Abstract
Introduction
The Sendai Consensus Guidelines (SCG) was formulated in 2006 to guide the management of intraductal papillary mucinous neoplasms (IPMN). The main area of controversy is the criteria for selection of branch duct (BD)-IPMN for resection. Although these guidelines have gained widespread acceptance, there is limited data to date supporting its use. This systematic review is performed to evaluate the utility of the Sendai Consensus Guidelines (SCG) for BD-IPMN.
Methods
Studies evaluating the clinical utility of the SCG in surgically resected neoplasms were identified. The SCG were retrospectively applied to all resected neoplasms in these studies. BD-IPMNs which met the criteria for resection were termed SCG+ve and those for surveillance were termed SCG−ve.
Results
Twelve studies were included, of which, 9 were suitable for pooled analysis. There were 690 surgically resected BD-IPMNs, of which, 24 % were malignant. Five hundred one BD-IPMNs were classified as SCG+ve and 189 were SCG−ve. The positive predictive value (PPV) of SCG+ve neoplasms ranged from 11 to 52 % and the NPV of SCG−ve neoplasms ranged from 90 to 100 %. Overall, there were 150/501 (29.9 %) of malignant BD-IPMNs in the SCG+ve group and 171/189 (90 %) of benign BD-IPMNs in the SCG−ve group. Of the 18 reported malignant (11 invasive) BD-IPMNs in the SCG−ve group, 17 (including all 11 invasive) were from a single study. When the results from this single study were excluded, 170/171 (99 %) of SCG−ve BD-IPMNs were benign.
Conclusion
The results of this review confirm the limitations of the SCG for BD-IPMN. The PPV of the SCG in predicting a malignant BD-IPMN was low and some malignant lesions may be missed based on these guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The management approach of pancreatic cystic neoplasms has been constantly evolving as the result of the improved understanding of the natural history of these neoplasms.1,2 In the past, the general consensus was that all mucinous cystic neoplasms were potentially malignant or malignant and should be surgically resected whereas serous cystic neoplasms were benign and could be managed conservatively.3 – 5 However, in recent times, with increasing knowledge of the natural history of these neoplasms;6 – 8 a more conservative approach has been adopted as more clinicians have realized that many benign branch-duct intraductal papillary mucinous neoplasms (BD-IPMNs) can be managed via surveillance.2,9 Today, it is widely accepted that main-duct (MD)-IPMNs and mixed-type (MT)-IPMNs should be distinguished from BD-IPMNs.2,9 This is because MD- and MT-IPMNs are associated with a high risk of malignancy in up to 92 % of cases10 and in general, should be resected in surgically fit patients.2,9,11 On the other hand, BD-IPMNs harbor a risk of malignancy in only approximately 15–25 % of cases and many patients may be managed via surveillance.10,11
In 2006, an international consensus by a panel of experts published guidelines2 for the management of IPMNs and mucinous cystic neoplasms (MCNs). These guidelines became commonly known as the Sendai Consensus Guidelines (SCG) and were updated recently in 2012 (ICG 2012) (Table 1).9 It is important to note that these guidelines9 were formulated based on expert opinion after extensive review of the available literature12,13 and not on robust clinical data. Interestingly, despite its widespread acceptance, there is limited data to date to support its use and its safety remains debatable.8,11,14 – 16 Several authors have questioned the safety of these guidelines for BD-IPMN because of the real risk of BD-IPMNs harboring a malignancy.10,17 According to the SCG, all main-duct intraductal papillary neoplasms (MD-IPMNs), mixed-type (MT) IPMNs, and MCNs should be resected whereas selected non-malignant BD-IPMNs could be observed.2,9 The main area of controversy in these guidelines was the selection of BD-IPMN for resection whereby it was recommended that only BD-IPMN which were >3 cm in size or those <3 cm which were symptomatic, had mural nodules, dilated main pancreatic duct, or positive cytology should be resected.2 Although the value of each of the individual parameters in the SCG such as presence of mural nodules, dilated duct, and size of >3 cm have since been validated by two recent systematic reviews16,18; to our knowledge, a systematic review of the utility of the guidelines, as a whole, has never been performed.
