.org/10.1007/s11605-014-2679-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2679-x