Abstract
Background
Hepatocellular carcinoma (HCC) has a high worldwide prevalence and mortality. While surgical resection and transplantation offers curative potential, donor availability and patient liver status and comorbidities may disallow either. Interventional radiological techniques such as radiofrequency ablation (RFA) may offer acceptable overall and disease-free survival rates.
Materials and Methods
Sixty-eight cirrhotic patients matched for age, sex, tumor size, and Child–Pugh grade with small (1–5 cm) unifocal HCC were studied retrospectively to find determinants of overall and disease-free survival in those treated with surgical resection and RFA between 1991 and 2003.
Results
Multivariate analysis using Cox proportional regression modeling showed that overall survival was related to tumor recurrence (p = 0.010), tumor diameter (p = 0.002), and treatment modality (p = 0.014); overall p = 0.008. Recurrence was independently related to the use of RFA over surgery (p = 0.023) on multivariate analysis; overall p = 0.034.
Conclusion
Surgical resection offers longer disease-free survival and potentially longer overall survival than RFA in patients with small unifocal HCC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is a common cause of cancer mortality worldwide.1,2 It has a high incidence in Southeast Asia and Africa as well as to a lesser extent in Europe and America.1–3 Hepatic cirrhosis is the most widely recognized condition predisposing to the development of HCC1,2, and worldwide, 90% of patients with HCC have chronic infection with hepatitis B or C. Its incidence is expected to rise and peak within the next 20 to 30 years mirroring the predicted worldwide epidemiology of viral hepatitis.
Orthotopic liver transplantation (OLT) is the optimal treatment for small-volume HCC in patients with favorable Child–Pugh A or B disease. This can increase 5-year survival up to 75–92%.4–6 However, the small donor pool and the current guidance (“Milan criteria”)5 that only patients with solitary HCCs of a diameter less than 5 cm or three or fewer tumors of maximum diameter of 3 cm preclude OLT for many patients.
Resectional surgery is the next most effective curative treatment for HCC but this may not always be possible because of the characteristics of the tumor or the grade of cirrhosis in the background liver. Few cirrhotic patients are suitable for radical resection,4,6–13 and recurrence rates are high.8,10,14 Therefore, parenchymal-sparing alternative or complementary techniques such as radiofrequency ablation (RFA), percutaneous ethanol injection (PEI), percutaneous acetic acid injection (PAI), and cryotherapy have evolved. Radiofrequency ablation has been shown to be more effective than other percutaneous techniques such as PEI and PAI,15,16 but its role as an alternative to surgery is still unclear. At present, there is only one study17 which compares percutaneous techniques with surgical resection and three which compare RFA alone with surgery.18–20
The aim of this study is to compare the procedural morbidity, mortality, and long-term overall and disease-free survival of patients with hepatocellular cancer who did not undergo OLT and were treated with either surgical resection or RFA in two high-volume liver centers.
Materials and Methods
Patients were treated either in the hepatic unit of the Department of Surgery of Verona, Italy or the hepato-biliary surgical unit at Southampton General Hospital, UK between 1991 and 2003. Only tumors less than 5 cm were included as RFA is not effective in the ablation of hepatoma lesions above this size. All HCC patients meeting Milan criteria were considered for OLT, but if excluded on the basis of age, comorbidity likely to yield poor 5-year survival, alcohol recidivism, or patient choice was eligible for this study. Patients were divided into two groups according to the treatment they had received; group A consisted of patients who had been treated with surgical resection between 1991 and 2003; group B patients had been treated with RFA after its introduction in 1998. Patients were not randomized but allocated to resection or RFA on clinical grounds. The details of both groups for the case control study are shown in Table 1.
Therapeutic Techniques
Surgery
In general, a trans-parenchymal surgical technique was used guided by intraoperative ultrasound to identify tumor margins and segmental vascular pedicles. Resections were completed as needed as per tumor location aiming always for 1 cm of clear resection margin. The type and extent of the resection was based on tumor location, parenchymal condition, and patient’s general condition and to some extent whether the resection was performed early or late in the study period. In the early period, more extensive radical resections were performed, but more recently, segmental resections were performed if acceptable resection margin could be guaranteed. Later, if a wedge resection with acceptable margins could be achieved, this was performed.
