Abstract
Introduction
Hand-assisted laparoscopic surgery (HALS) is often used in procedures too complex for completely minimally invasive approaches. However, there are concerns for whether this hybrid approach abrogates perioperative benefits of the completely minimally invasive technique.
Methods
We queried the 2012–2013 National Surgery Quality Improvement Program for adults undergoing elective HALS or open colectomy (OC). After propensity matching, short-term outcomes were compared. Subset analysis was performed for segmental resections. Multivariate analysis was used to determine predictors of utilizing either approach.
Results
This query included 8791 patients (OC 2707, HALS 6084). Predictors of HALS included male sex (OR 1.17, p = 0.006), increasing BMI (OR 1.01, p = 0.02), benign indication (OR 1.48, p < 0.001), and total abdominal colectomy (OR 10.39, p < 0.001). Younger age, black race, ASA class ≥3, inflammatory bowel disease, and low pelvic anastomosis were predictive of OC (all p < 0.05). HALS demonstrated reduced overall complications (p < 0.001), wound complications (p < 0.001), anastomotic leak (p = 0.014), transfusion (p < 0.001), postoperative ileus (p < 0.001), length of stay (p < 0.001), and readmission (p < 0.001) without increased operative time. For segmental resection, HALS demonstrated reduced overall complications, wound complications, respiratory complications, postoperative ileus, anastomotic leak, transfusion, length of stay, and readmissions (all p < 0.05).
Conclusions
Compared to OC, HALS demonstrates improved perioperative outcomes without increased operative time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopic approaches to colorectal surgery have been demonstrated to be technically feasible and in adherence with oncologic principles.1 However, the application of laparoscopy to colon resections has been hampered by concerns over heightened procedural complexity, steep learning curves, lack of tactile feedback, and difficulties in mobilization, all resulting in longer operating times compared to the open approach.2 Hand-assisted laparoscopic surgery (HALS) has been touted as a method to bridge the divide between open and laparoscopic surgery for learners and in difficult operative settings. Technological advances for HALS such as sleeveless devices allow for the maintenance of pneumoperitoneum while accommodating a larger incision and multiple hand exchanges, enabling more widespread application of the approach.3
There is hope that HALS can provide the benefits of the open approach without the burdens of the laparoscopic technique in the setting of complex cases where minimally invasive approaches may be too difficult. Several small randomized control trials and single-center experiences have demonstrated that use of HALS resulted in improved outcomes including lower intraoperative blood loss, decreased time to return of bowel function, decreased use of analgesics, and shorter hospital length of stay.4 – 8 For the majority of these studies, operative times were longer in HALS compared to open resections.
The original studies evaluating this procedure were carried out in academic centers, which may not accurately reflect the conditions of community hospitals. Thus, it is unclear whether the benefits seen in these high-volume centers would persist in a broader application of the technique. Given the variance of practice between institutions, it is unclear if the benefits seen in academic centers are applicable on a national scale. Therefore, the objective of this study was to utilize a large national surgical outcomes database to compare perioperative outcomes between HALS and open colorectal surgery on a population level.
Methods
Data Source
The American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) is a prospectively maintained database which collects information on operative approaches and 30-day patient outcomes. The combined NSQIP Participant Use Data File for 2012–2013 was selected due to availability of data regarding surgical approach.
Study Design
The Duke University Institutional Review Board approved this retrospective analysis of the NSQIP database. Adult patients were identified who had undergone elective open or hand-assisted laparoscopic colectomy for both benign and malignant indications. These results were filtered to include subjects with Current Procedural Terminology (CPT) codes: 44140, 44145, 44160, 44204, 44205, 44207, and 44210. Subjects who had received preoperative steroids or chemotherapy, had ostomies created during the procedure, or had laparoscopic converted to open procedures were excluded.
