Abstract
Background
Surgical procedures in pancreatic surgery are well established, but still involve time-consuming manual dissection. We compared the use of LigaSure with conventional dissection techniques in pancreatic surgery in a prospective randomised single-centre trial (registration number: NCT00850291).
Methods
Patients with tumours of the pancreatic head that were assumed to be technically resectable were randomised to LigaSure or conventional surgery. The primary endpoint of this study was overall operation time. Secondary endpoints were preparation time until tumour resection, intraoperative blood loss, number of given units of packed red blood cells, costs of surgery, postoperative morbidity, length of hospital stay and mortality.
Results
There was no difference in overall operation time between the two groups (P = 0.227). Median costs for pancreatic surgery were significantly less in the conventional group with €3,047 (range 2,004–5,543) vs. €3,527 (range 2,516–5,056, P = 0.009). Preparation time, intraoperative blood loss, number of units of packed red blood cells, postoperative morbidity, length of hospital stay and mortality did not differ between the two groups.
Conclusion
Our data indicate that the LigaSure device is equivalent to conventional dissection modalities in pancreatic surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The classic pancreaticoduodenectomy (PD) and the pylorus-preserving PD (PPPD) are well-established procedures for tumours of the pancreatic head. Both procedures involve time-consuming manual dissection. Appropriate haemostasis during dissection is crucial to avoid intraoperative and postoperative complications.
For vessels up to 2–3 mm in diameter, established methods of electrosurgical and ultrasonic thermal energy application are available.1 For vessels of larger diameter, clips are frequently used. Bearing in mind the risk of dislodgment of clips, manual ligation with sutures is often favoured.
In 1997, Kennedy et al. published a new technique for dissection based on a combination of pressure and bipolar electrical energy.2 Nowadays this technique is well known as the LigaSure™ method (Covidien Energy-based Devices, Boulder, Colorado). It enables the surgeon to seal vessels and tissue up to a diameter of 7 mm with seal integrity comparable to that of suturing and clipping. Furthermore, it offers an organic seal by fusing collagen and elastin within the vessels and tissue bundles, in contrast to electrothermal occlusion, which is attained by dehydration of the tissue and coagulated thrombus within the vessel.3,4 Verification of the seal is easy, as the sealed area is translucent. Additionally, the delivery of a precisely regulated amount of energy reduces to less than 2 mm the lateral thermal spread.2
Since the introduction of the LigaSure device in 1998, the electrothermal bipolar vessel coagulation system (EBVS) has been compared with conventional dissection techniques in a variety of procedures.5–8 The majority of published studies reported a shorter operation time and lower estimated blood loss.
In a small pilot study involving PD procedures we achieved promising results with reductions in operating time and blood loss (unpublished data). We therefore carried out this single-centre prospective, randomised trial of EBVS in pancreatic surgery to assess the impact on operation time and intraoperative blood loss, costs and postoperative morbidity.
Material and Methods
Methodology and findings are reported according to the guidelines of CONSORT (Consolidated Standards of Reporting Trials) guidelines 2010.9 The trial is registered at ClinicalTrials.gov (NCT00850291). High-quality data assessment was ascertained by the clinic’s internal study centre. Informed consent was obtained from all patients before randomisation. This study was approved by the Ethics Committee of the local association of physicians of Hamburg, Germany.
Inclusion Criteria
Patients, who were admitted to our institution with tumours of the pancreatic head between May 2008 and February 2010, were evaluated for inclusion. Written informed consent and age >18 were required for final inclusion and randomisation.
Randomisation
Randomisation was done using an online randomisation tool the day before surgery, with allocation into two groups: either EBVS dissection (group A) or conventional dissection (group B). Patients were blinded to the mode of dissection. The randomisation result was communicated to the surgeon and the assisting team on the day of surgery.
Exclusion Criteria
Additional resections except distal stomach, duodenum, first jejunal loop, gallbladder, and distal bile duct as well as spleen in case of a total pancreatectomy were defined as multivisceral resections and led to exclusion from statistical analysis. This applied also any sort of vascular resection including portal vein or palliation.
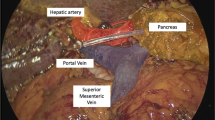
Operative Technique
As centre for pancreatic surgery (>250 procedures/year), the surgical technique is standardised at a high level. Surgeons involved were highly experienced in pancreatic surgery and confirmed sound expertise with use of LigaSure device prior to this trial.
