Abstract
Introduction
Crohn’s disease is one of the chronic inflammatory diseases of the gastrointestinal tract that is often complicated by stricture formation with resulting obstructive symptoms. The technical repertoire of strictureplasty procedures has increased over the years in an effort to manage the diverse presentations of this condition while limiting the need for bowel resection. In this comprehensive review, we describe, compare, categorize, and appraise the strengths and weaknesses of 15 unique strictureplasty techniques.
Methods
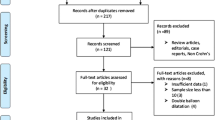
To identify all unique strictureplasty procedures, a Medline search utilizing “Crohn’s disease,” “surgical therapy,” “strictureplasty,” “enteroenterostomy,” “Heineke–Mikulicz,” and “side-to-side isoperistaltic” strictureplasty as medical subject headings was completed. PubMed, Ovid, Embase, and Cochrane database searches were conducted. Relevant articles between 1980 to December 2010 were reviewed. We initially selected 58 articles, but only 18 introduced novel surgical procedures related to 15 types of strictureplasty in Crohn’s disease.
Results
We identified 15 types of strictureplasty techniques. These were categorized into three main groups. The revised nomenclature will facilitate the reader to understand the differences and utility of each technique. These groups include the Heineke–Mikulicz-like strictureplasties, the intermediate procedures, and the enteroenterostomies. Heineke–Mikulicz strictureplasty was the most frequently used technique.
Conclusion
Various techniques of strictureplasty have been reported in the published literature. Strictureplasty has been shown to be a safe and efficacious technique that is comparable to bowel resection for stricturing Crohn’s disease. This technique spares bowel length and puts the Crohn’s disease patient at a lower risk of developing short bowel syndrome with repeated resections.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Crohn’s disease (CD) is a chronic inflammatory disease of the panintestine. It is often debilitating without an identifiable etiology and with little or no prospect of cure. Historically, the surgical treatment for CD was reserved for complications of the disease, complications of medical treatment, or failure of medical therapy. Complications of CD include bowel obstruction, perforation, and septic complications such as abscess, fistula, and intractability.
Surgical options employed in the management of obstructive symptoms typically involve limited segmental resection, bypass of the obstructing segment, and strictureplasty. The tenets of strictureplasty had been employed earlier in the late nineteenth century for treatment of benign, chronic strictures related to peptic ulcer disease in the duodenum. Hermann Heineke and Jan Mikulicz-Radecki described the Heineke–Mikulicz (HM) pyloroplasty for relieving short segment, benign strictures in the pyloric channel in 1886. Later in 1892, Mathieu Jaboulay proposed the technique of bypassing an obstructing stricture in the pyloric area by performing a gastroduodenostomy. At the turn of the twentieth century, John M. T. Finney presented a modification of the method of lateral anastomosis on five patients in which a medium-sized obstructing peptic stricture of the pylorus could be relieved while providing adequate drainage of the stomach without too much tension on the suture line.
These techniques have been used over the years for management of obstructing peptic ulcer disease. In the 1970s, Katariya et al.1 in India reported on a series of nine patients who underwent HM-like strictureplasty for the management of benign tubercular strictures. Later in the early 1980s, Emanoel Lee and Nicos Papaioannou2 presented their work on strictureplasty in nine patients with strictures related to CD. Since then, various authors have reported on novel techniques for the surgical management of CD strictures. With resection being the initial, predominant mode of management of CD strictures and due to the recurrent behavior of the disease, patients with CD have a high risk for repeated operative interventions and a subsequent risk for short bowel syndrome.
The purpose of this current review is to categorize, compare, and highlight the strengths and limitations of 15 published strictureplasty techniques used in the management of CD. Also, we highlight and summarize existing data on outcomes of strictureplasty procedures specifically in terms of recurrent disease, surgical recurrences, and complications.
Methods
To identify all unique strictureplasty procedures, a Medline search utilizing “Crohn’s disease,” “surgical therapy,” “strictureplasty,” “enteroenterostomy,” “Heineke–Mikulicz,” and “side-to-side isoperistaltic” strictureplasty as medical subject headings was completed. PubMed, Ovid, Embase, and Cochrane database searches were conducted. Relevant articles between 1980 to December 2010 were reviewed. We initially selected 58 articles, but only 18 introduced novel surgical procedures related to 15 types of strictureplasty in Crohn’s disease. Figures of some of these techniques were hand drawn following descriptions and diagrams as illustrated by the original reference articles presented in Table 1. The remaining 40 articles we scanned for the presence of indications, contraindications, complications, and outcomes of strictureplasty. Fourteen articles did not have data relevant to the purposes of this article and were omitted.
