Abstract
Objective
The aim of the study was to investigate the impact of the size of the esophageal hiatus on lower esophageal sphincter pressure (LESP) and acid reflux.
Methods
Patients with gastroesophageal reflux disease who underwent Nissen fundoplication in 2006–2008 were included. All underwent esophageal manometry and 22 had 24-h pH monitoring. The area of the esophageal hiatus was calculated from a photograph shot during surgery. A hiatal index was calculated via division of hiatal area with body mass index (BMI). Correlation and logistic regression analysis were performed.
Results
Twenty-eight patients (average age 44, 14 males) were enrolled. The mean BMI, LESP, DeMeester score, hiatal area, and hiatal index were 27 ± 3.9 kg/m2, 11.7 ± 6.6 mmHg, 43 ± 34, 3.83 ± 1.24 cm2, and 0.143 ± 0.048, respectively. There was a significant negative correlation between hiatal area, hiatal index and LESP (−0.513, p = 0.005, r = −0.439, p = 0.019 respectively). Additionally there was a negative correlation between hiatal area and total LES length (r = −0.508, p = 0.013) and a significant positive correlation between hiatal area, hiatal index, and DeMeester scores (0.452, p = 0.035, 0.537, p = 0.01, respectively). Height and hiatal area were significant factors in multiple linear regression.
Conclusions
The size of the esophageal hiatus significantly affects LESP and acid reflux, and hiatal index is a new value, which appears to reflect the amount of acid reflux. Total LES length is also shortened in patients with a large hiatus.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Existence of a hiatal hernia is one of the most important factors in the pathophysiology of gastroesophageal reflux disease (GERD).1 Presence of hiatal hernia with low lower esophageal sphincter (LES) pressure and resultant esophagitis is commonly associated with GERD.1–3
Esophageal hiatus is mainly formed by the right crus of the diaphragm and the crural diaphragm arises from the dorsal mesentery of the esophagus.4 It is innervated separately from the costal part of the diaphragm and acts in harmony with the LES. The crural diaphragm is in an oblique plane, which results in uneven pressure distribution around the esophagus with mainly anterior and lateral compression.4 This anatomic association is disrupted in the presence of GERD and hiatal hernia, and in a study using high-resolution manometry, a larger separation of LES and crural diaphragm was detected during inspiration in patients with GERD which results in less inspiratory pressure augmentation of the LES.5
The enlargement of the esophageal hiatus results in intrathoracic migration of the abdominal esophagus and LES, which causes induced or free reflux.3 As an initial observation, endoscopic assessment of gastroesophageal flap valve, which is an indirect assessment of the size of the esophageal hiatus, showed a strong correlation with the presence of GERD.6 A recent study that evaluated the cardia circumference by endoscopic measurement showed a direct positive correlation between cardia circumference and the presence and grade of GERD and Barrett’s esophagus.7 Another study showed that dilatation of the gastroesophageal junction or cardia is a progressive phenomenon and results in disruption of the clasp and sling fibers that form the LES.8
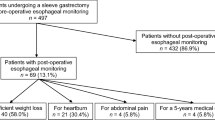
Surgical exploration during antireflux surgery allows direct visualization of the esophageal hiatus (Fig. 1). Surgical findings vary from a simple enlargement of the esophageal hiatus with minimal herniation to a 4–5-cm-large hiatal hernia and severe periesophageal fibrosis.9
Almost all of the criteria used for the diagnosis of GERD rely on intraluminal findings. Little is known about the size of the esophageal hiatus in GERD patients and its effects on LES pressure and other GERD parameters. This prospective study analyzes the impact of the size of the esophageal hiatus on LES pressure and acid reflux and discusses its potential as a clinical evaluation criterion.
Patients and Methods
Patients who have undergone laparoscopic Nissen fundoplication in our department during 2006–2009 were included in the study. Routine preoperative workup included upper gastrointestinal endoscopy, esophageal manometry, and 24-h pH monitoring. Demographic data, body mass index (BMI), and duration of symptoms were also recorded. Surgical treatment was offered to the patients with the conjoint decision of the surgeon (HFB) and gastroenterologists (OUB, AG) following assessment of the symptoms and preoperative findings. The ethics committee of the Marmara University Faculty of Medicine approved our study, and informed consent was obtained from all patients.
