Abstract
Introduction
The role of ablation for hepatic colorectal metastases (HCM) continues to evolve as ablation technology changes and systemic chemotherapy improves. Our aim was to evaluate the therapeutic efficacy of radiofrequency ablation (RFA) of HCM compared to surgical resection.
Methods
A retrospective review of our 1,105 patient prospective hepatic database from August 1995 to July 2007 identified 192 patients with only hepatic resection or only ablation for HCM.
Results
Patients who underwent RFA were similar to resection patients based on a similar Fong score (1.8 vs. 2.1 p = 0.28), presence of extrahepatic disease (15% vs. 9% p = 0.19), mean number of hepatic lesions (2.8 vs. 2.1 p = 0.14), and prior chemotherapy (67% vs. 60% p = 0.33). Median time to recurrence was shorter with ablation than resection (12.2 vs. 31.1 months; p < 0.001). Recurrence at the ablation–resection site was more common with ablation than resection occurring 17% vs. 2% (p ≤ 0.001) of the time, respectively. Distant recurrence in the liver was also more common with ablation occurring in 33% of patients vs. 14% for resection (p = 0.002).
Conclusions
Surgical resection is associated with a lower chance of recurrence and a longer disease-free interval than RFA and should remain the treatment of choice in resectable HCM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hepatic metastasis of colorectal cancer is quite common occurring at some time in 23% of all of the 190,000 colorectal patients diagnosed each year.1 While systemic chemotherapy can slow growth and even cause regression of hepatic metastases, long-term survival without local therapy is unlikely. Surgical resection of hepatic metastases continues to remain the optimal first-line treatment for hepatic colorectal metastases. Other therapies that have been used are ethanol injection and cryotherapy which have been supplanted by radiofrequency ablation (RFA) and microwave ablation. The role of RFA of hepatic colorectal metastases continues to evolve as the technology evolves and experience with RFA matures.2 There are many conflicting published series comparing efficacy of RFA and resection with some authors advocating a prospective trial comparing RFA and resection while others maintain that RFA is inferior to resection and patients should not be put at risk to compare the two therapies. The goal of this study was to evaluate the comparative therapeutic efficacy of RFA and surgical resection for hepatic colorectal metastases.
Methods
A review of a 1,105 patient prospective hepatic–pancreaticobiliary database from August 1995 to July 2007 was done under IRB approval to identify patients who had either only a resection or only an RFA of hepatic colorectal metastases. All patients included in this study had single lobar involvement. Patients who underwent combination resection and ablation or underwent extrahepatic organ resection and ablation or resection were excluded.
The decision to perform resection or RFA was determined by the treating surgeon at his discretion. In the patients undergoing hepatic resections, anatomic segmental liver resections were performed and classified as described by Couinaud3. Nonanatomical resections were performed when judged appropriate by the attending surgeon. For patients with disease that was felt to be unresectable because of the number, distribution, and/or location of the tumors or because of patient comorbid factors, ablation was performed. Standard preoperative evaluation of patients with metastatic colorectal cancer included three-phase computed tomography (CT) of the abdomen and pelvis and chest roentgenogram. Prior systemic chemotherapy of any type and duration was allowed. RFA was performed using intraoperative ultrasound guidance to ensure that at least a 1-cm ablation margin was achieved around the tumors.4,5
Postoperative complications and the length of hospital stay were prospectively evaluated. Complications were graded according to a standard five-point grading scale and have been utilized prospectively since June 2002.4,6 All in-hospital and 90-day postoperative complications were evaluated with the highest severity level recorded. Perioperative complications were defined as complications occurring within 30 days of the operation. RFA patients had one early CT (<1 month from RFA) to ensure RFA success and were then imaged per standard while resection patients were imaged per standard. Standard CT follow-up was utilized every 3 months for the first year and then every 6 months thereafter. Data were censored at the last recorded patient contact if an end point was not reached. Recurrence was also evaluated using serological markers and positron emission tomography scan. A recurrence was the reoccurrence of viable tumor by radiologic CT criteria of a vascular mass. In the event of subsequent hepatic therapy for recurrence of disease, only the first procedure was used for the purposes of this study. Clinicopathologic data along with perioperative complications were recorded. Analysis of data was done using JMP 4.0 and SPSS version 16.0.