Indications and Contraindications
Several authors3,21–23 have summarized indications and contraindications for strictureplasty. Initially, the presence of active disease was viewed as a contraindication for performing strictureplasty, but recent reports have shown that strictureplasty can be performed safely in the presence of active disease.24
Indications for strictureplasty include situations in which multiple strictures are encountered over extensive length of bowel, previous significant small bowel resection (>100 cm), patient with short bowel syndrome, stricture without phlegmon or septic fistula, duodenal strictures, recurrent ileocolic anastomotic strictures, recurrent strictures within 12 months of previous surgery, strictures at previous anastomotic sites, and growth retardation.3,21–23
On the other hand, severe inflammatory states in a patient with sepsis, associated abscess or phlegmon, and perforation with diffuse peritonitis remain contraindications to strictureplasty. Other contraindications include suspicion for carcinoma, hypoalbuminemia, likelihood of tension on the closure of the strictureplasty, intended strictureplasty site next to a segment requiring resection poor nutritional status, and surgeon inexperience.
Results
Obstructive symptoms in Crohn’s disease result from chronic fibrostenotic strictures that arise from shrinkage of mature granulation tissue as intraluminal ulcerations heal, bowel wall thickening from active CD flare-up, and adhesional disease in the peritoneal cavity. The earlier option for surgical treatment of complicated Crohn’s disease was intestinal resection of the strictured segment. Concepts of strictureplasty such as HM were applied later due to the emerging complication of short gut syndrome from the extensive resection of strictured small bowel segments.
For the purposes of this article, we categorize strictureplasties in three groups to facilitate their description and comparison. These three groups include HM-like procedures, intermediate procedures, and enteroenterostomies. Each category and each type of strictureplasty is reviewed separately.
HM-Like Procedures
HM strictureplasty was initially used earlier on for the reconstructive phase following surgical management of complicated duodenal peptic ulcer disease. The same technique is now used for the treatment of isolated short segment strictures (<10 cm). Over the years, modifications to the HM technique have been proposed by various. These HM-like procedures include the HM strictureplasty, Judd strictureplasty, Moskel–Walske–Neumayer (MWN) strictureplasty, double Heineke–Mikulicz strictureplasty, and widening ileocolic strictureplasty (Table 1).
Heineke–Mikulicz Strictureplasty
This is the most commonly performed strictureplasty technique. It is indicated for short segment strictures <10 cm.1–3,9 This technique is performed by making a single longitudinal incision over the stricture and extending it about 2 cm beyond the thickened bowel proximally and distally. The enterotomy is then closed (Fig. 1). This repair is relatively easy to perform, relieves obstruction, and maintains in-line peristaltic propagation of luminal contents without creation of a blind loop or stasis.
Judd Strictureplasty
In this technique, the strictured segment has an associated fistulous opening at its center. In this technique, the fistulous site is excised, and the remainder of the short segment (<10 cm) stricture is then opened in a longitudinal manner, encompassing the opening of the excised fistula. The defect is then closed as in the HM technique (Fig. 2). This technique confers the benefits of HM strictureplasty, as it is technically easy to perform with no significant tension on the suture line.4
MWN Strictureplasty
This type is suited for short segment strictures (<10 cm) in which there is dilatation of the proximal portion of the bowel. A Y-shaped longitudinal enterotomy is made across the stricture with the fork of the “Y” pointing toward the dilated portion. The defect is then closed in the HM fashion (Fig. 3). This technique finds favor due to the fact that it is technically easy to perform and reduces proximal dilatation of the bowel while conferring a gentle transition from dilated to nondilated bowel.4
Other variants of the HM technique include the double Heineke–Mikulicz strictureplasty described by Sasaki et al.5 where two HM strictureplasties are combined for two short strictures in tandem. Widening ileocolic strictureplasty is performed in an HM fashion for short strictures at the ileocecal region.6–8
Intermediate Procedures
Intermediate strictureplasty procedures have evolved from HM-like techniques to facilitate the management of stricturing CD in slightly longer segments of bowel (>10, <25 cm). This also encompasses short segment strictures separated by short segments (~5 cm) of normal bowel; however, the overall working length should preferably be less than 25 cm. These procedures include the Finney (FN) strictureplasty, Jaboulay procedure, combined HM and FN strictureplasty, modified FN strictureplasty, and ileocolic Finney strictureplasty (Table 1).