The aim of the present study was to perform a systematic review of the current literature to determine the utility of the SCG in the management of BD-IPMNs. This review was limited to studies which reported on all patients who underwent surgical resection with a definitive pathological diagnosis. The clinical utility of the SCG was determined by evaluating the positive predictive value (PPV) of the guidelines in predicting a malignant BD-IPMN and its negative predictive value (NPV) in predicting a benign BD-IPMN.
Materials and Methods
A computerized search of the PubMed database was conducted for studies evaluating the utility of the SCG for IPMNs published in English from 1 January 2006 to 31 July 2013 (the SCG was published in 2006). The keywords “IPMN” and “intraductal papillary mucinous neoplasm” were used. The reference lists of articles identified were subsequently examined to find relevant studies that had not been identified by the database searches. Only original clinical studies with full-text descriptions were included. The final inclusion of articles was determined by consensus between two authors (Goh and Tan); when this failed, a third author (Ooi) adjudicated. This study was conducted according to PRISMA guidelines.19
Inclusion and Exclusion Criteria
Two authors (Goh and Tan) independently identified and screened the search findings for potentially eligible studies. Inclusion criteria required the studies to (i) be written in English and published in full-text, (ii) reporting the SCG, and (iii) surgically resected and pathologically confirmed cases. Studies were evaluated for overlapping cohorts of patients based on the center of study and period of recruitment. Exclusion criteria were (i) abstracts, letters, editorials, expert opinions, technical notes, case reports, reviews; (ii) studies which did not classify cystic neoplasms according to the SCG; and (iii) studies focusing specifically on multifocal IPMN.
Definitions
Depending on the study methodology, the malignant potential of IPMN was classified on the basis of the most aggressive histological epithelial changes according to the two World Health Organization (WHO) classification systems.20,21 Neoplasms were graded as low-grade dysplasia/adenoma, intermediate-grade dysplasia/borderline, high-grade dysplasia (HGD)/carcinoma in situ (CIS) or invasive carcinoma.20,21 In this study, neoplasms were regarded as benign if they were classified as adenoma/low-grade dysplasia or borderline/intermediate-grade dysplasia. Malignant neoplasms were those classified as HGD/CIS or invasive carcinoma. When the criteria for surgical resection based on the SCG were met, these neoplasms were termed SCG+ve whereas those which did not meet SCG criteria for resection were termed SCG−ve.
Data Extraction and Outcomes of Interest
Data were extracted by two independent authors (BKG and DMT) using standardized forms. Data recorded included patient and study characteristics, treatment of IPMN, study definition of BD- and MD-IPMN, study definition of SCG+ve lesions, type of preoperative imaging performed, final pathology including malignant potential of IPMN, and classification of IPMN according to SCG+ve or SCG−ve lesions.
Statistical Analyses
The PPV of the SCG was defined as the N of malignant BD-IPMN (HGD + invasive)/total N of SCG+ve BD-IPMN whereas the NPV of the SCG was defined as the N of benign BD-IPMN/total N of SCG−ve BD-IPMN.
Results
The PubMed search yielded 1,106 articles which underwent abstract review. Following abstract review, 54 studies underwent full-text evaluation, which yielded 13 potential titles that evaluated the SCG.8,10,11,14,15,22 – 29 Of these 13 titles, 2 studies were excluded. The study by Baiocchi et al. was excluded as not all patients underwent surgical resection with a pathological diagnosis and separate data for the surgically resected patients was not available.29 The study by Sawhney et al. was also excluded as its definition of SCG+ve neoplasms deviated substantially from the original criteria.24 Essential criteria such as the presence of mural nodules and the presence of symptoms were not considered in the study.24 Hence, 11 studies were included based on our literature search. Additionally, we also included our recent study which analyzed the utility of the consensus guidelines in cystic mucinous neoplasms.30 Finally, 12 studies were included in this systematic review8,10,11,14,15,22,23,25 – 28,30 (Table 2). Seven studies included only BD-IPMNs8,10,11,22,23,26,27 and two studies included both MD- and BD-IPMNs but performed a separate analysis of BD-IPMNs.15,30 The data in these nine studies8,10,11,15,22,23,26,27,30 were used for subsequent pooled analysis of BD-IPMNs. The other three studies included in this systematic review were not included in the pooled analysis as one included both MD- and BD-IPMNs28 and the other two included a mixed group of pancreatic cystic neoplasms.14,25 There was insufficient data on BD-IPMNs alone for pooled analysis in these three studies.
