Abstract
A common distal radio-ulnar joint (DRUJ) stabilisation procedure uses a tendon graft running from the lip of the radial sigmoid notch to the ulnar fovea and through a bony tunnel to the ulnar shaft, before being wrapped round the distal ulna and sutured to itself. Such graft fixation can be challenging and requires a considerable tendon length. The graft length could be reduced by fixing the graft to the ulna using a bone anchor or interference screw. The aim of this study was to compare the strength of three distal ulna graft fixation methods (tendon wrapping and suturing, bone anchor and interference screw). Four human cadaveric ulnae were used. A tendon strip was run through a tunnel in the distal ulna and secured by: (1) wrapping round the shaft and suturing it to itself, (2) a bone anchor and (3) an interference screw in the bone tunnel. Load to failure was determined using a custom-made apparatus and an Instron machine. Maximum failure load was highest for the bone anchor fixation (99.3 ± 23.7 N) followed by the suturing (96.2 ± 12.1 N), and the interference screw fixation (46.9 ± 5.6 N). There was no significant difference between the tendon suturing and bone anchor methods, but the tendon suturing was statistically significantly higher compared to the interference screw (P = 0.028). In performing anatomical stabilisation of the DRUJ fixation of the tendon graft to the distal ulna with a bone anchor provides the most secure fixation. This may make the stabilisation technique less demanding and require a smaller tendon graft.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma to the distal radio-ulnar joint (DRUJ) can result in pain and instability [4]. The radial sigmoid notch of the DRUJ is shallow and does not fully maintain the joint’s stability, which mainly depends on surrounding ligaments, particularly the dorsal and volar DRUJ ligament [7]. In cases of DRUJ instability causing functional problems and ulna-sided wrist pain, reconstruction and stabilisation of the DRUJ may be required.
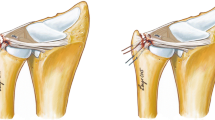
Adams and Berger described an anatomical reconstruction of the DRUJ [2]. In this technique, two tunnels are drilled, one in the ulna and one in the radius. The tendon runs through the radial tunnel and its two limbs are then brought to the ulnar fovea and passed through the ulnar tunnel. The two limbs of the tendon emerging from the ulnar tunnel are wrapped round the distal ulna and sutured to each other. Clinical evaluation of this procedure has yielded good results. In a series of 12 patients 11 were stabilised, recovering full range of motion and 85% grip strength [3]. However, this stabilisation technique requires a substantial length of tendon to allow wrapping round the ulna and suturing back to itself which may not always be available. In addition, we have found the technique whereby the tendon is wrapped round the distal ulna and sutured to itself technically demanding; maintaining sufficient tension on the tendon to keep the DRUJ reduced whilst suturing the two ends together is often difficult. Using a bone anchor or interference screw for graft fixation would require a shorter tendon graft. In addition, especially in the case of the interference screw, the graft tension can be easily maintained whilst the screw is inserted.
The aim of this study was to compare the strength of three graft fixation methods (tendon wrapping and suturing, bone anchor and interference screw) to the distal ulna.
Materials and Methods
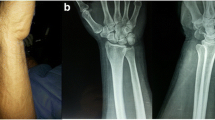
Four fresh frozen human cadaveric ulnae were used. They were thawed and stripped of all soft tissue. A 3.5 mm tunnel was drilled in each bone from the fovea to the distal ulnar shaft as described by Adams and Berger [2]. One tendon was harvested from its corresponding forearm. Two-millimeter-wide tendon strips were obtained from the tendon. One 2-mm strip was then inserted through the ulnar tunnel so that a tendon loop protruded from the ulna head and two ends protruded from mouth of the tunnel at the ulnar shaft. The decision to use a 3.5-mm tunnel and 2-mm tendon strips was based on a preliminary investigation using saw-bone (Sawbones®, UK) and pig tendons (Taylor’s Butchers, Preston, Lancashire). The dimensions were such that the tunnel was accommodating two lengths of tendon with a loop projecting from the ulna head and the tendon ends from the shaft. The preliminary tests showed that a 2.0-mm diameter graft could comfortably run twice through a 3.5-mm diameter tunnel. A thicker tendon could not run through twice, and a thinner tendon had a loose fitting.
The ulna was rigidly fixed using a custom-made clamp. The tendon loop emerging through the fovea end of the tunnel was loaded using a tendon hook attached to an Instron® machine. The bone–tendon construct was orientated so that the tendon loop was aligned with the direction of pull exerted by the Instron® machine (Fig. 1). Loading was set at 5 mm per minute.
Each ulna–tendon construct was taken though the following three protocol steps:
-
1.
The two graft ends emerging from the shaft end of the ulnar shaft tunnel were wrapped round the ulna and sutured to each other with a 3-0 vicryl whip suture (Ethibond; Ethicon, Somerville, NJ; Fig. 2). The ulna–tendon construct was loaded to failure.
-
2.
The sutured-ends of the tendon were removed. A bone anchor (Mini Bio-suture Tack bone anchors, Arthrex, UK) was used to fix the tendon to the distal ulna adjacent to the mouth of the ulnar shaft tunnel (Fig. 3). The ulna–tendon construct was again tested to failure.
-
3.
The sutured-ends of the tendon were again removed and the tendon was fixed to the ulnar tunnel using an interference screw (3 × 8 mm, non-cannulated Bio-Tenodesis screw, Arthrex, UK; Fig. 4) that was inserted though the ulna shaft tunnel end. The ulna–tendon construct was again tested to failure
The method of failure was noted and maximum load (N) recorded following each protocol step. Data was recorded using BlueHill® materials testing software.
