Abstract
Background
Tertiary peritonitis (TP) is defined as a severe recurrent or persistent intra-abdominal infection after adequate surgical source control of secondary peritonitis (SP). The aim of this study was to analyze the characteristics of patients with SP who will further develop TP in order to define early diagnostic markers for TP.
Study Design
Over a 1-year period, all patients on the surgical intensive care unit (ICU) with SP were prospectively assessed for the development of TP applying the definition of the ICU consensus conference. The Mannheim Peritonitis Index (MPI), C-reactive protein (CRP) and Simplified Acute Physiology Score II (SAPS II) were assessed at the initial operation (IO) that was diagnostic for SP and in the postoperative period.
Results
Among 69 patients with SP, 15 patients further developed TP, whereas 54 patients did not develop TP. Compared to SP, patients with transition to TP had significantly higher MPI at IO (28.6 vs. 19.8; p < 0.001), relaparotomy rate (2.00 vs. 0.11; p < 0.001), mortality (60% vs. 9%; p < 0.001), duration of ICU stay (14 vs. 4 days; p < 0.005), as well as SAPS II (45.1 vs. 28.4; p < 0.005) and CRP (265 mg/dL vs. 217 mg/dL; p < 0.05) on the second postoperative day after IO.
Conclusions
The MPI at IO as well as CRP and SAPS II at the second postoperative day helps to identify patients at risk for tertiary peritonitis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Definition of Tertiary Peritonitis
Peritonitis is one of the most frequent diagnoses on a surgical intensive care unit leading to severe sepsis.1 It is defined as an intra-abdominal peritoneal infection and can be classified into three major groups—primary, secondary, and tertiary peritonitis. Primary peritonitis—also referred to as spontaneous bacterial peritonitis—arises in the absence of an identifiable anatomical derangement and has a low incidence on surgical intensive care units. The most frequent entity is secondary peritonitis (SP) which is defined as an infection of the peritoneal cavity resulting from perforation, anastomotic disruption, ischemic necrosis, or other injuries of the gastrointestinal tract.2 Operative therapy is the treatment of choice and comprises surgical source control of the infectious focus and reduction of the bacterial load. Tertiary peritonitis (TP) is less common and is defined as a severe recurrent or persistent intra-abdominal infection after apparently successful and adequate surgical source control of SP.2 It is characterized by a prolonged systemic inflammation and organ dysfunction leading to a high rate of SIRS, sepsis, severe sepsis, or septic shock.1,3 As a result, mortality of TP ranges between 30% and 64%.2,4,5 The microbial flora encountered in TP is different from SP and displays mostly opportunistic and nosocomial facultative pathogenic bacteria and fungi (e.g., Enterococci, Enterobacter, Candida). Due to broad-spectrum antibiotic therapy, a significant proportion of microbes develop multi-resistance to antibiotics.
Diagnosis of TP
It is often difficult to differentiate between SP and TP since there is a continuum between both clinical situations and the exact time point when SP turns into TP is often missed. Figure 1 illustrates different clinical scenarios for patients with SP. If SP is diagnosed during an operation—which is referred to as “the initial operation” (IO) in this context—the patient will receive surgical source control (e.g., Hartmann’s procedure for colonic perforation). If surgical source control is successful, the majority of patients will recover. However, a subset of patients will develop clinical signs of recurrent or persistent intra-abdominal infection in spite of apparently successful source control, which often results in a reoperation. During subsequent relaparotomies, recurrent or persistent peritonitis is encountered in spite of adequate and successful surgical source control during the IO. This form of peritonitis is referred to as TP. Importantly, the diagnosis of TP can only be made in the absence of an obvious anatomical defect or disruption of the gastrointestinal hollow viscera; otherwise, the peritonitis has to be classified as ongoing SP—characterized by a primary failure of surgical source control (e.g., breakdown of the closure of the Hartmann’s pouch or breakdown of the suture repair following gastric perforation; Fig. 1). In fact, the most frequent way to diagnose TP, is a “planned” or “on demand” relaparotomy, which is performed in the interval after the IO (Fig. 1).6,7 However, a relaparotomy—either “planned” or “on demand”—may represent a late event in the management of peritonitis, and it is not necessarily the first relaparotomy after the IO when TP is encountered. Therefore, timely—non-operative—diagnosis of TP after the IO and subsequent initiation of an appropriate therapy may help to reduce the complication rate and to improve the prognosis. It is desirable to identify patients at risk for developing TP as early as possible or at least during the first days after the IO for SP.