Percutaneous RFA
The technique has been described previously.21 Between 1998 and 2003, a 460-kHz radiofrequency generator, with maximum power of 150 W and impedence range between 40 and 200 Ω (RITA Medical System, Mountain View, CA, USA) was used. All radiofrequency ablations were performed percutaneously. A repeat ultrasound was performed after the procedure to demonstrate the presence of a hyper-echoic spherical area of coagulative necrosis with a diameter greater than the tumor’s diameter.
Follow-up in both groups was with a combination of contrast-enhanced abdominal computed tomography scan and alpha fetoprotein levels. These were repeated after 1 month, then every 6 months for 2 years and then at least annually until the fifth year. In the group treated with RFA, the presence of partial or total contrast enhancement at the site of ablation was considered as local recurrence. Recurrences were treated when possible by further surgical resection, repeat RFA, or transarterial chemo-embolization.
Statistical Analysis
Patient data were retrospectively collated. Data gathered included age, sex, etiology of cirrhosis, tumor diameter, treatment method, biochemical profile to calculate Child–Pugh score, timing of intervention, and presence and timing of follow-up, recurrence, and death. Main end points were overall and disease-free survival.
Categorical data were compared using the χ 2 test, and measures of central tendency in parametric and nonparametric continuous datasets were compared using the Student’s t test and Mann–Whitney U test, respectively. Survival and disease-free survival were calculated and presented using the Kaplan–Meier method and comparison of overall and disease-free survival performed (for each relevant stratum) using the log-rank test. Cox regression modeling was used in univariate and multivariate mode to calculate hazard ratios (HR), regression coefficients, and p values for independent variables on the dependent variables overall and disease-free survival. Only variables deemed significant or close to significant on univariate analysis were put forward to the multivariate stage. All analyses were performed using the Statistical Package for the Social Sciences (SPSS) v 12 for Windows. Statistical significance was required at the 95% level.
Results
Ninety-eight patients [72 men, 26 women, mean age 67 (95% confidence interval, CI 65–69) years] treated for first presentation, small (1–5 cm) unifocal HCC were identified from our databases and their case notes re-examined. From this unmatched cohort, a second cohort of 68 nontransplanted patients appropriately matched for age, sex, etiology, tumor size, and Child–Pugh grade were identified for analysis. The etiology of the cirrhosis was viral in 59% of cases and alcohol in 31%, the remainder being hemochromatosis, mixed or idiopathic. All patients were graded according to the Child–Pugh classification as all treatments were performed prior to the introduction of Model for End-Stage Liver Disease (MELD) score: 76% were class A, 24% class B. The median diameter of the tumors was 3 (range 1–5) cm.
Treatment Morbidity and Mortality
The overall major complication rate was 21% (27% in group A vs 16% in group B, p = 0.085). In group A, three patients developed postoperative hepatic failure, and in group B, one patient developed an artero-portal fistula after RFA.
Blood transfusion was required in three patients in group A and was not required in group B. The median duration of hospital stay was 16 [interquartile range (IQR) 12–25] days in group A and 3 (IQR 2–4) days in group B (p < 0.001, Mann–Whitney U test). There was one treatment-related death in this series; in group B, a 65-year-old Child–Pugh B patient with a 3-cm subcapsular nodule in segment V died of complications of peritonitis due to colonic perforation caused by heat transmission after RFA.
Survival Analysis
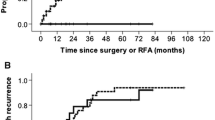
Overall Survival
The median follow-up for the whole study group was 32 (IQR 19–43) months. In group A, it was 43 (IQR 19–89) months and 30 (IQR 13–40) months in group B (p = 0.017, Mann–Witney U test). Overall, 61% of patients were still alive at the end of the follow-up. The median overall survival (Fig. 1) was 74 (95% CI 42–137) months in group A, but it was not attained in group B due to the difference in duration of follow-up for the two groups. The probability of overall survival at 1, 2, and 5 years was 91%, 81%, and 56% in group A vs 83%, 62%, and 57% in group B (p = 0.302).
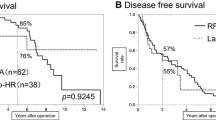
Disease-Free Survival
In total, 28 patients remained disease free (42%), while 40 had recurrence (58%). In group A, the median disease-free survival was 35 (95% CI 28–58) months and in group B 10 (95%CI 6–20) months (p = 0.028); see Fig. 2. In group A, the probability of disease-free survival at 1, 2, and 5 years was 77%, 67%, and 28% and for group B 42%, 29%, and 21%, respectively. In group A, true local recurrence at the site of resection was documented in 4% of patients, while 57% developed new sites of primary disease within the liver. In group B, local recurrence at the RFA site was seen in 30% of patients, while a further 30% developed new primary hepatic disease away from the site of the treated lesion (p < 0.001, χ 2 test). The shorter follow-up in group B should lead to caution in interpreting these results.
