Abstract
Background
Current diagnostic techniques establishing gastroesophageal reflux disease as the underlying cause in patients with respiratory symptoms are poor. Our aim was to provide additional support to our prior studies suggesting that the association between reflux events and oxygen desaturations may be a useful discriminatory test in patients presenting with primary respiratory symptoms suspected of having gastroesophageal reflux as the etiology.
Methods
Thirty-seven patients with respiratory symptoms, 26 with typical symptoms, and 40 control subjects underwent simultaneous 24-h impedance–pH and pulse oximetry monitoring. Eight patients returned for post-fundoplication studies.
Results
The median number (interquartile range) of distal reflux events associated with oxygen desaturation was greater in patients with respiratory symptoms (17 (9–23)) than those with typical symptoms (7 (4–11, p < 0.001)) or control subjects (3 (2–6, p < 0.001)). A similar relationship was found for the number of proximal reflux-associated desaturations. Repeat study in seven post-fundoplication patients showed marked improvement, with reflux-associated desaturations approaching those of control subjects in five patients; 20 (9–20) distal preoperative versus 3 (0–5, p = 0.06) postoperative; similar results were identified proximally.
Conclusions
These data provide further proof that reflux-associated oxygen desaturations may discriminate patients presenting with primary respiratory symptoms as being due to reflux and may respond to antireflux surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Up to 40 % of adults in the USA report experiencing symptoms of gastroesophageal reflux disease (GERD) on a monthly basis.1–4 Although the majority of patients complain of heartburn and/or regurgitation, many have reflux-related respiratory symptoms either in combination or alone.1,5 Abnormal esophageal acid exposure has been identified in up to 40 % of patients with chronic cough, as many as 75 % of patients with chronic hoarseness, and in up to 90 % of adults with asthma.1–3,6 Current diagnostic techniques aimed at establishing GERD as the underlying cause of respiratory symptoms are poor. Ambulatory esophageal pH monitoring, considered the gold standard for detecting reflux, suffers from lack of sensitivity in patients with extraesophageal symptoms and can be nonspecific. A trial of proton pump inhibitors, often utilized as an adjunct to GERD diagnosis, has been shown to be unreliable in relieving reflux-related airway symptoms.1–4,6
We have previously reported preliminary studies suggesting that the measurement of oxygen (O2) desaturations occurring in association with reflux events may be useful to discriminate reflux-related respiratory symptoms. These studies showed that nearly three quarters of GERD patients with predominant respiratory symptoms had O2 desaturations associated with esophageal acid exposure, compared with less than one third of those with predominant typical reflux symptoms.7 Corroborating these studies, others have previously reported O2 desaturation occurring in association with episodes of gastroesophageal reflux in 40 % of patients with GERD.4,8
The long-term efficacy of antireflux surgery for extraesophageal symptoms is not as good as when surgery is performed for heartburn or regurgitation.1,2,5,6 This fact is likely due to the difficulty in establishing reflux as the cause of the patient’s respiratory symptoms, emphasizing the need for better diagnostic methods. The aim of this study was to further refine the proof of principle that measurement of reflux-associated O2 desaturations (RADs) may be a useful discriminatory test for respiratory symptoms thought secondary to GERD. The usefulness of RADs was assessed by comparing their prevalence in patients with respiratory symptoms thought secondary to GERD to individuals with primary gastrointestinal (GI) complaints from GERD and to normal subjects, as well as by assessing the impact of antireflux surgery on RADs.
Patients and Methods
Study Population
The study population consisted of 63 patients with pathological GERD undergoing foregut diagnostic evaluation between January, 2007 and April, 2012 at the University of Rochester Esophageal Diagnostic Laboratory. The presence and severity of GERD symptoms were assessed at the initial visit including typical symptoms of heartburn, regurgitation, and dysphagia and respiratory symptoms of cough, hoarseness, and throat clearing. Control subjects completed a self-administered questionnaire to assess the presence of typical and atypical esophageal symptoms; a symptom score of 0 (asymptomatic) was required for inclusion. Thirty-seven of these patients reported a primary respiratory symptom. The primary complaint in the remaining 26 patients in the study population was a GI symptom. Fifty-two volunteers, who had neither GI symptoms nor prior GI surgery, were recruited as control subjects. Due to either elevated distal or proximal multichannel intraluminal impedance (MII)–pH scores, 12 volunteers were considered to have GERD and were excluded from the analysis, thus 40 subjects served as controls.
