Abstract
Background
Oxidants (and their generator, xanthine oxidase [XO]) play a role in inducing acute lung injury (ALI) expressed both structurally and functionally. Such damage has recently been demonstrated in the presence of pancreas ischemia–reperfusion (IR). We now investigated whether methylene blue (MB), a clinically used coloring agent and antioxidant in itself, protected the lung exposed to pancreas IR.
Materials and Methods
Isolated pancreata (eight replicates/group) were (1) continuously perfused (controls), (2) made ischemic (IR-0) for 40 min and reperfused without treatment, (3) organs procured from allopurinol-treated rats made ischemic and reperfused with allopurinol, and (4) made ischemic and treated upon reperfusion with three different doses of MB contained in the perfusate. All perfusate solutions were directed into the isolated lungs’ circulation whereby they were perfused for 60 min.
Results
Pancreas injury was documented in all IR organs by abnormally high reperfusion pressure, wet-to-dry ratio, amylase and lipase concentrations, and abnormal XO activity and reduced glutathione in the circulation. Lungs paired with IR-0 pancreata developed ∼60% increase in ventilatory plateau pressure and final Po 2/Fio 2 decrease by 35%. Their weight during reperfusion and bronchoalveolar lavage (BAL) volume and contents increased 1.5–2.5 times the normal values; XO and reduced glutathione values were abnormal both in the BAL and in the lung tissues. Lungs exposed to IR effluents containing allopurinol or 68 μM MB were minimally damaged, whereas perfusion solutions containing 42 or 128 μM MB were ineffective in preventing lung injury.
Conclusions
Ex vivo pancreas IR-induced ALI is preventable by MB, although at a narrow dose range.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemia–reperfusion (IR) is a complex set of events frequently encountered during circulatory disturbances.1 Warm IR of the pancreas is associated with microcirculatory derangements, e.g., increased vascular permeability, arterial constriction, stasis of capillary system, and increased level of circulating pancreatic enzymes.2–4 The systemic consequences of acute pancreatitis might resemble those reported after hepatic or intestinal IR.5 This contention is supported by clinical observations of acute lung injury (ALI) or multiple organ dysfunction syndromes that frequently accompany pancreatitis, even at an early stage.4,6
We have previously documented oxidants’ participation in the processes of ALI.4,5,7,8 Xanthine oxidase (XO) was demonstrated to be a significant source of stress oxidants: XO activity increases after bowel, hind limb, or hepatic IR or hemorrhage and resuscitation, both in animals and in humans.4,5,7–9 The role of XO in inducing remote ALI was demonstrated for pancreas IR as it had been for other organs, using XO oxidoreductase inhibitors (e.g., allopurinol, sodium tungsten).4,5,7–10
MB is a dye that competes with molecular oxygen for the transfer of electrons from flavo-enzymes. The shunting of electrons to and from the colorless reduced leukomethylene blue diverts their flow from the enzyme’s metal–sulfur center where molecular oxygen is normally converted into superoxide radicals and thus the generation of cytotoxic mediators is attenuated.11,12 The presence of MB would ultimately block at least part of the XO-dependent detrimental effects. MB was shown to be beneficial in preventing aortal dysfunction after exposure to post ischemic liver reperfusate in ex vivo conditions.13 Unlike sodium tungsten, MB is a relatively safe clinical compound.
On the basis of the above accumulated data regarding remote ALI, and the potentials of MB to protect organs from damage, we now evaluated the efficacy of increasing doses of MB in protecting the normal, isolated–perfused rat lung from the damaging effects of an IR pancreas. We also used allopurinol, a specific inhibitor of XO, as a reference for the beneficial effect of MB.
Materials and Methods
This study was performed in accordance with the Public Health Service policy on Humane Care and Use of Laboratory Animals, the National Institute of Health (NIH) Guide for the Care and Use of Laboratory Animals and the Animal Welfare Act and was approved by the Institutional Animal Care and Use Committee of Tel Aviv Sourasky Medical Center.