A review of all publications in peer review journals in the English Language from 1995 to 2007 was done. Unpublished studies and abstracts presented at national and international meetings were excluded. Trials were identified by conducting a comprehensive of Medline, Embase, Science Citation Index, Current Contents, and PubMed databases, using medical subject headings “colorectal liver metastasis,” “radiofrequency ablation,” “hepatectomy,” “colorectal recurrence,” and “comparative study.” A manual search of the abstracts was performed to identify for inclusion in this review. Only articles that included a comparative evaluation of hepatectomy to radiofrequency ablation during the same time interval, ablation recurrence, nonablation recurrence, resection margin recurrence, disease-free survival, and overall survival were included.
Results
Review of the database identified 308 patients who underwent hepatic resection and/or RFA for metastatic colorectal cancer with curative intent. One hundred and sixteen patients were excluded from this analysis because they had a concomitant resection and RFA at the time of their first hepatic procedure. Sixty-six patients had only hepatic RFA with curative intent while 126 patients underwent only resection with curative intent. Of the patients who had a resection, 106 had an anatomic resection; six had a nonanatomic resection; 12 had a combined anatomic and nonanatomic resection, and two had an unknown type of resection. The most common anatomic resection was a right lobectomy (N = 73) followed by extended right hepatectomy (N = 18) and left lateral segmentectomy (N = 13), left lobectomy (n = 10), extended left hepatectomy (n = 4), central resection (n = 5), caudate resection (n = 4), segmentectomy (n = 11), and bisegmentectomy (n = 5). Patients who underwent RFA were more likely to have a smaller hepatic lesion (3.2 vs. 5.3 cm, p < 0.001) and more likely to have more than one hepatic lesion (59% vs. 41%, p = 0.01) than patients undergoing resection (Table 1). There was no difference in the location or the number of involved hepatic segments between the two groups (Table 2). All other clinicopathologic characteristics were similar between the two groups (Table 3).
While there was no difference in the percentage of patients experiencing any complication (Table 3), resection patients were more likely to have a major complication (29% vs. 10%, p = 0.003). They also had a longer hospital stay (9.8 vs. 6.6 days, p = 0.014) and were more likely to receive a blood transfusion during the hospital stay (21% vs. 3%, p < 0.001).
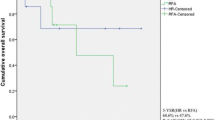
The median follow-up for all patients was 20.0 months. Recurrence was more common in patients undergoing RFA compared to resection (71% vs. 46%, p < 0.001). The patterns of recurrence were also different in patients who underwent RFA compared to resection. In the RFA group, recurrence was more common at the RFA–resection site (17% vs 2%, p < 0.001), in the same lobe as the RFA–resection (42% vs. 3%, p < 0.001), and in the liver distant to the RFA–resection (33% vs. 14%, p = 0.002). There was no difference in the percentage of patients experiencing extrahepatic recurrence (Table 3). In addition to being more likely to have a recurrence, RFA patients also recurred earlier than resection patients (median 12.2 vs. 31.1 months, p < 0.0005; Table 4, Fig. 1). When recurrence was stratified by extrahepatic recurrence, recurrence at the RFA–resection site, or distant hepatic recurrence, the median time to recurrence was always longer in the resection patients than the RFA patients.
Despite the differences in recurrence, there was no difference in survival with 49% of the RFA patients having died at last follow-up vs. 45% of the resection patients (p = 0.67). There was a trend towards improved overall survival in the resection patients with an increased median survival (36.4 vs. 27.0 months); however, this was not statistically significant (p = 0.31; Fig. 2). When only patients who did not have extrahepatic disease at the time of RFA or resection were analyzed, the median survival was 26.4 months for RFA patients and 38.3 months for resection patients (p = 0.13). The trend for increased survival was most evident when only patients who did not recur were analyzed with a median survival of 21.6 vs. 53.8 for patients undergoing RFA vs. resection respectively (p = 0.10; Fig. 3). Overall 5-year survival was statistically the same at 21% for the RFA group and 23% for the resection group.
In a review of the peer-reviewed literature that met our inclusion criteria, three articles were identified (Table 5). In comparing the literature to our results, there were similar rates of recurrence for both RFA and non-RFA recurrence. In a summary of all the data reported, resection still has a lower rate of liver recurrence when compared to RFA (Table 5).