Study and Patient Characteristics
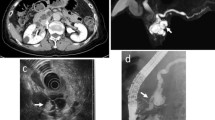
The detailed study characteristics of the 12 studies are summarized in Tables 2 and 3. The studies utilized a wide variety of imaging modalities to evaluate the neoplasms including computed tomography (CT), magnetic resonance imaging (MR), endoscopic ultrasonography (EUS), endoscopic retrograde cholangiopancreatography (ERCP), and intraductal ultrasound (IDUS).
Pooled analysis of 690 surgically resected BD-IPMNs in the nine studies is summarized in Table 4. There were a total of 168 malignant (94 invasive) BD-IPMNs. The incidence of malignant BD-IPMN ranged from 8 to 47 % in these nine surgical series and the overall incidence of a malignant BD-IPMN was 24 %. Five hundred one neoplasms were SCG+ve and 189 were SCG−ve.
Definitions of SCG in the Various Studies
Although these studies were performed to evaluate the utility of the SCG, there were some variations in the definition of SCG+ve among the different studies. According to the original SCG; a cut-off of ≥10 mm was used to define MD-IPMN and a main pancreatic duct (MPD) of >6 mm was used to define a dilated duct in BD-IPMN (Table 1). In this study, only four studies utilized all this criteria.4,10,15,23 Six studies used different criteria to define MD-IPMN11,8,25,27 and a dilated MPD in BD-IPMN.26,27,30 Furthermore, nine studies did not consider fluid cytology analysis in their SCG criteria.10,11,14,22,25 – 28,30
Utility of the SCG in BD-IPMN
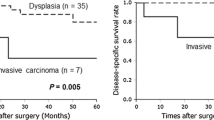
The PPV of the SCG+ve criteria in predicting a malignant BD-IPMN in the nine studies ranged from 11 to 52 %8,10,11,15,22,23,26,27,30 (Table 3). The NPV of the SCG−ve criteria for BD-IPMN ranged from 71 to 100 %. Pooled analysis demonstrated that, overall, there were 150 malignant (83 invasive) of 501 BD-IPMNs in the SCG+ve group (30 %) (Table 4). In the SCG−ve group, 18 of 189 BD-IPMN were malignant (10 %) which included 11 invasive neoplasms (Table 4).
Features of Malignant BD-IPMN in the SCG−ve Group
It is interesting to note that 17 of 18 malignant BD-IPMN in the SCG−ve group were from a single study including all 11 invasive BD-IPMNs.11 In this study, final pathological examination demonstrated that 8 of the 17 patients had focal involvement of the main pancreatic duct and strictly, by definition, should have been considered as MT-IPMNs.11 The remaining patient was reported by Nagai et al. which described a BD-IPMN demonstrating CIS in a patient with a 25-mm cyst with no mural nodules but associated with a dilated MPD of 5 mm.23 When the results from this single study was excluded, there were 170/171 benign BD-IPMNs (99 %) among SCG−ve lesions. In the remaining three studies14,25,28 not included in the pooled analysis, there was only one malignant IPMN in the SCG−ve group.14 This lesion was a 2.5-cm BD-IPMN with HGD which demonstrated a dilated MPD of 5 mm and positive fluid cytology.14 As the authors did not include fluid cytology in their criteria, this was considered a SCG−ve lesion in the study.14
Discussion
Currently, there is general consensus that MD- and MT-IPMN should be resected due to the high frequency of malignancy whereas selected BD-IPMNs may be managed conservatively.2,9,22 However, the indications for resection of BD-IPMN remain unclear11,23 although international consensus guidelines have been developed and widely adopted.2,22 The SCG was developed based on results from several large retrospective studies reporting that selected BD-IPMNs were benign and could be safely managed via surveillance.2,12 Although two recent systematic reviews16,18 have demonstrated that the individual parameters used in these guidelines were useful for predicting malignancy in BD-IPMN, there is limited data to date evaluating the overall utility of these guidelines.11
The overall incidence of malignancy of BD-IPMNs in this review ranged from 8 to 47 %. This is almost certainly due to selection and publication bias of the different studies. Sadakahari et al. only studied flat BD-IPMNs, i.e., BD-IPMNs without mural nodules. Hence, it was not surprising that the overall incidence of malignancy was the lowest at 8 %.26 On the other hand, in the series by Mimura et al., only patients who were SCG+ve underwent resection which explained the high incidence of malignancy of 47 %.15
