Abstract
Objective
To describe the endosonographic features of gastrointestinal ectopic pancreas, especially when histopathological diagnosis is unachievable with nonsurgical modalities.
Methods
Endoscopic ultrasonography was performed in 20 patients with endoscopically recognized ectopic pancreas. We then analyzed the endosonographic features of the lesions and the clinical aspects of the patients, including age, gender, symptoms, and lesion locations.
Results
Endoscopic ultrasonography revealed that the lesions originated from the second, third, and/or fourth layers of the gastrointestinal wall. Most lesions (95%, 19/20) were heterogenous, mainly hypoechoic or mixed, in echogenicity. The borders of the lesions were indistinct in 13 (13/20, 65%) and distinct in 7 (7/20, 35%) patients. Anechoic cystic or tubular structures within the lesions appeared in 7 of the 20 lesions (35%).
Conclusion
Ectopic pancreas usually appears as a submucosal lesion with characteristic central dimpling. Furthermore, characteristic endoscopic ultrasonographic features can readily assist in the diagnosis of ectopic pancreas without having to perform endoscopic biopsy or surgery. However, either endoscopic ultrasonography-guided fine needle aspiration or endoscopic removal of lesions should still be considered mandatory for the differential diagnosis of ectopic pancreas whenever typical endosonographic features cannot be well demonstrated.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ectopic pancreas, a relatively rare benign developmental anomaly, is defined as pancreatic tissue that has neither vascular nor anatomic continuity with the normally located pancreas proper.1 This lesion is also termed aberrant pancreas, heterotopic pancreas, pancreatic rest, and pancreatic heterotopia.2 Ectopic pancreas has been found in 0.55% to 13% of autopsies and has also been noted in approximately one of every 500 surgical operations involving the upper abdomen.3 In addition, it is most commonly located in the upper gastrointestinal (UGI) tract adjacent to the normal pancreas.4,5
Pathological diagnosis of ectopic pancreas is usually unachievable for two reasons: because adequate tissue samples cannot usually be taken during endoscopic biopsy using standard forceps6 and because surgery is usually unnecessary for most asymptomatic patients. In contrast, imaging techniques are helpful in establishing an early and definite differential diagnosis. Correlations between sonographic and histopathological patterns of ectopic pancreas have been previously established in the literature.7,8 Endoscopic ultrasonography (EUS) combines the techniques of gastrointestinal endoscopy and ultrasonography and provides clear and nonsurgical visualization of various subepithelial lesions in the UGI tract.9–13 In this study, we present our experience of using EUS in diagnosing ectopic pancreas and evaluate the role of EUS in determining these lesions.
Materials and Methods
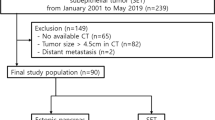
From April 2004 to October 2007, a total of 10,257 patients underwent panendoscopy; of them, ectopic pancreas was diagnosed endoscopically in 114 (1.1%) patients based on characteristic features of the lesions.14 Of the 114 patients, 20 underwent EUS examination. All EUS procedures were performed by two experienced endosonographers.
EUS was performed using a radial echoendoscope at a scanning frequency of 7.5 or 12 MHz (Olympus GF-UM 240; Olympus, Tokyo, Japan), as well as an ultrasonic miniprobe at a scanning frequency of 12 MHz (Olympus UM-2R; Olympus, Tokyo, Japan) introduced via an electronic esophagogastroduodenoscope (Olympus XQ-240; Olympus, Tokyo, Japan). EUS was performed to determine the location and size of the lesion, wall layer(s) involved, internal echotexture, and outer margin. Biopsy specimens were taken from all lesions with conventional biopsy forceps and sent for pathological diagnosis. Two patients also underwent exploratory laparotomy. Written informed consent to undergo EUS was obtained from all patients.
Results
The 20 patients ranged in age from 19 to 58 years (mean, 39 years), and comprised 11 men and 9 women. Thirteen patients presented with epigastric pain or dyspepsia. Ectopic pancreas was incidentally diagnosed in the other seven patients without preceding symptoms (Table 1).
