Abstract
Background
Percutaneous cholecystostomy is an alternative treatment for acute cholecystitis patients with high surgical risk.
Methods
One hundred and sixty-six patients consecutively treated by percutaneous cholecystostomy for acute cholecystitis in a single medical center were retrospectively reviewed.
Results
The cohort included 121 males and 45 females with mean age of 75.9 years. The overall inhospital mortality rate was 15.1 % (n = 25). Elevated serum creatinine level at diagnosis [odds ratio (OR) 1.497; p = 0.020], septic shock (OR 11.755; p = 0.001), and development of cholecystitis during admission (OR 7.256; p = 0.007) were predictive of inhospital mortality. Of 126 patients who recovered from calculous cholecystitis, 11 experienced recurrent cholecystitis within 2 months. Serum C-reactive protein (CRP) level >15 mg dl−1 at diagnosis [hazard ratio (HR) 10.141; p = 0.027] and drainage duration of cholecystostomy longer than 2 weeks (HR 3.638; p = 0.039) were independent risk factors of early recurrence. The 53 patients who underwent cholecystectomy had an 18.9 % perioperative complication rate and no operation-related mortality.
Conclusions
In-patients or those with septic shock or renal insufficiency have worse outcome. Prolonged drainage duration and high CRP level predict early recurrence. Removal of the drainage tube is recommended after resolution of the acute illness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acute cholecystitis is usually related to gallstone disease, a condition present in about 10–15 % of the adult western population.1 Acute calculous cholecystitis is associated with increased overall, cardiovascular disease, and cancer mortality.2 Although acalculous cholecystitis accounts for only ~10 % of acute cholecystitis, it usually occurs in critically ill patients and is associated with high morbidity and mortality.3 Patients diagnosed with acute cholecystitis should be initially treated with intravenous fluids, analgesia, and antibiotics, with nothing orally.4 Early cholecystectomy is the standard treatment with laparoscopy as the preferred method.5 The perioperative mortality rate of early laparoscopic cholecystectomy is around 1 % in low-risk patients.6,7 However, in the elderly and in patients with significant comorbidities, cholecystectomy can result in morbidity up to 41 % and perioperative mortality up to 18 %.7–11
Percutaneous cholecystostomy is a minimally invasive radiologic procedure first described by Radder for patients with acute cholecystitis in the 1980s.12 In previous studies, it has been shown as a safe option and alternative treatment for severe septic patients or for those with serious comorbidities not responding to conservative treatment or those unfit to undergo surgery.13–16 Clinical improvement within 72 h after percutaneous cholecystostomy is reliably common, with a range of 82–93 %.13–16 In a recent systemic review, rates for mortality caused by biliary tract infection and associated with the procedure were 3.6 and 0.36 %, respectively.13 Delayed cholecystectomy (2 months after the initial attack has subsided) was suggested in patients with gallstones to prevent recurrence.17–20
However, the clinical predictors of mortality for patients with acute cholecystitis treated with percutaneous cholecystostomy remain unclear, as well as how long the drainage tube should remain. The present study aimed to analyze these outcomes after cholecystostomy.
Material and Methods
Patients
Between January 2009 and August 2010, 166 patients consecutively diagnosed as acute cholecystitis who underwent percutaneous cholecystostomy at Taipei Veterans General Hospital were enrolled in this retrospective study. Diagnosis was based on clinical presentation, physical examination, laboratory data, and imaging studies like abdominal sonography or computer tomography (CT).20 When acute cholecystitis was diagnosed, all patients received immediate medical treatment and evaluation of their surgical risk based on the American Society of Anesthesiologists (ASA) classification.21 One hundred and six-one patients (97 %) were classified in ASA class III or IV and refused early cholecystectomy because of high surgical risk. The remaining five patients with ASA class II refused surgery due to personal reasons. The indications of percutaneous cholecystostomy were severe sepsis, septic shock, local gallbladder rupture, or poor response to 48-h medical treatment.
Percutaneous Cholecystostomy
Percutaneous cholecystostomy was performed by radiologists and was technically successful in all patients. After local anesthesia with lidocaine, an 8-Fr pigtail catheter (Bioteque Corporation, Taipei, Taiwan) was inserted into the gallbladder through transhepatic route under ultrasound guidance. Bile sample was obtained for culture.