The present systematic review demonstrated that the SCG has a low PPV ranging from 11 to 52 %. Overall, only 150 among 501 (30 %) SCG+ve BD-IPMNs were invasive or had HGD. Hence, utilization of the SCG in the management decision making, resulted in the resection of a large number of benign BD-IPMNs. This low PPV of the SCG has been recognized by many experts and hence, the SCG has been recently updated in Fukuoka to include a high risk and worrisome risk group in an attempt to decrease the number of benign BD-IPMNs being resected.9
Of concern in this study was that the NPV of the SCG ranged from 71 to 100 %. Overall, 18 of 189 (10 %) BD-IPMNs classified as SCG−ve were malignant and there were 11 invasive neoplasms. There has been general consensus that SCG−ve BD-IPMNs are almost always benign and can be observed. This has been supported by several large studies demonstrating the safety of observing BD-IPMNs with low rates of malignant transformation.31,32 Levy et al. reported that the 5-year actuarial risk of BD-IPMNs progressing to HGD was only 15 %.33 Hence, the finding in the present review is indeed worrying. This is especially so as even in the recently updated consensus guidelines9 (Table 1), many of these patients would remain classified as low risk.9
However, an interesting and important point to note was that in 11 of the 12 studies, only two malignant BD-IPMNs were found in the SCG−ve group and both were non-invasive with a dilated MPD of 5 mm.14,23 Interestingly, the revised consensus guidelines9 has lowered the threshold for a dilated MPD to 5 mm and both these patients would not have been classified as low risk. The results from two recent reports from the Memorial Sloan-Kettering Cancer Center and the Massachusetts General Hospital were consistent with the findings of these 11 studies.34 – 36 In a letter published by the Memorial Sloan-Kettering Cancer Center; of 283 surgically resected IPMNs, 38 % were BD-IPMNs and 35 were SCG−ve. Of the 35 SCG−ve patients, 5 (14 %) had HGD but none were invasive.34 The PPV of the SCG+ve cohort was 35 %. Similarly, the Massachusetts General Hospital reported a 6.5 % risk of HGD and no invasive malignancies among 46 Sendai−ve BD-IPMNs smaller than 3 cm based on the updated guidelines.35,36
In this review, 17 malignant BD-IPMNs including all 11 invasive BD-IPMNs in the SCG−ve cohort were reported in a single study by a single institution from Germany.11 This study contained the largest number of surgically resected SCG−ve neoplasms and reported a NPV of only 71 %.11 It is difficult to establish and one can only postulate why the results of this study was markedly differed from the other 11 published surgical series.36 A major reason was that 8 of the 17 malignant neoplasms in the study were, by definition, MT-IPMNs as there was focal involvement of the main duct.11,36 However, these were included in the study as these were presumed preoperatively to be BD-IPMNs. Another possible reason could be a difference in the interpretation and definition of a symptomatic neoplasm as the authors reported that 28 of 69 SCG−ve lesions had “mild” symptoms which were not “typical” pancreatic symptoms.11 The presence of symptoms has been shown to be an important predictor of malignancy in IPMNs.37 The infrequent use of more invasive modalities such as ERCP and EUS to characterize BD-IPMN before surgical resection could possibly also account for this difference. However, the frequency of the use of EUS or ERCP was not reported in the study.11 Nonetheless, it remains controversial whether the use of EUS and ERCP, which are both highly operator dependant, may improve the preoperative characterization of BD-IPMNs.36,38 – 40 Finally, fluid cytology was also not considered in the SCG+ve criteria in this study although nine other studies who similarly did not consider fluid cytology did not demonstrate these conflicting results.
