Abstract
Background
Single-incision laparoscopic colorectal surgery is an emerging modality. We incorporated this technique as an alternative to hand-assisted laparoscopic surgery. We investigated intraoperative and short-term outcomes following single-incision laparoscopic colectomy compared with hand-assisted laparoscopic colectomy.
Methods
Between July and November 2009, single-incision colorectal procedures were performed and matched to hand-assisted procedures based on five criteria: gender, age, body mass index, pathology, and type of procedure. Demographic, intraoperative, and postoperative data were assessed.
Results
Twenty-four pairs of patients with a mean age of 55.1 years and mean body mass index of 28.5 kg/m2 were matched. The majority of cases (79.2%) were right hemicolectomies. The ranges of incision length were 2–6 cm (single incision) and 5–11 cm (hand-assisted). Mean operating time was significantly longer for single-incision procedures (143.2 min) compared with hand-assisted procedures (112.8 min), p < 0.0004. There was no significant difference in the groups regarding conversions or intraoperative complications (p < 0.083 and p < 1.0, respectively). Mean length of stay for the single-incision approach (2.7 days) was significantly shorter compared with the hand-assisted approach (3.3 days), p < 0.02.
Conclusion
Single-incision laparoscopic colectomy is a safe and feasible alternative to hand-assisted laparoscopic surgery. Although the technique required longer operative time, it resulted in smaller incision size and significantly shorter length of hospitalization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Single-incision laparoscopic surgery is an emerging modality, first reported for gynecologic surgery in 19921 and 7 years later for general surgery.2 Slow to achieve wide-spread acceptance, this technique has recently experienced resurgence in its use, including increasing application for minimally invasive colorectal surgery. Single-incision laparoscopic colectomy (SILC) has been described through case reports and small case series.3–7 Considered safe and feasible,8,9 the single-incision technique results in improved cosmesis with the potential for decreased pain and fewer incisional hernias.4,7,10,11
Hand-assisted laparoscopic surgery (HALS) was first described in 1996 for colorectal surgery12 and was initially used as a bridge to facilitate completion of a minimally invasive procedure for surgeons with limited laparoscopic experience. This technique allows the surgeon to use tactile feedback to identify various structures in order to complete the operation in a shorter period of time13,14 and with lower conversion rate compared with conventional laparoscopic surgery (CLS).15,16 Hand-assisted laparoscopic surgery has since gained widespread acceptance, as it has resulted in reduced operative times yet comparable short-term benefits compared with CLS.13–16
Single-incision laparoscopic colectomy has yet to be compared with other minimally invasive modalities to evaluate its potential benefits and limitations. The purpose of this study was to assess whether the proven short-term benefits and outcomes of minimally invasive technique are maintained with the SILC approach. We report the first known case-matched series of SILC compared with HALS colectomy in regards to safety, efficacy, and patient outcomes.
Material and Methods
This study was approved by the Institutional Review Board. Twenty-four single-incision laparoscopic colorectal procedures performed between July and November 2009 were matched to 24 hand-assisted laparoscopic colorectal procedures based on five matching criteria: gender, age, body mass index (BMI), pathology (benign or malignant), and type of procedure (right hemicolectomy (RH), total colectomy (TC), or anterior rectosigmoidectomy (AR)). Demographic data including age, gender, BMI, and American Society of Anesthesiologists (ASA) score were collected. Intraoperative parameters including umbilical incision length (IL), estimated blood loss (EBL), total operative time (OT), and lymph node extraction (malignant cases only) were tabulated and analyzed. Single-incision laparoscopic colectomies that required conversion were analyzed within the SILC group. Postoperative outcomes including length of hospital stay (LOS), 30-day complications, and perioperative mortality were assessed.
Surgical Technique
Each procedure was performed by one of two board-certified colorectal surgeons (E.M.H. and T.B.P.) after obtaining informed consent. The SILS™ Port Multiple Instrument Access Port (n = 13, Covidien, Mansfield, MA), GelPOINT® (n = 9, Applied Medical, Rancho Santa Margarita, CA), or GelPort® (n = 2, Applied Medical) was utilized for the SILC procedures. The GelPort® (Applied Medical) was utilized for all HALS procedures. Standard non-articulating laparoscopic instruments were utilized for all procedures.