Eight of the 63 patients treated with antireflux surgery returned for post-Nissen fundoplication studies. A standardized symptom questionnaire was administered identifying the presence and severity of both pre- and postoperative typical and atypical reflux symptoms graded by frequency on a Likert scale (0–5, 5 = daily/with every meal).
Manometric Technique and Parameters
High-resolution manometry (HRM) was performed using a solid-state manometric assembly (Given Imaging, Duluth, GA). The catheter included 36 circumferential sensors spaced at 1 cm intervals with an outer diameter of 4.2 mm. Pressure transducers were calibrated at 0 and 100 mmHg using externally applied pressure prior to initiation of the study. Manometric studies were performed in the supine position after a minimum 6-h fast. Subjects underwent transnasal placement of the catheter, positioned to record from the pharynx to the stomach with the catheter secured to the subject’s nose by tape. The manometric protocol included at least a 30-s period of baseline recording followed by ten consecutive 5 ml water swallows. The HRM plots of individual successful swallows were subsequently analyzed with reference to the updated Chicago classification criteria for esophageal motility disorders.9
Ambulatory MII–pH Monitoring Technique and Parameters
Ambulatory 24-h MII–pH monitoring was performed using a dual pH probe catheter with six impedance sensors. The pH sensors were spaced 15 cm apart, at 5 and 20 cm from the distal tip of the catheter, along with impedance sensors located at 2 cm increments (3, 5, 7, 9, 15, and 17 cm from the distal tip). In 15 of the symptomatic patients, a similar catheter was utilized; however, the proximal pH sensor at 20 cm from the distal tip was absent.
After the MII–pH catheter was calibrated and passed transnasally, the distal pH sensor was placed 5 cm above the manometrically determined proximal border of the gastroesophageal junction (GEJ). The patient was then instructed on the appropriate diet and directed to keep a diary of the time and nature of meals, recumbency periods, and symptoms experienced. A portable digital data logger (Sandhill Scientific, Highlands Ranch, CO) was used to record MII–pH fluctuations. All data were downloaded and analyzed utilizing dedicated software (Sleuth, Sandhill Scientific, Highlands Ranch, CO).
Acid reflux episodes were defined as pH of <4 5 cm (distal) or 20 cm (proximal) above the GEJ and nonacid reflux episodes as a drop in impedance at ≥50 % from baseline 3, 5, 7, or 9 cm above the GEJ (distal) and 15 or 17 cm above the GEJ (proximal). Abnormal acid exposure was defined as a pH of <4 more than 4.5 % of the total time in the distal channel, more than 0.9 % of the total time in the proximal channel, or a distal DeMeester composite score of >14.7.10,11 Abnormal bolus exposure was defined as a total number of distal reflux episodes > 73, acid reflux episodes > 55, and nonacid reflux episodes > 48. Proximal total reflux episodes were defined as abnormal if >31, and proximal acid reflux episodes of >28.12 A value of 12 was used for the threshold of proximal nonacid reflux episodes, derived from the 95th percentile in 53 asymptomatic volunteers at our institution.
Ambulatory Pulse Oximetry Monitoring Technique and Parameters
Concomitant O2 saturation monitoring was performed using the Pulsox-300i (Konica Minolta Sensing, Inc.) and Finger Clip Probe SR-5C (Konica Minolta).7 Data were acquired and analyzed using Profox Oximetry Software (Profox Associates, Inc., Escondido, CA). The Pulsox-300i was secured to the wrist and the probe placed on the index finger in all patients. A glove was placed over the hand and device to minimize movement of the probe in relation to the finger and prevent artifactual data. The timing of the pulse oximetry was synchronized with the MII–pH monitoring at the onset of the study period. Oxygen desaturation events were defined as a drop in O2 saturation to <90 %, or a decrease of ≥6 % from baseline. A RAD was defined as the first O2 desaturation occurring during or within a 5-min interval following a reflux episode.
