Abstract
Objective
Ileal pouch anal anastomosis (IPAA) is the procedure of choice for most patients requiring surgery for ulcerative colitis and familial adenomatous polyposis because of its perceived improvement in health-related quality of life (HRQL). The aims of this cross-sectional study were to validate an English version of the Padova Inflammatory Bowel Disease Quality of Life questionnaire (PIBDQL) in patients undergoing IPAA and to investigate the pre- and postoperative predictors of long-term HRQL.
Materials and Methods
In May 2005, the English version of the PIBDQL, Short Inflammatory Bowel Disease Questionnaire, and the SF-36 were mailed to 1,379 patients who underwent IPAA at the Mount Sinai Hospital between 1982 and 2004. The test–retest reliability, internal consistency, construct validity, and discriminative ability of the English version of the PIBDQL were assessed.
Results
Nine hundred fifty-five patients (69%) (475 female, 480 male; mean, age 43 years) returned the questionnaires. The mean PIBDQL score was 21.1 (3.4), suggesting good quality of life. Test–retest reliability [intraclass correlation coefficient (ICC) = 0.784] and internal consistency (Cronbach’s α = 0.83) were good. Construct validity and discriminative ability of the English version of PIBDQL were adequate. Multivariate analysis revealed that women (p < 0.01) and Crohn’s disease patients (p < 0.01) had significantly worse PIBDQL scores.
Conclusions
The English version PIBDQL is a reliable and valid disease-specific instrument for assessing quality of life in patients with IPAA. In this series, female gender and CD were significant predictors of worse HRQL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ileal pouch-anal anastomosis (IPAA) is the procedure of choice for most patients requiring surgery for ulcerative colitis (UC) and selected patients with familial adenomatous polyposis (FAP).1–3 Due to refinements in technique and increased surgical experience, the complication rate has decreased considerably,4 and long-term outcome appears to be good.1,2,5–8 Patients embraced IPAA almost immediately because it eliminated the need for a permanent stoma. As well, several studies using generic instruments such as the Short Form 36 (SF-36) and the Cleveland Global Quality of Life score (CGQL) have documented excellent HRQL compared to UC patients and the normal population.9–14 However, the limitation of these instruments is that they lack discriminative ability.15,16 As shown by Ko et al.,17 there is a correlation between bowel function and HRQL, and generic instruments may fail to detect smaller differences in outcome.16 The Inflammatory Bowel Disease Questionnaire (IBDQ) or its shortened version (SIBDQ), have been used to measure HRQL after IPAA.18,19 However, this instrument was developed for use in trials assessing medical therapies in patients with inflammatory bowel disease and is not specific to patients with IPAA.
The Padova Inflammatory Bowel Disease Quality of Life instrument (PIBDQL) was developed in 1995 to assess HRQL in patients with inflammatory bowel disease.20 This questionnaire has been shown to be reliable in healthy controls and in UC and IPAA patients.21,22 It consists of items in four domains: intestinal symptoms, systemic symptoms, emotional function, and social function. In previous studies this instrument was shown to be sensitive to changes in the quality of life in Italian patients following IPAA.21–23
The aims of the present study were to validate an English version of the PIBDQL questionnaire in patients with UC, Crohn’s disease (CD), indeterminate colitis (IC) and FAP who had IPAA; secondly, to assess its test-retest reliability: and thirdly, to investigate the effects of various pre and post operative factors on HRQL.
Materials and Methods
Thirteen hundred seventy-nine patients who had the IPAA at the Mount Sinai Hospital between 1982 and 2004 were mailed a package containing the English version of the PIBDQL, the SIBDQ, and the SF-3624 in May 2005 as well as an explanatory letter and a self-addressed return envelope. A reminder card was mailed to all patients who had not returned the questionnaires 1 month after the first mailing. As well, 2 weeks following return of the fist 100 questionnaires, a second PIBDQL was sent to these patients to assess the test–retest reliability of the instrument. The study was approved by the Research Ethics Committee of the Mount Sinai Hospital.