Surgeons were instructed to use the LigaSure device (LigaSure V 5 mm, Open 20 cm; LS1520) instead of electrocautery, clipping or suturing from the time of skin incision until end of tumour resection (except bowel transsection) for patients randomised to group A. The following key preparation steps were obligatory in order to include a patient in the final analysis: Kocher manoeuvre of the duodenum, entering the lesser sac, mobilisation of the proximal jejunum, transsection of the omentum and of the retropancreatic tissue. The resection techniques were the same for benign and malignant diseases including patients with preoperatively unknown histology. Lymphadenectomy was performed along hepatoduodenal ligament, portal vein, right celiac trunk and the right hemicircumference of the superior mesenteric artery. Dissection of the superior mesenteric artery was carried out using suture ties in group B. In case of clearly benign disease lymphadenectomy was not performed. The gastroduodenal artery was suture-ligated primarily. Pancreatic dissection was done by scalpel in order to preserve the main pancreatic duct. All surgeons were asked to confirm sufficient usage of the LigaSure device in the operation report. Reconstruction was done in a standardised fashion.
Follow-up
All patients were visited daily until discharge from hospital. Data required for study endpoints were recorded prospectively in a web-based electronic case report file. For patients who met the exclusion criteria, only the cause of exclusion was recorded.
Study Endpoints
The primary endpoint was the overall operation time, measured from the start of skin incision until complete skin closure. Secondary endpoints were time from the start of skin incision until end of tumour resection, intraoperative blood loss, number of given packed red blood cell (PRBC), costs of surgery and postoperative outcome.
The intraoperative blood loss was calculated by subtracting the volume of fluid used for irrigation and the starting weight of applied gauzes from the suction volume and weight of used gauzes, and for corroboration we recorded the number of packed red blood cell units given within 24 h after skin incision. An absolute indication for PRBC transfusion was an Hb below 7 g/dl. A relative indication for transfusion was an Hb below 10 g/dl. Analysis of costs was based on €11.49/min for group A and €10.66/min for group B (€2.80/min for operation room and personnel, €1.25/min for surgeons (n = 3), €3.28/min for anaesthesia personnel, €4.16/min material costs in group A and €3.33/min in group B). All adverse events within the hospital stay were graded according to the Clavien-Dindo classification.10,11 Pancreatic fistulas and postoperative haemorrhage were additionally graded according to the recommendations of the International Study Group of Pancreatic Surgery.12,13
In summary, the collected data included age, date of procedure, procedure performed, estimated blood loss, operation time, time until end of tumour resection, location and type of disease, final pathological diagnosis, TNM classification, UICC stage, length of hospital stay, morbidity and mortality including Clavien-Dindo classification.
Statistical Analysis
The power calculation was based on personal experience in a small pilot study. Based on an average operation time of 360 min and a postulated time saving of 60 min, with a power of 90 %, a calculated group size of at least 43 was necessary. Calculations were based on a power value of 1–β = 0.9 and an α error of 0.05. Comparison of categorical patient characteristics was performed using the chi-square test. Data were reported as median and range (unless indicated otherwise) and differences were analysed with the Mann–Whitney U test. Differences with significance values of P < 0.05 two-sided were considered significant.
Results
Randomisation Results and Study Population
A total of 136 patients who were admitted to our institution with tumours of the pancreatic head between May 2008 and February 2010 were included in this study. Sixty-five patients were randomised into group A and 71 patients were randomised into group B. None of the patients received a neoadjuvant treatment.
A classic Whipple procedure was done in 70 cases: in 35 patients in the LigaSure group and in 35 patients in the conventional dissection group. A pylorus-preserving Whipple procedure was performed in 15 patients (LigaSure n = 5; conventional dissection n = 10). In four cases total pancreatectomy was necessary to achieve an appropriate surgical result (LigaSure n = 3; conventional n = 1, Table 2). In group A 22 patients were excluded because of meeting exclusion criteria (palliation, n = 10; vascular resection, n = 7; multivisceral resection, n = 5). In group B 25 patients were excluded (palliation, n = 13; vascular resection, n = 9; multivisceral resection, n = 3, Fig. 1).