Statistical Analysis
Descriptive statistics (median, 5th percentiles, and 95th percentiles) were used in control subjects to describe reflux and desaturation findings as they had a nonparametric distribution. In symptomatic patients, data were described as median (interquartile range). Data between groups were compared using the chi-square test for categorical data, while continuous data not normally distributed were compared using Mann–Whitney U and Kruskal–Wallis tests. A p value of <0.05 was considered significant. All statistical analyses were performed using the SPSS 20.0 statistical software package (SPSS Inc., Chicago, IL).
The study protocol was approved by the University of Rochester Medical Center Research Subjects Review Board and all participants gave written informed consent. Data were taken from a prospectively maintained database, which included demographic and clinical information from dictated notes, as well as operative, manometry, pH, radiology, and endoscopy reports. Data were extracted and recorded in a Microsoft Excel® database (Microsoft Corp., Redmond, WA) and analyzed.
Results
The demographics of the three study populations are shown in Table 1. Control subjects were younger than symptomatic patients, and those with predominant GI symptoms had the highest mean BMI. The most prominent symptom in the 37 patients with a primary respiratory complaint was cough occurring in 28 patients (75.7 %), hoarseness in 7 (18.9 %), and throat clearing in 2 (5.4 %). The majority of the respiratory patients (32/37, 86.5 %) also reported some degree of heartburn and/or regurgitation. The most prominent symptom in the 26 patients with primary GI complaints was heartburn occurring in 13 patients (50.0 %), regurgitation in 8 (30.8 %), globus sensation in 2 (7.7 %), epigastric pain in 2 (7.7 %), and dysphagia in 1 (3.8 %). Secondary symptoms of cough, hoarseness and/or aspiration were present in 19 (73.1 %) of the GI cohort. Select clinical features of the two symptomatic cohorts are shown in Table 2. The prevalence of mucosal and anatomical abnormalities was similar in both groups.
Ambulatory MII–pH Findings
Based upon distal esophageal pH and/or impedance monitoring, abnormal MII–pH studies were present in none of the control patients, 100.0 % (26/26) of the GI patients and 91.9 % (34/37) of the respiratory patients. Three (8.1 %) of the respiratory patients had abnormal proximal MII–pH studies, but normal distal MII–pH studies. Table 3 shows MII–pH data in each of the three study groups. Control subjects had a median of 32 (21–41) distal reflux episodes in 24-h, patients with typical symptoms a median of 66 (47–107, p < 0.001), and those with respiratory symptoms a median of 56 (40–70, p < 0.001). Slightly over half of the reflux events were detected proximally in both groups (1,063/1,880, 57 % GI; 1,127/2,101, 54 % respiratory). There was a significantly higher prevalence of respiratory patients (74 %, 26/35) with abnormally high reflux detected by the proximal pH sensor compared with GI patients (39 %, 5/13; p = 0.039). The number of proximal reflux events in both groups was considerably greater than control subjects (p < 0.001).
Desaturation Findings
The median number of total O2 desaturations in 24-h was comparable between control subjects (50 (27–65)) and GI patients (54 (22–117)); however, it was nearly three times higher in patients with primary respiratory symptoms (145 (88–212, p < 0.001)) (Fig. 1). Oxygen desaturation and RADs parameters derived from the 40 control subjects are shown in Table 4. Using these values, the upper limit of “normal” for total number of O2 desaturation in 24-h was defined as the 95th percentile (93 episodes). The cohort with primary respiratory symptoms had the highest prevalence of individuals with an elevated number of O2 desaturations (70 %) compared with 31 % in the GI group (p = 0.002) and, by definition, 5 % of control subjects (p < 0.001).