Data Collection
Medical records were reviewed for data collection. The following data were collected: (1) patients characteristics, such as age, sex, underlying diseases, and ASA scores; (2) clinical findings like vital signs on admission, symptoms, and indications of drainage; (3) serum biochemistry, including alanine aminotransferase (ALT), aspartate aminotransferase, total bilirubin (TB), alkaline phosphatase (Alk-P), γ-glutamyl-transferase (γ-GT), blood urea nitrogen, creatinine, complete blood cell counts, and C-reactive protein (CRP) by Rochi/Hitachi Modular Analytics Systems (Roche Diagnostics GmbH, Mannheim, Germany); (4) abdominal CT scan or sonography; (5) procedure-related complications and mortality; and (6) duration of drainage, hospital stay, inhospital mortality, and causes of mortality.
The patients were followed up until December 2011 (median follow-up, 25.4 months). During this period, the recurrence of biliary events and subsequent cholecystectomy was recorded. In patients who underwent cholecystectomy, the type of surgery, conversion rate from laparoscopic to open cholecystectomy, perioperative complications, and operation time were also recorded.
Statistical Analysis
All statistical analyses were performed using the SPSS 17.0 for Windows (SPSS. Inc., Chicago, IL, USA). Continuous variables were presented as mean ± standard deviation. Logistic regression was used to determine the effects of variables on inhospital mortality, conversion surgery, and perioperative complications. Only variables with p value proximal to 0.1 in univariate analysis were selected for multivariate analysis. Effects of categorical variables on outcomes were tested by chi-square test.
Univariate analysis of early recurrence of acute cholecystitis (within 2 months after the initial attack has subsided) was performed by log rank test, and multivariate analysis was performed by multivariate Cox regression models using variables selected by univariate analysis. Subjects were censored on the last day of follow-up (2 months) or cholecystectomy. The event considered was recurrent acute cholecystitis. A two-tailed p < 0.05 was considered as significant.
Results
Basic Patient Characteristics and Clinical Efficacy of Cholecystostomy
The basic characteristics of the enrolled patients showed that most (72.9 %) were male (Table 1). One hundred and fifty-one patients (90.9 %) had abdominal pain and 120 patients (72.3 %) had fever at the time of presentation. Changes of symptoms and laboratory data 3 days after percutaneous cholecystostomy were shown in Table 2. Clinical improvement of abdominal pain and fever within 3 days was noted in 129 (85.4 %) and 106 (88.3 %) patients, respectively. There was significant reduction of white blood cell count and improvement of laboratory data, including TB, ALT, γ-GT, and CRP.
Safety of Percutaneous Cholecystostomy
Drainage duration of cholecystostomy was 16.6 ± 14.0 days and 27 patients (16.3 %) experienced drainage tube-related complications, such as tube dislodgement (n = 17), bleeding that required transfusion (n = 6), bile leakage (n = 3), and tube obstruction (n = 1). Six patients with dislodged tubes underwent cholecystostomy re-insertion or revision because the acute illness did not resolve completely. Two of three patients with bile leakage suffered from peritonitis due to bile leak. One patient received emergency laparotomy and recovered well, while another refused surgery and died. One patient had biloma formation that improved after drainage and three had bloody drainage that improved after correction of coagulopathy or blood transfusion. Two patients had hematoma formation that resolved spontaneously under conservative treatment. One patient suffered from uncontrolled bleeding but refused surgery or angiographic intervention and died. Overall, the procedure-related mortality rate was 1.2 % (n = 2).