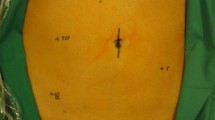
Our SILC technique has previously been reported.9,17 Patients undergoing RH were placed in the supine position. Patients undergoing AR or TC were placed in the lithotomy position. The single-incision device was inserted through a 2.5 cm transumbilical incision (Fig. 1a). The direction of dissection (medial-to-lateral or lateral-to-medial) was performed at the discretion of the operating surgeon. For each patient, the specimen was extracted through the transumbilical single incision after placement of an Alexis® wound retractor (Applied Medical, Rancho Santa Margarita, CA). Resection was achieved following extracorporealization. The anastomosis for RH was performed extracorporeally while the anastomosis for AR or TC was performed intracorporeally with the use of a 29 mm EEA stapler (Ethicon Endo-Surgery, Inc., Cincinnati, OH).
a Single-incision laparoscopic colectomy: three 5 mm trocars placed through transumbilical single-access port. b Hand-assisted laparoscopic anterior rectosigmoidectomy or total colectomy: three 5 mm trocars placed through abdomen, a 12 mm trocar and hand placed through hand-assist device. c Hand-assisted laparoscopic right hemicolectomy: two 5 mm trocars placed through the abdomen, one 12 mm trocar and hand placed through hand-assist device
Our HALS approach began with insertion of a laparoscopic port for initial entry into the peritoneum. Once pneumoperitoneum was achieved, an umbilical or Pfannenstiel incision was made, through which the GelPort® hand-assist device was placed. The initial incision for the hand port was 5 cm in length and was extended up to 8 cm as necessary depending on the surgeon’s hand size and the depth of the patient’s abdominal wall. In addition to the hand-assist device, two 5 mm trocars were utilized for RH (Fig. 1c) and three 5 mm trocars were placed for AR and TC (Fig. 1b). A 12 mm trocar was placed through the hand-assist device in all cases. The operation proceeded in a similar approach as the SILC procedure.
Statistical Analysis
Data analysis was performed using Intercooled Stata version 9.2 (Stata Corporation, College Station, TX). Categorical data, summarized as percentages, were compared with the chi-square test. For quantitative data, paired two-tailed Student’s t test was performed with significance level of alpha = 0.05. Results are presented as mean ± standard deviation.
Results
Twenty-four SILC and HALS cases each were paired together based on five matching criteria: gender (n = 12 male, p < 1.0), age (54.1 ± 8.6 years in the SILC group and 56.0 ± 11.1 years in the HALS group, p < 0.36), BMI (28.5 ± 7.2 kg/m2 in the SILC group and 28.5 ± 6.0 kg/m2 in the HALS group, p < 0.95), pathology (n = 15 (62.5%) cases for benign disease and n = 9 (37.5%) cases for malignant disease, p < 1.0), and surgical procedure (n = 19 (79.2%) RH, n = 3 (12.5%) AR, and n = 2 (8.3%) TC, p < 1.0), see Table 1. Ten patients (41.7%) in the SILC group and 12 patients (50%) in the HALS group had prior abdominal surgery (p < 0.49). The median ASA score for both the SILC and HALS groups was 2.
The mean IL was 3.3 ± 1.1 cm in the SILC group with a range of 2–6 cm (based on n = 21 patients for whom IL was recorded). The mean incision length for the HALS group was 6.6 ± 2.1 cm with a range of 5–11 cm (based on n = 17 patients for whom IL was recorded) and this was significantly greater than that of the SILC group, p < 0.00001. The EBL in the SILC and HALS groups was 62.5 ± 37.6 mL and 90.6 ± 60.6 mL, respectively (p < 0.06). The mean OT for the SILC group (143.2 ± 37.2 min) was significantly longer compared with that of the HALS group (112.8 ± 44.8 min), p < 0.0004. There were no conversions to open colectomy in either group. Three patients in the SILC group (12.5%) required conversion to another MIS technique (two HALS and one multiport laparoscopy) for completion of the procedure while no conversions were required for the HALS cases, p < 0.083. No intraoperative complications were encountered in either group. For the malignant cases, LN extraction in the SILC and HALS cases was 24.6 ± 12.3 and 18.6 ± 5.7, respectively (p < 0.22), see Table 2. There were no significant differences between surgeons with respect to EBL, OT, and intraoperative complication rate.