Organ Preparation and the Double-Organ System
Adult male Wistar rats (n = 96), weighing 350–420 g, were anesthetized with intraperitoneal barbiturate. One-half of the animal cohorts donated the pancreata and another—the lungs. Following laparotomy, the pancreata were exposed and separated from adjacent tissues and perfused according to Fujimoto et al’s method.14 After separate animals underwent a tracheotomy, their lungs were ventilated with 95% air–5% CO2 with a piston-type rodent ventilator (10 ml kg−1 tidal volume at a rate of 40 breaths min−1) and a thoracotomy was performed. The lungs were isolated and perfused as reported elsewhere5,7–9 with hemoglobin-free, modified, 5% (weight volume−1) bovine serum albumin (BSA)-enriched Krebs–Henseleit (Krebs) solution (in mM = 118 NaCl, 4.7 KCl, 27 NaHCO3, 2.5 CaCl2, 1.2 MgSO4, 1.2 KH2PO4, 0.05 EDTA, 11 α-d-glucose). Lungs were then suspended from a force displacement transducer (Grass Instruments Co., Quincy, MA, USA). The double-organ perfusion system used in this study is shown in Fig. 1 and was described in detail elsewhere.5,7 Two separate peristaltic pumps were used to perfuse the pancreas and the paired lung. Pre- and post-organ perfusate always passed through an in-line warmer and membrane oxygenator as well as thermometers. All physiological parameters were continuously recorded (Statham Medical P132284™ pressure transducer, Mennen Medical®, Clarence, NY, USA) positioned at the level of the perfusate entering/exiting the organs or the main bronchi. The data were logged onto a hemodynamic monitor (CS/3™, Datex-Ohmeda®, Helsinki, Finland).
The pancreata were always perfused with Krebs in a single-pass mode, while the lungs were perfused either in a single-pass (during the conjoint phase) or in a closed-loop recirculation mode (during stabilization and after the conjoint perfusion, see below). The isolated organs were put in an environmental chamber designed to control temperature and minimize water evaporation.
Drug and Experimental Protocol
Methylene blue (MB) 1% (Hope Pharmaceutics, St. Ana, USA) was added to the Krebs, making respective concentrations of 42, 68, and 128 μM solutions in three IR groups. The administration of MB took place at the time of pancreas + lung serial reperfusion (see below), passing via either organ and aiming to counteract the production of ROS, as would be done clinically.15
Allopurinol, a XO oxidoreductase inhibitor and a classic antioxidant standard, was shown to block XO production in the IR liver.16 Allopurinol (Sigma-Aldrich, Rehovot, Israel, 50 mg kg−1) was injected 6 h before the experiment intraperitoneally in animals whose pancreata were later treated with a 1 mM allopurinol Krebs solution that perfused one group of organs13 (see below).
Pancreata were divided into six groups (n = 8 replicates/group). Their paired lungs were never subjected to ischemia. One pancreas group served as non-ischemia control and another group was subjected to ischemia without treatment upon reperfusion (IR-0). A third IR group was treated with allopurinol (IR-A, see above), and three additional IR groups had pancreata reperfused with 42, 68, or 128 μM MB–Krebs solution (IR-42, IR-68, and IR-128, respectively).
After 30 min of pancreas stabilization, all IR pancreata were rendered ischemic by stopping the flow for 40 min;4 the control organs were continually perfused during that time. In the meantime, isolated lungs were stabilized so that, when pancreas ischemia terminated, the pancreas reperfusate (including the controls’) was shuttled into the pulmonary circulation. After 15 min of in-series pancreas + lung reperfusion (with or without treatment), the pancreas was removed from the circuit and the accumulated effluent was circulated through the only lung in a closed-loop manner for another 45 min. The pancreas was reperfused for 15 min because the vast majority of the endocellular enzymes and other compounds that indicate organ damage and are capable of inducing local and remote organ damage are released into the circulation during this period.4,5 The 45-min lung reperfusion4,5,7,8 is a time lag during which the slow build-up of lung damage can be recognized. Finally, since the pancreas flow rate is two to three times lower than that of the lung, additional fresh Krebs (the missing volume between the lung and the pancreas flow rates) was added during the 15-min in-series period to fill in for the larger pre-determined lung perfusion volume.
Determination of Organ Parameters
Organ viability vs. damage was assessed as previously reported,4 recording changes in pancreas perfusion pressure, exiting perfusate content, and post-experimental wet weight-to-dry weight ratio (WDR). Lung perfusion pressure, plateau ventilatory pressure, and changes in lung weight during the experiment were continuously recorded. Po 2/Fio 2 was calculated as well. We have previously demonstrated4,5 that pulmonary capillary pressure and airway compliance closely and directly correlate with perfusion pressure and ventilatory plateau pressure, respectively; the former were thus omitted in the present report.