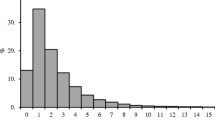
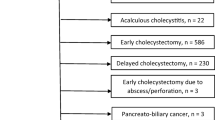
Clinical Outcomes and Predictors of Inhospital Mortality
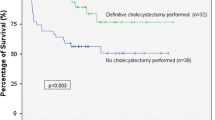
The clinical outcomes of all 166 patients were shown in Fig. 1. In total, 25 patients (15.1 %) died during hospitalization, most (n = 15, 60 %) due to acute cholecystitis-induced sepsis. On univariate analysis, levels of hemoglobin, serum albumin, and creatinine, Alk-P, diabetes mellitus, acalculous cholecystitis, septic shock, and in-patients admission for other reasons compared to out-patients primarily presenting at the emergency department (ED) had prognostic value on inhospital mortality (Table 3). By multivariate analysis, higher serum creatinine levels, presence of septic shock, and in-patients admission for other reasons were independent risk factors of inhospital mortality, which was 43.2 % (19 of 44) among patients with septic shock compared to 4.9 % for patients without septic shock (6 of 122) (p < 0.001). Receiver operating characteristic curve analysis demonstrated that a cutoff value of serum creatinine of 1.5 mg dl−1 had the best prognostic value for inhospital mortality, with 68 % sensitivity and 75.2 % specificity (Fig. 2). The average length of hospital stay was 24.8 ± 21.4 days. The calculous cholecystitis patients with choledocolithiasis or cystic duct stones did not have higher cholecystostomy-related complications and inhospital mortality compared with those with gallstones only (Supplementary Table 1).
The receiver operating characteristic curve of serum creatinine levels for predicting inhospital mortality. A cutoff value of 1.5 mg dl−1 has the best prognostic value, with 68 % sensitivity and 75.2 % specificity. The area under curve is 0.696 (p = 0.002). Sn sensitivity, Sp specificity, Cr creatinine
In this cohort, 15 patients recovered from acalculous cholecystitis and none had recurrent cholecystitis within 2 months. Among the 126 patients who recovered from calculous cholecystitis, 11 (8.7 %) had early recurrence of acute cholecystitis within 2 months while waiting for delayed cholecystectomy. On univariate and multivariate analyses, serum CRP level >15 mg dl−1 at diagnosis of acute cholecystitis and drainage duration of cholecystostomy tube longer than 2 weeks were predictive of early recurrence of acute cholecystitis (Table 4; Fig. 3). The cumulative recurrence rate at 2 months of patients with serum CRP level higher or lower than 15 mg dl−1 was 15.6 and 1.6 %, respectively. Patients with drainage duration more or less than 2 weeks had a cumulative recurrence rate of 16.7 and 4.8 %, respectively. The interval of recurrence was 37.8 ± 12.3 days post-drainage in the higher CRP group.
Cumulative recurrence rate of acute cholecystitis within 2 months in a patients with drainage duration of cholecystostomy of more or less than 2 weeks or b patients with serum C-reactive protein level higher or lower than 15 mg dl−1 at diagnosis of acute cholecystitis. The p value corresponds to log-rank test
In 53 patients who received cholecystectomy, laparoscopic cholecystectomy (LC) was performed in 35 (66.1 %) and was converted to open cholecystectomy (CONV) in 12 (34.3 %) due to severe adhesions. The rate of previous abdominal surgery between the LC and CONV patients was not different (13.1 vs. 8.3 %; p = 1.000). The overall operation-related complication rate was 18.9 % (Table 5) with no perioperative mortality. The mean operation time of LC, CONV, and OC was 117.1 ± 54.1, 230.8 ± 78.1, and 182.3 ± 74.2 min, respectively.
The outcomes of patients stratified with different indications for cholecystostomy are shown in Table 6. The patients with severe sepsis or septic shock had a higher inhospital mortality rate and a lower rate of remission of fever. There is no significant difference in laboratory data changes, improvement of abdominal pain, complications of cholecystostomy, early recurrence of acute calculous cholecystitis, perioperative complications, conversion rate, and operation time among the three groups.
The CONV patients had significantly more complications than LC patients (33.3 vs. 4.5 %; p = 0.042). No variables like age, white blood cell counts, serum CRP, or albumin levels, body mass index, and drainage duration of cholecystostomy were associated with conversion surgery or perioperative complications (Table 7). However, patients who underwent conversion surgery were all males (p = 0.032, Fisher’s exact test). Besides, neurologic comorbidities (i.e., cerebral vascular accidents, Parkinsonism, and seizure) were associated with conversion surgery. On multivariate analysis, neurologic comorbidities were not predicative of conversion surgery (p = 0.546).
Discussion
This study shows that percutaneous cholecystostomy is an effective and safe treatment for acute cholecystitis in patients at high risk for surgery. Serum creatinine level, septic shock, and inpatient admission for other reasons have predictive value on inhospital mortality. Moreover, higher serum CRP level and prolonged drainage duration of cholecystostomy are independent risk factors of early recurrence of acute calculous cholecystitis.