Endoscopy revealed that the lesions were localized in the antrum in 19 of the 20 patients; only one lesion was found in the duodenum. Eighteen lesions were centrally umbilicated (Fig. 1). Two lesions without central dimpling were diagnosed as ectopic pancreas based on the EUS findings and pathological confirmation of resected specimens (Fig. 2). Conventional biopsies were performed on all 20 lesions, but only 2 lesions (10%) were diagnosed as ectopic pancreas based on pathology (Table 1). EUS revealed lesions ranging in size from 8 to 20 mm (mean 12 ± 3 mm). Heterogenous, hypoechoic, or mixed echogenic lesions were seen in 19 patients. Only one patient had a homogenous echogenic lesion. The borders were indistinct in 13 (13/20, 65%) and distinct in 7 (7/20, 35%) lesions. Anechoic cystic or tubular structures within the lesions appeared in 7 (35%) of the 20 lesions (Fig. 2). Nine lesions involved only one sonographic layer of the gastrointestinal wall: three originated in the second (muscularis mucosae) layer, five in the third (submucosa) layer, and one in the fourth (muscularis propri) layer. Ten lesions involved both the second and third layers. Only one lesion involved the second, third, and fourth layers (Table 2).
Ectopic pancreas of stomach (case 8). a Endoscopic image showing a submucosal lesion with central dimpling at the greater curvature of the antrum. b Corresponding EUS images showing an indistinct, heterogenous, and intermediate hypoechoic lesion with an anechoic space involving the second and third sonographic layers of the stomach.
Ectopic pancreas of duodenum (case 10). a Endoscopic image of a submucosal tumor without central umblication in the duodenal bulb. b Endosonographic view of an indistinct, heterogenous, and mixed echogenic mass with an anechoic space involving the second, third, and fourth layers of duodenum. c Microscopically, the ectopic pancreatic tissue, which is composed of pancreatic acini and ducts with focal cystic change, is located in the muscularis mucosae, submucosa, and muscularis propri of duodenal wall.
Based on Hase’s classification, 18 out of 20 lesions were S-type lesions; the other 2 lesions were M-type lesions.8 Based on Changchien’s classification,15 there were 14 type 1 lesions, 4 type 2 lesions, and 2 type 3 lesions.
Discussion
Ectopic pancreas, an uncommon benign developmental anomaly, is characterized by the presence of pancreatic tissue in ectopic locations at various sites of the body, but most frequently in the GI tract adjacent to the pancreas proper. In 90% of cases, ectopic pancreas is found in the stomach, the duodenum, and the proximal jejunum.16 Although rare, ectopic pancreas has also been found in the appendix, ileum, Meckel’s diverticulum, gall bladder, bile ducts, liver, spleen, omentum, mesentery, perigastric, and periduodenal locations.17 In our series, ectopic pancreas was diagnosed during panendoscopy in about 1% (1.1%, 114 of 10,257) of patients. The most common location was the antrum of the stomach.
Grossly, ectopic pancreas in the stomach and duodenum can display a central depression, which corresponds to the opening of a duct. The gross appearance of so-called central dimpling implies the presumptive diagnosis of ectopic pancreas for an endoscopist during preoperative endoscopy. As in our series, 90% of the lesions were visualized endoscopically to be centrally umbilicated. The appearance of a “bull’s eye” can also be typically visualized on barium studies.7,18
Ectopic pancreatic tissue may be functionally active and secretive.19 Ectopic pancreas may also give rise to benign and malignant ectopic pancreatic tumors.20 In addition, rare complications resulting from ectopic pancreas have been reported, including gastric outlet obstruction, obstructive jaundice, intestinal obstruction, and intussusception.21,22 However, ectopic pancreas is usually asymptomatic and found incidentally during routine endoscopic or radiographic studies. Although most of our patients (13/20) complained of some gastrointestinal symptoms, e.g., epigastric pain and dyspepsia, none of the patients presented with specific symptoms attributable to ectopic pancreas. However, two patients (case 10 and 11) benefited from surgical resection of ectopic pancreas, with subsequent loss of the symptoms postoperatively. The need for surgical treatment depends on the symptoms, definitive diagnosis regarding the possibility of malignancy and other attributable complications, such as gastrointestinal obstruction or bleeding. Definitive pathological diagnosis was only possible in two of our patients because none of the others required surgical intervention.