Diagnostic Challenge
The value of clinical and laboratory parameters and scoring systems for sufficient diagnosis and monitoring of TP is still discussed controversially.5 However, the intensive care unit (ICU) consensus conference provided three categories for the diagnostic certainty of TP: “microbiologically confirmed”, “probable”, and “possible”.2 The Mannheim Peritonitis Index (MPI) represents a scoring system that estimates the severity and prognosis of secondary peritonitis at the onset of SP. It is applied easily under routine conditions during initial surgery for SP in the operating room. It was developed and first described in 1987 by Linder et al.8 and validated in several studies for SP.9,10 Recent studies reported encouraging results for the Mannheim Peritonitis Index regarding detection patients at risk for TP.11,12 Another score that has shown a potential to be successfully applied in TP is the Simplified Acute Physiology Score II (SAPS II) score.12 It was initially designed to predict mortality and disease severity of critically ill patients on surgical intensive care units.13,14 Laboratory parameters like C-reactive protein or procalcitonin have rarely been evaluated in the diagnosis of TP.5,15
However, there is still a lack of studies addressing the identification of risk factors for patients prone to develop TP. It would be desirable to have diagnostic markers that could predict at the onset of peritonitis—during the initial operation or the first postoperative days after—whether the individual patient will develop TP or not (Fig. 1).
The aims of this study were therefore (1) to compare patients’ characteristics, clinical outcome and microbial flora of patients with SP and TP and (2) to investigate the efficacy of clinical and laboratory parameters like C-reactive protein, Mannheim Peritonitis Index and SAPS II to early identify patients with SP at risk for the development of TP.
Material and Methods
Study Population and Definition of Secondary/Tertiary Peritonitis
During a 1-year period (01.01.2006–31.12.2006), all patients admitted to the surgical intensive care unit with a SP were recorded in a prospective database. Due to hospital policy, all patients with a secondary peritonitis are mandatorily admitted to the surgical intensive care unit—for at least 24 h. SP had to be diagnosed during a laparotomy, which was referred to as the IO (Fig. 1). During follow-up, patients with SP were continuously analyzed for the diagnosis of TP—in accordance with the “International Sepsis Forum Consensus Conference”.2 TP was therefore defined as intra-abdominal infection that persists or recurs ≥48 h following successful and adequate surgical source control during the IO.2 As indicated in Fig. 1, patients with an obvious failure of surgical source control after the IO or following procedures (e.g., insufficiency of the rectal stump, anastomotic insufficiency, etc.) were considered as ongoing SP and not as TP.
Demographic data, origin of peritonitis and intra-operative findings during IO, type of surgical procedure performed during IO, antibiotic treatment, and follow-up procedures like relaparotomies were collected. In order to assess the severity of peritonitis as early as at the IO, the Mannheim Peritonitis Index was calculated routinely during the IO as previously described.8,9 Furthermore, C-reactive protein was monitored daily during the first three postoperative days and on postoperative day 7 after IO. SAPS II scores were recorded during the first three postoperative days after IO as previously described.14 Mortality was defined as any death during postoperative hospitalization. Furthermore, intra-operative specimens of abdominal fluid were analyzed by standard microbiological techniques.