Hence, the findings in the present study seem to support the consensus decision to revise the SCG because of its low PPV whereby many benign BD-IPMNs would be resected. A low PPV was consistently observed in all the studies in this review (Tables 3 and 4). This was despite the inclusion of only surgically resected cases in this study which would most likely have resulted in a bias towards a higher incidence of malignant lesions. The NPV of SCG−ve lesions in most studies were high although some malignant lesions with HGD were occasionally missed (Tables 3 and 4). Nonetheless, it is important to take note that the results from a single study have raised concerns on the safety of the SCG as several invasive BD-IPMNs were missed.
The SCG may potentially be refined by the inclusion of additional criteria. The use of serum tumor markers which has been shown in several studies11,41,42 to predict malignancy in BD-IP MNs may potentially improve the accuracy of the SCG. In the study by Fritz et al., 8 of 11 invasive BD-IPMNs in the SCG−ve group demonstrated elevated serum tumor markers.11 Positron-emission tomographic scan has also been reported by some groups to be useful in distinguishing benign from malignant IPMNs and has been found to be superior to the SCG.25 In the future, the use of genomic, proteomic, or metabolomic analysis of cyst fluid may prove to be invaluable in selecting BD-IPMNs for resection.43,44
The strength of the present systematic review is that all patients in this study underwent surgery and a final pathological diagnosis was available for all resected BD-IPMNs.10 Hence, we were able to determine definitively the malignant potential of these neoplasms without postulating on the malignant potential of conservatively managed lesions which frequently have an insufficient period of follow-up.
However, as these were all surgically resected patients, it is very likely that the NPV and the PPV value in this study is an overestimate of the true incidence of malignancy in the SCG−ve group.14 Experienced clinicians were more likely to select patients at increased risk of malignancy for resection based on various clinical factors not used in the SCG such as serum tumor markers, age, and possibly, other unknown criteria.11,14,28 Furthermore, even within the Sendai−ve group, cysts within opposite ends of the spectrum would potentially have different risks of harboring a malignancy.36 For example, a 2.8-cm IPMN with a 4-mm duct would have a different malignant potential from a 1-cm cyst without main duct dilatation. We were also unable to determine the “true denominator” and hence, evaluate the sensitivity and specificity of the SCG as many patients with small SCG−ve neoplasms would have been observed. Finally, there were also some variations in the definitions of MD-IPMN and in the SCG criteria adopted by the different studies which may have impacted the results of this review.
In conclusion, the results of this study confirm the limitations of the SCG for BD-IPMN. The PPV of the SCG in predicting a malignant BD-IPMN is low and some malignant lesions may be missed based on these guidelines.
References
Spinelli KS, Fromwiller TE, Daniel RA, Kiely JM, Nakeeb A, Komorowski RA, Wilson SD, Pitt HA. Cystic pancreatic neoplasm. Observe or operate. Ann Surg 2004;239:651-659.
Tanaka M, Chari S, Adsay V, et al. International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatology 2006;6:17-12.
Goh BK, Tan YM, Cheow PC, Chung YF, Chow PK, Wong WK, Ooi LL. Cystic lesions of the pancreas: an appraisal of an aggressive resectional policy adopted at a single institution during 15 years. Am J Surg 2006;192:148-54.
Goh BK, Tan YM, Chung YF, et al. Pancreatic cysts: a proposed management algorithm based on current evidence. Am J Surg 2007;193(6):749-55.
Goh BK, Tan YM, Cheow PC, Chung YF, Chow PK, Wong WK, Ooi LL. Cystic neoplasms of the pancreas with mucin-production. Eur J Surg Oncol 2005;31:282-287.
Kobari M, Egawa S, Shibuya K, et al. Intraductal papillary mucinous tumors of the pancreas comprise 2 clinical subtypes: differences in clinical characteristics and surgical management. Arch Surg 1999;134:1131-36.
Terris B, Ponsot P, Paye F, et al. Intraductal papillary mucinous tumors of the pancreas confined to secondary ducts show less aggressive pathologic features as compared with those involving the main pancreatic duct. Am J Surg Pathol 2000;24:1372-77.