At the end of each experiment, lung airways were gently flushed three times with 1 ml of warm saline through the trachea, and the fluid was gently sucked out. Markers of altered bronchoalveolar lavage (BAL), e.g., increased regained volume and/or content, indicate abnormal alveolocapillary permeability.4,5
Biochemical Analyses
Aliquots of 1.0 ml of effluent were collected for laboratory analyses every 15 min throughout the experiment, with additional time points at 1, 5, and 10 min during the in-series reperfusion phase. Samples were processed in duplicate within 24 h from the experiment. Tissues were also assayed. The addition of MB to the Krebs did not interfere with any biochemical analyses.4,17
Abnormal amylase or lipase concentrations in the pancreas-exiting perfusate indicate pancreatic damage.18 They were determined by standard methods and kits for automated analyses (Roche-Böehringer Mannheim GmbH Diagnostics, Mannheim, Germany and Hitachi 747 Analyzer, Tokyo, Japan).
The total activity of XO plus its reduced form, xanthine dehydrogenase (XDH), was assessed following Hashimoto’s method19 (with modifications). After the tissue was washed in an ice-cold sucrose and bottled on a filter paper, it was homogenized with a micro-homogenizer with 0.25 M sucrose solution. After overnight dialysis against 200 ml of 0.25 M sucrose solution at 0°C, the fresh solution thus obtained was used to measure XO activity; overnight dialysis was proven not to cause any change in the activity. The activity was quantified spectrophotometrically by monitoring the formation of uric acid from xanthine through the increase in absorbance at 292 nm. One unit of activity was defined as 1 µmol min−1 of uric acid formed at 37°C, at pH 7.5. Activity was expressed in mU g−1 wet weight for tissues.
Reduced glutathione (GSH) is an intracellular low molecular weight thiol that exerts protective activities, primarily intracellularly.20 In case of glutathione deficiency, brain mitochondria may be damaged due to the accumulation of hydrogen peroxide and the lack of the protective glutathione activity.21 GSH was analyzed in fluids and in fresh organ specimens (Calbiochem #354102 kit, San Diego, CA, USA) and expressed as mM and μmol g−1 dry weight tissue, respectively.
All organs were weighed at the completion of the experiments. Portions were maintained in an oven at 70°C for 5 days and then reweighed to calculate their WDR.
Statistical Analyses
The data variables are summarized as means ± SD. A post hoc analysis was done at each time point after the analysis of variance (ANOVA), with comparisons between group means using the Student–Newman–Keuls’ test. Trends in each group were compared by ANOVA with repeated measures, followed by Tukey’s multiple comparison tests. The significance level was set at P ≤ 0.05.
Results
Pancreas Data
During stabilization, pancreas perfusion pressure was similar among all groups (39–46 mmHg) and remained unchanged in the control group throughout the experiments. It increased in all the IR organs within <3 min of reperfusion, reaching maximum values of 56–68 mmHg. IR also produced edema, as expressed by the 50–78% increase in pancreas WDR compared to the corresponding controls (Table 1).
The biochemical profiles of the various pancreatic effluents are displayed in Table 2. Amylase and lipase activities increased 2–4-fold in the IR groups, starting at 2 min of reperfusion and remained elevated throughout reperfusion, compared to control values. The total XO activity increased and the GSH content decreased during this phase in all IR pancreata except for the control, IR-A, and the IR-68 groups. There was a slight tendency of all abnormal values to decrease at 15 min of reperfusion.
The post-experimental XO activity and GSH content in the pancreas tissues are reported in Fig. 2. The XO activity in all IR-treated pancreata was 2–3-fold lower than those in the controls, reflecting loss of cell components, except for the IR-68 where XO activity was similar to the control’s and for the IR-A where XO was very low because its generation was inhibited by allopurinol. GSH concentration in the IR-0 tissues was multi-fold lower than in the controls, IR-68, or IR-A. This represents GSH pool being consumed due to oxidant/antioxidant misbalance, and lost from the disrupted cells as well.