The final analysed study population consisted of 43 patients in group A and 46 patients in group B. There was no significant difference between the two groups concerning median age or gender (Table 1). Among the 89 patients in both groups, 57 had malignant disease and 32 had benign disease. In the LigaSure group, the final pathological diagnoses were of 26 adenocarcinomas located at the pancreatic head, the papilla or the duodenum and three malignant neuroendocrine pancreatic tumours. In the group with conventional dissection there were 25 adenocarcinomas and three cholangiocellular malignant tumours. Comparison of TNM classifications between the two groups showed no significant difference (Table 1).
Study Endpoints: Surgical Outcome
Operative findings, such as performed procedure, median surgical time, time until end of tumour resection, blood loss and blood transfusion requirement, number of retrieved lymphnodes, resection margins and costs of surgery were compared for the two groups (Table 2). We were not able to demonstrate significant differences related to the defined primary endpoint of total operation time or in operative time taken to achieve tumour resection (P = 0.227 and P = 0.619). The median surgical time was 307 min (219–440) in the LigaSure group and 288 min (188–520) in the conventional dissection group. The median time to achieve tumour resection was 167 min (102–360) in group A and 165 (188–520) in group B. Results affected the cost analysis with median costs of €3,527 (2,516–5,056) in group A vs. €3,065 (2,004–5,543) in group B (only operation costs, P = 0.009).
The LigaSure group showed a lower median blood loss in comparison with the conventional dissection group but this did not reach significance (450.00 ml, range 100–1,300 vs. 525 ml, range 200–2,600; P = 0.357). The number of given PRBC units was equal in both groups, P = 0.507. Analysis of number of lymphnodes retrieved and non-R0 resections did not show significant differences between the two groups (P = 0.215 and P = 0.434). In the conventional dissection group a severe haemorrhage due to perforation of the vena cava that required a vascular graft was recorded. No adverse event that was related to the LigaSure device was recorded; this applied also to postoperative morbidity and mortality events in group A.
Study Endpoints: Postoperative Outcome
The postoperative complications were classified according to the Clavien-Dindo classification. The overall complication rate was 67.8 % (n = 30) in group A and 58.7 % (n = 27) in group B (P = 0.277). Thirty-five patients in group A (81.4 %) and 36 patients in group B (78.3 %) developed no complications or complications which did not require any intervention under general anaesthesia (≤Grade IIIa). Eight patients (18.6 %) in group A and ten patients (21.7 %) in group B developed complications from grade IIIb to V (Table 3). Mortality due to surgical reasons was 4.7 % in group A (n = 2) and 6.5 % (n = 3) in group B. Statistical analysis did not show any significant differences related to the severity grades of postoperative complications (P = 0.527; Table 3). Analysis comparing major complication rates based on a cut off between ≤Grade IIIa and ≥Grade IIIb did not reveal a difference between the two groups likewise (n = 8, 18.6 % vs. n = 10, 21.7 %, P = 0.713). Neither the pancreatic fistula rate nor the fistula grades indicated a difference between the two groups. This applies also to the occurrence of chylous fistulas, haemorrhage and necessity of relaparotomy due to postoperative haemorrhage (grade ≥B, predominant late onset, Table 3). The median postoperative stay was 17 days (8–104) in group A and 19 days (9–65) in group B (P = 0.266).
Discussion
Since its commercial launch, the LigaSure device has been increasingly used in a variety of surgical procedures, with mixed results. The majority of retrospective case-control studies have reported shorter operation times and/or lower blood loss with the use of the LigaSure device (e.g. radical prostatectomy, cystectomy and pelvic exenterations).14,15
To date, one case report and a pilot study with 14 patients have compared the LigaSure device with conventional modalities in pancreatic surgery. Both reported reductions in operation time and in blood loss.16,17
This is the first prospective randomised trial comparing the use of the LigaSure technique with conventional haemostatic and dissection methods in pancreatic surgery. Contrary to our expectations, which were based on an unpublished small pilot study, we were not able to show significant differences with regard to operation time or time until end of tumour resection or other secondary endpoints in our trial. Accordingly, cost analysis revealed significant higher costs of surgery by using the LigaSure device instead of conventional dissection methods (P = 0.009, Table 2). The results of cost analysis are not surprising, bearing in mind, that the overall operation time as well as the time until end of tumour resection was comparable in both groups and that the LigaSure device is a disposable article which is an additional and crucial matter of expense for each surgery in the LigaSure group.