Finney Strictureplasty
This is one of the conventional techniques used to manage medium-sized strictures usually >10 and <25 cm.3,4,9 It entails folding the strictured segment in a “U”-shape manner, then creating a longitudinal enterotomy on the antimesenteric border. The anterior and posterior walls are closed in a continuous single or double-layer manner (Fig. 4). Finney strictureplasty results in the creation of a lateral diverticulum and subsequent functional bypass while relieving obstruction. The lateral diverticulum can result in luminal stasis and bacterial overgrowth and blind loop syndrome. A meta-analysis by Tichansky et al.25 showed a lower rate of recurrence and re-operation in cases with Finney strictureplasty when compared with those of the HM strictureplasty.
Finney strictureplasty. The strictured area is folded over itself, forming a “U” configuration. A single longitudinal enterotomy is closed in a “U” configuration. The opposed edges of the bowel are sutured together to create a blind pouch to overcome the stricture. Single- or double-layer absorbable or nonabsorbable sutures are used for this purpose
Jaboulay Strictureplasty
This technique was initially described back in the late nineteenth century by Mathieu Jaboulay. It initially was used to bypass a strictured pyloric segment complicated by peptic ulcer disease. This technique is suitable for medium-sized (>10 and <25 cm) strictures. With this technique, bowel length is spared; however, there is the creation of a lateral diverticulum with resulting blind loop and stasis in the strictured segment. Caution should be exercised when applying this technique to bypass long strictured segments of bowel because of the increased morbidity linked with blind loop, malnutrition, and malabsorption in an already nutritionally compromised patient (Fig. 5).2
Other variants of intermediate strictureplasty include the combined Heineke–Mikulicz and Finney strictureplasty technique described by Fazio and Tjandra10 where both techniques are combined to prevent significant angulation of the bowel. A modified variant of the Finney procedure by Selvaggi et al.11 and also the ileocolic Finney strictureplasty12,13 have also been described for use on medium-sized strictures.
Enteroenterostomies
Newer innovative techniques have been described over the recent years to facilitate the management of even longer strictured segments of bowel (>20 up to 90 cm) without the need for resection. These techniques are strongly considered for cases where there is extensive stricturing CD such that massive bowel resection would significantly increase the risk for short bowel syndrome.
The surgical techniques applied to these longer diseased segments fall under the category of enteroenterostomies. This technique was first published by Michelassi14 in the early 1990s.
Michelassi Strictureplasty
Michelassi14 proposed a novel technique of performing strictureplasties on significantly long strictured segments (>20 cm) or a long portion of bowel containing multiple short strictures in tandem, making the creation of multiple HM strictureplasties unsafe. This technique has been performed on segments as long as 90 cm.
Technical aspects of this procedure (Fig. 6) involve dividing the bowel and its mesentery in the midpoint of the strictured segment. The proximal and distal ends are then advanced side by side to each other. An outer interrupted suture line is created. A longitudinal enterotomy is then created. An inner row of running sutures is placed and continued anteriorly after making a Cornell stitch transition at the apex. The finished anterior suture line is reinforced with interrupted stitches.14,15
This technique appears favorable since it avoids the resection of large amount of bowel, relieves obstruction, and eludes the creation of blind loops as well as bypassed loops. Notwithstanding the obvious advantages, this technique inherently is difficult to perform and is even more so in instances where the mesentery is thickened and foreshortened.
Poggioli Strictureplasty
A modified form of Michelassi’s side-to-side isoperistaltic enteroenterostomy has been proposed and published by two groups: Poggioli et al.16 and Federici di Abriola et al.,17 respectively. These authors describe a technique whereby a long strictured segment (>20 cm) of bowel is plastied using a modification of the side-to-side isoperistaltic strictureplasty technique described by Michelassi.