Statistical Analysis
Because there were possible non-random differences between the patients selected to receive HALS and open colectomies, we developed propensity scores, defined as the conditional probability of receiving a HALS colectomy. Propensity scores were based on the following variables: age, sex, race, BMI, indication (neoplastic, benign, IBD), operative year, American Society of Anesthesiologists (ASA) classification, bowel prep status, and extent of surgery. Patients were then matched using a 1:1 nearest neighbor method. The primary endpoints were 30-day postoperative mortality and overall complication rates. Secondary endpoints were individual 30-day complications as defined by the NSQIP database. These include wound complications, cardiac complications, respiratory complications, renal complications, venous thromboembolism, urinary tract infection, postoperative ileus, anastomotic leak, bleeding, postoperative sepsis, need for reoperation, length of stay, readmission, and mortality. A subset analysis was performed in those who received segmental colectomies only in order to eliminate bias from higher-complexity operations. Multivariate logistic regression modeling was used to determine predictors of utilizing either operative approach. A p value of <0.05 was considered statistically significant. All statistical analysis was performed using R (The R Foundation for Statistical Computing, version 3.0 2, Vienna, Austria).
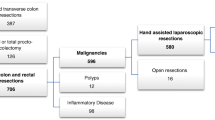
Results
In total, 8791 patients met the study criteria. Of these, 2707 (30.8%) patients received planned open colectomies and 6084 (69.2%) received HALS. For all patients, the median age was 63 (IQR 53, 72) and the median BMI was 27.8 (IQR 24.3, 32.3). Baseline characteristics and unadjusted outcomes between open versus HALS are shown in Table 1. Compared with open resections, patients who received HALS were more likely to be male, younger, white, and have benign disease. In unadjusted analysis, HALS was associated with a lower rate of overall complications, specifically wound complications (15.1 versus 8.6%, p < 0.001), urinary tract infection (2.9 versus 1.9%, p = 0.003), VTE complications (1.7 versus 1.0%, p < 0.001), respiratory complications (3.9 versus 1.9%, p < 0.001), renal complications (1.4 versus 0.6%, p < 0.001), anastomotic leak (4.6 versus 3.1%, p < 0.001), postoperative ileus (17.7 versus 8.6%, p < 0.001), need for blood transfusion (12.2 versus 4.4%, p < 0.001), and septic complications (5.4 versus 2.6%, p < 0.001). HALS was also associated with a shorter length of stay (median 6 days versus 4 HALS, p < 0.001) and lower reoperation (5.8 versus 3.8%, p < 0.001) and readmission rates (11.1 versus 7.8%, p < 0.001).
After matching for clinical, disease, and treatment factors, HALS was associated with lower rates of overall complications (13.6 versus 21.5%, p < 0.001), wound complications (8.8 versus 13.8%, p < 0.001), anastomotic leak (3.1 versus 4.7%, p = 0.014), transfusion requirement (5.0 versus 10.7%, p < 0.001), postoperative ileus (8.8 versus 18.0%, p < 0.001), length of stay (median 4 versus 6 days, p < 0.001), and readmissions (6.9 versus 11.4%, p < 0.001), without requiring longer operative time (median 148 versus 150 min, p = 0.111) (Table 2). Thirty-day postoperative mortality and need for operation were not different between HALS and open resection after matching.
When examining those that received segmental resection only, as depicted in Table 3, HALS was still associated with improved rate of overall complications, wound complications, respiratory complications, postoperative ileus, anastomotic leak, transfusion requirement, length of stay, and readmissions (all p < 0.05). Additionally, there was a slight decrease in operative time associated with segmental HALS (median 137 versus 141 min, p = 0.038).
Independent predictors of utilizing HALS include male sex (OR 1.17, p = 0.006), increasing BMI (OR 1.01, p = 0.02), benign indications for surgery other than inflammatory bowel disease (IBD) (OR 1.48, p < 0.001), and intention to perform total abdominal colectomy (OR 10.39, p < 0.001), as depicted in Table 4. Younger age, black race, ASA class ≥3, inflammatory bowel disease, and surgery requiring low pelvic anastomosis were predictive of open surgery (all p < 0.05).