Post-experimental pancreas tissue total xanthine oxidase (XO + XDH) and reduced glutathione (GSH) data. *p < 0.01 vs. controls, IR-A and IR-68 organs; †p ≤ 0.02 vs. all groups. Abbreviations: IR-0 ischemia–reperfused, untreated pancreata; IR-42 ischemia-reperfused, MB 42 μM-treated organs; IR-68 ischemia-reperfused, MB 68 μM-treated organs; IR-128 ischemia–reperfused, MB 128 μM-treated organs; IR-A ischemia-reperfused, allopurinol-treated pancreata
Lung Ventilatory Data
Ventilatory plateau pressure, an important index of lung damage, was similar among all lungs during the stabilization period (Fig. 3, upper plane). During reperfusion, it did not change significantly in the controls, IR-A, and in the IR-68 groups, but it did in the IR-0 > IR-42 > IR-128 groups. The final Po 2/Fio 2 values were the lowest in the IR-0-attached lungs compared to all other groups of lungs, including the IR-treated ones (Table 3).
Lung ventilatory plateau pressure (upper plane) and perfusion pressure (lower plane) values. *p < 0.05 vs. control, IR-A and IR-68 groups. Abbreviations: IR-0, lungs attached to ischemia–reperfused, untreated pancreata; IR-42 lungs attached to ischemia–reperfused, MB 42 μM-treated organs; IR-68 lungs attached to ischemia–reperfused, MB 68 μM-treated organs; IR-128 lungs attached to ischemia–reperfused, MB 128 μM-treated organs; IR-A lungs attached to ischemia–reperfused, allopurinol-treated pancreata
Lung Circulatory Data
Pulmonary perfusion pressure is reported in Fig. 3 (lower plane): it was similar in all lungs during stabilization and remained unchanged in the control and changed minimally in the lungs that were attached to the IR-A and the IR-68 pancreata. The lungs that were reperfused with the IR-0, the IR-42, and the IR-128-MB effluents showed 2–4-fold increase in the perfusion pressure by the end of reperfusion.
All lungs remained isogravimetric during stabilization; the control, the IR-A, and the IR-68 lungs did not gain much weight during the entire experiments (Fig. 4). In contrast, the IR-0 and the IR-42, and less so the IR-128, lungs progressively gained weight, starting at 5 min of reperfusion: they ultimately reached ∼4 times the IR-A and controls’ weight gain. This picture paralleled lungs’ WDRs (Table 1): IR-0 lungs recorded the highest values while IR-A and IR-68s values changed minimally comparably.
Intra-experimental lung weight gain. *p ≤ 0.05 vs. control, IR-A and IR-68 groups. Abbreviations: IR-0 lungs attached to ischemia–reperfused, untreated pancreata; IR-42 lungs attached to ischemia–reperfused, MB 42 μM-treated organs; IR-68 lungs attached to ischemia–reperfused, MB 68 μM-treated organs; IR-128 lungs attached to ischemia–reperfused, MB 128 μM-treated organs; IR-A lungs attached to ischemia–reperfused, allopurinol-treated pancreata
Analysis of IR-0s BAL volumes and contents proved abnormal as well. High BAL amylase concentration indicates disrupted alveolocapillary barrier. Amylase in the IR-0, the IR-42, and the 128-MB BALs was two to three times higher compared to the corresponding controls, IR-A and IR-68s (Table 3). The total XO activity, also adjusted to the total BAL volume, was low in most IR-treated lungs compared to the IR-0-attached lungs, as were the trends of the retrieved volumes; it was minimal in the IR-A lungs. The GSH profiles were rather high in the controls and in the IR-68s and slightly lower in the IR-As, compared to the IRs (Table 3).
Lung Tissue XO and GSH
The post-experimental total XO activity in the lung tissues is displayed in Fig. 5. The IR-0 lungs’ XO was ∼75% higher than in the controls; XO activity in the IR-A lungs was minimal and that of the IR-68 group was the lowest among all IR-MB-treated groups. Contrarily, GSH contents in the control and in the IR-68 and the IR-128 lungs were higher by a mean of 60–80% compared to the IR-0- and the IR-42-attached organs (Fig. 5). They were also higher than the content detected in the IR-A lungs.