Randomised prospective studies comparing the LigaSure dissection with conventional techniques in abdominal surgery are rare but the results are comparable to ours. A pilot trial comparing LigaSure with conventional suture ligation for abdominal hysterectomy did not show any significant advantages with the LigaSure technique.18 Another multicentre randomised trial of LigaSure vs. conventional surgery in colorectal cancer and gastric cancer, with 174 patients, showed a significantly shorter operating time and less blood loss only in a subgroup of the study population.19 Merely one randomised trial with 40 patients in each group reported a shorter operating time and decreased blood loss in the LigaSure group; this trial involved extended gastric cancer resection.20
Even though reported results are in accordance to the results of preceding randomised studies evaluating the LigaSure device in abdominal surgery, our study design included some weak points, which needs to be discussed: the time from skin incision to the end of tumour resection was a secondary endpoint, but it could equally have been chosen as the primary endpoint, especially as the device was used only in this part of the operation. However, even if the preparation phase had been taken as the primary endpoint, it would not have changed the final results, as shown in our “Results” section.
The ligasure group had a higher proportion of classic pancreaticoduodenectomies and total pancreatectomies, which take slightly longer than pylorus-preserving pancreatectomies. While this difference did not achieve statistical significance it could have influenced the primary endpoint. But conversely, the lack of pancreatic reconstruction in the total pancreatectomy patients may have had the opposite effect.
Based on the organic sealing by fusing collagen and elastin within the vessels and tissue bundles and the reduced lateral thermal spread by application of the LigaSure device a difference in postoperative morbidity rates was to be expected but the overall morbidity and mortality rates according to the Clavien-Dindo classification did not reveal significant differences. Detailed evaluation of postoperative outcome (fistula rates and grades, postoperative haemorrhage) was performed. Results were in accordance to the Clavien-Dindo classification. Although we provided P of subgroup analysis and detailed evaluation of postoperative outcome (fistula rates and grades, postoperative haemorrhage) in addition to the Clavien-Dindo score, our study cohort might have been too small to achieve significant differences concerning these secondary endpoints.
Even though the surgical mortality rate was 5.6 %, the overall mortality rate was higher than expected in this trial. Our mortality rate between 1994 and 2010 after major pancreatic resections was constantly between 4 and 5 %.21–23 In contrast to our former studies the present mortality rate was based on all events that occurred until discharge. Mortality rates published before are mainly based on 30-day mortality rates leading to a potential underreporting of actual mortality rates. However, even if we exclude patients suffering from death after 30 days our rate is still unexpectedly high. In spite of repeated analysis of possible influencing clinical characteristics, we were not able to explain this fact. Hence, we have to consider it as a coincidence due to the limited study cohort size.
Conclusion
Randomised trials of surgical procedures often generate unexpected results. In summary the expected advantages of the LigaSure system were not proven. Based on our results, and considering that this is the first prospective, randomised trial dealing with the LigaSure technique in pancreatic surgery, we have to conclude that the LigaSure method is equal to conventional techniques, but does not offer any significant advantage, despite additional costs.
References
Harold KL, Pollinger H, Matthews BD, Kercher KW, Sing RF, Heniford BT. Comparison of ultrasonic energy, bipolar thermal energy, and vascular clips for the hemostasis of small-, medium-, and large-sized arteries. Surg Endosc 2003; 17: 1228–1230.
Kennedy JS, Stranahan PL, Taylor KD, Chandler JG. High-burst-strength, feedback-controlled bipolar vessel sealing. Surg Endosc 1998; 12: 876–878.
Amaral JF. Ultrasonic dissection. Endosc Surg Allied Technol 1994; 2: 181–185.
Sigel B, Dunn MR. The mechanism of blood vessel closure by high frequency electrocoagulation. Surg Gynecol Obstet 1965; 121: 823–831.
Cipolla C, Graceffa G, Sandonato L, Fricano S, Vieni S, Latteri MA. LigaSure in total thyroidectomy. Surg Today 2008; 38: 495–498.
Eroglu A, Turkyilmaz A, Aydin Y, Erdem AF, Tokur M, Karaoglanoglu N. The use of the LigaSure Vessel Sealing System in esophageal cancer surgery. Ann Thorac Surg 2007; 84: 2076–2079.