Statistical Analysis
Results for the Mannheim Peritonitis Index were expressed as median and displayed in box plots. Box plots are representing the lower, median, and upper quartile whereas whiskers indicate the 10th–90th percentile. Outliers are illustrated by dots. Age, body mass index, Mannheim Peritonitis Index, intensive care unit stay, and the number of relaparotomies per patient were compared by Mann–Whitney test. Frequencies for co-morbidities, underlying malignancy as well as mortality data, frequency of relaparotomies and frequency of specific bacteria were compared by Fisher’s exact test. C-reactive protein values and SAPS II scores are expressed as means ± SEM and compared by T test. p values ≤0.05 were considered statistically significant. To determine the diagnostic accuracy of the Mannheim Peritonitis Index measurement during initial operation as well as C-reactive protein and SAPS II measurements 2 days after initial operation, for the distinction between TP and SP, corresponding receiver operating characteristic curves were calculated. Furthermore, the area under the receiver operator characteristic curve was defined. Cut-off values for the Mannheim Peritonitis Index, C-reactive protein, and SAPS II with the corresponding sensitivity, specificity, and confidence intervals were given. Data were processed with SPSS 16.0/GraphPadPrism 5.
Results
Demographic Data of the Study Population
Over a 1-year period (2006), 1,091 patients were admitted to the surgical intensive care unit. Among the 1,091 intensive care unit patients, 69 were diagnosed having SP. The diagnosis of SP was made intra-operatively in all 69 patients during the IO. Among those, 15 patients (21.7%) further developed TP—according to the ICU consensus conference definition.2 These patients were referred to as TP patients throughout this study. The remaining 54 patients with SP (78.3%) did not develop TP and were therefore referred to as SP patients. Demographic data of the study population are summarized in Table 1. There was no significant difference in gender distribution, age, body mass index, cardiovascular and pulmonary co-morbidities as well as malignant diseases between SP and TP patients (Table 1).
Etiology and Source of Peritonitis
Etiologies and infection source of secondary peritonitis for all patients (n = 69) found at the IO are depicted in Fig. 2, separately for TP patients (n = 15) and SP patients (n = 54). The majority of patients had perforated diverticulitis or other colonic perforations at the IO. Less frequent were other causes like gastric/duodenal perforations, anastomotic insufficiencies, or appendicitis. However, there was no significant difference in terms of anatomical site and source of infection between TP and SP patients.
Detailed Characteristics of TP patients
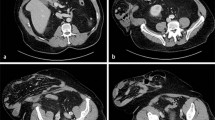
Detailed patient characteristics of TP patients are summarized in Table 2. In only one out of the 15 patients (6.7%), TP was diagnosed non-operatively. In this patient (patient #14), the diagnosis of TP was made 5 days after the IO by clinical signs of infection and laboratory and CT radiographic measurements. In the remaining 14/15 patients (93.3%), TP was diagnosed intra-operatively by relaparotomies after the IO (either first or second relaparotomy; Table 2). As required by the ICU consensus conference definition of TP, these patients showed persistent or recurrent peritonitis ≥48 h following successful and adequate surgical source control which was achieved during IO.2 There was no failure of surgical source control of the IO (e.g., insufficiency of the rectal stump, anastomotic insufficiency, etc.). The median time period between initial operation and diagnosis of TP was 87 h (range 48–338 h).
Severity, Clinical Course, and Outcome of Secondary and Tertiary Peritonitis
The mean Mannheim Peritonitis Index, which was recorded at the IO in all patients (n = 69), revealed significant higher values for TP patients (28.6 ± SD 7.0; median 20, range 17–39) compared to SP patients (19.8 ± SD 8.2; median 20, range 4–37; p ≤ 0.001, Mann–Whitney test) as illustrated in Fig. 3. Elevated severity of peritonitis at the IO of TP patients was paralleled by a higher frequency of relaparotomies following the IO (14/15 patients; 93.3%) compared to SP patients (5/54 patients; 9.3%; p ≤ 0.001; Fisher’s exact test; Table 3). The mean number of relaparotomies following IO per patient was 2.00 (±0.93 SD) for TP patients compared to 0.11 (±0.37 SD) for SP patients (p ≤ 0.001; Mann–Whitney test; Table 3). All relaparotomies in the five SP patients were “programmed relaparotomies”. In the TP group, there were nine patients with “programmed relaparotomies” and five patients with “on demand relaparotomies” that were initiated by clinical detection. As a consequence, the concept of “programmed relaparotomies” was applied with a significantly higher frequency in TP patients (60.0%) compared to SP (9.3%; p ≤ 0.001; Fisher’s exact test; Table 3). The timing and chronology of relaparotomies in relation to the IO is illustrated in Fig. 4. Impaired outcome of TP patients compared to SP patients was paralleled by significantly longer hospitalization on the intensive care unit, since median intensive care unit stay for TP patients was 13 days (range 3–77 days) compared to 4 days (range 1–50 days) for SP patients (p = 0.002, Mann–Whitney test; Table 3). Compared to SP patients, TP patients were characterized by higher frequency of multi-organ failure (73.3% vs. 18.5%; p ≤ 0.001, Fisher’s exact test) and higher mortality (60.0% vs. 9.3%; p ≤ 0.001, Fisher’s exact test; Table 3). All deaths in the TP group (9/15) were due to septic multi-organ failure as a result of tertiary peritonitis. There were no autopsies performed.