Post-experimental lung tissue total xanthine oxidase (XO + XDH) and reduced glutathione (GSH) data. *p < 0.01 vs. the controls, IR-A- and IR-68-treated organs; † p < 0.05 vs. control, IR-A- and IR-MB-treated groups; ‡ p < 0.05 vs. all groups. Abbreviations: IR-0 lungs attached to ischemia–reperfused, untreated pancreata; IR-42 lungs attached to ischemia–reperfused, MB 42 μM-treated organs; IR-68 lungs attached to ischemia–reperfused, MB 68 μM-treated organs; IR-128 lungs attached to ischemia–reperfused, MB 128 μM-treated organs; IR-A lungs attached to ischemia–reperfused, allopurinol-treated pancreata
Discussion
This study reiterates our previous report that ALI may be induced soon after a normal rat lung is exposed to the effects of warm ischemia of the pancreas.4 The present double-organ model investigated clinical characteristics of ALI, e.g., pulmonary permeability abnormality and relative hypoxia that had previously been associated with pancreatitis.22 The present blood-free protocol further establishes one of our group’s initial suspicions: that all organs that undergo IR would probably “talk the same language” but would also “respond with the same phrase”: they will transmit remote damage by the same pathological code, XO and ROS, and these can be withheld by drugs such as allopurinol and MB.
The results of the present study confirm the long-standing hypothesis that the oxidant/antioxidant misbalance, i.e., XO increase and GSH decrease, is associated with pulmonary vascular and ventilatory injury.4,13 This occurred despite the ∼2 times lower total XO activity recorded in the pancreas compared to those found in the liver, for example4,5,7,9 and the pancreatic effluent being diluted before entering the pulmonary circulation. The potentials of XO to induce ALI following pancreas IR is strongly supported by the data gathered from the IR-treated (both allopurinol and MB) organs. Amylase and lipase leaked out of all pancreata during reperfusion at similar magnitudes in all IR organs, because of the IR-induced cellular lyses. Nevertheless, the exposure of the normal lungs to the 68-MB-treated and the IR-A organs’ reperfusates did not conclude in ALI, despite the presence of high amylase and lipase. Only the presence of abnormally high XO activity and a relatively reduced GSH content in the circuit, without sufficient antioxidant (allopurinol or MB) counter-activity, was associated with lung damage.
MB, a low molecular weight and partially liposoluble vital dye, competes with oxygen for electrons that are transferable from flavo-enzymes.11,12 Some authors suggested that MB inhibits the production of superoxides by competing with molecular oxygen at the metal–sulfur centers of XO, enabling anaerobic oxidation of purine substrates.12,23 Others contended that MB acts as a “parasitic” electron acceptor, shunting electron flow from the normal pathway to the colorless, reduced form of MB, leukomethylene blue, and thus effectively bypassing the generation of ROS.11 In the presence of NO, MB can also act as an antioxidant by eliminating the superoxide that reacts with NO to produce peroxynitrite.24 The efficacy of MB in protecting the rat-isolated aorta from reperfusion-induced dysfunction was demonstrated in a similar isolated perfused double-organ model where MB was used in similar dose regimens.17 The selective protection that was obtained with MB in this study is similar to that of allopurinol, a specific anti-XO compound, and substantiates the role of XO and ROS in the generation of such damage.
The effect of MB is likely to be in a bell-shaped manner. It is difficult to explain why MB is beneficial in ALI at a 68 μM regimen but is ineffective when 42 and 128 μM solutions are applied. The therapeutic range is narrow, especially considering the inhibition of guanylate cyclase17 and NADH cytochrome c reductase23 by MB. Indeed, the relative ineffectiveness of the MB 128 μM solution in protecting lung parameters could originate by the excessive MB-dependent blocking effect on the guanylate cyclase. It was previously concluded that the inhibition of NO could become disadvantageous to the epithelial–endothelial alveolocapillary integrity of the lung, which could outweigh the protective benefits of MB. Under such circumstances, the hypoxia in our 42 >128 μM groups could have further down-regulated the effects of MB as previously documented.25 Together with ROS endothelial-damaging potentials,10 which would ultimately lead to vascular tone impairment, rather high MB dose could generate a vicious cycle of edema, hypoxia, and therapeutic disappointment, as was herein demonstrated.