Instruments
The PIBDQL instrument was developed at the University of Padova, Italy to assess quality of life in patients with IBD20 and has been used predominantly in patients with UC having IPAA21–23 and patients with CD undergoing surgery.25 The instrument consists of 29 items, which explore intestinal symptoms (eight questions; score range, 0–24), systemic symptoms (seven questions; score range, 0–21), emotional function (nine questions; score range, 0–27), and social function (five questions; score range, 0–15). Possible scores for each item range from 0 to 3 and correspond to never or hardly ever, sometimes, often, and always or nearly always. The total score can range from 0 to 87 with a higher score indicating a worse HRQL. The translation–back-translation technique was used to translate the PIBDQL into English from Italian. The instrument has previously been shown to be valid if self-administered.
The SIBDQ is a disease-specific health-related quality of life questionnaire developed by Irvine and colleagues at McMaster University and is a shortened version of the IBDQ.26 It consists of four domains including intestinal symptoms (three questions), systemic symptoms (two questions), emotional function (three questions), and social function (three questions). Each item is scored on a scale of 1 to 7 (1, worst; 7, best) so the total score may range from 7 to 70,27 with higher scores indicating better quality of life.
The Medical Outcomes Study 36-Item Short Form Health Survey (SF-36) is a generic HRQL instrument. There are seven domains including physical functioning, physical health, bodily pain, general health, vitality, social functioning, emotional status, and mental health.28 Scores may range from 0 to 100 for each domain with a higher score indicating a better health status. The SF-36 has been used extensively to assess the HRQL in the normal population and in various disease states. As well, it has been used previously to assess HRQL in IPAA patients.8,12,13
Data Analysis
Preoperative, surgical, and outcome data on all patients having a IPAA at the Mount Sinai Hospital are entered prospectively into the Mount Sinai Hospital IBD Database using Microsoft Access software. Questionnaire data obtained during this study were also entered into the database. The statistical analysis was performed using both Microsoft Excel and SAS 8.0 software (SAS Institute Inc., Cary, NC, USA). Data are presented as mean and SD. Differences were tested using two-tailed Student’s t test for continuous data and Yates chi-square test for proportions.
Test–retest reliability was assessed using the ICC. The internal consistency of the English version of the PIBDQL was investigated with the Cronbach’s α.29 A Cronbach’s α of >0.8 indicates excellent internal consistency.
Construct validity was assessed by measuring the amount of correlation between the domain scores of the PIBDQL with the corresponding domains of the SF-36 and SIBDQ using the Spearman correlation coefficient.
To determine which variables are associated with HRQL in patients who had a IPAA, the following 12 variables were analyzed: gender, age at diagnosis (for inflammatory bowel disease patients), age at the first operation, current age, diagnosis (ulcerative colitis, Crohn’s disease, indeterminate colitis, or famililial polyposis), duration of disease, time in months since last operation (IPAA or closure of ileostomy for those patients having a defunctioning ileostomy), pouch type (J or S), IPAA type (stapled or handsewn), postoperative complications, postoperative anastomotic leak, and previous combined abdominal and perineal reconstructive procedure. Univariate analysis of variance method (ANOVA) was performed for each putatitive predictor of PIBDQL, and multiple linear regression was then performed modeling PIBDQL on all predictors that were significant in the univariate analysis. Statistically significant predictors from the multiple regression model were then analyzed with Tukey Honestly Significant Difference (HSD) post hoc test to identify differences between levels of multicategory predictors. A level of p < 0.05 was considered significant for all analyses.
Sample Size Calculation
Setting α (the probability of a type I error) at 0.05 (two-tailed), β (the probability of a type II error) at 0.10, and the smallest detectable r (expected Pearson correlation coefficient, effect size) at 0.20, a sample size of 259 patients was calculated to be adequate for assessing construct validity.
