Abstract
Background
This study aims to evaluate the incidence of forearm soft tissue abnormalities associated with radial head fracture severity based on the Mason classification system.
Methods
Eighteen patients (age 18–45 years) were prospectively evaluated with elbow radiographs and magnetic resonance imaging (MRI) following longitudinal forearm trauma. MRI was performed within 10 days of the initial injury. Radiographs and MR images were evaluated in a blinded fashion by two musculoskeletal radiologists.
Results
Thirteen of 18 patients presented with Mason type I radial head fractures. In all patients with Mason type I fractures, the interosseous membrane (IOM) was intact. Two patients had Mason type II fractures with associated partial and compete tearing of the IOM and three patients had Mason type III fractures with complete tearing of the IOM. Edema was noted in the pronator quadratus in six of 13 type I injuries and seen in all type II and III injuries. No structural forearm soft tissue abnormalities were present in patients with Mason type I injuries. The presence of edema within the pronator quadratus correlated with distal forearm pain.
Conclusions
The severity of radial head fracture correlates with longitudinal forearm injury evidenced by the presence of IOM tearing. The findings suggest patients with Mason type II or III fractures of the radial head should undergo further evaluation of the forearm for associated soft tissue injuries. Edema within the pronator quadratus was present following forearm trauma regardless of the severity of fracture and was related to symptomatic forearm pain.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Longitudinal forearm stability is maintained by several anatomic structures. Primary stabilization is provided by the radius and ulna and secondary stabilizers including the interosseous membrane (IOM), triangular fibrocartilage complex (TFCC), forearm muscles, and, to a lesser extent, the surrounding soft tissues [14, 20, 21, 26]. Fractures of the radial head following longitudinal forearm trauma often result in pain within the mid- and distal forearm regardless of the severity of injury. In patients with injury to both the primary and secondary forearm stabilizers, chronic debilitating conditions may develop due to forearm instability [19, 23]. The classic case of radial head fracture associated with longitudinal forearm instability has been described as the Essex-Lopresti lesion. This rare injury was first described by Curr and Coe in 1946 and Essex-Lopresti in 1954 [5, 6]. Patients with this type of injury, if not addressed, may go on to develop severe wrist pain and decreased range of motion. This severe type of injury has been extensively studied in the literature both in clinical and cadaveric studies [9, 10]. However, soft tissue pathology associated with less severe forearm injuries has not been fully described.
Hausmann et al. [7] examined the association of IOM injuries with Mason type I radial head fractures. The Mason classification system defines three main categories of radial head fracture: type I—non-displaced, type II—minimally displaced segmental fracture, and type III—comminuted fracture [11]. Type I fractures are the least severe and are often treated with early mobilization. These patients typically recover well with no long-term sequelae of forearm instability. The data presented by Hausmann confirms the presence of partial IOM injuries in several patients. However, no patient demonstrated tearing of the central IOM fibers. The Essex-Lopresti lesion, on the other hand, is composed of type III fractures with known IOM disruption and associated forearm instability.
The purpose of our study was to evaluate the degree of structural soft tissue abnormalities associated with the severity of radial head fractures based on the Mason classification system. Our hypothesis is that as the severity of radial head fracture increases based on the Mason classification system, the incidence and severity of forearm soft tissue injuries will also increase. The data obtained from our research will then be used to suggest a clinical evaluation protocol for patients with forearm pain following radial head fractures.
Materials and Methods
Patient Selection
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from all patients for being included in the study. Eighteen patients age 18–45 years (average 29 years, 13 male, 5 female) were prospectively evaluated following a longitudinal forearm injury. The patients were determined to have sustained a longitudinal forearm injury by a board certified orthopedic hand surgeon based on history and clinical examination findings. Inclusion criteria included unilateral upper extremity trauma with radial head fracture. Patients with complex polytrauma involving the wrist/hand or other remote anatomic structures were excluded. Patients with prior elbow or upper extremity trauma and surgery were also excluded.
Radiographic Imaging
All 18 patients underwent complete radiographic imaging of the elbow including anteroposterior, lateral, and two oblique views. Twelve of these patients underwent radiographic imaging of the wrist and seven patients underwent radiographic imaging of the forearm. All images were evaluated in a blinded fashion by two board-certified musculoskeletal radiologists. Radial head fractures were classified using the Mason classification system (type I—undisplaced marginal fracture, type II—displaced segmental fracture, type III—comminuted fracture) [11].