Pelaez-Luna M, Chari ST, Smyrk TC, et al. Do consensus indications for resection in branch duct intraductal papillary mucinous neoplasm predict malignancy? A study of 147 patients. Am J Gastroenterol 2007;102:1759-64.
Tanaka M, Fernandez-del Castillo C, Adsay V, et al. International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatology 2012;12:183-97.
Tang RS, Weinberg B, Dawson DW, et al. Evaluation of guidelines for management of pancreatic branch-duct intraductal papillary mucinous neoplasm. Clin Gastroenterol Hepatol 2008;6:815-19.
Fritz S, Klauss M, Bergmann F, et al. Small (Sendai negative) branch-duct IPMNs: not harmless. Ann Surg 2012:256:313-20.
Matsumoto T, Aramaki M, Yada K, et al. Optimal management of the branch duct type intraductal papillary mucinous neoplasms of the pancreas. J Clin Gastroenterol 2003;36:261-65.
Sugiyama M, Izumisato Y, Abe N, et al. Predictive factors for malignancy in intraductal papillary-mucinous tumors of the pancreas. Br J Surg 2003;90:1244-49.
Lee CJ, Scheiman J, Anderson MA, et al. Risk of malignancy in resected cystic tumors of the pancreas ≤3 cm in size: is it safe to observe asymptomatic patients? A multi-institutional report. J Gastrointestin Surg 2008;12:234-242.
Mimura T, Masuda A, Matsumoto I, et al. Predictors of malignant intraductal papillary mucinous neoplasm of the pancreas. J Clin Gastroenterol 2010;44(9):e224-29.
Kim KW, Park SH, Pyo J, et al. Imaging features to distinguish malignant and benign branch-duct type intraductal papillary mucinous neoplasms of the pancreas. A meta-analysis. Ann Surgery 2014;259:72-81.
Jang JY, Kim SW, Lee SE, et al. Treatment guidelines for branch duct type intraductal papillary mucinous neoplasms of the pancreas: when can we operate and observe. Ann Surg Oncol 2008;15(1):199-205.
Anand N, Sampath K, Wu Bu. Cyst features and risk of malignancy in intraductal papillary mucinous neoplasms of the pancreas: a meta-analysis. Clin Gastro Hepatol 2013;11(8):913-21.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. BMJ 2009;339.
Hruban RH, Takaori K, Klimstra DS, et al. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol 2004;28:977-87.
Adsay NV, Fukushima N, Furukawa T, Hruban RH, Klimstra DS, Kloppel G, et al. Intraductal neoplasm of the pancreas. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, editors. WHO classification of tumors of the digestive system. Lyon WHO Press; 2010. p. 304-13.
Rodriguez JR, Salvia R, Crippa S, et al. Branch-duct intraductal papillary mucinous neoplasms: observations in 145 patients who underwent resection. Gastroenterology 2007;133:72-9.
Nagai K, Doi R, Ito T, et al. Single-institution validation of the international consensus guidelines for treatment of branch duct intraductal papillary mucinous neoplasms of the pancreas. J Hepatobiliary Pancreat Surg 2009;16:353-58.
Sawhney MS, Al-Bashir S, Cury MS, Brown A, Chuttani R, Pleskow DK, Callery MP, Vollmer CM. International Consensus guidelines for surgical resection of mucinous neoplasms cannot be applied to all cystic lesions of the pancreas. Clin Gastroenterol Hepatol 2009;7:1373-76.
Pedrazzoli S, Sperti C, Pasquali C, Bissoli S, Chierichetti F. Comparison of international consensus guidelines versus 18-FDG PET in detecting malignancy of intraductal papillary mucinous neoplasms of the pancreas. Ann Surg 2011;254:971-6.
Sadakari Y, Ienaga J, Kobayashi K, et al. Cyst size indicates malignant transformation in branch duct intraductal papillary mucinous neoplasm of the pancreas without mural nodules. Pancreas 2010;39(3):232-36.
Woo SM, Ryu JK, Lee SH, et al. Branch duct intraductal papillary mucinous neoplasms in a retrospective series of 190 patients. Br J Surg 2009;96:405-11.