Mannheim Peritonitis Index (MPI) at the initial operation. Significantly higher MPI values for patients who further developed tertiary peritonitis (TP; n = 15) compared to patients who did not (SP; n = 54; p ≤ 0.001; Mann–Whitney test). Boxes represent the lower, median, and upper quartiles; whiskers indicate the 10th–90th percentile and outliers are illustrated by dots.
Microbiological Data
Figures 5 and 6 illustrate the microbiological spectrum of microbial isolates obtained from the IO and the antibiotic therapy initiated during the IO—separately for TP patients (n = 15 specimens) compared to SP patients (n = 54 specimens). The distribution of microbiological species at the time of the IO did not differ significantly between TP and SP patients with the exception of Escherichia coli. There was a significantly higher proportion of E. coli in isolates from TP patients compared to SP patients (73.3% vs. 37.0%; p ≤ 0.05; Fisher’s exact test; Fig. 5). As depicted in Fig. 6, antibiotic therapy initiated during IO after detection of secondary peritonitis did not differ significantly between TP and SP patients. The majority of patients were treated with imipenem/cilastatin (SP 27.8%; TP 46.7%; p = 0.21; Fisher’s exact test) or piperacillin/tazobactam (SP 51.9%; TP 53.3%; p = 1.00; Fisher’s exact test). Figure 7 delineates the changes in the microbiological spectrum in TP patients compared to SP patients. This analysis compares isolates of TP patients from the relaparotomy that was diagnostic for TP and isolates from the IO of SP patients (n = 54 specimens). In the TP group (n = 15 patients), only 11 specimens were obtained during relaparotomy and could be included into the analysis. There was a significant microbiological shift towards Enterococcus and Candida species in TP with significantly higher proportions of Enterococcus (*p ≤ 0.05; Fisher’s exact test) and Candida (**p ≤ 0.01; Fisher’s exact test) in TP patients compared to SP patients (Fig. 7).
Microbiological spectrum of microbial isolates obtained from the initial operation. Comparison between patients who further developed tertiary peritonitis (TP; n = 15 specimens) compared to patients who did not (SP; n = 54 specimens). Significantly higher proportion of E. coli in TP compared to SP (*p ≤ 0.05; Fisher’s exact test). Dotted lines separate gram-negative bacteria, gram-positive bacteria, and fungi.
Antibiotic treatment initiated during the initial operation at the onset of secondary peritonitis. There was no difference in the antibiotic spectrum between patients who further developed tertiary peritonitis (TP; n = 15) compared to patients who did not (SP; n = 54 specimens; Fisher’s exact test).
Comparison of the microbiological spectrum between secondary peritonitis (SP) and tertiary peritonitis (TP). The microbial isolates of patients with TP were obtained from the relaparotomy that was diagnostic for TP (n = 11 specimens). Isolates of patients with SP were obtained from the initial operation (n = 54 specimens). Significantly higher proportion of Enterococcus (*p ≤ 0.05; Fisher’s exact test) and Candida (**p ≤ 0.01; Fisher’s exact test) in TP compared to SP. Dotted lines separate gram-negative bacteria, gram-positive bacteria, and fungi.
