Abstract
Background
Laparoscopy-assisted distal gastrectomy (LADG) with standard D2 dissection is a complex procedure usually performed only by experienced surgeons, and the feasibility of this procedure still remains unclear.
Method
Patients who underwent LADG at the Cancer Institute Hospital between April 2006 and October 2008 were recruited for this study. Early surgical outcomes were compared between patients who underwent complete D2 dissection (complete D2 group; n = 42) and those who underwent D1 + beta dissection (D1 + beta group; n = 179) to determine the feasibility of laparoscopic D2 lymph node dissection.
Results
In complete D2 group, the operation time was longer (253 ± 10 vs 224 ± 4 min; P = 0.005), and the number of retrieved lymph nodes was larger (41 ± 2 vs 35 ± 1; P = 0.002) compared with those in D1 + beta group. The other early surgical outcomes monitored for the two groups were not different between groups.
Conclusions
LADG with complete D2 lymph node dissection can be performed safely if the procedure is standardized and an experienced laparoscopic surgeon performs the surgery. To be accepted as a standard treatment for advanced gastric cancer, well-designed prospective trial is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Laparoscopy-assisted gastrectomy (LAG) is increasingly performed in Japan since the first case of laparoscopy-assisted distal gastrectomy (LADG) with Billroth I reconstruction was reported.1 Several advantages of LAG compared with conventional open gastrectomy have been documented,2–8 including reductions in bleeding and pain and reduced disturbance of respiratory function. However, LAG has limitations for lymph node dissection,7 and at present in Japan, generally accepted laparoscopic lymph node dissection is D1 and D1 + beta lymph node dissection (D1 + station 7, 8a, 9 lymph nodes dissection), while complete laparoscopic D2 lymph node dissection is performed by experienced surgeons.7,9–13
A large randomized controlled trial conducted in Europe failed to prove the efficacy of conventional open gastrectomy with D2 lymph node dissection due to the high morbidity and mortality rate.14–17 By comparison, in Japan, the procedure for conventional open gastrectomy with complete D2 lymph node dissection (D1 + station 7, 8a, 9, 11p, 12a, 14v lymph node dissection) is well established and accepted as a standard practice for the treatment of advanced gastric cancer.18–20 Therefore, the feasibility of LAG with D2 lymph node dissection should be investigated so that LAG is accepted as a standard treatment for advanced gastric cancer.
It is difficult to perform LAG with complete D2 lymph node dissection since this type of surgery involves major vessel and pancreatic tissue exposure, and there is, therefore, an increased risk of major vessel injury and postoperative pancreas-related infections associated with the procedure. Therefore, the establishment of standardized procedures for D1 + beta lymph node dissection might be an initial step towards the introduction of complete laparoscopic D2 lymph node dissection. In our institute where these procedures have been standardized,21 the number of laparoscopic D2 lymph node dissections is gradually increasing. In the present study, the early surgical outcomes of laparoscopic D2 lymph node dissection was investigated, and these surgical outcomes were compared with those following D1 + beta lymph node dissection. The feasibility of laparoscopic D2 lymph node dissection following standardization of LAG with D1 + beta lymph node dissection was thereby determined.
Patients and Methods
Patients who were treated with LADG with extraperigastric lymph node dissection performed by one of the two specialists (F.T. or H.N.) at the Cancer Institute Hospital between April 2006 and October 2008 were included in the study. All patients had histologically proven adenocarcinoma prior to surgery, and all surgeries were conducted with a curative intent.
Patients’ characteristics, including gender, age, body mass index, and preoperative comorbidity, were collected from their respective clinical records. Information on the operation procedure, operation time, intraoperative bleeding, intraoperative complications, degree of lymph node dissection, and number of retrieved lymph nodes were collected from surgical charts. The postoperative clinical course, such as the day of first flatus, the day of first oral intake, postoperative morbidity, mortality, and the duration of the postoperative hospital stay were also collected from clinical records. All data collection was performed retrospectively.
Indication for LADG with D2 Lymph Node Dissection
Laparoscopy-assisted distal gastrectomy with D2 lymph node dissection is indicated in patients with cT2N0 or cT1N1 gastric cancer. LADG with D2 lymph node dissection is also indicated even in patients with cT1N0 early gastric cancer if tumor invasion to proper muscle layer (T2a) or first tier lymph node metastasis was suspected intraoperatively.