Univariate Analysis
On univariate analysis for overall survival age, sex, and Child Score did not achieve statistical significance for affecting survival, whereas tumor diameter, treatment method, and the presence of recurrence were associated with increased risk of death. In a similar analysis for disease-free survival, tumor diameter and treatment method were the only variables noted to have a significant effect.
Multivariate Analysis
On multivariate analysis using tumor size, treatment modality, and presence of recurrence, the most significant factor associated with death was the presence of hepatic recurrence (HR = 5.4, p = 0.010) Other independent risk factors for death identified on the multivariate analysis were: larger primary tumor nodule diameter (HR = 2.5, p = 0.003), treatment by RFA (HR = 4.0, p = 0.014). On multivariate analysis of disease-free survival using tumor size and treatment method, only treatment method retained its correlation with disease-free survival (HR = 2.3, p = 0.022, overall p for the regression model 0.034).
Other Analyses
In smaller tumors where surgery may be thought to be not as advantageous (≤3 cm) compared to larger tumors, median survival was not attained in either group, but median disease-free survival remained significantly different, being 47 months in group A and 8 months in group B (p < 0.001).
As RFA is a relatively new procedure and the expertise and technical considerations may have changed during the course of the study, an analysis was performed to determine whether the main outcome measure were related to the number of procedures performed during the time-course of our study. Including procedure number in multivariate analysis of disease-free survival did lead to a significant correlation between disease-free survival (DFS) and procedure performed at a hazard ratio very close to unity (HR 1.03, p = 0.003), but this was not replicated in a similar multivariate analysis for overall survival (Table 2). An analysis of overall and disease-free survival in both surgical and RFA groups for the first 25 procedures (group 1) and for later (26 to end of series) procedures (group 2) showed no statistically significant change in the relationship for overall and disease-free survival between the two groups (Table 3).
Discussion
Orthotopic liver transplantation is the gold-standard treatment in HCC with surgical resection a close second. Insufficient donor pool, patient comorbidity (or age in certain countries), alcohol recidivism, and extent of local disease are a cause for these treatment modalities to be impossible in a significant proportion of cases. Of the parenchymal-sparing procedures available, RFA has been demonstrated to be the most useful in early-stage disease for small (<5 cm), localized cancers.15,22,23 Although the role of RFA when surgery is not possible is well established, its precise role as an alternative to surgery remains debatable.
Vivarelli et al.18 retrospectively analyzed results for 158 nonrandomized cirrhotic patients, half treated surgically and half with RFA. Surgery demonstrated better results in 1- and 3-year survival, 83% and 65% vs 78% and 33%, and also in 1- and 3-year disease-free survival, 79% and 50% vs 60% and 20%, respectively. The authors noted the advantages of surgery to be more pronounced in Child A patients and in those with single, larger (>3 cm) tumors. Our message is similar and has comparable survival statistics (although disease-free survival at 1 year is lower in our cohort for RFA patients) in confirming the superiority of surgical resection, but in addition, we observed increased disease-free survival of patients undergoing resection even in the smaller tumor-size subgroup <3 cm. Since the overall message in this study is that surgery is the better treatment modality in the 1–5 cm tumor-size range, it should be emphasized that this is still true in the lower regions of this range. RFA at present should be considered as an acceptable alternative when surgery is not possible and not in patients who simply have a smaller tumor.
Wakai et al.,17 in a similar study of 149 patients undergoing surgical resection or percutaneous ablation (either RFA, microwave ablation, or PEI) found that surgery (p = 0.006) and smaller tumor size (p = 0.017) were associated with better outcomes in a retrospective study of 69 months median follow-up. The study had similar design to the one presented here, but interestingly an analysis of tumor size with a cut-off of 2 cm found that surgical resection was more effective in the larger sizes. In our subgroup analysis, we find that the improved DFS of patients undergoing surgical resection is significant below tumor diameter 3.5 cm. This difference may be a reflection of both the racial differences between the studies (all patients in the Wakai et al. study were Japanese) and different ranges of tumor sizes and may be because three different percutaneous ablative therapies were used in the Japanese study. We preferred to use RFA alone given its proven survival benefit over other ablative therapies in early-stage small HCC. A similar retrospective Asian study19 in 148 Child–Pugh A patients treated with surgery or RFA showed higher rates of local recurrence in the RFA group but no difference in overall and recurrence-free survival rates.