The LOS in the SILC group was significantly shorter compared with that in the HALS group (2.7 ± 0.8 days compared with 3.3 ± 1.1 days, p < 0.02). Two postoperative complications (8.3%) were encountered in the SILC group (anastomotic bleeding and wound infection) and none were encountered in the HALS group, p < 0.15. No patients required reoperative intervention. One perioperative death was encountered in a patient following palliative SILC right hemicolectomy as a result of complications from metastatic disease. There were no significant differences between surgeons with respect to LOS, postoperative complication rate, and perioperative mortality.
Discussion
Single-incision laparoscopic technique was first reported in the gynecologic surgical literature in 1992 for a supracervical hysterectomy with bilateral salpingo-oopherectomy1 and in the general surgical literature in 1999 for a single-incision cholecystectomy.2 In the last 2 years, however, advancements in instrumentation and port devices have revived interest in this approach. The adaptation of the single-incision approach has recently emerged for colorectal surgery in the form of case reports4,7,10,11,18 and small case series.8 These reports have indicated improved cosmesis as the primary benefit,4,7,8,10,11 with additional benefits and potential limitations having yet to be elicited. We previously demonstrated safety and feasibility of the technique in a cohort of unselected patients undergoing single-incision right colectomy.9 In order to further investigate outcomes, we undertook a matched-case analysis comparing the single-incision approach with hand-assisted laparoscopic surgery.
Hand-assisted laparoscopic surgery represents a modification of conventional laparoscopic surgery, designed to help overcome several of the technical challenges of CLS.13,14,16 HALS allows surgeons to use a hand for dissection or retraction, thereby providing direct tactile feedback during a procedure. In addition, it allows surgeons to maintain a minimally invasive approach and retain the short-term benefits of laparoscopic surgery, including short length of stay, small incision, and reduced perioperative complications.14,16 Compared with open surgery, the smaller incision used for HALS may contribute to fewer incisional hernias and faster recovery.13
In this series, the incision length for patients in the SILC group was significantly smaller in comparison to the incision length for patients in the HALS group (p < 0.00001). In all SILC cases, the initial incision length was 2.5 cm. In 16 patients (76.2%), the incision was extended by 1 cm or less at the time of specimen extraction. In five cases (23.8%), the IL was extended by 1–2.5 cm beyond the initial incision, for extraction of a bulky specimen (n = 4) or exchange of the SILS™ device for a GelPort® due to dislodgement (n = 1) in a patient with large abdominal girth. Other reports have described similar incision lengths, ranging from 2–3.5 following the SILC procedure.4,7,8,10,11,18 Although it may be expected that the absence of multiple trocar-site incisions and an overall smaller extraction-site incision following SILC would result in improved cosmesis, we did not directly assess the patients’ perceptions of their incisions. Establishing a validated questionnaire to address this outcomes measure will be an important consideration when comparing SILC to established MIS procedures. In addition to the known benefit of improved cosmesis, we believe that a smaller single incision provides the potential for diminished postoperative pain.
On average, the SILC technique required 30 min longer to complete compared with the HALS technique. We did not utilize flexible (articulating) instruments as they were not readily available, would have added additional cost, and were not required to complete the procedure. With more complex procedures and advances in technology, utilization of such instrumentation may be warranted. Since the surgeons in this series only recently adopted the SILC technique, it is plausible that the SILC OT may diminish with increased experience. It is further noted that the HALS cases in this study were completed after each surgeon had gained competence with the technique. In addition, previous studies have found HALS to require shorter OT compared with CLS.15 Thus, one may expect similar findings when comparing HALS to SILC.
For each technique, the postoperative complication rate and perioperative mortality rate were low. For one patient in the SILC group, a postoperative flexible sigmoidoscopy revealed bleeding at the ileorectal anastomosis and an endoscopic clip (Olympus, Center Valley, PA) was placed across the anastomosis at the site of bleeding. A second patient in the SILC group experienced a wound infection that was managed with local wound care. No postoperative complications were encountered in the HALS group. A single postoperative mortality occurred in the SILC group - a 52 year-old female with extensive pulmonary and hepatic metastatic disease who underwent a palliative resection for cecal obstruction. Her operation was completed in 100 min without any adverse events; however, her postoperative course was complicated by respiratory failure, for which supportive care was voluntarily withdrawn.