Numbering of Lymph Node Station and Degree of Lymph Node Dissection
The number of each lymph node station was assigned according to the Japanese Classification of Gastric Carcinoma.22 Stations 1 to 6 were perigastric lymph nodes while 7, 8a, 9, 11p, 12a, and 14v were second-tier lymph nodes and were located along the left gastric artery, the common hepatic artery, the celiac axis, the proximal half of the splenic artery, the proper hepatic artery, and the surface of the superior mesenteric vein at the lower border of the pancreas, respectively. D1 + beta lymph nodes were defined as regional lymph nodes with some additional second-tier lymph nodes (stations 7, 8a, and 9). Conversely, all second-tier lymph nodes were dissected during complete D2 lymph node dissection (Fig. 1).
Extragastric lymph node station. D1 + beta lymph node dissection includes station 7, 8a, and 9 lymph node (open oval) retrieval. In distal gastrectomy with D2 lymph node dissection, station 11p and 12a lymph node (shaded oval) have to be dissected as well as station 7, 8a, and 9 lymph nodes. Moreover, station 14v lymph node (shaded oval) should also be dissected in patient with lower third gastric cancer.
Conversion from LADG to Conventional Open Gastrectomy
Laparoscopy-assisted distal gastrectomy was converted to conventional open gastrectomy if intraoperative findings showed (1) advanced gastric cancer was obviously exposed the serosal membrane, (2) positive second-tier lymph nodes following frozen examination of retrieved lymph nodes, (3) uncontrollable bleeding or adhesion, and (4) any other difficulties in performing laparoscopic surgery.
Operation Procedures of LAG with Complete D2 Lymph Node Dissection
We previously reported our standardized laparoscopic procedure for LAG with D1 + beta lymph node dissection; thus techniques for station 11p, 12a, and 14v lymph node dissection were highlighted in this manuscript.21
Dissection of Station 6 and 14v Lymph Nodes
The origin of the right gastroepiploic vein and the surface of the superior mesenteric vein at the lower border of the pancreas were exposed for the dissection of station 14v lymph nodes. The right gastroepiploic artery and vein were divided separately at its origin using a clip (Lapro-Clip™; single absorbable ligating clip cartridge, Covidien) and Ligasure (Covidien), then station 6 and 14v lymph node dissection were completed.
Dissection of Station 5 and 12a Lymph Nodes
The origin of the right gastric artery and vein was exposed using AutoSonix™ ULTRA SHEARS™. The left border of the proper hepatic artery and portal vein was also exposed, and station 12a lymph nodes were completely dissected. The right gastric artery and vein were then divided using clips and Ligasure at its origin.
Dissection of Station 7, 8a, 9, and 11p Lymph Nodes
The pancreatic capsule was dissected using AutoSonix™ ULTRA SHEARS™ at the line of the superior pancreatic border. The splenic artery and its origin were exposed, and the surface of splenic vein was also exposed toward the pancreatic tail as far as the root of the posterior gastric artery, then station 11p lymph node was completely retrieved. Next, the left gastric artery and vein were divided at their origins, respectively. Subsequently, common hepatic artery and celiac axis were exposed; thus, station 7, 8a, and 9 lymph node dissection were also completed.
Comparison of Early Surgical Outcomes
In the present study, operation time, intraoperative bleeding, the number of retrieved lymph nodes, the day of first flatus, the day of first oral intake, postoperative morbidity, mortality, and the duration of the postoperative hospital stay were compared between patients who underwent LADG with complete D2 lymph node dissection (complete D2 group) and patients who underwent LADG with D1 + beta lymph node dissection (D1 + beta group). Surgery-related complications included intra-abdominal bleeding, anastomotic leakage, anastomotic bleeding, enteric injury, pancreas related infection, intra-abdominal abscess, and other complications related to the surgical procedure itself. Complications unrelated to surgery included respiratory and cardiovascular complications.
Statistic Analyses
All continuous data are presented as the mean ± standard error. Statistical analyses were performed using the chi-square test, Fisher’s exact test, Student’s t test, and Mann–Whitney U test. P < 0.05 was considered significant.