In this series, percutaneous cholecystostomy was technically successful in all patients, with a clinical improvement rate of 88 % that is comparable to another study.13 Laboratory data also significantly improved within the first 3 days. Most complications of cholecystostomy were minor while fatal complications were rare. Compared to the high morbidity and mortality rates of cholecystectomy in patients with high surgical risk and acutely inflamed gallbladder,7,10,11 this study confirmed that percutaneous cholecystostomy is a technically easier, relative safer, and effective treatment that may be a good bridge for delayed cholecystectomy until the patient’s condition improves.
In previous studies, Joseph et al.22 found that in-patients who developed acute cholecystitis on admission had significantly higher 30-day mortality than patients who presented to the ED primarily with acute cholecystitis. Ha et al.19 found that shock on admission was an independent risk factor for inhospital death. In the present study, patients with septic shock and in-patients with acute cholecystitis were associated with higher inhospital mortality. In-patients admitted for other reasons often have more comorbidities or concomitant acute illnesses than out-patients presenting with cholecystitis at the ED. Septic shock is associated with poor prognosis in patients with infection, with mortality rate approximately 40 % even with optimal treatment.23 This suggests that inhospital mortality is mainly associated with the patient’s general condition and severity of sepsis.
Interestingly, the present study reveals that higher serum creatinine level is an independent risk factor of mortality. Elevated serum creatinine level reflects underlining chronic kidney disease and/or acute renal failure due to sepsis. It has been known that chronic kidney disease and acute renal failure are associated with increased risk of infection-related mortality.24,25 Based on the findings here, more attention should be given to patients who develop acute cholecystitis during admission, who manifest with septic shock, or who have serum creatinine levels >1.5 mg dl−1 on diagnosis.
How long the drainage tube should remain is still unclear. Morse et al.17 found that the cholecystostomy tube should remain in place in critically ill patients until cholecystectomy because removal of the drainage tube before subsequent cholecystectomy is associated with high recurrence of cholecystitis. In the present study, 11 patients suffered from recurrent acute cholecystitis within 2 months while waiting for delayed cholecystectomy. However, drainage duration of cholecystostomy tube longer than 2 weeks is an independent risk factor of early recurrence. It is demonstrated in animal studies that irritation of the gallbladder mucosa (mechanically or by infusion of irritant) results in acute cholecystitis.26,27 Patients with prolonged drainage duration in the present study may have more irritation of gallbladder mucosa that resulted in recurrent cholecystitis. Furthermore, bacterial colonization of the drainage catheter may also increase the risk of infection.28 In this study, most patients had resolution of acute cholecystitis within 8–10 days from cholecystostomy insertion to full recovery. Therefore, the cholecystostomy tube is better removed after resolution of the acute illness.
Moreover, higher serum CRP levels at diagnosis also predict early recurrence. Higher CRP level reflects more severe local inflammation that may lead to easy recurrence of cholecystitis. Sub-acute cholecystectomy (within 6 weeks after resolution of acute illness) may be suggested in these patients to prevent early recurrence. However, prospective studies are needed to elucidate the advantages and disadvantages of sub-acute surgery on these patients.
Notably, 35 patients in the present study began as laparoscopic cholecystectomy and 12 converted to the open procedures due to severe adhesion in the abdomen during surgery. The conversion rate of laparoscopic cholecystectomy in patients with acute cholecystitis ranges between 5 and 30 % in different cohorts.20 There are many established factors associated with conversion, including age over 60 years, WBC >18,000 cumm−1 at the time of presentation, male, obesity, emergency status, serum albumin, multiple comorbidities, previous abdominal surgery, and inexperienced operator.20,29,30 In the current study, the conversion rate is only significantly related to males and neurologic comorbidities, not to age, WBC, levels of albumin and CRP at diagnosis, previous abdominal surgery, drainage duration, or obesity. The surgeons in this study were all experienced in laparoscopic surgery. Nevertheless, most patients enrolled were male, which may explain the relatively higher conversion rate in this study.