Only one randomized controlled trial20 comparing surgery and RFA has been performed comparing Child–Pugh A patients with unifocal HCC less than 5 cm in diameter. Comparing 90 patients in each group, the trial could not detect a difference in overall and disease-free survival between patients treated with surgery or RFA. While KM curves were produced and 1-, 2-, 3-, and 4-year survivals calculated, p values for the log-rank test were not given, and multivariate analysis, while showing that only serum albumin was associated with a difference in survival, was not repeated for disease-free survival. This would be necessary to allow a more detailed comparison with the data presented.
Our study is one of the first to directly compare overall and disease-free survival between surgical resection and RFA alone using both log-rank test against Kaplan–Meier curves and Cox proportional regression modeling of likely determinants of survival and recurrence. The major finding in terms of overall survival following confounding is that surgery, smaller tumors, and no recurrence is associated with improved survival. In multivariate analysis of disease-free survival, the type of intervention is the only independent predictor of improved DFS. The main criticism of our study is its retrospective nature. Furthermore, it should not be read as suggesting surgical resection is a superior treatment modality to OLT in patients meeting Milan criteria.
The contrasting results between the studies discussed in this paper suggest the need for a randomized prospective trial comparing resection with RFA in unifocal HCC (either as a bridge to OLT or where OLT is not possible) to be performed in the Western Hemisphere where etiology of cirrhosis is likely to be more variable and across Child–Pugh classes where surgery may still be offered. This is the second retrospective European study comparing surgery and RFA in the treatment of small HCC, which in the absence of prospective data will help to guide present practice and guide scientific and ethical hypothesis generation for future prospective studies.
At present, it is widely agreed that surgical resection remains the better treatment for discrete, nontransplantable HCC in favorable patients. It offers the best overall survival, and RFA should be considered as the best available option when surgery is not feasible. However, the morbidity and mortality of liver resection in these difficult patients must be borne in mind and, with probe development and adjuvant maneuvers, RFA may yet prove to be equally effective. The use of both treatments can be supported in specialist, multi-disciplinary liver units where the choice of technique at present should be decided on a case-by-case basis.
Conclusion
Surgical resection remains the best treatment for small, unifocal nontransplanted HCC in favorable patients. It offers the best disease-free survival and, through this reduced recurrence, may offer improved overall survival. RFA should be considered as the best available option when surgery is not feasible.
Summary
Radiofrequency ablation is a potential alternative to surgery in patients with hepatocellular carcinoma. Surgical resection and RFA are compared in 68 nontransplanted cirrhotic patients with small unifocal HCC. Surgery has a clear benefit in preventing recurrence and a small survival benefit which does not preclude future randomized trials.
References
Colombo M, de Franchis R, Del Ninno E, Sangiovanni A, De Fazio C, Tommasini M et al. Hepatocellular carcinoma in Italian patients with cirrhosis. N Engl J Med 1991;325(10):675–680.
Yoshizawa H. Hepatocellular carcinoma associated with hepatitis C virus infection in Japan: projection to other countries in the foreseeable future. Oncology 2002;62(Suppl 1):8–17.
Kiyosawa K, Tanaka E. Characteristics of hepatocellular carcinoma in Japan. Oncology 2002;62(Suppl 1):5–7.
Utsunomiya T, Shimada M, Taguchi KI, Hasegawa H, Yamashita Y, Hamatsu T et al. Clinicopathologic features and postoperative prognosis of multicentric small hepatocellular carcinoma. J Am Coll Surg 2000;190(3):331–335.
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334(11):693–699.
Zhou XD, Tang ZY, Yang BH, Lin ZY, Ma ZC, Ye SL et al. Experience of 1000 patients who underwent hepatectomy for small hepatocellular carcinoma. Cancer 2001;91(8):1479–1486.
Colombo M. Nonpercutaneous therapies of hepatocellular carcinoma. Hepatogastroenterology 2001;48(37):25–28.