Results
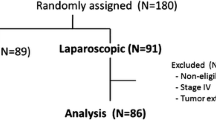
Between April 2006 and October 2008, 221 patients underwent LADG with lymph node dissection performed by one of the two specialists (F.T. or H.N) at the Cancer Institute Hospital. Of these, 179 patients underwent LADG with D1 + beta lymph node dissection (D1 + beta group), and 42 patients underwent LADG with complete D2 lymph node dissection (complete D2 group).
The patients’ characteristics and operative findings are given in Tables 1 and 2. Younger patients were more frequently observed in the complete D2 group. The operation time was significantly longer, and the number of retrieved lymph nodes was significantly larger for the complete D2 group compared to the D1 + beta group (253 ± 10 vs 224 ± 4 min; P = 0.005 and 41 ± 2 vs 35 ± 1; P = 0.002, respectively). Intraoperative bleeding was not different between groups, and intraoperative transfusion was not required in any of the patients in the present study. Conversion to open gastrectomy was required in six patients of D1 + beta group (three patients for further lymph node dissection, two patients due to severe intraabdominal adhesion, and one patient for total gastrectomy due to positive proximal margin). In complete D2 group, one patient required conversion to open surgery due to uncontrollable bleeding from the gastrocolic trunk, which happened during station 14v lymph node dissection.
The postoperative clinical course of patients in both groups is given in Table 3. The incidence of surgery-related complication was similar, and postoperative mortality was not observed. Re-operation was not required in any patient in this study.
Discussion
Open gastrectomy with D2 lymph node dissection is a standard surgical procedure for advanced gastric cancer. The procedure is widely accepted in Japan despite a large randomized controlled study conducted in Europe that failed to prove the efficacy of D2 lymph node dissection.14,16,17 LAG has been widely accepted as a treatment for early gastric cancer, and many advantages, including reduced pain and bleeding, less postoperative respiratory disturbance, early bowel movement, and short postoperative hospital stay, have been reported.2–8 Nevertheless, laparoscopic D2 lymph node dissection has not been widely investigated since it is considered to be technically difficult. LAG with D2 lymph node dissection is performed only in a few institutes by highly experienced surgeons.7,9–12,23,24 Furthermore, the quality of lymph node dissection differs between institutes, and the operation time for LAG with D2 lymph node dissection was generally longer than that for conventional open gastrectomy with D2 lymph node dissection.7,9,11
Approximately 50 operations are required to complete a surgeons’ learning curve in LAG.2,25,26 Moreover, we previously reported that standardization of each laparoscopic procedure resulted in favorable early surgical outcomes such as shortened operation time or less intraoperative bleeding, even if specialists for LAG (more than 200 cases of experience) performed surgery.21 The present study was conducted following the standardization period; in other words, feasibility of laparoscopic D2 lymph node dissection following standardization could be investigated as a preliminary study.
As expected, the operation time for the complete D2 group was longer (by about 30 min) than for the D1 + beta group, due in part to the additional lymph nodes that required dissection. Thus, in patients with middle third gastric cancer, D2 lymph node dissection is achieved by the removal of station 11p (along with the splenic artery) and 12a (along with the proper hepatic artery) lymph nodes as well as D1 + beta lymph node dissection. In addition, station 14v (surface of superior mesenteric vein at the level of lower border of pancreas) lymph nodes were dissected if the tumor was located in the lower third of the stomach.
The quality of lymph node dissection is occasionally determined from the number of retrieved lymph nodes.7,11 In the present study, the number of retrieved lymph nodes was significantly larger for the complete D2 group than for the D1 + beta group. This difference might be a result of the aggressive lymph node dissection, including dissection from the suprapancreatic area, for the complete D2 group.
The higher frequency of postoperative morbidity following complete D2 lymph node dissection was of some concern, since a European randomized trial reported a higher frequency of postoperative morbidity after D2 lymph node dissection compared with those following either D0 or D1 lymph node dissection.15,16 Intraoperative bleeding and postoperative pancreas-related infections were of particular concern for the complete D2 group since the procedure requires the exposure of major vessels and the pancreas capsule, both of which could be injured during the procedure. In the present study, one patient of complete D2 group required conversion due to uncontrollable bleeding even though all operations were performed by experienced surgeons. However, the incidence of postoperative morbidity and mortality was not different, and any other intraoperative complication was not observed. We consider, therefore, laparoscopic D2 lymph node dissection can be performed safely. However, since it is a technically difficult procedure, standardization of the laparoscopic procedure is required, and experienced surgeons should carry out the surgery.