Moreover, there is limited data about perioperative morbidities and mortality of subsequent cholecystectomy in patients previously treated with cholecystostomy. The perioperative morbidity rate varies from 12 to 30 % in several retrospective studies with small patient numbers.31,32 In a recent systemic review, more than 40 % of patients eventually came to surgery, with 2.1 % mortality rate in elective cholecystectomy (mainly laparoscopic, either sub-acute or delayed).13 In this study, which has larger patient numbers, the overall perioperative complication rate is 19.2 % with no perioperative mortality. In addition, the CONV patients in this study have a higher perioperative complication rate than LC patients. The results here are comparable to a large cohort in the USA.33 Taken together, patients treated with cholecystostomy have a high conversion rate of interval laparoscopic cholecystectomy, which is associated with high morbidity rate after cholecystectomy.
The limitations of this study pertain primarily to its retrospective nature, which results in incomplete data acquisition for some patients. Furthermore, the patients treated at the study institution, which is a veterans hospital and tertiary center with a large population of elderly males with advanced comorbidities, may not correlate well with the general population.
In conclusion, percutaneous cholecystostomy is an effective treatment for acute cholecystitis in patients with high surgical risk. The outcomes are worse in patients with renal insufficiency and septic shock, and in-patients who developed cholecystitis during admission. High serum CRP level and prolonged drainage duration of cholecystostomy significantly predict early recurrence within 2 months. Removal of the drainage tube is suggested after resolution of the acute illness.
References
Halldestam I, Enell EL, Kullman E, Borch K. Development of symptoms and complications in individuals with asymptomatic gallstones. Br J Surg 2004;91:734–738.
Ruhl CE, Everhart JE. Gallstone disease is associated with increased mortality in the United States. Gastroenterology 2011;140:508–516.
Kalliafas S, Ziegler DW, Flancbaum L, Choban PS. Acute acalculous cholecystitis: incidence, risk factors, diagnosis, and outcome. Am Surg 1998;64:471–475.
Miura F, Takada T, Kawarada Y, Nimura Y, Wada K, Hirota M, Nagino M, Tsuyuguchi T, Mayumi T, Yoshida M, Strasberg SM, Pitt HA, Belghiti J, de Santibanes E, Gadacz TR, Gouma DJ, Fan ST, Chen MF, Padbury RT, Bornman PC, Kim SW, Liau KH, Belli G, Dervenis C. Flowcharts for the diagnosis and treatment of acute cholangitis and cholecystitis: Tokyo guidelines. J Hepatobiliary Pancreat Surg 2007;14:27–34.
Gurusamy KS, Samraj K. Early versus delayed laparoscopic cholecystectomy for acute cholecystitis. Cochrane Database Syst Rev 2006:CD005440.
Steiner CA, Bass EB, Talamini MA, Pitt HA, Steinberg EP. Surgical rates and operative mortality for open and laparoscopic cholecystectomy in Maryland. N Engl J Med 1994;330:403–408.
Huber DF, Martin EW, Jr., Cooperman M. Cholecystectomy in elderly patients. Am J Surg 1983;146:719–722.
Pessaux P, Regenet N, Tuech JJ, Rouge C, Bergamaschi R, Arnaud JP. Laparoscopic versus open cholecystectomy: a prospective comparative study in the elderly with acute cholecystitis. Surg Laparosc Endosc Percutan Tech 2001;11:252–255.
Decker G, Goergen M, Philippart P, Mendes da Costa P. Laparoscopic cholecystectomy for acute cholecystitis in geriatric patients. Acta Chir Belg 2001;101:294–299.
Houghton PW, Jenkinson LR, Donaldson LA. Cholecystectomy in the elderly: a prospective study. Br J Surg 1985;72:220–222.
Margiotta SJ, Jr., Willis IH, Wallack MK. Cholecystectomy in the elderly. Am Surg 1988;54:34–39.
Radder RW. Ultrasonically guided percutaneous catheter drainage for gallbladder empyema. Diagn Imaging 1980;49:330–333.
Winbladh A, Gullstrand P, Svanvik J, Sandstrom P. Systematic review of cholecystostomy as a treatment option in acute cholecystitis. HPB (Oxford) 2009;11:183–193.
Davis CA, Landercasper J, Gundersen LH, Lambert PJ. Effective use of percutaneous cholecystostomy in high-risk surgical patients: techniques, tube management, and results. Arch Surg 1999;134:727–731.
Browning PD, McGahan JP, Gerscovich EO. Percutaneous cholecystostomy for suspected acute cholecystitis in the hospitalized patient. J Vasc Interv Radiol 1993;4:531–537.