The technique begins by severing the bowel and dividing the mesentery at the proximal junction of the stricture. The nondiseased bowel is then advanced over the strictured segment. A longitudinal enterotomy is made on both overlapping segments, and a side-to-side enteroenterostomy is then performed in the usual manner (Fig. 7).
The use of proximal, nondiseased bowel offers better laxity of the mesentery and better suture line integrity. However, it should be cautioned that this technique is challenging to perform and carries the inherent risk of a potential two-fold bowel loss should the repair fail or a complication arise.
Sasaki et al.18 describe a variant of Michelassi’s technique in which Heineke–Mikulicz strictureplasty is added to both ends of the strictureplasty. Likewise, another variant of the enteroenterostomy described by Hotokezaka et al.19 adds bowel resection to the strictureplasty. Side-to-side ileocolic strictureplasty7,20 has also been described and is best applied on medium-sized strictures.
To summarize all of the above 15 procedures, we generated Table 1 to highlight the definitions and recommended stricture length for each technique. We have come to appreciate that there is much overlap and similarity between these strictureplasty techniques; nonetheless, one can easily recognize disparities between them when they are classified into three main groups.
Discussion
Strictureplasty technique has been utilized increasingly over the past 30 years in the management of obstructing Crohn’s disease. Conventional techniques such as HM strictureplasty and Finney strictureplasty are the most widely reported methods in the literature. Modifications of these techniques have evolved over the years in an attempt to provide more options to patients and facilitate the possibility of preserving bowel length in a disease process known to have significant unavoidable recrudescence and need for reoperations.
Complications from strictureplasties in Crohn’s disease have been documented. In a meta-analysis by Yamamoto et al.,26 a group of 1,112 patients who underwent 3,259 strictureplasties was studied. Four percent of these patients had septic complications such as anastomotic leaks, fistula, and abscess formation. Almost half of these patients required a laparotomy for the sepsis. It was also noted that the strictureplasty site was involved in septic complications in about 78% of patients with sepsis. Overall, the perioperative complication rate reported by most authors spans from 0% to 57% and averages 13%.26–31
Data for procedure-specific recurrence rates are available only for a few strictureplasty techniques. In one study, Michelassi’s32 side-to-side isoperistaltic strictureplasty was shown to have a recurrence rate of 23%. This rate compares favorably with the 5-year recurrent rates of 28–41% for both the HM and Finney strictureplasties. Furthermore, in a meta-analysis by Tichansky et al.,25 506 patients were evaluated and they demonstrated lower morbidity rates with the HM strictureplasty technique when compared with the Finney strictureplasty cases. However, the HM technique was noted to have a higher recurrence rate of 32% and reoperative rate of 23% when compared with the Finney strictureplasty. Some authors have shown that fewer recurrences of disease occur at strictureplasty sites than resection sites.33 Site-specific recurrences as low as 4%20,34 have also been reported, but this finding contradicts results from a study35 from Japan in which 103 patients underwent 293 strictureplasties and they reported a 20% site-specific recurrence. Surgical recurrence is also an important outcome marker for strictureplasty in Crohn’s disease. Dietz et al.31 in a retrospective review of 314 patients who underwent 1,124 strictureplasty procedures reported an operative recurrence rate of 34% within a 7.5 years of follow-up period. In addition, some reports show no statistical difference in CD recurrence or surgical recurrence in patients who undergo strictureplasty versus those who undergo a resection.24,32,36–38 Taking this into consideration, one can see how performing a strictureplasty does not necessarily put a patient at a higher risk for recurrent disease when compared to the resection option. Therefore, it is beneficial to minimize bowel resection whenever possible.
Reports of the development of adenocarcinoma in the small bowel due to Crohn’s disease have been documented in a couple of case reports. This risk is even more concerning given the fact that the diseased bowel is conserved with strictureplasty. Some authors recommend tissue biopsies for frozen section in areas with suspicious features when performing a strictureplasty. Theoretically, it seems plausible that the relief of mechanical bowel obstruction with strictureplasty would reduce inflammatory indices of Crohn’s disease and thus decreases the risk for malignant transformation.38,39
Conclusion
The safety and efficacy of strictureplasty for Crohn’s disease have been supported by several reports.21,23,24,40,41 Various techniques of strictureplasty have undergone evolutionary change over the years to allow for the management of even longer strictured segments of bowel and more complicated strictures while minimizing the need for bowel resection. Data on procedure-specific outcomes on most of these techniques are still lacking. It makes it difficult to fully appraise these techniques in regards to their specific complication rates or recurrences. Nonetheless, it is imperative to recognize strictureplasty as an adjunct in the surgical armamentarium for the treatment of stricturing Crohn’s disease rather than as a complete replacement for a well-planned, limited resection should the need arise. The treating surgeon is now more equipped with options to manage these patients who otherwise would be treated solely with bowel resection and left with an unwarranted risk of developing short bowel syndrome due to the panintestinal and notably recrudescent nature of Crohn’s disease.