The BAL data that were retrieved from the IR-coupled lungs, both treated or not, further support our results that MB selectively but beneficially protected the gas-exchanging components of the lung, including the vascular phase. The pancreas-originated enzymatic load and the total XO activity in the various perfusates, mainly in the IR-0 and the IR-42 BALs, indicate that the fluid and the enzymes traversed the alveolocapillary membrane from the vascular bed and scattered within the tissue to be later detected.26 The findings of low XO in the IR-68 and IR-128 BALs, and the lower retrieved volumes, represent limited solutes scattering and fluid permeability through the less damaged alveolocapillary barrier in the presence of effective antioxidant activity of the MB-68 and the MB-128 regimens.5,26 Another explanation for the low XO in the BAL content of the two high MB groups, which would illustrate an integration of the two separate phase activities, may be that these concentrations—but not the MB-42—inhibited ROS production within the lung tissue after inducing initial membrane damage. This is supported by the significantly higher amylase activity detected in the IR-128 group’s BAL compared to those of the IR-MB-68 and the MB-42 groups.
GSH is an essential component in tissue oxidants-antioxidants balance.21,26 Remotely induced damaged lungs pretreated with N-acetyl-l-cysteine were least damaged.26 GSH affords direct scavenging potentials, such as trapping H2O2 and consequently decreasing the production of the highly reactive hydroxyl radical.27 It is also a natural scavenger of the superoxide anion, protecting the cellular protein thiol groups, which are essential for protein function and cellular integrity.20,27,28 The data that emerged from the present study, regarding GSH relationship with XO in the pancreas, support the primary contention described previously,4,29 i.e., that the oxidant/antioxidant misbalance associated or not with the loss of intra- and extracellular GSH that follows remote organ IR may lead to lung edema, hypoxia, and increased vascular permeability in an otherwise normal lung. In the IR-0, IR-42, and the IR-128 lungs, the pancreatas’ and lungs’ GSH leaked out of the organs, and was low in the same groups’ BAL, probably because it also had been consumed in the circuit as an antioxidant, as was shown earlier.26 Contrarily, the higher GSH contents in the IR-68 lungs indicate a proportionately lesser antioxidant consumption because of the low oxidative activity in the circuit as a result of adequate activity of MB. This explanation is supported by our previous demonstrations of MB’s dose-dependent organ protection17,26 and by the data retrieved from the IR-A group of lungs. In addition, the prophylactic use of MB was recently proven in reducing the neurological injury while improving clinical outcome in a rabbit spinal cord IR model.30 These authors found higher GSH levels in the MB-treated group, concluding, as did we, that MB is efficacious because of its antioxidant properties.
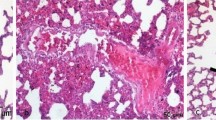
The findings of this study may be relevant to the prevention of clinical lung injuries associated with IR conditions. The present model could mimic clinical syndromes such as shock,1 aortic aneurysm repair,29,31,32 and liver or pancreas transplantation,33,34 all of which are no flow–reflow events that affect the function of large areas, and may damage remote organs upon reperfusion. Better definition of species- and dose-specific characteristics of MB’s efficacy may lead to its consideration as a possible therapeutic tool in such conditions. Both in this and in previous studies,4,5,7,26 indices of ALI (e.g., disturbed Po 2/Fio 2 ratio or alveolar transudate) would stand for MB’s efficacy. “Wet lung” is indeed one of the therapeutic objectives and telling early signs of ALI; it would represent non-distensible or fluid-filled alveoli, disruption of the ultra thin physiologic barrier between the air and the vascular compartment that is at the basis of normal oxygen transport from the alveoli to the pulmonary venous circuit. In our IR-68-MB-treated group, the alveoli were presumably empty and compliant enough to contain larger lavage volumes, resulting in lower retrieved fluid volumes as was in the controls and the appropriately protected lungs.5
Furthermore, clinical acute pancreatitis is diagnosed mainly by acute abdominal pain associated with a concomitant increase in the serum amylase and lipase levels.18 Even though injury is usually mild, severe pancreatic damage develops in 20% of the patients, of whom 15–25% will die, many critically ill and those suffering from ARDS.6,35 Since this study documented tissue edema, abnormal BAL indices, and hypoxia in association with post-ischemia pancreatitis, and since all these phenomena were attenuated when XO and ROS damaging activities were controlled by MB (and comparably by allopurinol), these findings support our primary hypothesis—and now report—of reducing lung injury by the use of various antioxidants: mannitol, N-acetyl-l-cysteine, and now MB, at the first signs of ALI, thus preventing their deterioration into full blown ALI.4,5,7,9,26,36 Finally, while this manuscript was edited for publication, others have demonstrated the possible role of MB in protecting the lung from the effects of rat mesenteric artery-induced IR.37 This report both follows our previous data in animals17,38 and further supports the present promising clinical findings.