The current study has some limitation, however, since the long-term outcome has not been evaluated, and the number of patients who underwent complete D2 dissection is relatively low. Continued monitoring of patients is required to determine the long-term efficacy of laparoscopic D2 lymph node dissection, thereby enabling its acceptance as a standard surgical procedure for advanced gastric cancer. Moreover, well-designed prospective study comparing LADG with D2 lymph node dissection and conventional open gastrectomy with D2 lymph node dissection is required as a next step.
In conclusion, LADG with complete D2 lymph node dissection is a safe procedure, provided experienced surgeons perform the surgery following standardization. To be accepted as a standard treatment, well-designed prospective study is warranted in the future.
References
Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 1994;4:146–148.
Kim MC, Jung GJ, Kim HH. Learning curve of laparoscopy-assisted distal gastrectomy with systemic lymphadenectomy for early gastric cancer. World J Gastroenterol 2005;11:7508–7511.
Adachi Y, Suematsu T, Shiraishi N, Katsuta T, Morimoto A, Kitano S, Akazawa K. Quality of life after laparoscopy-assisted Billroth I gastrectomy. Ann Surg 1999;229:49–54. doi:10.1097/00000658-199901000-00006.
Adachi Y, Shiraishi N, Shiromizu A, Bandoh T, Aramaki M, Kitano S. Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg 2000;135:806–810. doi:10.1001/archsurg.135.7.806.
Mochiki E, Nakabayashi T, Kamimura H, Haga N, Asao T, Kuwano H. Gastrointestinal recovery and outcome after laparoscopy-assisted versus conventional open distal gastrectomy for early gastric cancer. World J Surg 2002;26:1145–1149. doi:10.1007/s00268-002-6286-8.
Mochiki E, Kamiyama Y, Aihara R, Nakabayashi T, Asao T, Kuwano H. Laparoscopic assisted distal gastrectomy for early gastric cancer: Five years’ experience. Surgery 2005;137:317–322. doi:10.1016/j.surg.2004.10.012.
Miura S, Kodera Y, Fujiwara M, Ito S, Mochizuki Y, Yamamura Y, Hibi K, Ito K, Akiyama S, Nakao A. Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection: a critical reappraisal from the viewpoint of lymph node retrieval. J Am Coll Surg 2004;198:933–938. doi:10.1016/j.jamcollsurg.2004.01.021.
Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, Ponzano C. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg 2005;241:232–237. doi:10.1097/01.sla.0000151892.35922.f2.
Noshiro H, Nagai E, Shimizu S, Uchiyama A, Tanaka M. Laparoscopically assisted distal gastrectomy with standard radical lymph node dissection for gastric cancer. Surg Endosc 2005;19:1592–1596. doi:10.1007/s00464-005-0175-9.
Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Hasumi A. Laparoscopic total gastrectomy with distal pancreatosplenectomy and D2 lymphadenectomy for advanced gastric cancer. Gastric Cancer 1999;2:230–234. doi:10.1007/s101200050069.
Ziqiang W, Feng Q, Zhimin C, Miao W, Lian Q, Huaxing L, Peiwu Y. Comparison of laparoscopically assisted and open radical distal gastrectomy with extended lymphadenectomy for gastric cancer management. Surg Endosc 2006;20:1738–1743. doi:10.1007/s00464-006-0031-6.
Kim MC, Kim HH, Jung GJ. Surgical outcome of laparoscopy-assisted gastrectomy with extraperigastric lymph node dissection for gastric cancer. Eur J Surg Oncol 2005;31:401–405. doi:10.1016/j.ejso.2004.11.007.
Nakajima T. Gastric cancer treatment guidelines in Japan. Gastric Cancer 2002;5:1–5. doi:10.1007/s101200200000.
Hartgrink HH, van de Velde CJ, Putter H, Bonenkamp JJ, Klein Kranenbarg E, Songun I, Welvaart K, van Krieken JH, Meijer S, Plukker JT, van Elk PJ, Obertop H, Gouma DJ, van Lanschot JJ, Taat CW, de Graaf PW, von Meyenfeldt MF, Tilanus H, Sasako M. Extended lymph node dissection for gastric cancer: who may benefit? Final results of the randomized Dutch gastric cancer group trial. J Clin Oncol 2004;22:2069–2077. doi:10.1200/JCO.2004.08.026.