Maeda T, Takenaka K, Taguchi K, Kajiyama K, Shirabe K, Shimada M et al. Small hepatocellular carcinoma with minute satellite nodules. Hepatogastroenterology 2000;47(34):1063–1066.
Arii S, Yamaoka Y, Futagawa S, Inoue K, Kobayashi K, Kojiro M et al. Results of surgical and nonsurgical treatment for small-sized hepatocellular carcinomas: a retrospective and nationwide survey in Japan, The Liver Cancer Study Group of Japan. Hepatology 2000;32(6):1224–1229.
Horigome H, Nomura T, Nakao H, Saso K, Takahashi Y, Akita S et al. Treatment of solitary small hepatocellular carcinoma: consideration of hepatic functional reserve and mode of recurrence. Hepatogastroenterology 2000;47(32):507–511.
Makuuchi M, Imamura H, Sugawara Y, Takayama T. Progress in surgical treatment of hepatocellular carcinoma. Oncology 2002;62(Suppl 1):74–81.
Poon RT, Fan ST, Lo CM, Ng IO, Liu CL, Lam CM et al. Improving survival results after resection of hepatocellular carcinoma: a prospective study of 377 patients over 10 years. Ann Surg 2001;234(1):63–70.
Kosuge T, Makuuchi M, Takayama T, Yamamoto J, Shimada K, Yamasaki S. Long-term results after resection of hepatocellular carcinoma: experience of 480 cases. Hepatogastroenterology 1993;40(4):328–332.
Izumi N, Asahina Y, Noguchi O, Uchihara M, Kanazawa N, Itakura J et al. Risk factors for distant recurrence of hepatocellular carcinoma in the liver after complete coagulation by microwave or radiofrequency ablation. Cancer 2001;91(5):949–956.
Lin SM, Lin CJ, Lin CC, Hsu CW, Chen YC. Randomised controlled trial comparing percutaneous radiofrequency thermal ablation, percutaneous ethanol injection, and percutaneous acetic acid injection to treat hepatocellular carcinoma of 3 cm or less. Gut 2005;54(8):1151–1156.
Livraghi T, Giorgio A, Marin G, Salmi A, de Sio I, Bolondi L et al. Hepatocellular carcinoma and cirrhosis in 746 patients: long-term results of percutaneous ethanol injection. Radiology 1995;197(1):101–108.
Wakai T, Shirai Y, Suda T, Yokoyama N, Sakata J, Cruz PV et al. Long-term outcomes of hepatectomy vs percutaneous ablation for treatment of hepatocellular carcinoma < or = 4 cm. World J Gastroenterol 2006;12(4):546–552.
Vivarelli M, Guglielmi A, Ruzzenente A, Cucchetti A, Bellusci R, Cordiano C et al. Surgical resection versus percutaneous radiofrequency ablation in the treatment of hepatocellular carcinoma on cirrhotic liver. Ann Surg 2004;240(1):102–107.
Hong SN, Lee SY, Choi MS, Lee JH, Koh KC, Paik SW, et al. Comparing the outcomes of radiofrequency ablation and surgery in patients with a single small hepatocellular carcinoma and well-preserved hepatic function. J Clin Gastroenterol 2005;39(3):247–252.
Chen MS, Li JQ, Zheng Y, Guo RP, Liang HH, Zhang YQ et al. A prospective randomised trial comparing percutaneous local ablative therapy and partial hepatectomy for small hepatocellular carcinoma. Ann Surg 2006;243(3):321–328.
Nicoli N, Casaril A, Marchiori L, Mangiante G, Hasheminia AR. Treatment of recurrent hepatocellular carcinoma by radiofrequency thermal ablation. J Hepatobiliary Pancreat Surg 2001;8(5):417–421.
Garcea G, Lloyd TD, Aylott C, Maddern G, Berry DP. The emergent role of focal liver ablation techniques in the treatment of primary and secondary liver tumours. Eur J Cancer 2003;39(15):2150–2164.
Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Solbiati L, Gazelle GS. Small hepatocellular carcinoma: treatment with radio-frequency ablation versus ethanol injection. Radiology 1999;210(3):655–661.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Abu-Hilal, M., Primrose, J.N., Casaril, A. et al. Surgical Resection Versus Radiofrequency Ablation in the Treatment of Small Unifocal Hepatocellular Carcinoma. J Gastrointest Surg 12, 1521–1526 (2008). https://doi.org/10.1007/s11605-008-0553-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0553-4