Measurement of Esophageal Hiatus
Laparoscopic Nissen fundoplication was performed in all patients through five-port incisions using 30° scope (Fig. 2). A photograph of the esophageal hiatus was either shot during surgery or captured from video recording of the operation. A surgical instrument of known size was used as a scale. The photograph was always from the right side of the esophageal hiatus following hiatal dissection and from the same angle to prevent any calculation bias. The circumferential margin of the esophageal hiatus (square centimeter) was drawn by the surgeon using a graphics program. The depiction starts from the posterior crural triangle, and the edges of the crural fibers were outlined as the esophageal hiatus. The surface area was blindly calculated by one of the authors (BE) using a graphics program. The hiatal area was divided by BMI to calculate an individualized value, which was named as hiatal index.
Statistics
Pearson correlation analysis, independent samples Student’s t test, and multiple stepwise linear regressions were performed. Age, height, weight, hiatal area and hiatal index, and total and abdominal LES lengths were analyzed for their role on LES pressure and 24-h pH scores. p < 0.05 values were considered statistically significant. All values are expressed as arithmetic mean and standard deviation. The data were analyzed using SPSS (15.0) software.
Results
Twenty-eight patients were included in the study. All underwent esophageal manometry and endoscopy. Twenty-four-hour pH monitoring was performed in 22 patients. It could not be performed in six patients due to patient incompliance. The average age was 43.6 ± 11.8 years (14 males).
Endoscopy, Esophageal Manometry, and 24-h pH Monitoring Findings
Twenty-five patients had endoscopic findings of different sizes of hiatal hernia. Fifteen patients had various grades of esophagitis; six patients had antral gastritis or pangastritis. Mean LES pressure was 11.7 ± 6.6 mmHg. LES pressure was less than 10 mmHg in 16 patients and less than 7 mmHg in seven patients. Average DeMeester score was 43.3 ± 33.8 (9.5–111.4). Five patients had scores over 85. Average total and abdominal LES lengths were 2.87 ± 0.83 cm (1.5–4.5) and 2 ± 0.98 cm (0–3.5).
Hiatal Area and Hiatal Index
Average hiatal area was 3.83 ± 1.24 cm2 (1.94–6.91), and average BMI was 27.2 ± 3.9 kg/m2 (20.6–35.9). BMI was over 30 in six patients. Average hiatal index was 0.143 ± 0.048.
Effects of Hiatal Area and Hiatal Index on LESP and 24-h pH Scores
In our study group, we had a group of patients with normal LES pressure (n = 7) and normal pH values (n = 4). These patients were operated on mainly due to the clinical symptomatology. Patients with normal LES pressures (n = 7) were compared with the remaining patients (n = 21), and there was a significant difference of hiatal index (0.114 ± 0.026 vs 0.152 ± 0.05, p = 0.04). The difference of hiatal area was very close to significance (2.87 ± 0.51 vs 4.15 ± 1.26, p = 0.07).
This difference was more profound when patients with abnormal pH values (n = 18) were compared with patients with normal pH scores (n = 4). We found significant difference of hiatal area (2.39 ± 0.22 vs 4.04 ± 1.05, p < 0.001) and hiatal index (0.089 ± 0.015 vs 0.153 ± 0.042, p < 0.001) between the two groups.
Correlations
The correlations are listed in Table 1. There was a significant negative relationship between hiatal area and LES pressure (r = −0.513, p = 0.005; Fig. 3). This relationship was still significant with hiatal index (r = −0.439, p = 0.019; Fig. 4).
There was no correlation between the duration of symptoms and LES pressure (r = −0.339, p = 0.26). There was also a significant positive correlation between hiatal area and 24-h pH monitoring scores (r = 0.452, p = 0.035; Fig. 5). This relationship was even more significant with hiatal index (r = 0.537, p = 0.01; Fig. 6).
LES pressures and 24-h pH monitoring scores did not have any correlation (r = −0.317, p = 0.15). There was no correlation between BMI and hiatal area and hiatal index (r = 0.083, p = 0.68; r = −0.323, p = 0.09, respectively). There was also a significant negative correlation between total LES length and hiatal area (r = −0.508, p = 0.013) and hiatal index (r = −0.435, p = 0.038), and as expected, there was also a very strong positive correlation between LES pressure and total LES length (r = 0.649, p = 0.001).
Multiple Linear Regression Analysis
Among LES pressure, 24-h pH scores, age, hiatal area, hiatal index, weight, height, and total LES length, only height was found to be a significant determinant of 24-h pH scores (p = 0.002), and its overall contribution to the pH scores was found to be 37% (adjusted R square value 0.37). In both models, hiatal area was the only factor that had a significant impact on LES pressure (p = 0.008) and contributed an overall 27% to LES pressure (adjusted R square value 0.27). However, when total LES length was added to the model, hiatal area and total LES length both became significant factors affecting LES pressure (p = 0.04, p = 0.02 respectively).