We analyzed the pathology results for the nine patients in each group (37.5%) with malignant disease to assess the adequacy of the oncologic resections. Neither technique hindered the ability to extract an adequate number of lymph nodes, as evidenced by a median lymph node extraction of 19 in the SILC group and 17 in the HALS group. These values exceeded the median values of 10 and 12 reported for laparoscopic technique in national randomized studies comparing open to laparoscopic approach for colectomy19–21. To further enumerate additional parameters such as single-incision site (“port-site”) recurrence, long-term follow up will be required.
Mean length of hospital stay following SILC and HALS was 2.7 and 3.3 days, respectively (p < 0.02). Although statistically significant, we did not evaluate whether this reduction in LOS resulted in an economic benefit, an important consideration for future studies, following the single-incision technique. Both groups were placed on identical postoperative recovery pathways, which included early feeding and ambulation, absence of a nasogastric tube, early removal of Foley catheter, and additional quality measures. Patients were discharged following evidence of bowel activity, either passage of flatus or bowel movements, and absence of abdominal strain or distention. The significant difference between the two groups may be attributed to diminished pain from decreased trauma and incision size with SILC, leading to earlier return of bowel function. In reports comparing HALS to CLS, patients were likely to experience more pain14–16 and early postoperative bowel obstruction14 with the HALS technique. It should be noted, however, that these parameters were not primary outcomes of this study.
Conversion was required in three SILC cases. In one patient, lengthening of the incision for specimen extraction resulted in inability to reestablish pneumoperitoneum with the SILS™ device, and thus the GelPort® was introduced to complete the procedure with hand-assisted technique. The second conversion to HALS was required for additional mobilization of the transverse colon for a tension-free ileocolic anastomosis. In the third conversion, two auxiliary ports were placed outside of the single incision to facilitate primary suture closure of colorectal anastomosis following a positive air insufflation test. Conversion to open technique was not required for these three cases, which reflects the ability to maintain a minimally invasive platform and avoid the negative outcomes associated with open conversions, such as prolonged LOS22 and increased postoperative morbidity.23
Many of the SILC cases involved lysis of adhesions before proceeding to mobilization of the colon and these procedures were able to be completed safely through a single incision. In a study of 430 CLS colorectal procedures, adhesions were determined to be a specific indication for conversion, accounting for 30% of conversions to open technique.24 Given that 50% of patients undergoing HALS and 41.7% of patients undergoing SILC had undergone previous abdominal surgery, the results of this study indicate that surgeons should not be dissuaded from using either minimally invasive approach to perform colectomy in such patients.
Conclusion
Single-incision laparoscopic colectomy can be utilized for surgical resection of benign or malignant disease of the colon. When compared with hand-assisted laparoscopic surgical technique, single-incision laparoscopic colectomy resulted in smaller incision length and shorter length of hospital stay at the expense of longer operative time. Furthermore, single-incision procedures that prove to be complex can be salvaged with hand-assisted or multiport technique rather than conversion to an open approach. With increased adoption of the single-incision technique, shorter operative times and fewer conversions may be realized.
Abbreviations
- AR:
-
Anterior rectosigmoidectomy
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- EBL:
-
Estimated blood loss
- HALS:
-
Hand-assisted laparoscopic surgery
- IL:
-
Incision length
- LN:
-
Lymph node
- LOS:
-
Length of hospital stay
- OT:
-
Total operative time
- RH:
-
Right hemicolectomy
- SILC:
-
Single-incision laparoscopic colectomy
- TC:
-
Total colectomy
References
Pelosi MA, Pelosi MA, 3rd: Laparoscopic supracervical hysterectomy using a single-umbilical puncture (mini-laparoscopy). J Reprod Med 1992;37:777–784.
Bresadola F, Pasqualucci A, Donini A, Chiarandini P, Anania G, Terrosu G, Sistu MA, Pasetto A: Elective transumbilical compared with standard laparoscopic cholecystectomy. Eur J Surg 1999;165:29–34.
Brunner W, Schirnhofer J, Waldstein-Wartenberg N, Frass R, Weiss H Single incision laparoscopic sigmoid colon resections without visible scar: A novel technique. Colorectal Dis 2010;12:66–70
Bucher P, Pugin F, Morel P: Single port access laparoscopic right hemicolectomy. Int J Colorectal Dis 2008;23:1013–1016.
Leroy J, Cahill RA, Asakuma M, Dallemagne B, Marescaux J: Single-access laparoscopic sigmoidectomy as definitive surgical management of prior diverticulitis in a human patient. Arch Surg 2009;144:173–179; discussion 179.