Histological diagnosis of ectopic pancreas is usually difficult when tissue specimens are obtained using conventional endoscopic biopsy forceps. For precise histological diagnosis, endoscopic techniques for obtaining deeper specimens are necessary, such as EUS-guided biopsy or combined strip biopsy and bite biopsy.23,24 Endoscopic removal of gastric aberrant pancreas is also useful for accurate diagnosis and treatment.25 The diagnosis of ectopic pancreas was based on the pathological appearance of specimens taken with standard endoscopic biopsy forceps in only two cases in our series.
EUS can clearly identify the structure of the intestinal wall, visualize sonographic features of the lesion and its layer(s) of origin, and thus readily assist in the differential diagnosis of subepithelial tumors. Based on the correlations between endosonographic and histopathological patterns of ectopic pancreas that have been established in the literature,7,8 endoscopists may benefit from EUS to determine the anatomic nature of an endoscopically recognized ectopic pancreas. Hase et al.8 described two types of aberrant pancreas: an M-type and an S-type. When we classified the EUS patterns in our 20 cases (lesions) into these two types, we found that the ectopic pancreatic tissue penetrated into the muscularis propria in the 2 M-type lesions and solely originated from the submucosal layer in the 18 S-type lesions, respectively. The latter type is therefore a good candidate for safe endoscopic removal, although none of our patients underwent the procedure.
In a study by Changchien et al.,15 13 cases of gastric aberrant pancreas were classified into three types based on the morphology of the muscular (the fourth) layer: type 1 (six cases), indicated an intact fourth layer with normal thickness; type 2 (four cases), indicated a thickened fourth layer; and type 3 (three cases), indicated a thickened fourth layer composed of some hyperechoic densities (tubular-like structures). Mucosectomy was performed without any complications in six cases (four type 1 and two type 2). They concluded that EUS provides practical information for selecting patients for a safe endoscopic mucosectomy.
The characteristic EUS features of ectopic pancreas, including indistinct margin, heterogeneous echogenicity (mainly hypoechoic accompanied by scattered small hyperechoic areas), an anechoic area and fourth-layer thickening, and location within the second, third, and/or fourth layers are very useful in establishing a preoperative diagnosis of ectopic pancreas. The heterogeneous hypoechoic or mixed echogenicity, resembling that of the normal pancreatic parenchyma, corresponds to the acinous tissue with scattered adipose tissue within the lesion. Anechoic areas indicate duct dilatation, and fourth-layer thickening is considered a consequence of the hypertrophy of the muscularis propria. The fact that the margins were mostly indistinct in our patients correlates with the histological findings of a lobular structure of the acinous tissue at the margin. However, the atypical features of homogenous hypoechoic echogenicity solely within the fourth layer on EUS in case 11 led to a misdiagnosis of gastrointestinal stromal tumor (GIST); ectopic pancreas was later diagnosed based on pathology of the resected specimen.
Conclusion
The characteristic endosonographic features of ectopic pancreas correlate well with specific histological components, making EUS a useful diagnostic modality without having to perform endoscopic biopsy or surgery. However, either EUS-guided fine needle aspiration or endoscopic removal of the lesion should still be considered mandatory for the differential diagnosis of ectopic pancreas whenever endosonographic features cannot be well demonstrated.
References
Feldman M, Friedman LS, Brandt LJ, et al. Anatomy, histology, embriology, and developmental anomalies of the pancreas. Sleisenger & Fordtran’s gastrointestinal and liver disease, vol 1, 8th ed. Philadelphia: Saunders Elsevier, 2006, pp 1183–1184.
Dolan RV, ReMine WH, Dockerty MB. The fate of heterotopic pancreatic tissue. Arch Surg 1974;109:762–765.
DeBord JR, Majarakis JD, Nyhus LM. An unusual case of heterotopic pancreas of the stomach. Am J Surg 1981;141:269–273.
Burke GW, Binder SC, Barron AM, Dratch PL, Umlas J. Heterotopic pancreas: gastric outlet obstruction secondary to pancreatitis and pancreatic pseudocyst. Am J Gastroenterol 1989;84:52–55.
Armstrong C, King P, Dixon J, Macleod I. The clinical significance of heterotopic pancreas in the gastrointestinal tract. B J Surg 1981;68:384–387.