Setting α at 0.05 (two-tailed), β at 0.20, the smallest detectable R 2 (the proportion of variation in the HRQL outcome explained by this model) at 0.02 with the consequent effect size at 0.0204 and a maximum number of predictors at 10, the subsequent sample size was calculated to be 802 patients to be adequate for multiple regression analysis to assess the significant predictors of long-term HRQL.
Results
Patients Characteristics
Nine hundred fifty-five (69%) of the 1,379 patients returned the questionnaires. The characteristics of the respondents and those who did not return the questionnaires were similar as shown in Table 1. The majority of patients had surgery for ulcerative colitis. The proportion of male and female patients in the cohort was similar. Over 80% of patients had a J pouch constructed and a stapled ileoanal anastomosis. Over 50% experienced at least one complication. Nine percent of patients experienced an ileoanal anastomotic leak.
Validation of the English Version of PIBDQL
Of the 955 patients who returned the questionnaires, only 862 (90.3%) patients provided complete data for PIBDQL questions. The mean total PIBDQL score was 21.1 (13.4), indicating a fairly good quality of life. The mean domain scores were 7.8 (4.1) for intestinal symptoms, 6.1 (4.5) for systemic symptoms, 5.0 (4.8) for emotional function, and 2.3 (2.8) for social function.
Seventy-eight of the 100 patients who were sent a second questionnaire package to evaluate test–retest reliability returned it with complete data on PIBDQL at a mean time of 20 (5) days following completion of the first assessment. Test–retest reliability was excellent for the instrument overall as well as for each of the four domains as shown in Table 2. To determine internal consistency of the English PIBDQL, Cronbach’s α was calculated on the 862 questionnaires where there were complete data. Cronbach’s α was 0.83 demonstrating good internal consistency.
Construct validity of the English PIBDQ was analyzed with Spearman correlation test because of the distribution of the PIBDQ scores. The English PIBDQ was correlated with the generic SF-36 and the disease-specific SIBDQ. The English PIBDQ single item and overall scores correlated well with all SF-36 and SIBDQ domains (p < 0.0001) as shown in Tables 3 and 4.
Factors Influencing Quality of Life
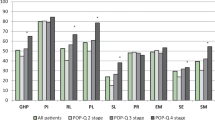
Twelve variables that might potentially affect quality of life were assessed: gender, age at diagnosis (for inflammatory bowel disease patients), age at the first operation, current age, diagnosis (ulcerative colitis, Crohn’s disease, indeterminate colitis, or famililial polyposis), duration of disease, time in months since last operation (IPAA or closure of ileostomy for those patients having a defunctioning ileostomy), pouch type (J or S), IPAA type (stapled or handsewn), postoperative complications, postoperative anastomotic leak, and previous combined abdominal and perineal reconstructive procedure. As shown in Table 5, only gender, diagnosis, length of follow-up, pouch type, IAA type, and previous pouch reconstruction seemed to predict quality of life of patients in univariate comparisons. These predictors were then included in a generalized linear model. On multivariate regression analysis, female patients were found to have worse HRQL than male patients on the PIBDQL. There were five categories in the diagnosis variable (UC, CD, ID, FAP, other). The Tukey HSD post hoc test confirmed that the PIBDQL scores for CD patients were significantly higher (and so worse) than those for UC patients and those for FAP patients. PIBDQ score also showed a trend toward a significant linear relationship with whether a patient had had pouch reconstruction or not (p < 0.06). ANOVA and t test showed that patients who had their pouch reconstructed scored significantly worse.