Merchant AM, Lin E: Single-incision laparoscopic right hemicolectomy for a colon mass. Dis Colon Rectum 2009;52:1021–1024.
Remzi FH, Kirat HT, Kaouk JH, Geisler DP: Single-port laparoscopy in colorectal surgery. Colorectal Dis 2008;10:823–826.
Chambers W, Bicsak M, Lamparelli M, Dixon A: Single-incision laparoscopic surgery (sils) in complex colorectal surgery: A technique offering potential and not just cosmesis. Colorectal Dis 2009
Ramos-Valadez DI, Patel CB, Ragupathi M, Bartley Pickron T, Haas EM: Single-incision laparoscopic right hemicolectomy: Safety and feasibility in a series of consecutive cases. Surg Endosc 2010
Bucher P, Pugin F, Morel P: Transumbilical single incision laparoscopic sigmoidectomy for benign disease. Colorectal Dis 2010;12:61–65.
Bucher P, Pugin F, Morel P: Single-port access laparoscopic radical left colectomy in humans. Dis Colon Rectum 2009;52:1797–1801.
Bemelman WA, Ringers J, Meijer DW, de Wit CW, Bannenberg JJ: Laparoscopic-assisted colectomy with the dexterity pneumo sleeve. Dis Colon Rectum 1996;39:S59–61.
Aalbers AG, Doeksen A, MI VANBH, Bemelman WA: Hand-assisted laparoscopic versus open approach in colorectal surgery: A systematic review. Colorectal Dis 2009;12:287-295
Cima RR, Pattana-arun J, Larson DW, Dozois EJ, Wolff BG, Pemberton JH: Experience with 969 minimal access colectomies: The role of hand-assisted laparoscopy in expanding minimally invasive surgery for complex colectomies. J Am Coll Surg 2008;206:946–950; discussion 950–942.
Aalbers AG, Biere SS, van Berge Henegouwen MI, Bemelman WA: Hand-assisted or laparoscopic-assisted approach in colorectal surgery: A systematic review and meta-analysis. Surg Endosc 2008;22:1769–1780.
Marcello PW, Fleshman JW, Milsom JW, Read TE, Arnell TD, Birnbaum EH, Feingold DL, Lee SW, Mutch MG, Sonoda T, Yan Y, Whelan RL: Hand-assisted laparoscopic vs. Laparoscopic colorectal surgery: A multicenter, prospective, randomized trial. Dis Colon Rectum 2008;51:818–826; discussion 826–818.
Patel CB, Ramos-Valadez DI, Ragupathi M, Haas EM: Single incision laparoscopic-assisted right hemicolectomy technique: Application for a mass of the ascending colon (with video). Surgical Laparoscopy Endoscopy Percutaneous Techniques 2010
Remzi FH, Kirat HT, Geisler DP: Laparoscopic single-port colectomy for sigmoid cancer. Tech Coloproctol 2009
Clinical Outcomes of Surgical Therapy Study Group. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med 2004;350:2050–2059.
Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM: Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (mrc clasicc trial): Multicentre, randomised controlled trial. Lancet 2005;365:1718–1726.
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM: Laparoscopic surgery versus open surgery for colon cancer: Short-term outcomes of a randomised trial. Lancet Oncol 2005;6:477–484.
Gonzalez R, Smith CD, Mason E, Duncan T, Wilson R, Miller J, Ramshaw BJ: Consequences of conversion in laparoscopic colorectal surgery. Dis Colon Rectum 2006;49:197–204.
Rottoli M, Bona S, Rosati R, Elmore U, Bianchi PP, Spinelli A, Bartolucci C, Montorsi M: Laparoscopic rectal resection for cancer: Effects of conversion on short-term outcome and survival. Ann Surg Oncol 2009;16:1279–1286.
Casillas S, Delaney CP, Senagore AJ, Brady K, Fazio VW: Does conversion of a laparoscopic colectomy adversely affect patient outcome? Dis Colon Rectum 2004;47:1680–1685.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gandhi, D.P., Ragupathi, M., Patel, C.B. et al. Single-Incision Versus Hand-Assisted Laparoscopic Colectomy: A Case-Matched Series. J Gastrointest Surg 14, 1875–1880 (2010). https://doi.org/10.1007/s11605-010-1355-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-010-1355-z