Abstract
Objective
Lateral internal sphincterotomy is an effective treatment for fissure in ano but carries a definite risk of incontinence. In trial to avoid this complication, segmental lateral internal sphincterotomy was used to treat chronic anal fissures.
Design
The lateral internal sphincterotomy was done in two parts and at different planes.
Setting
This study was conducted in the General Surgery Department, Zagazig University Hospital, Egypt.
Patients
This study was undertaken on 50 patients (43 men and seven women, with mean age of 37.3 years) with chronic fissure in ano from January 2009 to December 2010.
Interventions
Under general or local anesthesia, lateral internal sphincterotomy was done in two segments under direct vision. Preoperative and postoperative anal manometry study was recorded.
Main Outcome Measures
Postoperative course with early and long-term results were recorded. Mean follow-up was 18.5 months (ranging from 6 to 24 months).
Results
In 31 patients, the technique was done under general anesthesia and the remainder under local anesthesia. The fissures and anal wounds were healed within 4 weeks. Pain was significantly reduced in all patients at day 1 postoperative. Early complications included mild hematoma and urine retention in one male patient (2%). No transient or any persistent degree of incontinence occurred in these patients group.
Conclusion
Segmental lateral internal sphincterotomy is a safe, easy, and effective procedure and not associated with risk of incontinence for the treatment of chronic anal fissure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anal fissure (AF) is a common disorder which affects all age groups with an equal incidence in both sexes; 90% are situated posteriorly and 10% anteriorly.1 The exact etiology of AF is unknown but trauma caused by fecal mass, diarrhea, constant saddle vibration in bikers, water steam from bidet toilets, and hypertonicity of the internal sphincter are thought to be initiating factors.2–5 Lateral internal sphincterotomy is considered the gold standard therapy of chronic anal fissure. It relieves symptoms with high rate of healing and less long-term recurrence.6 This optimal therapy has, however, been associated with the development of period of transient postoperative impairment of anal continence in 30% of patients which can become permanent.7,8 To avoid these side effects, segmental lateral internal sphincterotomy was used for treatment of chronic anal fissure in this study.
Patients and Methods
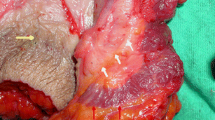
During a period of 2 years between January 2009 and December 2010, 50 patients (43 males and seven females, with median age of 37.3 years; range, 17–57 years) with chronic anal fissure have been enrolled in this study. A chronic anal fissure was defined by duration of symptoms longer than 3 months, presence of induration at fissure edges, sentinel pile, hypertrophied anal papillae, and circular muscle fibers at the base of the cutaneous defect. The fissure was found posterior in 44 patients, anterior in five patients, and both in one patient. The most common symptoms encountered in this series were: pain and discomfort with bowel movements in all cases (100%) and bright rectal bleeding in 80%. Also, an occasional undue expulsive force from a hard fecal mass was found in 60% of our patients, and constipation in 53%. No history of anal incontinence was found in this patient group. Anal manometry was performed for all patients preoperatively and 3 months postoperatively, using the waterfilled 10 F balloon rectal catheter of the Ellipse 4 Andromeda water cystometry system (Andromeda, Medizinishe Systeme GambH Wallbergstr, 5 D-82024 Taufkinhen) and recorded in centimeters H2O for each case. All patients have received medical therapy as the first line of treatment but presented with recurrent or persistent fissures. The medical treatment was in the form of a stool softener, analgesics, and 0.2% glyceryl trinitate for at least 6 weeks. Informed consent was obtained from all patients after the nature of the procedure was explained. In the lithotomy position, segmental lateral sphincterotomy was performed under general anesthesia in 31 cases and under local anesthesia in 19 cases, using an Eisenhammer speculum in the anal canal. The internal sphincter is divided in two segments from anoderm up to dentate line but not in the same line. First segment starts from anoderm line to a point midway between it and the dentate line, where the internal sphincter is divided under direct vision. Second segment starts from a part midway point between the anoderm line and dentate line to dentate line, where the internal sphincter is divided under direct vision. The two segments are equal in length and parallel with about 1 cm between them. Good haemostasis is achieved by using diathermy. The wounds were left open to heal with secondary intention (Fig. 1). Third generation cephalosporin antibiotics were given perioperatively, in all patients. The mean follow-up period was 18.5 months (6–24 months) for early and late complications.