Discussion
The complete excision of the diseased bowel with the virtual elimination of the risk of cancer and the preservation of the natural route of defecation make IPAA the procedure of choice for the elective treatment of most patients requiring surgery for UC.30,31 As well, IPAA is an option for patients with familial polyposis and indeterminate colitis.11,24 Surgical outcomes are good in most patients.31 As well, functional results and quality of life are also important outcome measures.5,16
This study confirmed the reliability and validity of the PIBDQL to assess quality of life in patients having IPAA. The test–retest reliability of the English PIBDQL was assessed by comparing results obtained on two different occasions approximately 20 days apart. All but three patients who were assessed in this part of the study had had a pouch for more than 1 year so it is likely that their results are stable.1,26 The test–retest reliability verified the homogeneity of the English PIBDQL scores, as the four domains and the overall score showed no statistically significant difference. Similarly, this study showed that the instrument has high internal consistency.34 As well, the internal consistency was comparable to that reported for the Cleveland Global Quality of Life score.1
Construct validity was analyzed through the correlation of the English PIBDQL with the generic SF-36 and with the disease-specific SIBDQ. As expected, the English PIBDQL scores correlated moderately well with all SF-36 and SIBDQ domains. As one would expect, the correlations between the intestinal symptoms scores and the single item scores of the SF-36 were lower. Thus, it can be deduced that this questionnaire performs better in patients having IPAA. It measures what it is meant to measure but in a slightly different way from the previously validated instruments.
The discriminative ability of the PIBDQL was demonstrated analyzing the predictors of HRQL. Gender and diagnosis were found to affect PIBDQL scores. Previous studies have not shown that women have worse quality of life following IPAA. In this series, female patients experienced the same rate of postoperative complications and IAA leaks, and they reported the same stool frequency as male patients but they were significantly younger, and more women had had a pouch reconstruction. This may account for the observed difference. Furthermore, a recent study from the Academic Medical Centre of Amsterdam pointed out that body image and cosmesis are more important to female patients who undergo IPAA.35
As measured by the English PIBDQL, CD patients had a significantly worse long-term HRQL compared to UC or FAP patients. Patients with Crohn’s disease are more likely to require excision of their pouch,24 but it appears that those who still have their pouch also have a worse quality of life.
Patients who had had a pouch reconstruction had significantly worse PIBDQL scores on univariate analysis and a trend toward significance on multivariate analysis. Intestinal symptoms and social function were the domains that were poorer in this group of patients. These patients tend to have poorer functional results likely due to stretching of and injury to the anal sphincter at reconstructive surgery.36 Poorer functional results tend to impact negatively on quality of life, so these results are not unexpected. That the results were not significant on multivariate analysis is likely due to the relatively small number of patients who had had reconstructive surgery in this series.
This study showed that the English version of the PIBDQL is useful in determining predictors of poor HRQL outcome after IPAA. In the Italian version, this questionnaire was also shown to be valid in assessing HRQL of patients after IPAA. In fact, studies performed with generic instruments such as CGQL or SF-36 have claimed that the HRQL is equal in patients with IPAA compared to healthy controls.1,13 However, CGQL failed to differentiate IPAA patients from healthy controls and patients with mild UC or in remission from moderate UC. Studies using SF-36 showed a difference between IPAA and UC patients only because patients were all affected by severe UC.13,23 Thus, it seems that generic instruments may lack discriminative ability, and comparisons between patient groups using a non-disease specific instrument should be interpreted with caution.
In conclusion, this study demonstrated that quality of life is good in most patients following IPAA. Furthermore, the English version of the PIBDQL questionnaire was shown to have good test–retest reliability, internal consistency, and construct validity. Thus, this instrument can be used to assess quality of life in this cohort of patients.
References
Fazio VW, O’Riordain MG, Lavery IC, et al. Long term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg 1999;230(4):575–586. doi:10.1097/00000658-199910000-00013.
Robb B, Pritts T, Gang G, et al. Quality of life in patients undergoing ileal pouch anal anastomosis at the University of Cincinnati. Am J Surg 2002;183:343–360. doi:10.1016/S0002-9610(02)00804-8.
Parks AG, Nicholls RJ. Proctocolectomy without ileostomy fro ulcerative colitis. BMJ 1978;2:85–88.