References
Katariya RN, Sood S, et al. Stricture-plasty for tubercular strictures of the gastro-intestinal tract. Br. J. Surg. 1977; 64: 496–498
Lee EC, Papaioannou N. Minimal surgery for chronic obstruction in patients with extensive or universal Crohn’s disease. Ann. R. Coll. Surg. Eng. 1982; 64: 229–233
Milsom JW. Strictureplasty and mechanical dilation in strictured Crohn’s disease. In: Michelassi F, Milsom JW (eds). Operative strategies in inflammatory bowel disease. New York: Springer; 1999:259–267
Gaetini A, DeSimone M, Resegotti A. Our experience with strictureplasty in the surgical treatment of Crohn’s disease. Hepato-gastroenterol , 1989; 36: 511–515
Sasaki I, et al. Extended strictureplasty for multiple short skipped strictures of Crohn’s disease. Dis. Colon Rectum, 1996; 39: 342–344
Tjandra JJ, Fazio VW. Strictureplasty for ileocolic anastomotic strictures in Crohn’s disease. Dis. Colon Rectum. 1993; 36: 1099–103
Taschieri AM, et al. Description of new “bowel-sparing” techniques for long strictures of Crohn’s disease. Am. J. Surg. 1997; 173: 509–512
Sampietro GM, et al. A prospective longitudinal study of nonconventional strictureplasty in Crohn’s disease. J. Am. Coll. Surg. 2004; 199: 8–22
Gordon PH and Nivatvongs S. Crohn’s disease. Principles and practice of surgery for the colon, rectum and anus, 3rd edition. St. Louis: Quality Medical; 1999:856–860.
Fazio VW, Tjandra JJ. Strictureplasty for Crohn’s disease with multiple long strictures. Dis. Colon Rectum, 1993; 36; 71–72
Selvaggi F. et al. A new type of strictureplasty for the treatment of multiple long stenosis in Crohn's disease. Inflamm Bowel Dis. 2007; 13: 641–642
Poggioli G. et al. Conservative surgical management of terminal ileitis; side-to-side enterocolic anastomosis. Dis. Colon Rectum. 1997; 40: 234–239.
Tonelli F, Fazi M, Di Martino C. Ileocecal strictureplasty for Crohn’s disease: long-term results and comparison with ileocecal resection. World J. Surg. 2010; 34:2860–2866
Michelassi F: Side-to-side isoperistaltic strictureplasty for multiple Crohn’s strictures. Dis Colon Rectum. 1996; 39: 345–349
Hurst RD, Michelassi F. Strictureplasty for Crohn’s disease: techniques and long-term results. World J. Surg. 1998; 22: 359–363
Poggioli G. et al. A new model of strictureplasty for multiple and long stenoses in Crohn’s ileitis: side-to-side diseased to disease-free anastomosis. Dis. Colon Rectum. 2003; 46: 127–130
di Abriola FG, De Angelis P, Dall’Oglio L, Di Lorenzo M. Strictureplasty: an alternative approach in long segment bowel stenosis Crohn’s disease. J. Pediatr. Surg. 2003; 38: 814–818
Sasaki I. et al. New reconstructive procedure after intestinal resection for Crohn’s Disease: modified side-to-side isoperistaltic anastomosis with double Heineke–Mikulicz procedure. Dis. Colon Rectum 2004; 47: 940–943
Hotokezaka M, Ikeda T, Uchiyama S, Hayakawa S, Tsuchiya K, Chijiiwa K. Side-to-side-to-end strictureplasty for Crohn’s disease. Dis. Colon Rectum. 2009; 52: 1882–1886
Tonelli F et al. Strictureplasty in Crohn’s disease: surgical option. Dis. Colon Rectum. 2000; 43: 920–926
P. Roy and D. Kumar. Strictureplasty: British Journal of Surgery 2004; 91: 1428–1437
Laureti S. and Fazio VW. Obstruction in Crohn’s disease: strictureplasty versus resection. Current Treatment Options in Gastroenterology 2000; 3: 191–201.