1 External anal sphincter. 2 Internal anal sphincter. 3 Anal verge. 4 Dentate line. Segmental lateral internal sphincterotomy procedure. In this procedure, internal sphincterotomy is done in two incisions: first incision (a–b) extends from the anal verge points a′ to b midway between the anal verge and dentate line and divided the internal anal sphincter in this area. Second incision (a′–b′) extends from the midway point between the anal verge to dentate line a′ and to dentate line point b′ and divided the internal anal sphincter in this area. The two incisions a–b and a′–b′ are equal in length and are parallel with about 1 cm between them
Results
The main presenting symptom in this group of patients was pain, which occurred during defecation and hours afterwards. Pain was significantly reduced in all patients in the first postoperative hours while symptoms such as bleeding and irritation were reduced in most patients in the next day. No patient reported incontinence on direct questioning preoperative. The operation time ranged from 15 to 25 min (mean, 17 min). The main hospital stay was 1 day. During follow-up, one patient complained of minor bleeding during the first 3 days (2%) and one patient (2%) developed perianal abscess at 2 weeks postoperative, which was incised and drained under general anesthesia. No fissure relapse was observed during follow-up period. Anal fissures and sphincterotomy wounds show complete healing within 4 weeks (ranging from 2 to 5 weeks). An increased basal tone of the internal sphincter and an elevated resting pressure were the preoperative manometric findings in all of our patients. After 3 months postoperatively, basal tone of the internal sphincter and resting anal pressure retuned to normal levels in all patients. The mean maximal resting pressure value was found to be 108.19 ± 15.18 cm H2O preoperatively and 70.27 ± 9.33 cm H2O at 3 months postoperatively. No anal incontinence was reported in this patients group after segmental lateral sphincterotomy during the period of follow-up.
Discussion
In our study, 100% patients were presented with painful defecation and 80% with bleeding, corresponding to 98.8% and 71.4% in other study. High percentage of male to female (6.1:1) in our study was due to the fact that most of the female patients avoid presenting to male surgeons for treatment due to shyness or modesty. This study favored the reports that anal fissure is common in middle age and at posterior midline of anus.9 The most recent theories on etiopathogenesis of anal fissures have focused on increased tonicity of the internal anal sphincter, which contains smooth muscle fibers whose contraction is controlled by neural influences and myogenic mechanism.10 Factors causing internal sphincter hypertonia are not well understood, but a significant role in perpetrating the muscle spasm is played by the trauma caused by passage of hard stools on the mucosa.4,5 Spasm of the sphincter not only promotes constipation (thus setting up a vicious cycle) but also leads to compression of the terminal arterioles supplying the mucosa of the anal canal. Impaired blood flow in this already poorly perfused area prevents fissure healing.10 Since the introduction of the posterior internal sphincterotomy by Eisenhammer11 in 1951, chronic anal fissure has been managed with surgery once conservative measures failed. The more safe lateral sphincterotomy, popularized by Notaras12 in 1969, has until now been the mainstay of treatment to reduce the pathologically raised pressure profile within the anal canal. Despite the surgery is highly efficacious and succeeds in curing chronic anal fissure in more than 90% of patients (often exceeds 95% with high satisfaction), postoperative impairment of continence is not uncommon. The incidence is not well documented and varies between 0% and 35% for flatus incontinence, 0% and 21% for liquid incontinence, and 0% and 5% for solid stool incontinence.13 To minimize this risk, several authors have tried a more limited division of internal sphincter, a tailored or controlled sphincterotomy 14 and recently, injection of botulinum toxin.15 No incontinence or failure of fissure healing were reported in this patients group which treated by segmental lateral internal sphincterotomy. From the data of previous studies, we believed that the incontinence follow lateral internal sphincterotomy due to gutter formation at the site of sphincter division. This gutter allowed to rectal contents (flatus or stool) to pass through it in spite of internal anal sphincter contraction. The prove for this theory that, the risk of incontinence more with total (up to dentate line) than limited (up to fissure apex only) lateral internal sphincterotomy,16 because total technique produces groove extends from the anal verge to the dentate line in same continuity. Also, open lateral sphincterotomy is associated with more risk of incontinence than the closed one because the groove after the open one is deeper. Also, incontinence after lateral internal sphincterotomy is usually in a form of flatus incontinence,9 because flatus are easy to pass through this groove. One study reported that perianal injection of autologous fat treated the anal incontinence well.17 We think this is due to obliteration of anal gutters by the injected fat. The extended gutter formation from the anal verge to the dentate line is responsible for incontinence complication after total lateral internal sphincterotomy. With our technique, total internal sphincterotomy was done in two short incisions and not in the same continuity, producing good relief of sphincter hypertonia leading to good fissure healing, and secondly, two short incisions healed rapidly by second intension and without gutter formation avoiding anal incontinence. This manuscript represents preliminary data, which need more evaluation studies on long run about its efficacy and complications.