In summary, acute lung injury is a frequent complication of pancreatitis. An early increase in alveolocapillary membrane permeability can ensue, leading to lung functional deterioration and hypoxia. While the precise pathophysiology of post-pancreatitis clinical ALI is incompletely understood, this experimental work in an isolated, double-organ animal model points to clinically feasible therapeutic strategies, such as a non-toxic antioxidant, MB, that is currently in use for other indications, and that is potentially capable of attenuating remotely induced ALI.
References
Tan S, Yokoyama Y, Dickens E, Cash TG, Freeman BA, Parks DA. Xanthine oxidase activity in the circulation of rats following hemorrhagic shock. Free Radic Biol Med 1993;15:407.
Gullo L, Cavicchi L, Tomassetti P, Spagnolo C, Freyrie A, D’Addato M. Effects of ischemia on the human pancreas. Gastroenterology 1996;111:1033.
Cuthbertson CM, Christophi C. Disturbances of the microcirculation in acute pancreatitis. Br J Surg 2006;93:518.
Flaishon R, Szold O, Weinbroum AA. Acute lung injury following pancreas ischaemia–reperfusion: role of xanthine oxidase. Eur J Clin Invest 2006;36:831.
Weinbroum A, Nielsen VG, Tan S et al. Liver ischemia–reperfusion increases pulmonary permeability in rat: role of circulating xanthine oxidase. Am J Physiol 1995;268:G988.
Renner IG, Savage WT 3rd, Pantoja JL, Renner VJ. Death due to acute pancreatitis. A retrospective analysis of 405 autopsy cases. Dig Dis Sci 1985;30:1005. [Review].
Weinbroum AA, Hochhauser E, Rudick V, Kluger Y, Sorkine P, Karchevsky E et al. Direct induction of acute lung and myocardial dysfunction by liver ischemia–reperfusion. J Trauma 1997;43:627.
Nielsen VG, Tan S, Weinbroum A, McCammon AT, Samuelson PN, Gelman S et al. Lung injury after hepatoenteric ischemia–reperfusion: role of xanthine oxidase. Am J Respir Crit Care Med 1996;154:1364.
Weinbroum AA, Dembo G, Hochhauser E, Rudick V, Vidne BA. External pacing does not potentiate allopurinol protection of the heart from liver ischemia–reperfusion—a study in an isolated perfused liver-heart rat model. Med Sci Monit 2001;7:1145.
Jarasch ED, Bruder G, Heid HW. Significance of xanthine oxidase in capillary endothelial cells. Acta Physiol Scand Suppl 1986;548:39.
Salaris SC, Babbs CF, Voorhees WD 3rd. Methylene blue as an inhibitor of superoxide generation by xanthine oxidase. A potential new drug for the attenuation of ischemia/reperfusion injury. Biochem Pharmacol 1991;42:499.
Kelner MJ, Bagnell R, Hale B et al. Potential of methylene blue to block oxygen radical generation in reperfusion injury. Basic Life Sci 1988;49:895.
Weinbroum AA, Hochhauser E, Rudick V et al. . Multiple organ dysfunction following remote circulatory arrest: common pathway of radical oxygen species. J Trauma 1999;47:691.
Fujimoto K, Hosotani R, Wada M et al. Ischemia–reperfusion injury on the pancreas in rats: identification of acinar cell apoptosis. J Surg Res 1997;71:127.
Faust KB, Chiantella V, Vinten-Johansen J, Meredith JH. Oxygen-derived free radical scavengers and skeletal muscle ischemic/reperfusion injury. Am Surg 1988;54:709.
Yokoyama Y, Beckman JS, Beckman TK et al. Circulating xanthine oxidase: potential mediator of ischemic injury. Am J Physiol 1990;258:G564.
Weinbroum AA, Kluger Y, Shapira I, Rudick V. Methylene blue abolishes aortal tone impairment induced by liver ischemia–reperfusion in a dose response manner: an isolated-perfused double-organ rat model study. Shock 2001;15:226.
Bradley EL. A clinically based classification system for acute pancreatitis. Arch Surg 1993;128:586.
Hashimoto S. A new spectrophotometric assay method of xanthine oxidase in crude tissue homogenate. Anal Biochem 1974;62:426.