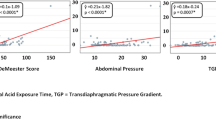
The median number of distal reflux events associated with O2 desaturation was significantly greater in patients with respiratory symptoms (17 (9–23)) than in those with GI symptoms (7 (4–11, p < 0.001)) or control subjects (3 (2–6, p < 0.001)) (Fig. 2; Table 5). Using a 95th percentile threshold of 11 derived from the control subjects, 70 % of patients with primary respiratory symptoms had an abnormally high median number of distal RADs, compared with 27 % (p = 0.001) of patients with GI symptoms and 8 % (p < 0.001) of control subjects.
A similar pattern was seen for the median number of proximal RADs: eight (5–14) in patients with respiratory symptoms versus three (1–6, p < 0.001) with GI symptoms and one (0–3, p < 0.001) in control subjects (Fig. 3). Using a 95th percentile threshold of seven, 62 % of patients with primary respiratory symptoms had elevated proximal RADs, compared with 19 % (p = 0.001) of patients with primary GI symptoms and 10 % (p < 0.001) of control subjects.
As can be seen in Tables 3 and 5, acid reflux was more prevalent than nonacid reflux in all groups and there was a stronger association between acid reflux and O2 desaturations than between nonacid reflux. Patients with primary respiratory symptoms had significantly higher numbers of acid (14 (6–21)) and nonacid (2 (1–3)) RADs when compared with GI patients (acid, 5 (1–10, p < 0.001) and nonacid, 1 (0–3, p = 0.016) RADs) and control subjects (acid, 2 (1–5, p < 0.001) and nonacid, 1 (0–2, p = 0.004) RADs). Similarly, upright (14 (8–20)) and supine (1 (0–2)) RADs were higher in respiratory patients when compared with GI patients (upright, 5 (3–10, p < 0.001) and supine, 0 (0–1, p = 0.271) RADs) and control subjects (upright, 3 (2–6, p < 0.001) and supine, 0 (p < 0.001) RADs).
Postoperative Findings
Twenty-seven of the 63 symptomatic patients underwent antireflux surgery; 12 (46 %) patients with primary GI and 15 (41 %) with primary respiratory symptoms. Seven of the 27 (three from the respiratory cohort and four from the GI cohort) had postoperative MII–pH/O2 saturation studies. Six were female (85.7 %) and one male (14.3 %), with a mean age of 61 years (range, 43–69). Median scores for the primary respiratory symptom in the three patients improved following antireflux surgery (four preoperatively versus two postoperatively; p = 0.369) at a mean follow-up of 38 months. With the exception of two patients with primary GI symptoms and documented recurrent reflux, all patients had marked improvement in the median number of total O2 desaturations (242 preoperatively versus 93 postoperatively, p = 0.032), as well as the median number of distal RADs at an average of 29 months following Nissen fundoplication (20 preoperatively versus 3 postoperatively, p = 0.058) (Figs. 4 and 5). Improvement was similar in proximal RADs (12 preoperatively versus 1 postoperatively, p = 0.090) (Fig. 6; Table 6). Excluding the two patients with recurrent reflux, postoperative values for RADs approached those of control subjects and none of the patients had an abnormal number of distal RADs following surgery. Symptom improvement correlated with a decrease in median RAD number in two of the three respiratory patients; however, one patient did not have sustained improvement in symptomatology.
Discussion
These data validate our previous report of the correlation between O2 desaturation and reflux episodes in patients with atypical symptoms possibly due to GERD.7 We have established normal reference thresholds derived from asymptomatic control subjects without GERD, which are of course key to the interpretation of results in symptomatic patients. We have further confirmed that patients with primary “reflux-related” respiratory symptoms have a significantly higher prevalence of both distal and proximal RADs compared with patients with primary typical (GI) symptoms. In fact, RAD events and data in the GI symptom group were similar to those of control subjects. Perhaps most importantly, successful antireflux surgery decreased the number of RADs to values comparable to normal control subjects, a powerful “proof of principle” finding.