Fazio VW, Tekkis PP, Remzi F, et al. Quantification of risk for pouch failure after ileal pouch anal anastomosis surgery. Ann Surg 2003;238:605–617.
McLeod RS, Baxter NN. Quality of life of patients with inflammatory bowel disease after surgery. World J Surg 1998;28:375–381. doi:10.1007/s002689900400.
Pemberton JH, Phillips SF, Ready RR, et al. Quality of life after Brooke ileostomy and ileal pouch-anal anastomosis. Comparison of performance status. Ann Surg 1989;209:620–628. doi:10.1097/00000658-198905000-00015.
Karlbolm U, Raab Y, Ejerblad S, et al. Factors influencing the functional outcome of restorative proctocolectomy in ulcerative colitis. Br J Surg 2000;87:1401–1408. doi:10.1046/j.1365-2168.2000.01533.x.
Provenzale D, Shearin M, Phillips-Bute BG, et al. Health-related quality of life after ileoanal pull-through evaluation and assessment of new health status measures. Gastroenterology 1997;113:7–14. doi:10.1016/S0016-5085(97)70074-X.
Delaney CP, Dadvand B, Remzi FH, et al. Functional outcome, quality of life and complication after ileal pouch-anal anastomosis in selected septuagenarians. Dis Colon Rectum 2002;45(7):890–894. doi:10.1007/s10350-004-6323-9.
Delaney CP, Fazio VW, Remzi FH, et al. Prospective, age related analysis of surgical results functional outcome and quality of life after ileal pouch-anal anastomosis. Ann Surg 2003;238:221–228.
Delaney CP, Remzi FH, Gramlich T, et al. Equivalent function, quality of life and pouch survival rates after ileal pouch-anal anastomosis for indeterminate and ulcerative colitis. Ann Surg 2002;236:43–48. doi:10.1097/00000658-200207000-00008.
Tiainen J, Matikainen M. Health related quality of life after J pouch-anal anastomosis for ulcerative colitis: long term results. Scand J Gastroenterol 1999;34(6):601–605. doi:10.1080/003655299750026065.
Muir AJ, Edwards LJ, Sanders MS, et al. A prospective evaluation of health related quality of life after ileal pouch anal anastomosis for ulcerative colitis. Am J Gastroenterol 2001;95(5):1480–1485. doi:10.1111/j.1572-0241.2001.03801.x.
Coffey JC, Winter DC, Neary P, et al. Quality of life after ileal pouch-anal anastomosis: an evaluation of diet and other factors using the Cleveland global Quality of life instrument. Dis Colon Rectum 2002;45(1):30–38.
Irvine EJ. Quality of life: measurement in inflammatory bowel disease. Scand J Gastroenterol Suppl 1993;199:36–39. doi:10.3109/00365529309098355.
McLeod RS. Quality of life measurement in the assessment of surgical outcome. Adv Surg 1999;33:293–309.
Ko CY, Rusin LC, Schoetz DJ, et al. Long term outcomes of ileal pouch anal anastomosis: the association of bowel function and quality of life 5 years after surgery. J Surg Res 2001;98:102–107. doi:10.1006/jsre.2001.6171.
Hauser W, Dietz N, Steder-Neukamm U, Janke KH, Stallmach A. Biopsychosocial determinants of health-related quality of life after ileal pouch anal anastomosis for ulcerative colitis. Inflamm Bowel Dis 2004;10(4):399–407. doi:10.1097/00054725-200407000-00011.
Barton JG, Paden MA, Lane M, Postier RG. Comparison of postoperative outcomes in ulcerative colitis and familial polyposis after ileal-anal pouch anastomosis. Am J Surg 2001;182(6):616–620. doi:10.1016/S0002-9610(01)00795-4.
Martin A, Dinca M, Leone L, et al. Quality of life after proctocolectomy and ileo anal anastomosis for severe ulcerative colitis. Am J Gastroenterol 1998;93(2):166–169. doi:10.1111/j.1572-0241.1998.00166.x.