Magnetic Resonance Imaging (MRI)
Following radiographic evaluation and clinical examination, all 18 patients underwent MRI of the forearm. The patient’s forearm was positioned in supination with the arm raised above the head and the elbow extended. Studies were performed in a 3-T GE Signa MR750 scanner. The scan protocol consisted of AX T1 (TR 709, TE 20, matrix 320 × 224, FOV 14 cm, ST 5 mm, SP 1 mm), AX T2 FS (TR 5446, TE 51, matrix 320 × 224, FOV 12 cm, ST 5 mm, SP 1 mm), COR T1 (TR 1134, TE 17, matrix 384 × 224, FOV 28 cm, ST 2 mm, SP 0.5 mm), COR T2 FS (TR 3089, TE 53, matrix 384 × 224, FOV 28 cm, ST 2 mm, SP 0.5 mm), COR MPSPGR FS (TR 175, TE 2.7, matrix 320 × 192, FOV 28 cm, ST 2 mm, SP 0.5 mm), SAG T1 (TR 750, TE 18, matrix 384 × 224, FOV 28 cm, ST 2 mm, SP 0.5 mm), SAG T2 FS (TR 3967, TE 52, matrix 384 × 224, FOV 28 cm, ST 2 mm, SP 0.5 mm). All studies were evaluated in a blinded fashion by two board-certified musculoskeletal radiologists.
Data Evaluation
Statistical analysis was performed with p value calculations determined using Spearman correlation coefficients. Inter-observer variation was determined using Kappa statistics. Correlation significance using a simple t test was evaluated comparing the Mason classification of radial head fracture to the presence of structural soft tissue injuries in the forearm. Additionally, the clinical presence of distal forearm pain was analyzed for significance compared to the presence of soft tissue abnormalities in the forearm on MRI. Forearm pain was documented by patient report and physical examination at rest and with forearm motion. Pain was documented as being present or absent prior to any treatment. If there was a discrepancy between the radiologists’ interpretation, a consensus opinion was determined based on a discussion between the radiologists and a review of the final report.
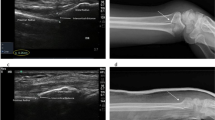
The data from our study is summarized in Table 1. Thirteen of 18 patients presented with non-displaced Mason type I radial head fractures (Fig. 1a). Two patients had Mason displaced type II fractures and three patients had displaced Mason type III fractures (Fig. 1b, c). No fractures of the distal forearm were identified. One patient with a Mason type II fracture also demonstrated a non-displaced fracture of the scaphoid. No patients had radiographic evidence of an elbow dislocation.
Results
All patients demonstrated pain and swelling with reduced range of motion at the elbow. Seven of the 13 patients with non-displaced fractures complained of pain in the mid- to distal forearm. All five patients with displaced (Mason type II and III fractures) reported pain in the distal forearm.
In all patients with Mason type I fractures, the main fibers of the central IOM were intact based on MRI (Fig. 2a). Both patients with Mason type II radial head fractures demonstrated partial/complete tearing of the IOM (Fig. 2b). All patients with comminuted radial head fractures (Mason type III) demonstrated complete tearing of the central IOM (Fig. 2c). The TFCC was intact in all type I and type II fractures. There was partial tearing of the TFCC in two of the patients with Mason type III fractures; the third patient with a Mason type III fracture had an intact TFCC. Edema was present in the soft tissues surrounding the radial head in all patients (Fig. 3a). Edema was present in the pronator quadratus in six of the 13 patients with non-displaced Mason type I fractures and in all patients with displaced (Mason type II and III fractures, Fig. 3b). No additional structural soft tissue abnormalities were identified in the distal forearm.
The central portion of the interosseous membrane was evaluated in each patient with MR imaging (AX T2 FS). a In all patients with Mason type I radial head fractures, the central IOM was intact (arrow). b In this patient with Mason type II fractures, partial disruption of the central IOM was identified (arrow). c In all patients with Mason type III fractures, complete IOM disruption was present (arrow)
Soft tissue abnormalities were present in all three Mason classification groups. However, no structural abnormalities were demonstrated on MR imaging in patients with Mason type I fractures (AX T2 FS). a In all patients, there was edema and some degree of joint effusion at the elbow on MR imaging. b In patients with distal forearm pain, moderate edema was demonstrated in the pronator quadratus muscle
The Mason classification of radial head fracture significantly correlated to the presence of central IOM injury (p < 0.01). Non-structural soft tissue injury, as noted by edema in the pronator quadratus, significantly correlated to the presence of distal forearm pain (p < 0.01). There was no significant difference between Mason classification of radial head injury and the presence of pain or edema in the pronator quadratus (p > 0.05). No significant inter-observer variably was identified in this study.