Discussion
The pathophysiology of GERD is very complex and the extent of contribution of different anatomic structures is unknown. However, most of the recent data show that the anatomic configuration of the esophageal hiatus of the diaphragm has a critical role in the pathophysiology of GERD.1,3,10–12
Three major mechanisms, namely transient LES relaxations, strain-induced reflux in the setting of low or normal LES pressure, and free reflux during periods of low LES pressure or deglutitive relaxation, have been described in the pathophysiology of reflux.11 The latter two mechanisms are frequent in patients with hiatus hernia.3 It has been shown that small increases in intra-abdominal pressure easily overcome the low resting LES pressure leading to reflux in patients with hiatal hernia.10,11 Additionally, the esophagogastric junction opens wider in these patients leading to increased refluxate volume.3 This has been clinically confirmed where more reflux occurred in patients with hiatal hernia, compared with GERD patients without hiatal hernia and normal subjects.11 The lack of crural support for the LES leads to reflux in any occasion with low LES pressure or swallow-induced relaxation. In patients with hiatal hernia during straining, gastric distention, deep inspiration, and swallow-induced LES relaxation, LES malfunctions lead to more severe reflux than other GERD patients.3,12,13 It has been observed that increased refluxate volume leads to erosive esophagitis and different grades of Barrett’s esophagus.2,14,15,16 Hiatal hernia is also associated with shortened total and abdominal LES length, and presence of a hiatal hernia and a defective LES are important predictors of abnormal esophageal acid exposure.17
Our results also show that a large esophageal hiatus leads to diminished LES pressure, acid reflux, and a shortened total LES length. Also, a low LES pressure and decreased esophageal motility are usually associated with a large esophageal hiatus. In our study, we had five patients with a low LES pressure (<10 mmHg) and decreased esophageal motility. In those patients, the average hiatal area was 5.1 cm2 and HI was 0.189. These values were significantly higher than other patients in the study (p = 0.02, both) indicating a more severe GERD.
During expiration, the hiatus narrows and double pressure peak can be observed with manometry.1,18 Even though LES pressure may be within normal values during manometry, any change in intra-abdominal pressure during daily activities can induce reflux when there is no crural support.1,19
In our study, the height of the patient had a strong correlation with pH score, and it was also found to be important in linear regression analysis. This finding may be coincidental, as we did not find the same relationship with weight or BMI. In patients with a 24-h pH scores over 80 (five patients on the top of Figs. 5 and 6), the only significant difference with the remaining patients was height (1.79 ± 0.1 m vs 1.66 ± 0.09 m, p = 0.01). We believe that this may be due to the changes in the anatomic configuration of the diaphragm in tall patients leading to easier and more frequent increases in intra-abdominal pressure.
Anatomic investigations of the esophageal hiatus showed that the diaphragmatic crura of the neonates are hypertrophied, and in adults, the crura become thinner and smaller.20 During this transition, factors (straining, weight lifting, pregnancy), which increase intra-abdominal pressure in a thin and tall patient, may lead to permanent hiatal enlargement. Also, recent research showed that during normal inspiration, the hiatus enlarges; however, with deep inspiration, it narrows.10 In the situation of a large hiatus with thin crura, this diaphragmatic support is lacking.
We do not have adequate information about the size of esophageal hiatus in normal people and GERD patients. In a study focusing on gastroesophageal junction anatomy and its clinical consequences, a detailed intraoperative measurement of extraluminal cardia perimeter was performed. The average cardia perimeter was 6.3 cm in control subjects, 8.9 cm in GERD patients, and 13.8 cm in patients with Barrett’s esophagus.8 Similar findings were observed with endoscopic assessment of the circumference of the cardia, where the length of the circumference showed a direct correlation with esophagitis and Barrett’s esophagus.7 Granderath et al. performed several studies to tailor the hiatal closure according to the size of the esophageal hiatus in order to improve postoperative dysphagia.21,22 In their study of 55 patients, mean size of the esophageal hiatus was 5.09 cm2.21 They recommended reinforced hiatal closure in patients with hiatal sizes more than 5 cm2. Intraoperative measurement of the esophageal hiatus was also recommended by Reardon for the same purpose.23 Currently, a study is underway which aims to calibrate the esophageal hiatus with an inflatable silicon balloon pre- and postcrural repair to prevent postoperative dysphagia and long-term intrathoracic migration.24 The expected diameter of an esophageal hiatus postcrural repair is 18–20 mm in these studies, which results in an estimated hiatal surface area of 2.5–3 cm2.23,24
In our study, BMI had no correlation with hiatal area and hiatal index, which are unexpected findings. This is may be due to our patient group who had patients with relatively normal BMIs and severe GERD. From these findings, we think that it should be very important to have 5-cm2 hiatus in a patient with a BMI of 20. In our patients with a BMI ≤ 25, five patients had hiatal areas ≥3.83 cm2 (cohort average) and six patients had HIs ≥ 0.143 (cohort average). In these patients, average DeMeester score was 82 (36–111), and all had esophagitis despite being on proton pump inhibitors. Thus, in thin patients, reflux is more severe in the setting of a large hiatus, probably due to the low pressure threshold to overcome the resting LES pressure in a small abdomen.