Discussion
Resection of colorectal metastases to the liver remains the treatment of choice when possible. Although there was not a difference in overall survival between RFA and resection in our study, there were consistent patterns that favored the resection group. Patients who underwent resection were less likely to recur and had a longer disease-free interval despite having a larger-sized lesion. The similarity of the Kaplan Meier survival curves for the first 60 months made the 9.4-month median survival advantage in the resection group nonsignificant. After 72 months, the curves separate with the RFA curve going to zero while the resection curve levels out and continues to 142 months at 17%. Potentially, with a larger number of patients and longer follow-up, differences in survival may become statistically significant.
It has already been shown that RFA can be safely done for unresectable hepatic tumors.7,8 While some series have shown RFA to be equivalent to resection, others have found RFA to be inferior to resection based on overall survival.9–11 All of these series, like ours, are case series comparing RFA for unresectable colorectal hepatic metastasis to resection and thus subject to a selection bias since the groups are not equivalent. The 5-year survival of 21% reported here is comparable to other published 5-year survival rates for unresectable hepatic colorectal metastasis treated with RFA of 14% to 31%.10,12–14 Our 5-year survival of 21% following resection is also lower than others have reported.9–11
Our local recurrence at the RFA site of 17% fits well within the widely varying published rates of 2% to 40%.7,9–11,14–18 All of our RFAs were done surgically (open or laparoscopic) allowing for accurate probe placement under ultrasound guidance. Our local recurrence rate of 2% following resection is at the low end of reported rates varying from 3.8% to 10.4% and indicates that our resections are adequate.15,19
In addition to differences in overall recurrence rates, the differences in the pattern of recurrence were interesting. Invariably, RFA patients were more likely to recur nearer the RFA site. This could be due to incomplete ablation secondary to lesion size, heat sink effect, or the limitations of the modality. Alternatively, the lower local failure rate with resection may be due to removing hepatic parenchyma that is at a higher risk than the rest of the liver for recurrence. Interestingly, RFA patients were also more likely to fail in the liver distant to the RFA site. As expected, local therapy in the liver did not affect the rate of or time to extrahepatic recurrence.
The lack of survival benefit despite a decreased risk of recurrence and increased time to recurrence in the resection group is likely multifactorial. First, when there is a hepatic recurrence in the absence of extrahepatic disease, a second RFA or resection can often be done. Second, the number of options and efficacy of adjuvant chemotherapy has increased dramatically over the recent years. Finally, there is a selection difference between the two groups even though it is not evident when the frequency of comorbidities is examined (Table 3). Our institutional bias has always been to “resect when possible.” This has included systematic chemotherapy to downstage patients making them resectable, utilizing preoperative portal vein embolization to increase the size of the liver remnant and combining RFA with resection (these were excluded from this study). Some of the RFA patients would have been refused resection based on comorbidities. Perhaps this is best quantified by the shorter survival of the RFA patients when only patients who did not recur are analyzed. This difference is probably due to a higher severity of the comorbidities in the RFA group compared to the resection group. Unfortunately, there is no good scoring system to measure the overall severity of comorbidities in each group and do a statistical comparison.
In conclusion, RFA was associated with a higher hepatic recurrence rate and shorter time to recurrence but no difference in overall survival compared to resection.
References
Sjovall A, Jarv V, Blomqvist L, Singnomklao T, Cedermark B, Glimelius B, et al. The potential for improved outcome in patients with hepatic metastases from colon cancer: a population-based study. Eur J Surg Oncol 2004;30:834–841. doi:10.1016/j.ejso.2004.06.010.
Nicholl MB, Bilchik AJ. Thermal ablation of hepatic malignancy: useful but still not optimal. Eur J Surg Oncol 2008;34:318–323. doi:10.1016/j.ejso.2007.07.203.
Couinaud C. Le Foi: Etudes Anatomogiques et Chirugicales. Paris: Masson, 1957.
Martin RC, Edwards MJ, McMasters KM. Morbidity of adjuvant hepatic arterial infusion pump chemotherapy in the management of colorectal cancer metastatic to the liver. Am J Surg 2004;188:714–721. doi:10.1016/j.amjsurg.2004.08.042.
Martin RC, Scoggins CR, McMasters KM. Microwave hepatic ablation: initial experience of safety and efficacy. J Surg Oncol 2007;96:481–486. doi:10.1002/jso.20750.