Discussion
Elbow and forearm fractures represent 8–10 % of adult fractures typically occurring after a fall on the outstretched arm. Disruption of the primary and secondary forearm stabilizers may occur during these injuries [3, 4, 17, 18]. Early diagnosis and treatment of complex forearm injuries is essential. Trousdale et al. [25] demonstrated only 20 % of patients with a delayed diagnosis of this injury had a positive outcome.
In 1946 Curr and Coe, and in 1951 Essex-Lopresti described an injury pattern following longitudinal forearm trauma consisting of radial head fracture, distal radio-ulnar joint (DRUJ) disruption, and tearing of the IOM [5, 6]. Patients with Essex-Lopresti injuries tend to have poor clinical outcomes unless treatment is targeted at forearm stabilization. Recent work has described surgical techniques to repair/reconstruct the IOM along with radial head replacement/reconstruction resulting in forearm stabilization [1, 2, 10].
Hausmann et al. [7] evaluated the association of Mason type I radial head fractures with injury of the IOM. In that prospective study of 14 patients, injury of the IOM was seen in nine cases. This study suggested that partial IOM injuries of the distal accessory fibers often occur with Mason type I fractures. The authors further described the forearm as a complex biomechanical structure similar to a joint functioning to transfer forces from the wrist to the elbow.
The location of IOM injury may have a significant impact on long-term clinical outcomes. The IOM is a complex anatomic structure composed of several anatomic regions [14]. The central third, sometimes referred to as the interosseous ligament, is the most important anatomically for forearm stabilization [12]. The position of the forearm at the time of injury also influences the pattern of trauma due to IOM tension [13]. Proper identification of not only the presence of an IOM injury but the location and anatomic region involved can affect clinical outcomes. Clinical examination techniques, such as the radius pull test, may identify unstable IOM injuries [22]. Radiographs may also demonstrate radial shortening in cases of longitudinal forearm trauma [23]. Advanced imaging techniques utilizing MRI and ultrasound have advanced in recent years and currently represent a viable option in the diagnosis of forearm soft tissue injuries [8, 15, 16, 24].
The goal of our research was to identify patterns of IOM and forearm soft tissue injury in association with the Mason classification of radial head fractures in patients suffering from longitudinal forearm trauma. Our data confirms the findings of prior studies that patients with non-displaced Mason type I radial head fractures demonstrate no evidence of significant central IOM injury. Furthermore, our study identified edema in the pronator quadratus as a potential underlying cause of distal forearm pain in patients with Mason type I radial head fractures. As the severity of injury increased resulting in displaced (Mason type II and type III) radial head fractures, the presence of significant central IOM injures were present in all patients. Based on our findings and the results of prior research, patients with Mason non-displaced type I radial head fractures do not initially require advanced imaging even if suffering from distal forearm pain. However, patients with displaced type II or type III radial head fractures should undergo ultrasound or MRI of the forearm to identify possible IOM injuries that may require surgical intervention.
The limitations of our study include a low sample size of displaced (Mason type II and III fractures). This study was performed over a 3-year period and only five patients with Mason type II and III injuries were identified and were willing and able to participate in our study. However, based on our data and published data, there is agreement in the increased incidence of IOM injuries with advancement of Mason classification. Our study did not identify tearing of the distal membranous portion of the IOM as described in Hausmann et al. [7] This discrepancy may be due to differences in scanning technique or timing of the scan relative to the date of injury. This discrepancy, however, should not affect clinical management as that portion of the IOM is not significantly involved in forearm stabilization. The patients were also scanned with the forearm supinated rather than a neutral position which can change the orientation and tautness of the IOM. The supinated position of the forearm was chosen so that all patients were scanned in a similar position thereby ensuring uniformity of the data. The DRUJ was not formally evaluated in our study; if the patient had specific wrist injuries, they were excluded from the study. No patient demonstrated gross DRUJ on clinical examination prior to MR imaging. If a TFCC injury was noted on MRI, then further evaluation of the wrist was performed clinically.
The data presented in our study, along with prior work, provides a clinical guideline in evaluating patients with longitudinal forearm arm injuries. The primary focus should be on history, clinical examination, and radiographic findings. If the radial head demonstrates a displaced or comminuted component, then advanced imaging with ultrasound or MRI is warranted to determine the extent of soft tissue injury. If the patient has a non-displaced radial head fracture and complains of distal forearm pain, initial conservative treatment is advised with appropriate clinical follow-up and initial advanced imaging is not indicated in these patients.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 [5]. Informed consent was obtained from all patients for being included in the study. JM declares that he has no conflict of interest. GG declares that he has no conflict of interest. EC declares that she has no conflict of interest. JY declares that he has no conflict of interest. Informed consent was obtained from each patient who participated in this study. No private, personal, or identifying information was used or published in this manuscript.