Cotgreave IA, Grafström RC, Moldeus P. Modulation of pneumotoxicity by cellular glutathione and precursors. Bill Rur Physiopathol Respir 1986;22:263s.
Jain A, Martensson J, Stole E, Auld PA, Meister A. Glutathione deficiency leads to mitochondrial damage in brain. Proc Natl Acad Sci U S A 1991;88:1913.
Guice KS, Oldham KT, Johnson KJ, Kunkel RG, Morganroth ML, Ward PA. Pancreatitis-induced acute lung injury. An ARDS model. Ann Surg 1988;208:71.
Kelner MJ, Bagnell R, Hale B et al. Methylene blue competes with paraquat for reduction by flavo-enzymes resulting in decreased superoxide production in the presence of heme proteins. Arch Biochem Biophys 1988;262:422.
Beckman JS, Beckman TW, Chen J et al. Apparent hydroxyl radical production by peroxynitrite: implications for endothelial injury from nitric oxide and superoxide. Proc Natl Acad Sci U S A 1990;87:1620.
Kim JJ, Moon DG, Koh SK. The role of nitric oxide in vivo feline erection under hypoxia. Int J Impot Res 1998;10:145.
Weinbroum AA, Rudick V, Ben-Abraham R, Karchevski E. N-acetyl-L-cysteine for preventing lung reperfusion injury after liver ischemia–reperfusion: a possible dual protective mechanism in a dose–response study. Transplantation 2000;69:853.
Ross D. Glutathione, free radicals and chemotherapeutic agents: mechanism of free radical induced toxicity and glutathione dependent protection. Pharmacol Ther 1988;37:231. [Review].
Folch E, Gelpi E, Rosello-Catafau J, Closa D. Free radicals generated by xanthine oxidase mediate pancreatitis-associated organ failure. Dig Dis Sci 1998;43:2405.
Svensson LG, Crawford ES, Hess KR, Coselli JS, Safi HJ. Experience with 1509 patients undergoing thoracoabdominal aortic operations. J Vasc Surg 1993;17:357.
Bardakcia H, Kaplana S, Karadenizb U, Ozerc C, Bardakcid Y, Ozoguld C, Birincioglua CL, Cobanoglua A. Methylene blue decreases ischemia–reperfusion (I/R)-induced spinal cord injury: an in vivo study in an I/R rabbit model. Eur Surg Res 2006;38:482.
Kretzschmar M, Klein U, Palutke M, Schirrmeister W. Reduction of ischemia–reperfusion syndrome after abdominal aortic aneurysmectomy by N-acetylcysteine but not mannitol. Acta Anaesthesiol Scand 1996;40:657.
Gelman S. The pathophysiology of aortic cross-clamping and unclamping. Anesthesiology 1995;82:1026.
Clavien PA, Harvey PR, Strasberg SM. Preservation and reperfusion injuries in liver allografts. An overview and synthesis of current studies. Transplantation 1992;53:957.
Koelzow H, Gedney JA, Baumann J, Snook NJ, Bellamy MC. The effect of methylene blue on the hemodynamic changes during ischemia reperfusion injury in orthotopic liver transplantation. Anesth Analg 2002;94:824.
Hudson LD, Steinberg KP. Epidemiology of acute lung injury and ARDS. Chest 1999;116:74S.
Galley HF, Richardson N, Howdle PD, Walker BE, Webster NR. Total antioxidant capacity and lipid peroxidation during liver transplantation. Clin Sci (Lond) 1995;89:329.
Greca FH, Gonçalves NMFM, Souza Filho ZA, Noronha L, Silva RFKC, Rubin MR. The protective effect of methylene blue in lungs, small bowel and kidney after intestinal ischemia and reperfusion. Acta Cir Bras 2008;23:149.
Galili Y, Bem-Abrahan R, Weinbroum A et al. Methylene blue prevents pulmonary injury after intestinal ischemia–reperfusion. J Trauma 1998;45:222.
Acknowledgment
Esther Eshkol is thanked for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weinbroum, A.A. Methylene Blue Attenuates Pancreas Ischemia–Reperfusion (IR)-Induced Lung Injury: A Dose Response Study in a Rat Model. J Gastrointest Surg 13, 1683–1691 (2009). https://doi.org/10.1007/s11605-009-0945-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-009-0945-0