Laboratory Parameters
The mean C-reactive protein (±SEM) during the first postoperative days after the IO (postoperative day 1–postoperative day 7) was significantly higher in TP patients (204 ± 13 mg/L) compared to SP patients (166 ± 8 mg/L; p ≤ 0.05, T test). The time course of C-reactive protein values during the first postoperative days after the IO is displayed in Fig. 8 for SP and TP patients. Both curves decline from preoperative values to postoperative day 1. On the second postoperative day, C-reactive protein is at its maximum and again declining over the next days. Although both curves run parallel to each other, mean C-reactive protein values for TP patients are significantly higher compared to SP patients on the second postoperative day (265 ± 17 vs. 217 ± 12 mg/L; p = 0.05, T test) and on postoperative day 7 (174 ± 23 vs. 119 ± 11 mg/L; p = 0.03, T test; Fig. 8).
Time course of C-reactive protein (CRP) in the perioperative period of the initial operation in patients who further developed tertiary peritonitis (TP) and patients who did not (SP). Mean CRP ± SEM values are indicated preoperatively (preop.) and on postoperative days 1, 2, 3, and 7 (d1, d2, d3, and d7). Significantly higher CRP values for TP compared to SP on the second postoperative day (p = 0.05) and postoperative day 7 (p = 0.03; T test).
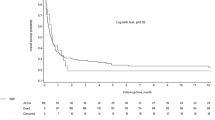
The mean SAPS II score (±SEM) during the first three postoperative days after the IO operation was significantly higher in TP patients (46.1 ± 3.7) compared to SP patients (29.7 ± 2.0) (p ≤ 0.001, T test). The time course of SAPS II values during the first three postoperative days after the initial operation is depicted in Fig. 9. SAPS II scores for TP patients on the first (47.1 ± 4.2), second (45.1 ± 4.0), and third postoperative days (44.9 ± 4.0) were significantly higher compared to SP patients on the respective days (30.7 ± 2.1, 28.4 ± 2.0, and 30.3 ± 2.5, respectively; p ≤ 0.001, p ≤ 0.001, and p = 0.004, respectively; T test; Fig. 9).
Time course of SAPS II scores in the postoperative period after the initial operation in patients who further developed tertiary peritonitis (TP) and patients who did not (SP). Mean SAPS II scores ± SEM values are indicated on the first three postoperative days (d1–d3). Significantly higher SAPS II scores for TP compared to SP during the whole period (p ≤ 0.001, p ≤ 0.001, and p = 0.004, respectively; T test).
Early Detection of Tertiary Peritonitis
In order to asses to what extent intra-operative Mannheim Peritonitis Index measurement during the IO and C-reactive protein and SAPS II measurements on postoperative day 2 could differentiate between TP patients and SP patients, the corresponding receiver operating characteristic curve was constructed and the area under the receiver operator characteristic curve was calculated. The area under the receiver operator characteristic curve for the Mannheim Peritonitis Index at the initial operation was 0.794 (95% confidence interval = 0.672–0.915; p ≤ 0.001). A sensitivity of 80.0% and specificity of 68.5% were achieved with a Mannheim Peritonitis Index cut-off value of 22 (Table 3). The area under the receiver operator characteristic curve for C-reactive protein and SAPS II on the second postoperative day after initial operation was 0.696 (95% confidence interval = 0.562–0.830; p = 0.02) and 0.797 (95% confidence interval = 0.634–0.960; p ≤ 0.001), respectively. A cut-off value for C-reactive protein of 215 mg/L led to a sensitivity of 80.0% and a specificity of 57.4%. A cut-off value of 39 for the SAPS II score revealed a sensitivity of 80.0% with a specificity of 74.5% (Table 4).