Cone MM, Rea JD, Diggs BS, et al. Predicting malignant intraductal papillary mucinous neoplasm: a single center review. Am J Surg 2011;201:575-79.
Baiocchi GL, Bertagna F, Gheza F, et al. Searching for indicators of malignancy in pancreatic intraductal papillary mucinous neoplasms: the value of 18FDG-PET confirmed. Ann Surg Oncol 2012;19:3574-80.
Goh BK, Thng CH, Tan DM, et al. Evaluation of the Sendai and 2012 International Consensus Guidelines based on initial cross-sectional imaging findings for the management of mucinous cystic lesions of the pancreas: a single institution experience with 114 surgically-treated patients. Am J Surg 2014 Jan 17. doi:10.1016/j.amjsurg.2013.09.031.
Maguchi H, Tanno S, Mizuno N, et al. Natural history of branch-duct intraductal papillary mucinous neoplasm in Japan. Pancreas 2011;40(3):364-70.
Salvia R, Crippa S, Falconi M, et al. Branch-duct intraductal papillary mucinous neoplasms of the pancreas: to operate or not to operate? Gut 2007;56:1086-90.
Levy P, Jouannaud V, O’Toole D, et al. Natural history of intraductal papillary mucinous tumors of the pancreas: actuarial risk of malignancy. Clin Gastroenterol Hepatol 2006;4:460-68.
Correa-Gallego C, Brennan MF, Fong Y, et al. Liberal resection for (presumed) Sendai negative branch-duct intraductal papillary mucinous neoplasms—also not harmless. Ann Surg 2013 Aug 23
Sahora K, Mino-Kenudson M, Brugge W, et al. Branch duct intraductal papillary mucinous neoplasms: does cyst size change the tip of the scale? A critical analysis of the revised international consensus guidelines in a large single-institutional series. Ann Surg 2013;258(3):466-75.
Goh BK. Sendai Consensus Guidelines for branch-duct IPMN: guidelines are just guidelines. Ann Surg 2014 Jan 16
Moriya T, Hashimoto, Traverso LW. The duration of symptoms predicts the presence of malignancy in 210 resected cases of pancreatic intraductal papillary mucinous neoplasms. J Gastrointest Surg 2011;15:762-71.
Cone MM, Rea JD, Diggs BS, et al. Endoscopic ultrasound may be unnecessary in the preoperative evaluation of intraductal papillary mucinous neoplasm. HPB (Oxford) 2011;13:112-116.
Gerke H, Jaffe TA, Mitchell RM, et al. Endoscopic ultrasound and computer tomography are inaccurate methods of classifying cystic pancreatic lesions. Dig Liver Dis 2006;38:39-44.
Brugge WR. Evaluation of pancreatic cystic lesions with EUS. Gastrointest Endosc 2004;59:698-707.
Fritz S, Hackert T, Hinz U, et al. Role of serum carbohydrate 19-9 and carcinoembryonic antigen in distinguishing between benign and invasive intraductal papillary mucinous neoplasm of the pancreas. Br J Surg 2011;98:104-110.
Goh BK, Tan YM, Thng CH, et al. How useful are clinical, biochemical, and cross-sectional imaging features in predicting potentially malignant and malignant cystic lesions of the pancreas? Results from a single institution experience with 220 surgically treated patients. J Am Coll Surg 2008;206(1):17-27.
Park WG, Wu M, Bowen R, et al. Metabolomic-derived novel cyst fluid biomarkers for pancreatic cysts: glucose and kynurenine. Gastrointest Endosc 2013;78(2):295-302.
Khalid A, Zahid M, Finkelstein SD, et al. Pancreatic cyst fluid DNA analysis in evaluating pancreatic cysts: a report of the PANDA study. Gastrointest Endosc 2009;69(6):1095-102.
Conflict of Interest
All authors have no conflict of interests to declare and there was no source of funding.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Goh, B.K.P., Tan, D.M.Y., Ho, M.M.F. et al. Utility of the Sendai Consensus Guidelines for Branch-Duct Intraductal Papillary Mucinous Neoplasms: A Systematic Review. J Gastrointest Surg 18, 1350–1357 (2014). https://doi.org/10.1007/s11605-014-2510-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-014-2510-8