Yoshida T, Sakamoto A, Kuroki K, Kojo A, Watanabe H, Tanaka K. Electrocoagulation biopsy of aberrant pancreas of the stomach. Am J Gastroenterol 1976;66:554–558.
Matsushita M, Hajiro K, Okazaki K, Takakuwa H. Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest Endosc 1999;49:493–497.
Hase S, Nakazawa S, Yoshino J, Kojima Y, Niwa Y, Ohashi S. A study on gastric and small intestinal aberrant pancreas by endoscopic ultrasonography with special reference to comparison with histological appearance. Jpn J Gastroenterol 1989;86:1684–1691.
Geller A, Wang KK, Dimagno EP. Diagnosis of foregut duplication cysts by endoscopic ultrasonography. Gastroenterology 1995;109:838–842.
Shen EF, Arnott IDR, Plevris J, Penman ID. Endoscopic ultrasonography in the diagnosis and management of suspected upper gastrointestinal submucosal tumors. Br J Surg 2002;89:231–235.
Rosch T, Lorenz R, Dancygier H, Wichert AV, Classen M. Endosonographic diagnosis of submucosal upper gastrointestinal tract tumors. Scand J Gastroenterol 1992;27:1–8.
Boyce GA, Sivak MV, Rosch T, Classen M, Fleischer DE. Evaluation of submucosal upper gastrointestinal tract lesions by endoscopic ultrasound. Gastrointest Endosc 1991;37:449–454.
Zhou PH, Yao LQ, Zhong YS, He GJ, Xu MD, Qin XY. Role of endoscopic miniprobe ultrasonography in diagnosis of submucosal tumor of large intestine. World J Gastroenterol 2004;10:2444–2446.
Perrillo RP, Zuckerman GR, Shatz BA. Aberrant pancreas and leiomyoma of the stomach: indistinguishable radiologic and endoscopic features. Gastrointest Endosc 1977;23:162–163.
Changchien CS, Hsiaw CM, Hu TH. Endoscopic ultrasonographic classification of gastric aberrant pancreas. Chang Gung Med J 2000;23:600–607.
Kilman WJ, Berk RN. The spectrum of radiographic features of aberrant pancreatic rests involving the stomach. Radiology 1977;123:291–296.
Theoni RF, Gudgaudas RK. Ectopic pancreas: usual and unusual features. Gastrointestinal Radiol 1980;5:37–42.
Pang LC. Pancreatic heterotopia: a reappraisal and clinicopathologic analysis of 32 cases. South Med J 1988;81:1264–1275.
Hammock L, Jorda M. Gastric endocrine pancreatic heterotopia report of a case with histologic and immunohistochemical findings and review of the literature. Arch Pathol Lab Med 2002;126:464–467.
Hideki U, Ryuichi D, Koichi H, Akiko S, Kenichiro H, Hiroshi N. Carcinoma arising from ectopic pancreas in the stomach: endoscopic detection of malignant change. J Clin Ultrasound 1998;26:265–268.
Shaib Y, Rabaa E, Feddersen R, Jamal M, Qaseem T. Gastric outlet obstruction secondary to heterotopic pancreas in the antrum: case report and review. Gastrointest Endosc 2001;54:527–530.
Mulholland KC, Wallace WD, Epanomeritakis E, Hall SR. Pseudocyst formation in gastric ectopic pancreas. J Pancreas (Online) 2004;5(6):498–501.
Vilmann P, Hancke S, Henriksen FW, Jacobsen GK. Endoscopic ultrasonography-guided fine-needle aspiration biopsy of lesions in the upper gastrointestinal tract. Gastrointest Endosc 1995;41:230–235.
Karita M, Tada M. Endoscopic and histologic diagnosis of submucosal tumors of the gastrointestinal tract using combined strip biopsy and bite biopsy. Gastrointest Endosc 1994;40:749–753.
Lee TH, Wang HP, Lin JT. Application of endoscopic mucosal resection for diagnosis of aberrant pancreas. Gastroenterol J Taiwan 2004;21(3):215–215.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chen, SH., Huang, WH., Feng, CL. et al. Clinical Analysis of Ectopic Pancreas with Endoscopic Ultrasonography: An Experience in a Medical Center. J Gastrointest Surg 12, 877–881 (2008). https://doi.org/10.1007/s11605-008-0476-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-008-0476-0