Discussion
Our results demonstrate that the utilization of HALS is associated with fewer postoperative complications than in patients treated with open colectomy. In this study, we found that HALS provides a significant reduction in several postoperative complications including wound complications, respiratory complications, postoperative ileus, and anastomotic leak. In addition to these benefits, using HALS did not increase operative time. These combined benefits challenge previously held concerns surrounding the use of HALS over open colectomy in cases too complex for minimally invasive approach and instead, support the use of HALS for instruction of trainees as well as in difficult cases. HALS and open techniques both mobilize the colon from a lateral to medial direction, as opposed to the straight laparoscopic technique in which the approach is medial to lateral.8 This similarity facilitates learning and execution of the approach. Given the reduced complications with HALS use compared to open colectomy and conversely, the worsened outcomes following conversion to open surgery, surgeons may consider converting to HALS before open surgery following attempted laparoscopic dissection.9 , 10
Our study is unique in that we have used propensity matching to evaluate differences between operative cohorts. Benlice et al. have also recently reviewed the 2012–2013 datasets of NSQIP to analyze HALS and open colectomy patients.11 Their study identified patients undergoing elective open and laparoscopic colectomy. Similar to our analysis, they identified significantly higher rates of superficial surgical site infection, length of stay, and postoperative ileus following open colectomy compared to the minimally invasive approach. However, their findings demonstrated a significant difference in operative time between the two groups. We believe that their exclusion criteria did not appropriately control for the complexity of procedures, as it did not exclude patients who underwent ostomy creation or conversion from HALS to open. These selection criteria likely distort the operative times observed in their analysis, negating a strong benefit of HALS. Additionally, this study did not examine factors influencing surgeon selection of approach between HALS and open. This information may help to better select patients suitable for this approach.
There has been a debate as to whether HALS approaches should be the standard therapy in selected cases. Our data identify that HALS approaches are more likely to be used in male patients, likely due to the anatomical considerations of a narrow pelvis being more amenable to laparoscopic compared to open surgery. Patients with higher BMI are similarly more likely to undergo HALS colectomy, likely also due to anatomical considerations and a higher overall risk of wound complications in this patient population. Patients undergoing total colectomies were more likely to undergo HALS, as Marcello postulated in his study, because HALS could allow for more flexibility in the handling of the transverse mesocolon and omentum especially in cases with significant adhesions, such as IBD patients.12 However, our data show that colectomies performed for IBD were more likely to be performed open than those for other indications. The 1:1 propensity matching carried out in the current study attempts to account for the differences in the baseline characteristics of the patients receiving HALS and open colectomies. However, there are other factors which play a role in surgical decision-making which are not captured by the NSQIP dataset, and this selection bias cannot be fully accounted for in this study, or by any other NSQIP analysis.
Patients with higher ASA class were preferentially selected to undergo open colectomy, likely due to the concern that they would not tolerate the insufflation necessary for laparoscopic surgery. However, these patients may have also received open colectomies due to concern that they would not tolerate the prolonged operations historically associated with laparoscopic approaches. The current study demonstrates that operative times are equivalent which may harken a shift in practice toward HALS or laparoscopic approaches in these populations. Though the perceived increased cost of equipment to perform hand-assisted laparoscopic procedures has been an obstacle to their broader application, it has already been demonstrated that costs associated with HALS and straight laparoscopic approaches are equivalent.13 Equivalent operative time between HALS and open colectomies may tip the economic scales further away from open surgery toward HALS approaches.
Our study was limited by its retrospective nature and resultant potential selection bias. We have attempted to reduce possible selection bias by use of propensity match based on known confounding variables and further subgroup analysis of segmental resection. Further benefit could be derived from comparing the performance of individual surgeons; unfortunately, this data is not available through NSQIP. Our follow up is also confined to 30 days, which limits the analysis of long-term outcomes including need for reoperation, cancer recurrence, disease-free survival, and mortality beyond 30 days. Despite these limitations, there is no large-scale institutional study examining this comparison. Further research is needed to evaluate the direct benefits of HALS compared to open surgical approach, specifically examining individual performance of surgeons, benefits to surgeons in training, and differences in postoperative outcomes.