Martin R, Paty P, Fong Y, Grace A, Cohen A, DeMatteo R, et al. Simultaneous liver and colorectal resections are safe for synchronous colorectal liver metastasis. J Am Coll Surg 2003;197:233–241. doi:10.1016/S1072-7515(03)00390-9.
Curley SA, Izzo F, Delrio P, Ellis LM, Granchi J, Vallone P, et al. Radiofrequency ablation of unresectable primary and metastatic hepatic malignancies: results in 123 patients. Ann Surg 1999;230:1–8. doi:10.1097/00000658-199907000-00001.
Wong SL, Edwards MJ, Chao C, Simpson D, McMasters KM. Radiofrequency ablation for unresectable hepatic tumors. Am J Surg 2001;182:552–557. doi:10.1016/S0002-9610(01)00813-3.
Oshowo A, Gillams A, Harrison E, Lees WR, Taylor I. Comparison of resection and radiofrequency ablation for treatment of solitary colorectal liver metastases. Br J Surg 2003;90:1240–1243. doi:10.1002/bjs.4264.
Aloia TA, Vauthey JN, Loyer EM, Ribero D, Pawlik TM, Wei SH, et al. Solitary colorectal liver metastasis: resection determines outcome. Arch Surg 2006;141:460–466. doi:10.1001/archsurg.141.5.460.
Abdalla EK, Vauthey JN, Ellis LM, Ellis V, Pollock R, Broglio KR, et al. Recurrence and outcomes following hepatic resection, radiofrequency ablation, and combined resection/ablation for colorectal liver metastases. Ann Surg 2004;239:818–825. doi:10.1097/01.sla.0000128305.90650.71.
Gillams AR, Lees WR. Radio-frequency ablation of colorectal liver metastases in 167 patients. Eur Radiol 2004;14:2261–2267. doi:10.1007/s00330-004-2416-z.
Machi J, Oishi AJ, Sumida K, Sakamoto K, Furumoto NL, Oishi RH, et al. Long-term outcome of radiofrequency ablation for unresectable liver metastases from colorectal cancer: evaluation of prognostic factors and effectiveness in first- and second-line management. Cancer J 2006;12:318–326. doi:10.1097/00130404-200607000-00011.
Abitabile P, Hartl U, Lange J, Maurer CA. Radiofrequency ablation permits an effective treatment for colorectal liver metastasis. Eur J Surg Oncol 2007;33:67–71. doi:10.1016/j.ejso.2006.10.040.
Pawlik TM, Scoggins CR, Zorzi D, Abdalla EK, Andres A, Eng C, et al. Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 2005;241:715–722. doi:10.1097/01.sla.0000160703.75808.7d, discussion.
Livraghi T, Solbiati L, Meloni F, Ierace T, Goldberg SN, Gazelle GS. Percutaneous radiofrequency ablation of liver metastases in potential candidates for resection: the “test-of-time approach”. Cancer 2003;97:3027–3035. doi:10.1002/cncr.11426.
van Duijnhoven FH, Jansen MC, Junggeburt JM, van Hillegersberg R, Rijken AM, van Coevorden F, van dS Jr, et al. Factors influencing the local failure rate of radiofrequency ablation of colorectal liver metastases. Ann Surg Oncol 2006;13:651–658. doi:10.1245/ASO.2006.08.014.
Wood TF, Rose DM, Chung M, Allegra DP, Foshag LJ, Bilchik AJ. Radiofrequency ablation of 231 unresectable hepatic tumors: indications, limitations, and complications. Ann Surg Oncol 2000;7:593–600.
Kokudo N, Miki Y, Sugai S, Yanagisawa A, Kato Y, Sakamoto Y, et al. Genetic and histological assessment of surgical margins in resected liver metastases from colorectal carcinoma: minimum surgical margins for successful resection. Arch Surg 2002;137:833–840. doi:10.1001/archsurg.137.7.833.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reuter, N.P., Woodall, C.E., Scoggins, C.R. et al. Radiofrequency Ablation vs. Resection for Hepatic Colorectal Metastasis: Therapeutically Equivalent?. J Gastrointest Surg 13, 486–491 (2009). https://doi.org/10.1007/s11605-008-0727-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0727-0