Discussion
Definition of Tertiary Peritonitis
The standard treatment for SP is an immediate laparotomy with surgical source control and antibiotic therapy. However, a few patients will develop a clinical syndrome—also referred to as TP, which is characterized by a persistent intra-abdominal infection, an altered microbial flora, failure of the immune response, and progressive organ dysfunction leading to high mortality. There is still an ongoing debate about the definition of TP. In fact, some opinions deny the existence of TP as a distinct entity. In the past, TP has simply been defined as failed surgical source control or inadequate antibiotic therapy of SP. Other definitions emphasized the impaired host response to peritoneal infection.16 This heterogeneity of definitions resulted in varying inclusion criteria and incommensurable results in clinical studies focusing on TP.5 In the current study, we applied the latest ICU consensus conference guideline that provides a precise definition. TP was defined as intra-abdominal infection that persists or recurs ≥48 h following successful and adequate surgical source control.2 This definition contains two essential conditions, which have to be met: the time period (≥48 h) and successful surgical source control. Although the ICU guideline does not provide further explanation for “successful surgical source control”,2 our interpretation of this term was a complete and sustainable eradication of the surgical focus. If a patient presented—during relaparotomy or clinically—with an obvious failure of previous surgical source control in terms of a “technical problem”, this patient was not classified as TP but as SP patient. Other examples of “failure of surgical source” control comprise insufficiency of the rectal stump after Hartmann’s procedure, anastomotic insufficiency, or other technical problems that lead to disruption of the physical integrity of the gastrointestinal hollow organs.
Nevertheless, there is consensus that SP and TP exist in a continuum and the transition between both may be quite subtle. Although TP may be diagnosed during relaparotomy as a simple discrete point in the illness, in reality, it evolves gradually over several hours or days. In the current study, TP was diagnosed during relaparotomy in 14/15 patients. Only one patient was diagnosed having TP by clinical and laboratory measures 120 h after initial operation. For all patients with TP, the time interval between the initial operation and the diagnosis of TP was 87 h (median) and thus considerably long. In addition, it is important to emphasize that in six patients the diagnosis was made not until the second relaparotomy, while during the first relaparotomy the intra-abdominal situation was estimated innocuously. It was therefore the aim of this study to compare clinical and laboratory parameters between patients with SP who will further develop TP (TP patients) and who will not (SP patients). The necessity to define early predictors for TP becomes evident looking upon the devastating mortality rate for TP of 60% encountered in this study, which was relatively high compared to other studies—reporting mortality rates ranging between 27% and 64%.11,12,17 We also observed a clear relationship between peritonitis type (TP vs. SP) and mortality, which was in contrast to other publications.16
Risk Factors and Microbial Flora of TP
Several epidemiologic and clinical risk factors have already been identified that might predispose to TP, which include age, etiology of peritonitis, malnutrition, and multi-resistant microorganisms.15 With regard to the patient’s age or etiology and infection source of peritonitis, we were unable to detect significant differences between TP and SP. Concerning the microbial flora encountered in the initial operation, we did only find a higher proportion of E. coli in TP patients compared to SP patients. All other bacteria were equally distributed. It has recently been shown that there is a microbial shift in TP towards Enterococcus, Enterobacter, Pseudomonas, Candida albicans and other opportunistic bacteria and fungi.11,12,17 However, in this study, we could only demonstrate a significant shift towards Enterococcus and C. albicans between patients who suffered from TP compared to SP. In our opinion, microbiology is not suited as an early diagnostic marker for the identification of patients at risk for TP, since microbiological studies—including resistance analysis—take up to 1 week. Nevertheless, future studies will be necessary to investigate the microbial shift as well as the antibiotic resistance data in our patients.
Predictive Parameters for TP
In the current study, we analyzed three early and easily accessible parameters for identification of patients who might further develop TP: Mannheim Peritonitis Index, SAPS II, and C-reactive protein. Some might argue that due to persisting systemic inflammation repeated surgical procedures or intermittent nosocomial infections, the value of clinical (Mannheim Peritonitis Index, SPAS II) and laboratory parameters (C-reactive protein) for sufficient diagnosis of TP is limited.5 In fact, there are conflicting data concerning the value applying such parameters for the detection of TP.15,17 Unlike other studies, our approach was to analyze these parameters as early as possible—at the IO that was diagnostic for SP and on the first postoperative days.
The Mannheim Peritonitis Index was initially designed to estimate the prognosis and predict mortality of patients with SP.8–10 In our study population, the Mannheim Peritonitis Index was significantly higher in patients that later on developed TP compared to SP (28.6 vs. 19.8). Similar results have been shown in two recent publications analyzing the Mannheim Peritonitis Index in TP.11,12 In addition, the receiver operator characteristic analysis in the current study revealed encouraging results with an area under the receiver operator characteristic curve of 0.794 for the detection of TP. With regard to the receiver operator characteristic analysis, it has to be considered that the Mannheim Peritonitis Index is an early—if not the earliest—marker for TP. It is accessible immediately during the IO. This renders the Mannheim Peritonitis Index to a diagnostic tool of high potential.