Our study evaluated the intraoperative hiatus size; however, with current radiologic methods, the esophageal hiatus can be reconstructed using computerized tomography or magnetic resonance imaging. We may be able to have inspiratory and expiratory size measurements with these radiologic methods. When the hiatal area is corrected with BMI, a specific individualized value is obtained, and the role of this new value is still to be investigated in further studies.
An objective preoperative assessment of the size of the esophageal hiatus can help us stratify patients to appropriate treatment options, rather than recommending fundoplication for all patients with GERD. Current surgical principles of antireflux surgery include repair of the hernia, reduction of the esophageal hiatus to a normal size, division of short gastric vessels, and formation of a total or partial fundoplication.25 But there is a subgroup of patients who have normal LES pressures despite hiatal enlargement. We had five patients with pathologic pH scores and LES pressures >15 mmHg. Average hiatal area and hiatal index in these patients were 3.13 cm2 and 0.127, respectively, which are both lower than our cohort averages. In these patients, do we really need to add a fundoplication to hiatal repair or can we use endoscopic antireflux methods or techniques that will lead to crural hypertrophy? This issue was studied by a group in Germany on the basis of preventing postoperative unwanted side effects (lifelong inability to vomit, gas bloating) of conventional antireflux surgery, and two prospective trials were carried out.26,27 They applied reinforced hiatal closure without fundoplication in the management of gastroesophageal reflux and both of the studies showed improvement at 3 months postoperatively. But long-term results are lacking.
Our study is limited by two-dimensional image measurements. We tried to overcome this by taking the photograph from the same angle. Another limitation was abdominal CO2 insufflation, which obscures the respiratory changes in the hiatal area during expiration and inspiration.
Conclusion
This is one of the first studies to show a direct correlation between the surgically measured size of the esophageal hiatus and the acid reflux, LES pressure, and total LES length. The size of the esophageal hiatus significantly affects LES pressure and acid reflux. Hiatal area is especially important with its significant contribution to an effective LES mechanism. When hiatal area is divided by BMI, it gives a new value, which appears to reflect the amount of acid reflux and may have a role in the preoperative assessment and decision making.
References
Kahrilas PJ, Lin S, Chen J, Manka M. The effect of hiatus hernia on gastro-oesophageal pressure. Gut 1999;44:476–482.
Sontag SJ, Schnell TG, Miller TQ, Nemchausky B, Serlovsky R, O’Connell S, Chejfec G, Seidel UJ, Brand L. The importance of hiatal hernia in reflux esophagitis compared with lower esophageal sphincter pressure or smoking. J Clin Gastroenterol 1991;13:628–643.
van Herwaarden MA, Samsom M, Smout AJ. Excess gastroesophageal reflux in patients with hiatus hernia is caused by mechanisms other than transient LES relaxations. Gastroenterology 2000;119(6):1439–1446.
Costa MM, Pires-Neto MA. Anatomical investigation of the esophageal and aortic hiatuses: physiologic, clinical and surgical considerations. Anat Sci Int 2004;79(1):21–31.
Pandolfino JE, Kim H, Ghosh SK, Clarke JO, Zhang Q, Kahrilas PJ. High-resolution manometry of the EGJ: an analysis of crural diaphragm function in GERD. Am J Gastroenterol 2007;102(5):1056–1063.
Hill LD, Kozarek RA, Kraemer SJ, Aye RW, Mercer CD, Low DE, Pope CE 2nd. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc 1996;44(5):541–547.
Seltman AK, Kahrilas PJ, Chang EY, Mori M, Hunter JG, Jobe BA. Endoscopic measurement of cardia circumference as an indicator of GERD. Gastrointestinal Endosc 2006;63:22–31.
Korn O, Csendes A, Burdiles P, Braghetto I, Stein HJ. Anatomic dilatation of the cardia and competence of the lower esophageal sphincter: a clinical and experimental study. J Gastrointest Surg 2000;4(4):398–406.
Mattioli S, D’Ovidio F, Pilotti V, Di Simone MP, Lugaresi ML, Bassi F, Brusori S. Hiatus hernia and intrathoracic migration of esophagogastric junction in gastroesophageal reflux disease. Dig Dis Sci 2003;48(9):1823–1831.