Conclusions
Compared to open colectomy, hand-assisted laparoscopic surgery demonstrates improved perioperative outcomes without requiring a significant increase in total operative time. In cases considered too difficult for a totally minimally invasive approach, HALS provides a favorable alterative to the traditional open approach.
Abbreviations
- NSQIP:
-
National Surgical Quality Improvement Program
- HALS:
-
Hand-assisted laparoscopic surgery
References
Bilimoria, K.Y., et al., Laparoscopic-assisted versus open colectomy for cancer: comparison of short-term outcomes from 121 hospitals. J Gastrointest Surg, 2008. 12(11): p. 2001–9.
Hassan, I., et al. Hand-assisted versus laparoscopic-assisted colorectal surgery: Practice patterns and clinical outcomes in a minimally-invasive colorectal practice. Surgical Endoscopy. 2008. 22: p.739–743.
Litwin, D.E., et al., Hand-assisted laparoscopic surgery (HALS) with the HandPort system: initial experience with 68 patients. Ann Surg, 2000. 231(5): p. 715–23.
Osarogiagbon, R.U., et al., Hand-assisted laparoscopic colectomy compared with open colectomy in a nontertiary care setting. Clin Colorectal Cancer, 2007. 6(8): p. 588–92.
Kang, J.C., et al., Hand-assisted laparoscopic colectomy vs open colectomy: a prospective randomized study. Surg Endosc, 2004. 18(4): p. 577–81.
Chung, C.C., et al., Hand-assisted laparoscopic versus open right colectomy: a randomized controlled trial. Ann Surg, 2007. 246(5): p. 728–33.
Maartense, S., et al., Hand-assisted laparoscopic versus open restorative proctocolectomy with ileal pouch anal anastomosis: a randomized trial. Ann Surg, 2004. 240(6): p. 984–91; discussion 991–2.
Anderson, J., et al., A comparison of laparoscopic, hand-assist and open sigmoid resection in the treatment of diverticular disease. Am J Surg, 2007. 193(3): p. 400–3; discussion 403.
Aalbers, A.G., et al., Hand-assisted laparoscopic versus open approach in colorectal surgery: a systematic review. Colorectal Dis, 2010. 12(4): p. 287–95.
Masoomi, H., et al., Risk factors for conversion of laparoscopic colorectal surgery to open surgery: does conversion worsen outcome? World J Surg, 2015. 39(5): p. 1240–7.
Benlice C, Costedio M, Kessler H, Remzi FH, Gorgun E. Comparison of straight vs hand-assisted laparoscopic colectomy: an assessment from the NSQIP procedure-targeted cohort. Am J Surg. 2016;212(3):406–412.
Caputo, D., et al., Conversion in mini-invasive colorectal surgery: the effect of timing on short term outcome. Int J Surg, 2014. 12(8): p. 805–9.
Marcello, P.W., et al., Hand-assisted laparoscopic versus laparoscopic colorectal surgery: a multicenter, prospective, randomized trial. Dis Colon Rectum, 2008. 51(6): p. 818–26; discussion 826–8.
Author’s Contribution
All authors meet the definition of authorship as outlined by ICMJE in that all made substantial contribution to the design of the study or interpretation of data, drafted or revised the work, had final approval of this submission, and agree to be accountable for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Financial Disclosures
None
Disclosures
These data were presented as an oral presentation at the 11th Academic Surgical Congress on February 2nd, 2016. The data used in this study are derived from a de-identified NSQIP file. The American College of Surgeons and the Commission on Cancer have not verified and are not responsible for the analytic or statistical methodology employed, or the conclusions drawn from these data by the investigators.
Grant Support
None.
Rights and permissions
About this article
Cite this article
Leraas, H.J., Ong, C.T., Sun, Z. et al. Hand-Assisted Laparoscopic Colectomy Improves Perioperative Outcomes Without Increasing Operative Time Compared to the Open Approach: a National Analysis of 8791 Patients. J Gastrointest Surg 21, 684–691 (2017). https://doi.org/10.1007/s11605-016-3350-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-016-3350-5