Kiviniemi H, Makela JT, Autio R, Tikkakoski T, Leinonen S, Siniluoto T, Perala J, Paivansalo M, Merikanto J. Percutaneous cholecystostomy in acute cholecystitis in high-risk patients: an analysis of 69 patients. Int Surg 1998;83:299–302.
Morse BC, Smith JB, Lawdahl RB, Roettger RH. Management of acute cholecystitis in critically ill patients: contemporary role for cholecystostomy and subsequent cholecystectomy. Am Surg 2010;76:708–712.
McKay A, Abulfaraj M, Lipschitz J. Short- and long-term outcomes following percutaneous cholecystostomy for acute cholecystitis in high-risk patients. Surg Endosc 2012;26(5):1343–1351.
Ha JP, Tsui KK, Tang CN, Siu WT, Fung KH, Li MK. Cholecystectomy or not after percutaneous cholecystostomy for acute calculous cholecystitis in high-risk patients. Hepatogastroenterology 2008;55:1497–1502.
Strasberg SM. Clinical practice. Acute calculous cholecystitis. N Engl J Med 2008;358:2804–2811.
Little JP. Consistency of ASA grading. Anaesthesia 1995;50:658–659.
Joseph T, Unver K, Hwang GL, Rosenberg J, Sze DY, Hashimi S, Kothary N, Louie JD, Kuo WT, Hofmann LV, Hovsepian DM. Percutaneous cholecystostomy for acute cholecystitis: ten-year experience. J Vasc Interv Radiol 2012;23:83–88.
Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP. The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA 1995;273:117–123.
Wang HE, Gamboa C, Warnock DG, Muntner P. Chronic kidney disease and risk of death from infection. Am J Nephrol 2011;34:330–336.
Uchino S, Kellum JA, Bellomo R, Doig GS, Morimatsu H, Morgera S, Schetz M, Tan I, Bouman C, Macedo E, Gibney N, Tolwani A, Ronco C. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA 2005;294:813–818.
Morris CR, Hohf RP, Ivy AC. An experimental study of the role of stasis in the etiology of cholecystitis. Surgery 1952;32:673–685.
Roslyn JJ, DenBesten L, Thompson JE, Jr., Silverman BF. Roles of lithogenic bile and cystic duct occlusion in the pathogenesis of acute cholecystitis. Am J Surg 1980;140:126–130.
Crnich CJ, Drinka P. Medical device-associated infections in the long-term care setting. Infect Dis Clin North Am 2012;26(1):143–164.
Rattner DW, Ferguson C, Warshaw AL. Factors associated with successful laparoscopic cholecystectomy for acute cholecystitis. Ann Surg 1993;217:233–236.
Rosen M, Brody F, Ponsky J. Predictive factors for conversion of laparoscopic cholecystectomy. Am J Surg 2002;184:254–258.
Lee KT, Wong SR, Cheng JS, Ker CG, Sheen PC, Liu YE. Ultrasound-guided percutaneous cholecystostomy as an initial treatment for acute cholecystitis in elderly patients. Dig Surg 1998;15:328–332.
Costi R, Le Bian A, Cauchy F, Diop PS, Carloni A, Catherine L, Smadja C. Synchronous pyogenic liver abscess and acute cholecystitis: how to recognize it and what to do (emergency cholecystostomy followed by delayed laparoscopic cholecystectomy). Surg Endosc 2012;26(1):205–213.
Kaafarani HM, Smith TS, Neumayer L, Berger DH, Depalma RG, Itani KM. Trends, outcomes, and predictors of open and conversion to open cholecystectomy in Veterans Health Administration hospitals. Am J Surg 2010;200:32–40.
Acknowledgments
The authors thank Ms. Chi-Yi Peng for her editing assistance. This work was supported by grants from the Taipei Veterans General Hospital in Taipei, Taiwan (nos. V101B-021 and V101A-015).
Conflict of Interest
None
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 18 kb)
Rights and permissions
About this article
Cite this article
Hsieh, YC., Chen, CK., Su, CW. et al. Outcome After Percutaneous Cholecystostomy for Acute Cholecystitis: a Single-Center Experience. J Gastrointest Surg 16, 1860–1868 (2012). https://doi.org/10.1007/s11605-012-1965-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-012-1965-8