Pandolfino JE, Shi G, Curry J, Joehl RJ, Brasseur JG, Kahrilas PJ. Esophagogastric junction distensibility: a factor contributing to sphincter incompetence. Am J Physiol Gastrointest Liver Physiol 2002;282:G1052–G1058.
Pandolfino JE, Shi G, Trueworthy B, Kahrilas PJ. Esophagogastric junction opening during relaxation distinguishes nonhernia reflux patients, hernia patients, and normal subjects. Gastroenterology 2003;125(4):1018–1024.
Holloway RH. The anti-reflux barrier and mechanisms of gastro-oesophageal reflux. Baillieres Best Pract Res Clin Gastroenterol 2000;14(5):681–699.
Kahrilas PJ, Shi G, Manka M, Joehl RJ. Increased frequency of transient lower esophageal sphincter relaxation induced by gastric distention in reflux patients with hiatal hernia. Gastroenterology 2000;118(4):688–695.
Jones MP, Sloan SS, Rabine JC, Ebert CC, Huang CF, Kahrilas PJ. Hiatal hernia size is the dominant determinant of esophagitis presence and severity in gastroesophageal reflux disease. Am J Gastroenterol 2001;96(6):1711–1717.
Avidan B, Sonnenberg A, Schnell TG, Sontag SJ. Hiatal hernia and acid frequency predict presence and length of Barrett’s esophagus. Dig Dis Sci 2002;47(2):256–264.
Cameron AJ. Barrett’s esophagus: prevalence and size of hiatal hernia. Am J Gastroenterol 1999;94(8):2054–1059.
Fein M, Ritter MP, DeMeester TR, Oberg S, Peters JH, Hagen JA, Bremner CG. Role of the lower esophageal sphincter and hiatal hernia in the pathogenesis of gastroesophageal reflux disease. J Gastrointest Surg 1999;3(4):405–410.
Bredenoord AJ, Weusten BL, Carmagnola S, Smout AJ. Double-peaked high-pressure zone at the esophagogastric junction in controls and in patients with a hiatal hernia: a study using high-resolution manometry. Dig Dis Sci 2004;49(7–8):1128–1135.
Bredenoord AJ, Weusten BL, Timmer R, Smout AJ. Intermittent spatial separation of diaphragm and lower esophageal sphincter favors acidic and weakly acidic reflux. Gastroenterology 2006;130(2):334–340.
Moes MJ, Filly RA. The neonatal diaphragmatic crura are hypertrophied: a necessary preparation for the first breath? J Ultrasound Med 2003;22(7):715–718.
Granderath FA, Schweiger UM, Pointner R. Laparoscopic antireflux surgery: tailoring the hiatal closure to the size of hiatal surface area. Surg Endosc 2007;21(4):542–548.
Granderath FA, Schweiger UM, Kamolz T, Pointner R. Dysphagia after laparoscopic antireflux surgery: a problem of hiatal closure more than a problem of the wrap. Surg Endosc 2005;19(11):1439–1446.
Reardon PR. A modest proposal. Surg Endosc 2006;20(6):995.
Fourtanier G. A new method to calibrate the hiatus. Surg Endosc 2007;21(9):1674–1675.
Patti MG, Arcerito M, Feo CV, De Pinto M, Tong J, Gantert W, Tyrrell D, Way LW. An analysis of operations for gastroesophageal reflux disease: identifying the important technical elements. Arch Surg 1998;133(6):600–607.
Linke GR, Zerz A, Tutuian R, Marra F, Warschkow R, Müller-Stich BP, Borovicka J. Efficacy of laparoscopic mesh-augmented hiatoplasty in GERD and symptomatic hiatal hernia. Study using combined impedance–pH monitoring. J Gastrointest Surg 2008;12(5):816–821.
Müller-Stich BP, Linke GR, Borovicka J, Marra F, Warschkow R, Lange J, Mehrabi A, Köninger J, Gutt CN, Zerz A. Laparoscopic mesh-augmented hiatoplasty as a treatment of gastroesophageal reflux disease and hiatal hernias—preliminary clinical and functional results of a prospective case series. Am J Surg 2008;195(6):749–756.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Batirel, H.F., Uygur-Bayramicli, O., Giral, A. et al. The Size of the Esophageal Hiatus in Gastroesophageal Reflux Pathophysiology: Outcome of Intraoperative Measurements. J Gastrointest Surg 14, 38–44 (2010). https://doi.org/10.1007/s11605-009-1047-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-009-1047-8