Bonenkamp JJ, Songun I, Hermans J, Sasako M, Welvaart K, Plukker JT, van Elk P, Obertop H, Gouma DJ, Taat CW. Randomised comparison of morbidity after D1 and D2 dissection for gastric cancer in 996 Dutch patients. Lancet 1995;345:745–748. doi:10.1016/S0140-6736(95)90637-1.
Cuschieri A, Fayers P, Fielding J, Craven J, Bancewicz J, Joypaul V, Cook P. Postoperative morbidity and mortality after D1 and D2 resections for gastric cancer: preliminary results of the MRC randomised controlled surgical trial.The Surgical Cooperative Group. Lancet 1996;347:995–999. doi:10.1016/S0140-6736(96)90144-0.
Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, Sydes M, Fayers P. Patient survival after D1 and D2 resections for gastric cancer: long-term results of the MRC randomized surgical trial. Surgical Co-operative Group. Br J Cancer 1999;79:1522–1530. doi:10.1038/sj.bjc.6690243.
Kodera Y, Schwarz RE, Nakao A. Extended lymph node dissection in gastric carcinoma: where do we stand after the Dutch and British randomized trials? J Am Coll Surg 2002;195:855–864. doi:10.1016/S1072-7515(02)01496-5.
Maruyama K, Okabayashi K, Kinoshita T. Progress in gastric cancer surgery in Japan and its limits of radicality. World J Surg 1987;11:418–425. doi:10.1007/BF01655804.
Lee SW, Shinohara H, Matsuki M, Okuda J, Nomura E, Mabuchi H, Nishiguchi K, Takaori K, Narabayashi I, Tanigawa N. Preoperative simulation of vascular anatomy by three-dimensional computed tomography imaging in laparoscopic gastric cancer surgery. J Am Coll Surg 2003;197:927–936. doi:10.1016/j.jamcollsurg.2003.07.021.
Hiki N, Fukunaga T, Yamaguchi T, Nunobe S, Tokunaga M, Ohyama S, Seto Y, Yoshiba H, Nohara K, Inoue H, Muto T. The benefits of standardizing the operative procedure for the assistant in laparoscopy-assisted gastrectomy for gastric cancer. Langenbecks Arch Surg 2008;393:963–971. doi:10.1007/s00423-008-0374-7.
Japanese Gastric Cancer A. Japanese Classification of Gastric Carcinoma—2nd English Edition. Gastric Cancer 1998;1:10–24.
Huscher CG, Mingoli A, Sgarzini G, Brachini G, Binda B, Di Paola M, Ponzano C. Totally laparoscopic total and subtotal gastrectomy with extended lymph node dissection for early and advanced gastric cancer: early and long-term results of a 100-patient series. Am J Surg 2007;194:839–844. doi:10.1016/j.amjsurg.2007.08.037, discussion 844.
Azagra JS, Ibanez-Aguirre JF, Goergen M, Ceuterick M, Bordas-Rivas JM, Almendral-Lopez ML, Moreno-Elola A, Takieddine M, Guerin E. Long-term results of laparoscopic extended surgery in advanced gastric cancer: a series of 101 patients. Hepatogastroenterology 2006;53:304–308.
Lee SI, Choi YS, Park DJ, Kim HH, Yang HK, Kim MC. Comparative study of laparoscopy-assisted distal gastrectomy and open distal gastrectomy. J Am Coll Surg 2006;202:874–880. doi:10.1016/j.jamcollsurg.2006.02.028.
Fujiwara M, Kodera Y, Miura S, Kanyama Y, Yokoyama H, Ohashi N, Hibi K, Ito K, Akiyama S, Nakao A. Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection: a phase II study following the learning curve. J Surg Oncol 2005;91:26–32. doi:10.1002/jso.20166.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tokunaga, M., Hiki, N., Fukunaga, T. et al. Laparoscopy-Assisted Distal Gastrectomy with D2 Lymph Node Dissection Following Standardization—A Preliminary Study. J Gastrointest Surg 13, 1058–1063 (2009). https://doi.org/10.1007/s11605-009-0840-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-009-0840-8