The second parameter was the SAPS II score, initially designed to predict mortality and disease severity of critical ill patients.13,14 We could demonstrate that SAPS II was significantly higher during the first three postoperative days after initial operation in TP patients (46.0) compared to SP patients (29.7). Interestingly, the curves for TP and SP patients ran completely parallel to each other over the whole period. The receiver operator characteristic analysis on the second day revealed an area under the receiver operator characteristic curve of 0.797, which demonstrates the diagnostic potential of this scoring system for early identification of patients at risk for TP. Our results are consistent with a recent study that reported similar SAPS II scores for TP (45.6) and SP (31.9) patients—underlining the importance of this parameter.12
The third parameter tested in our study was the acute phase protein C-reactive protein. Although C-reactive protein constitutes a routine parameter in patients with abdominal infections, it has hardly been explicitly evaluated in the diagnosis of TP.5,15 In our study, the time course of C-reactive protein displayed a curve with two peaks: one peak preoperatively and one peak on the second postoperative day after the IO. In between, on the first postoperative day, lower C-reactive protein values were observed, possibly due to an operative clearing effect. Interestingly, although both curves run parallel, C-reactive protein values of TP patients were significantly higher compared to SP patients on the peak of the second postoperative day (265 vs. 217) after the IO. However, the corresponding area under the receiver operator characteristic curve was only 0.696. The main problem of C-reactive protein is the lack of specificity for abdominal infections, as shown in numerous studies.18–20 A rise of C-reactive protein during the postoperative period may simply be the result of the operative trauma.21,22 Nevertheless, this study shows a high diagnostic potential of C-reactive protein. This hypothesis has to be addressed in further studies.
Conclusion
In conclusion, due to high mortality of tertiary peritonitis and often delayed diagnosis, it is crucial to identify patients at risk for developing tertiary peritonitis as early as possible: at the initial operation that reveals the diagnosis of peritonitis and during the first postoperative days. Our results indicate that the Mannheim Peritonitis Index assessed at the initial operation and the time course of C-reactive protein and SAPS II during the first days after initial operation are promising diagnostic candidates for the future.
Abbreviations
- CRP:
-
C-reactive protein
- ICU:
-
Intensive care unit
- IO:
-
Initial operation
- MPI:
-
Mannheim Peritonitis Index
- SAPS II:
-
Simplified Acute Physiology Score II
- SP:
-
Secondary peritonitis
- TP:
-
Tertiary peritonitis
- SP patient:
-
Patient with SP who did not further develop TP
- TP patient:
-
Patient with SP who further developed TP
References
Weiss G, Steffanie W, Lippert H. Peritonitis: main reason of severe sepsis in surgical intensive care. Zentralbl Chir 2007;132:130–137. doi:10.1055/s-2006-960478.
Calandra T, Cohen J. The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med 2005;33:1538–1548. doi:10.1097/01.CCM.0000168253.91200.83.
Reemst P, Van Goor H, Goris RJ. SIRS, MODS and tertiary peritonitis. Eur J Surg 1996;576(Suppl):47–48. discussion 49.
Buijk SE, Bruining HA. Future directions in the management of tertiary peritonitis. Intensive Care Med 2002;28:1024–1029. doi:10.1007/s00134-002-1383-6.
Evans HL, Raymond DP, Pelletier SJ, Crabtree TD, Pruett TL, Sawyer RG. Diagnosis of intra-abdominal infection in the critically ill patient. Curr Opin Crit Care 2001;7:117–121. doi:10.1097/00075198-200104000-00010.
Koperna T, Schulz F. Relaparotomy in peritonitis: prognosis and treatment of patients with persisting intraabdominal infection. World J Surg 2000;24:32–37. doi:10.1007/s002689910007.
Koperna T. Surgical management of severe secondary peritonitis. Br J Surg 2000;87:378. doi:10.1046/j.1365-2168.2000.01369-12.x.
Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E. The Mannheim Peritonitis Index. An instrument for the intraoperative prognosis of peritonitis. Chirurg 1987;58:84–92.
Billing A, Frohlich D, Schildberg FW. Prediction of outcome using the Mannheim Peritonitis Index in 2003 patients. Peritonitis Study Group. Br J Surg 1994;81:209–213. doi:10.1002/bjs.1800810217.
Fugger R, Rogy M, Herbst F, Schemper M, Schulz F. Validation study of the Mannheim Peritonitis Index. Chirurg 1988;59:598–601.
Panhofer P, Izay B, Riedl M, Ferenc V, Ploder M, Jakesz R, Gotzinger P. Age, microbiology and prognostic scores help to differentiate between secondary and tertiary peritonitis. Langenbecks Arch Surg 2009;394(2):265–271.
Weiss G, Meyer F, Lippert H. Infectiological diagnostic problems in tertiary peritonitis. Langenbecks Arch Surg 2006;391:473–482. doi:10.1007/s00423-006-0071-3.
Agha A, Bein T, Frohlich D, Hofler S, Krenz D, Jauch KW. “Simplified Acute Physiology Score” (SAPS II) in the assessment of severity of illness in surgical intensive care patients. Chirurg 2002;73:439–442. doi:10.1007/s00104-001-0374-4.
Le Gall Jr., Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 1993;270:2957–2963. doi:10.1001/jama.270.24.2957.
Malangoni MA. Evaluation and management of tertiary peritonitis. Am Surg 2000;66:157–161.
Evans HL, Raymond DP, Pelletier SJ, Crabtree TD, Pruett TL, Sawyer RG. Tertiary peritonitis (recurrent diffuse or localized disease) is not an independent predictor of mortality in surgical patients with intraabdominal infection. Surg Infect (Larchmt) 2001;2:255–263. discussion 264–255. doi:10.1089/10962960152813296.
Nathens AB, Rotstein OD, Marshall JC. Tertiary peritonitis: clinical features of a complex nosocomial infection. World J Surg 1998;22:158–163. doi:10.1007/s002689900364.
Dahaba AA, Hagara B, Fall A, Rehak PH, List WF, Metzler H. Procalcitonin for early prediction of survival outcome in postoperative critically ill patients with severe sepsis. Br J Anaesth 2006;97:503–508. doi:10.1093/bja/ael181.
Mokart D, Merlin M, Sannini A, Brun JP, Delpero JR, Houvenaeghel G, Moutardier V, Blache JL. Procalcitonin, interleukin 6 and systemic inflammatory response syndrome (SIRS): early markers of postoperative sepsis after major surgery. Br J Anaesth 2005;94:767–773. doi:10.1093/bja/aei143.
Reith HB, Mittelkotter U, Debus ES, Kussner C, Thiede A. Procalcitonin in early detection of postoperative complications. Dig Surg 1998;15:260–265. doi:10.1159/000018625.
Lindberg M, Hole A, Johnsen H, Asberg A, Rydning A, Myrvold HE, Bjerve KS. Reference intervals for procalcitonin and C-reactive protein after major abdominal surgery. Scand J Clin Lab Invest 2002;62:189–194. doi:10.1080/003655102317475443.
Meisner M, Tschaikowsky K, Hutzler A, Schick C, Schuttler J. Postoperative plasma concentrations of procalcitonin after different types of surgery. Intensive Care Med 1998;24:680–684. doi:10.1007/s001340050644.
Acknowledgments
The authors thank all the members of the intensive care unit team for continuous support. They further thank Tim Holland-Letz, Department of Medical Informatics, Biometry and Epidemiology, Ruhr-University Bochum for statistical assistance.
Author information
Authors and Affiliations
Corresponding author
Additional information
Ansgar M. Chromik and Andreas Meiser contributed equally to this publication.
Rights and permissions
About this article
Cite this article
Chromik, A.M., Meiser, A., Hölling, J. et al. Identification of Patients at Risk for Development of Tertiary Peritonitis on a Surgical Intensive Care Unit. J Gastrointest Surg 13, 1358–1367 (2009). https://doi.org/10.1007/s11605-009-0882-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-009-0882-y