References
Adams JE, Culp R, Osterman AL. Interosseous membrane reconstruction for the Essex-Lopresti injury. J Hand Surg. 2010;35:129–36.
Adams JE, Osterman MN, Osterman AL. Interosseous membrane reconstruction for forearm longitudinal instability. Technol Hand Surg. 2010;14:222–5.
Amis AA, Miller JH. The mechanisms of elbow fractures: an investigation using impact tests in vitro. Injury. 1995;26:163–8.
Bado JL. The Monteggia lesion. Clin Orthop. 1967;50:71–86.
Curr J, Coe W. Dislocation of the inferior radioulnar joint. Br J Surg. 1946;34:74.
Essex-Lopresti P. Fractures of the radial head with distal radio-ulnar dislocation. J Bone Joint Surg. 1951;33B:244–7.
Hausmann J, Vekszler G, Breitenseher M, et al. Mason type-I radial head fractures and interosseous membrane lesions—a prospective study. J Trauma. 2009;66:457–61.
Jaakkola JI, Riggans DH, Lourie GM, et al. Ultrasonography for the evaluation of forearm interosseous membrane disruption in a cadaver model. J Hand Surg. 2001;26:1053–7.
Jungbluth P, Frangen TM, Arens S, et al. The undiagnosed Essex-Lopresti injury. Br J Bone Joint Surg. 2006;88:1629–33.
Marcotte AL, Osterman AL. Longitudinal radioulnar dissociation: identification and treatment of acute and chronic injuries. Hand Clin. 2007;2:195–208.
Mason ML. Some observations on fractures of the head of the radius with a review of 100 cases. Br J Surg. 1954;42:123–32.
McGinley JC, D’addessi L, Sadeghipour K, et al. Mechanics of the antebrachial interosseous membrane: response to shearing forces. J Hand Surg. 2001;26A:733–41.
McGinley JC, Hopgood BC, Gaughan JP, et al. Forearm and elbow injury: the influence of rotational position. J Bone Joint Surg. 2003;85A:2403–9.
McGinley JC, Kozin SH. Interosseous membrane anatomy and functional mechanics. Clin Orthop. 2001;383:108–22.
McGinley JC, Roach N, Gaughan JP, et al. Forearm interosseous membrane imaging and anatomy. J Skelet Radiol. 2004;33:561–8.
McGinley JC, Roach N, Hopgood BC, et al. Forearm interosseous membrane trauma: MRI diagnostic criteria and injury patterns. J Skelet Radiol. 2006;35:275–81.
Mikic ZD. Galeazzi fracture-dislocations. J Bone Joint Surg. 1975;57:1071–80.
Morgan WJ, Breen TF. Complex fractures of the forearm. Hand Clin. 1994;10:375–90.
Poitevin LA. Anatomy and biomechanics of the interosseous membrane: its importance in the longitudinal stability of the forearm. Hand Clin. 2001;17:97–110.
Rabinowitz RS, Light TR, Havey RM, et al. The role of the interosseous membrane and triangular fibrocartilage complex in forearm stability. J Hand Surg. 1994;19:385–93.
Skahen 3rd JR, Palmer AK, Werner FW, et al. The interosseous membrane of the forearm: anatomy and function. J Hand Surg. 1997;22:981–5.
Smith AM, Urbanosky LR, Castle JA, et al. Radius pull test: predictor of longitudinal forearm instability. J Bone Joint Surg. 2002;84A:1970–6.
Sowa DT, Hotchkiss RN, Weiland AJ. Symptomatic proximal translation of the radius following radial head resection. Clin Orthop. 1995;317:106–13.
Starch DW, Dabezies EJ. Magnetic resonance imaging of the interosseous membrane of the forearm. J Bone Joint Surg. 2001;83A:235–8.
Trousdale RT, Amadio PC, Cooney WP, et al. Radio-ulnar dissociation. A review of twenty cases. J Bone Joint Surg. 1992;74:1486–97.
Werner FW, An KN. Biomechanics of the elbow and forearm. Hand Clin. 1994;10:357–73.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
McGinley, J.C., Gold, G., Cheung, E. et al. MRI Detection of Forearm Soft Tissue Injuries with Radial Head Fractures. HAND 9, 87–92 (2014). https://doi.org/10.1007/s11552-013-9561-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-013-9561-2