Jobanputra S. and Weiss E. Strictureplasty. Clin Colon Rectal Surg. 2007; 20: 294–302.
Roy P, Kumar D. Strictureplasty for active Crohn’s disease. Int J Colorectal Dis, 2006; 21: 427–432
Tichansky D, Cagir B, Yoo E, Marcus S, Fry R. Strictureplasty for Crohn’s disease: meta-analysis. Dis Colon Rectum 2000; 43: 911–919.
Yamamoto T, Fazio V, Tekkis P. Safety and efficacy of strictureplasty for Crohn’s disease: a systemic review and meta-analysis. Dis Col Rectum, 2007; 50: 1968–1986.
Spencer M, Nelson H, Wolff B, Dozois R. Strictureplasty for obstructive Crohn’s disease: the Mayo experience. Mayo Clin Proc, 1994; 69: 33–36.
Scarpa M, Ruffolo C, et al. Intestinal surgery for Crohn’s disease: predictors of recovery, quality of life, and costs. J Gastrointest Surg, 2009; 13: 2128–2135
Binion D, Theriot K, Shidham S, et al. Clinical factors contributing to rapid reoperation for Crohn’s disease patients undergoing resection and/or strictureplasty. J Gastrointest Surg, 2007; 11: 1692–1698
Froehlich F, Juillerat P et al. Fibrostenotic Crohn’s disease. Digestion 2007;76: 113–115
Dietz D, Laureti S, Fazio V et al. Safety and long-term efficacy of strictureplasty in 314 patients with obstructing small bowel Crohn’s disease. J Am Coll Surg. 2001; 192: 330–337
Baba S and Nakai K. Strictureplasty for Crohn’s disease in Japan. J. Gastroenterol, 1995; 30: 135–138
Fichera A, et al. Patterns and operative treatment of recurrent Crohn’s disease: a prospective longitudinal study. J. Surg. 2006; 140:649–654
T. Yamamoto and M. Keighley. Long-term results of strictureplasty without synchronous resection for jejunoileal Crohn’s disease. Scand J Gastroenterology 1999; 2: 180–184.
Futami K, Arima S. Role of strictureplasty in surgical treatment of Crohn’s disease. J. Gastroenterol 2005; 40: 35–39.
Reese G, Purkayastha S, et al. Strictureplasty vs. resection in small bowel Crohn’s disease: an evaluation of short-term outcomes and recurrence. Meta-analysis. Colorectal Disease, 2006; 9: 686–694.
Fernhead N, Chowdhury R, et al. Long-term follow-up of strictureplasty for Crohn’s disease. British Journal of Surgery, 2006; 93: 475–482.
Broering D, et al. Quality of life after surgical therapy of small bowel stenosis in Crohn’s disease. Digestive Surgery, 2001; 18: 124–130.
Dasari B, Maxwell R, Gardiner K. Assessment of complications following strictureplasty for small bowel Crohn’s disease. Irish Journal of Medical Science, 2009; 179: 201-205.
Tonelli F, Fedi M, Paroli M, Fazi M. Indications and results of side-to-side isoperistaltic strictureplasty in Crohn’s disease. Dis Colon Rectum, 2004; 47: 494–501
Uchino M, Ikeuchi H, et al. Long-term efficacy of strictureplasty for Crohn’s disease. Surgery Today, 2010; 40: 949–953
Acknowledgments
The authors would like to thank Ms. Elizabeth Crosby for her help.
Author information
Authors and Affiliations
Corresponding author
Additional information
This manuscript has not been presented or planned to be presented as a poster or on a podium.
Rights and permissions
About this article
Cite this article
Ambe, R., Campbell, L. & Cagir, B. A Comprehensive Review of Strictureplasty Techniques in Crohn’s Disease: Types, Indications, Comparisons, and Safety. J Gastrointest Surg 16, 209–217 (2012). https://doi.org/10.1007/s11605-011-1651-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1651-2