Respiratory symptoms have long been recognized to be associated with gastroesophageal reflux.1,5 A large body of literature exists reporting the prevalence of pathological GERD in these patients, ranging from 10 % in those with a chronic cough, to 90 % of adults with asthma.2,3,6 To date, no test proving a cause and effect relationship has been established, although several techniques have been investigated. Most data would suggest that in patients with primary typical symptoms and demonstrable GERD, secondary respiratory symptoms have a higher probability of improving following antireflux surgery than in patients with isolated respiratory symptoms, although confirming a reflux-related cause is challenging in any patient with respiratory symptoms.
Ambulatory 24-h esophageal pH monitoring has proven a useful tool to detect pathologic gastroesophageal reflux; however, it can be normal in patients with reflux-related extraesophageal symptoms and does not provide cause and effect data.2,4,6 A positive test confirms the presence of pathological reflux but gives little to no data on the relationship of reflux to symptoms. Ambulatory pH and multichannel impedance monitoring combined with a symptom diary has been used in an attempt to establish a temporal relationship between symptoms and reflux episodes via a variety of symptom indices, but calculation of these indices has not proven to be reliable particularly for atypical symptoms.2 Some extraesophageal symptoms with a readily definable onset, such as cough, might reasonably be correlated to reflux events. Others with a less definable onset, such as sore throat, hoarseness, or globus sensation, do not lend themselves to such temporal correlations. Other investigations, including upper endoscopy, lack sensitivity, while laryngoscopy has been shown to have poor specificity.3
Empiric therapy with proton pump inhibitors (PPIs) is the initial therapeutic step in patients suspected of having any GERD-related symptoms. It is widely thought that respiratory symptoms may take longer to respond to antisecretory medications than typical heartburn or regurgitation, although few data support this contention. Patients are most commonly treated with twice daily PPI therapy for 3–6 months with an assessment of the responsiveness of atypical complaints. Improvement on such therapy, although uncommon, suggests a causal relationship. The unresponsive majority are often referred for MII/pH testing on therapy to confirm acid suppression, detect abnormal nonacid reflux, and determine the relationship to symptoms via calculation of symptom indices.1,3 While this approach is far from perfect, has little data validating its usefulness, and is problematic for many atypical symptoms as mentioned above, it has been reported that patients with cough and a positive symptom index respond well to antireflux surgery.13
Antireflux surgery has been shown to provide excellent long-term relief of typical symptoms, ranging from 80 to 90 % at follow-up intervals of 10-years. Outcomes in patients with reflux-suspected airway symptoms, however, are less good with an average of 65–75 % of patients reporting some improvement.1 This finding is likely due to diagnostic uncertainty, emphasizing the need for a test to predict a cause and effect relationship. The marked reduction in RADs to normal limits in our six patients following antireflux surgery, and coincidentally no improvement in the two patients with proven recurrent reflux, reinforces the possibility that RAD measurement may indeed be a useful discriminatory test.
Others have similarly explored the correlation between reflux and O2 saturation. Casanova and colleagues reported 24-h simultaneous oximetry and pH monitoring in 15 patients with COPD and pH proven GERD. Oxygen desaturation was correlated with episodes of increased esophageal acidity in 40 % of patients.4 Wenzl et al. studied 22 infants with recurrent regurgitation or respiratory problems with simultaneous MII–pH and polygraphy. Twenty-one of the 22 infants had reflux-related O2 desaturation. One-hundred twenty-eight episodes of gastroesophageal reflux (from a total of 329 episodes) were associated with breathing irregularities and accompanied by O2 saturation of <90 %.8 Our preliminary report quantifying this association identified a remarkably high prevalence (75 %) of O2 desaturations associated with gastroesophageal reflux in patients with respiratory symptoms7; the current study replicates these results. Of note, any O2 desaturation event within an arbitrarily threshold of 10-min following a reflux episode was used in our preliminary report. We have subsequently performed statistical ROC analysis identifying a 4- to 5-min window as the most accurate threshold and, as a result, used this time frame for the current study.