Scarpa M, Angriman I, Ruffolo C, et al. Health related quality of life after restorative proctocolectomy for ulcerative colitis: long-term results. World J Surg 2004;58(2):122–126.
Martin A, Leone L, Fries W, et al. Quality of life in inflammatory bowel disease. Ital J Gastroenterol 1995;27:450–454.
Scarpa M, Ruffolo C, Polese L, Martin A, D’Incà R, Sturniolo GC, D’Amico DF, Angriman I. Quality of life after restorative proctocolectomy for ulcerative colitis: different questionnaires lead to different interpretations. Arch Surg 2007;142(2):158–165. doi:10.1001/archsurg.142.2.158.
Brown CJ, MacLean AR, Cohen Z, MacRae HM, O’Connor BI, McLeod RS. Crohn’s disease and indeterminate colitis and the ileal pouch anal-anastomosis: outcomes and patterns of failure. Dis Colon Rectum 2005;48:1542–1549. doi:10.1007/s10350-005-0059-z.
Scarpa M, Ruffolo C, D’Incà R, Filosa T, Bertin E, Ferraro S, Polese L, Martin A, Sturniolo GC, Frego M, D’Amico DF, Angriman I. Health related quality of life after ileo-colonic resection for Crohn’s disease: long-term results. Inflamm Bowel Dis. 2007;13(4):462–469. doi:10.1002/ibd.20080.
Guyatt G, Mitchell A, Irvine EJ, Singer J, Williams N, Goodacre R, Tompkins C. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterol 1989;96(3):804–810.
Irvine EJ, Zhou Q, Thompson AK. CCRPT Investigators. The Short Inflammatory Bowel Disease Questionnaire: a quality of life instrument for community physicians managing inflammatory bowel disease. Am J Gastroenterol 1996;91(8):1571–1578.
Stewart AL, Hays RD, Ware JE. The MOS short form general health survey: reliability and validity in patient population. Med Care 1988;36:925–930.
Bland JM, Altman DG. Cronbach’s alpha. BMJ 1997;314:572.
Fazio VW, Ziv Y, Church JM, et al. Ileal pouch-anal anastomosis complications and function in 1005 patients. Ann Surg 1995;222:120–127. doi:10.1097/00000658-199508000-00003.
Michelassi F, Lee J, Rubin M, et al. Long term functional results after ileal pouch anal restorative proctocolectomy for ulcerative colitis. Ann Surg 2003;238(3):433–445.
Bambrick M, Fazio VW, Hull TL, Pucel G. Sexual function following restorative proctocolectomy in women. Dis Colon Rectum 1996;39(6):610–614. doi:10.1007/BF02056936.
Tiainen J, Matikainen M, Hilunen KM. Ileal J pouch-anal anastomosis, sexual dysfunction and fertility. Scand J Gastroenterol 1999;34(2):185–188. doi:10.1080/00365529950173069.
Streiner GL, Norman DR. Health Measurement Scales: A Practical Guide to their Development and Use. Oxford: Oxford University Press, 1990.
Polle SW, Dunker MS, Slors JF, Sprangers MA, Cuesta MA, Gouma DJ, Bemelman WA. Body image, cosmesis, quality of life, and functional outcome of hand-assisted laparoscopic versus open restorative proctocolectomy: long-term results of a randomized trial. Surg Endosc 2007;21(8):1301–1307. doi:10.1007/s00464-007-9294-9.
Cohen Z, Smith D, McLeod R. Reconstructive surgery for pelvic pouches. World J Surg 1998;22(4):342–346. doi:10.1007/s002689900394.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scarpa, M., Victor, C.J., O’Connor, B.I. et al. Validation of an English Version of the Padova Quality of Life Instrument to Assess Quality of Life Following Ileal Pouch Anal Anastomosis. J Gastrointest Surg 13, 416–422 (2009). https://doi.org/10.1007/s11605-008-0775-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0775-5