Nienhuijs S, de Hingh I. Conventional versus LigaSure hemorrhoidectomy for patients with symptomatic Hemorrhoids. Cochrane Database Syst Rev 2009; CD006761.
Saiura A, Yamamoto J, Koga R, Sakamoto Y, Kokudo N, Seki M, Yamaguchi T, Yamaguchi T, Muto T, Makuuchi M. Usefulness of LigaSure for liver resection: analysis by randomized clinical trial. Am J Surg 2006; 192: 41–45.
Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med 2010; 7: e1000251.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, de Santibanes E, Pekolj J, Slankamenac K, Bassi C, Graf R, Vonlanthen R, Padbury R, Cameron JL, Makuuchi M. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250: 187–196.
Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213.
Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005; 138: 8–13.
Wente MN, Veit JA, Bassi C, Dervenis C, Fingerhut A, Gouma DJ, Izbicki JR, Neoptolemos JP, Padbury RT, Sarr MG, Yeo CJ, Buchler MW. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007; 142: 20–25.
Bansal N, Roberts WS, Apte SM, Lancaster JM, Wenham RM. Electrothermal bipolar coagulation decreases the rate of red blood cell transfusions for pelvic exenterations. J Surg Oncol 2009; 100: 511–514.
Daskalopoulos G, Karyotis I, Heretis I, Delakas D. Electrothermal bipolar coagulation for radical prostatectomies and cystectomies: a preliminary case-controlled study. Int Urol Nephrol 2004; 36: 181–185.
Belli G, Fantini C, Ciciliano F, D'Agostino A, Barberio M. Pancreaticoduodenectomy in portal hypertension: use of the Ligasure. J Hepatobiliary Pancreat Surg 2003; 10: 215–217.
Gehrig T, Muller-Stich BP, Kenngott H, Fischer L, Mehrabi A, Buchler MW, Gutt CN. LigaSure versus conventional dissection technique in pancreatoduodenectomy: a pilot study. Am J Surg 2011; 201: 166–170.
Hagen B, Eriksson N, Sundset M. Randomised controlled trial of LigaSure versus conventional suture ligature for abdominal hysterectomy. BJOG 2005; 112: 968–970.
Takiguchi N, Nagata M, Soda H, Nomura Y, Takayama W, Yasutomi J, Tohyama Y, Ryu M. Multicenter randomized comparison of LigaSure versus conventional surgery for gastrointestinal carcinoma. Surg Today 2010; 40: 1050–1054.
Lee WJ, Chen TC, Lai IR, Wang W, Huang MT. Randomized clinical trial of Ligasure versus conventional surgery for extended gastric cancer resection. Br J Surg 2003; 90: 1493–1496.
Bockhorn M, Burdelski C, Bogoevski D, Sgourakis G, Yekebas EF, Izbicki JR. Arterial en bloc resection for pancreatic carcinoma. Br J Surg 2011; 98: 86–92.
Bockhorn M, Cataldegirmen G, Kutup A, Marx A, Burdelski C, Vashist JK, Mann O, Liebl L, Konig A, Izbicki JR, Yekebas EF. Crossing the Rubicon: when pancreatic resection with curative intent ends in an R2 status. Impact of "desmoplastic pseudo-pancreatitis" and anatomical site of irresectability. Ann Surg Oncol 2009; 16: 1212–1221.
Yekebas EF, Bogoevski D, Cataldegirmen G, Kunze C, Marx A, Vashist YK, Schurr PG, Liebl L, Thieltges S, Gawad KA, Schneider C, Izbicki JR. En bloc vascular resection for locally advanced pancreatic malignancies infiltrating major blood vessels: perioperative outcome and long-term survival in 136 patients. Ann Surg 2008; 247: 300–309.
Author information
Authors and Affiliations
Corresponding author
Additional information
Financial support was obtained from Covidien Germany, Gewerbepark 1, 93333 Neustadt/Donau, Germany.
Faik Guentac Uzunoglu and Maximilian Bockhorn contributed equally to this work.
Rights and permissions
About this article
Cite this article
Uzunoglu, F.G., Bockhorn, M., Fink, J.A. et al. LigaSure™ Vs. Conventional Dissection Techniques in Pancreatic Surgery—a Prospective Randomised Single-Centre Trial. J Gastrointest Surg 17, 494–500 (2013). https://doi.org/10.1007/s11605-012-2107-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-2107-z