Limitations of our data include the considerably younger age of control subjects compared with the symptomatic populations, as well as the relatively low number of postoperative patients.
Conclusions
These data provide further proof of principle that measurement of the association between reflux events and O2 desaturation may be a useful discriminatory test in GERD patients presenting with primary respiratory symptoms, and may improve following antireflux surgery.
References
Kaufman JA, Houghland JE, Quiroga E, Cahill M, Pellegrini CA, Oelschlager BK. Long-term outcomes of laparoscopic antireflux surgery for gastroesophageal reflux disease (GERD)-related airway disorder. Surg Endosc 2006;20(12):1824–30.
Gurski RR, da Rosa AR, do Valle E, de Borba MA, Valiati AA. Extraesophageal manifestations of gastroesophageal reflux disease. J Bras Pneumol 2006;32(2):150–60.
Farrokhi F, Vaezi MF. Extra-esophageal manifestations of gastroesophageal reflux. Oral Dis 2007;13(4):349–59.
Casanova C, Baudet JS, del Valle Velasco M, Martin JM, Aguirre-Jaime A, de Torres JP, Celli BR. Increased gastro-oesophageal reflux disease in patients with severe COPD. Eur Respir J 2004;23(6):841–5.
Johnson WE, Hagen JA, DeMeester TR, Kauer WK, Ritter MP, Peters JH, Bremner CG. Outcome of respiratory symptoms after antireflux surgery on patients with gastroesophageal reflux disease. Arch Surg 1996;131(5):489–92.
DeVault KR. Extraesophageal symptoms of GERD. Cleve Clin J Med 2003;70(5):20–32.
Salvador R, Watson TJ, Herbella F, Dubecz A, Polomsky M, Jones CE, Raymond DR, Peters JH. Association of gastroesophageal reflux and O2 desaturation: a novel study of simultaneous 24-h MII-pH and continuous pulse oximetry. J Gastrointest Surg 2009;13(5):854–61.
Wenzl TG, Silny J, Schenke S, Peschgens T, Heimann G, Skopnik H. Gastroesophageal reflux and respiratory phenomena in infants: status of the intraluminal impedance technique. J Pediatr Gastroenterol Nutr 1999;28(4):423–8.
Bredenoord AJ, Fox M, Kahrilas PJ, Pandolfino JE, Schwizer W, Smout AJ, International High Resolution Manometry Working Group. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil 2012;24(1):57–65.
Dobhan R, Castell DO. Normal and abnormal proximal esophageal acid exposure: results of ambulatory dual-probe pH monitoring. Am J Gastroenterol 1993;88(1):25–9.
Jamieson JR, Stein HJ, DeMeester TR, Bonavina L, Schwizer W, Hinder RA, Albertucci M. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am J Gastroenterol 1992;87(9):1102–11.
Shay S, Tutuian R, Sifrim D, Vela M, Wise J, Balaji N, Zhang X, Adhami T, Murray J, Peters JH, Castell DO. Twenty-four hour ambulatory simultaneous impedance and pH monitoring: a multicenter report of normal values from 60 healthy volunteers. Am J Gastroenterol 2004;99(6):1037–43.
Mainie I, Tutuian R, Agrawal A, Adams D, Castell D. Combined multichannel intraluminal impedance–pH monitoring to select patients with persistent gastro-oesophageal reflux for laparoscopic Nissen fundoplication. Br J Surg 2006;93(12):1483–7.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digestive Disease Week 2012
The Society for Surgery of the Alimentary Tract Plenary Session
San Diego, California, 21 May 2012
Rights and permissions
About this article
Cite this article
Wilshire, C.L., Salvador, R., Sepesi, B. et al. Reflux-Associated Oxygen Desaturations: Usefulness in Diagnosing Reflux-Related Respiratory Symptoms. J Gastrointest Surg 17, 30–38 (2013). https://doi.org/10.1007/s11605-012-2065-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-2065-5