Conclusion
Segmental lateral internal sphincterotomy is a novel, safe, and effective way of treating chronic anal fissure, and it is not associated with any risk of anal incontinence.
References
Dykes SL, Madoff RD. Benign anorectal: anal fissure. In: Wolff BG, Fleshman JW, Beck DE, Pemberton JH, Wexner SD, eds. The ASCRS textbook of colon and rectal surgery. New York: Springer, 2007: 178–191
Brisinda G, Cadeddu F, Brandara F, Brisinda D, Maria G. Treating chronic anal fissure with botulinum neurotoxin. Nat Clin Pract Gastroenterol Hepatol 2004; 1:82–89
Elia Guedea M, Gracia Solanas JA, Royo Dachary P, Ramirez Rodriguez JM, Aguilella Diago V, Martinez Diez M. Prevalence of anal diseases after Scopinaro’s biliopancreatic bypass for super-obese patients. Cir Esp 2008; 84:132–137
Sauper T, Lanthaler M, Biebl M, Weiss H, Nehoda H. Impaired anal sphincter function in professional cyclists. Wien Klin Wochenschr 2007; 119: 170–173
Garg P. Water stream in a bidet-toilet as a cause of anterior fissure-in-ano: a preliminary report. Colorectal Dis 2010; 12:601–602
Aivaz O, Rayhanabad J, Nguyen V, Haigh PI, Abbas M. Botulinum toxin A with Fissurectomy is a viable alternative to lateral internal sphincterotomy for chronic anal fissure. Am Surg 2009; 75: 925–928
Hyman N. Incontinence after lateral internal sphincterotomy: a prospective study and quality of life assessment. Dis Colon Rectum 2004; 47:35–38
Brown CJ, Dubreuil D, Santoro L, Liu M, O’Connor BI, McLeod RS. Lateral internal sphincterotomy is superior to topical nitroglycerin for healing chronic anal fissure and does not compromise long-term fecal continence: six-years follow up of multicenter, randomized, controlled trail. Dis Colon Rectum 2007; 50:442–448.
García-Granero E, Sanahuja A, García-Botello SA, Faiz O, Esclápez P, Espí A, Flor B, Minguez M, Lledó S. The ideal lateral internal sphincterotomy: clinical and endosonographic evaluation following open and closed internal anal sphincterotomy. Colorectal Dis. 2009; 11:502–7
Ayantunde AA, Debrah SA. Current concepts in anal fissures. World J Surg 2006; 30:2246–60.
Eisenhammer S. The evaluation of the internal anal sphincterotomy operation with special reference to anal fissure. Surg Gynecol Obstet 1959; 109:583–90.
Notaras MJ. Lateral subcutaneous sphincterotomy for anal fissure- a new technique. J R Soc Med 1969; 62:713.
Nelson R. Non surgical therapy for anal fissure. Cochrane Database Syst Rev 2006; 4:CD003431.
Menteş BB, Güner MK, Leventoglu S, Akyürek N. Fine-tuning of the extent of the lateral internal sphincterotomy: spasm-controlled vs. up to the fissure apex. Dis Colon Rectum 2008; 51:128–33.
Wollina U. Pharmacological sphincterotomy for chronic anal fissures by botulinum toxin a. J Cutan Aesthet Surg. 2008 Jul;1(2):58–63.
Menteş BB, Ege B, Leventoglu S, Oguz M, Karadag A Extent of lateral internal sphincterotomy: up to the dentate line or up to the fissure apex? Dis Colon Rectum. 2005; 48:365–70.
Shafik A. Perianal injection of autologous fat for treatment of sphincteric incontinence. Dis Colon Rectum 1995; 38:583–7.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lasheen, A.E., Morsy, M.M. & Fiad, A.A. Segmental Internal Sphincterotomy—A New Technique for Treatment of Chronic Anal Fissure. J Gastrointest Surg 15, 2271–2274 (2011). https://doi.org/10.1007/s11605-011-1689-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1689-1