Statistical Analysis
Paired analysis was performed with each ulna acting as its own control. Paired t-test was used for analysis (SPSS, version 14). Statistical significance was established at the P < 0.05 level.
Results
The maximum load to failure was highest for the bone anchor fixation (99.28 ± 23.69 N, mean ± standard deviation), followed by the simple suture fixation (96.23 ± 12.07 N) and the interference screw fixation (46.90 ± 5.64 N, Fig. 5). There was no significant difference between the simple suture and bone anchor methods (P = 0.09), but the simple suture was significantly higher compared to the interference screw (P = 0.028).
No ulnae fractured during testing. All sutured tendons failed by failure of the suture. All bone anchor fixations failed at the suture by slipping. All interference screw fixations failed by slipping of the tendon through the tunnel.
Discussion
DRUJ instability is a commonly encountered condition. The key ligamentous stabilisers of the DRUJ are the volar and dorsal DRUJ ligaments which are components of the triangular fibrocartilage complex [1, 10]. Several stabilisation techniques have been described. An anatomical reconstruction of the volar and dorsal DRUJ ligaments has been described by Adams and Berger [2]. However, the procedure is technically demanding, and requires a substantial length of tendon graft. The aim of this biomechanical study was to investigate the potential use of alternative fixation methods of the tendon graft to the ulna.
Fixation of the tendon graft to the ulna using interference screw or bone anchor has several potential theoretical advantages. The need to wrap the graft around the ulna is removed reducing the length of tendon graft required. In addition, these fixation methods do not require a suture to be tied whilst maintaining the graft under tension, which is technically demanding.
The results of this study suggest that the fixation of the tendon graft to the ulna using a bone anchor can be as secure as to that proved by wrapping the two ends of the tendon graft round the ulna and suturing them to each other. This would be clinically important as bone anchor fixation is much less technically demanding and can be achieved with a shorter tendon graft length.
It was surprising to see that the fixation strength when using a double graft fixed by one interference screw is lower than that achieved by suturing of the two tendon ends and lower than that achieved with a bone anchor. This is in contrast to previous reports showing that interference screw fixation provides more stable constructs as compared to suture tacks and bone anchors [5, 6, 9]. Investigators have demonstrated that for small-diameter interference screws fixing a single graft, the optimum graft:tunnel ratio is 60–90% [8]. Our graft:tunnel ratio was slightly higher than this (two 2-mm diameter grafts through a 3.5-mm diameter tunnel) because we felt that grafts less than 2 mm diameter would be too thin for clinical use in DRUJ stabilisation. In addition, we felt that a tunnel greater than 3.5 mm in diameter would exceed 1/3rd of the distal ulna width and could predispose to fracture. The difference between our results and previous reports may be due to the fact that two tendon strips were fixed in the bone tunnel in this study but only one tendon strip was fixed in previous studies. It might be that two tendon strips, when opposed against each other in the tunnel, reduce the interference effect of the screw, allowing the graft to slip out of the tunnel when a pulling force is applied. Adjustments to the diameter of the graft, the tunnel or the diameter or length screw may be needed to overcome this effect, but these parameters were not examined here.
There are certain limitations to this study. There was no objective assessment of the strength of suture tying. In addition, the strength of the suture tied in a laboratory environment may be greater than in vivo where there are surgical confines of space and access. As a formal joint stabilisation procedure was not performed in this experimental protocol, it was not necessary, in the simple suture fixation method, to tie the suture whilst maintaining the two tendon ends under tension. Furthermore, although differences in the strength of the three fixation methods have been examined, there was no attempt to determine whether the three methods can provide similar stability to the DRUJ.
In conclusion, within the limitations of this study, fixation of a tendon graft to the distal ulna with a bone anchor can be as strong as the fixation described by Adams and Berger [2] whereby the two tendon ends are wrapped round the ulna and sutured to each other. The use of bone suture anchors may thus be preferable especially when a short graft is harvested. Interference screw fixation is weaker and should be avoided.
References
Acosta R, Hnat W, Scheker LR. Distal radio-ulnar ligament motion during supination and pronation. J Hand Surg [Br]. 1993;18:502–5. doi:10.1016/0266-7681(93)90159-D.
Adams BD, Berger RA. An anatomic reconstruction of the distal radioulnar ligaments for posttraumatic distal radioulnar joint instability. J Hand Surg [Am]. 2002;27:243–51. doi:10.1053/jhsu.2002.31731.
Adams BD, Lawler E. Chronic instability of the distal radioulnar joint. J Am Acad Orthop Surg. 2007;15:571–5.
Jeffe R, Chidgey LK, Lastayo PC. The distal radio-ulnar joint: anatomy and management of disorders. J Hand Ther. 1996;9:129–38.
Kurosaka M, Yoshiya S, Andrish JT. A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med. 1987;15:225–9. doi:10.1177/036354658701500306.
Lee SK, Kubiak EN, Liporace FA, et al. Fixation of tendon grafts for collateral ligament reconstructions: a cadaveric biomechanical study. J Hand Surg [Am]. 2005;30:1051–5. doi:10.1016/j.jhsa.2004.12.013.
Linscheid RL. Biomechanics of the distal radioulnar joint. Clin Orthop Relat Res 1992;275:46–55.
Matsumoto A, Yoshiya S, Muratsu H, et al. Mechanical evaluation of a soft tissue interference screw with a small diameter: significance of graft/bone tunnel cross-sectional area ratio. Knee Surg Sports Traumatol Arthrosc. 2006;14:330–4. doi:10.1007/s00167-005-0675-0.
Okuno H, Tanaka J, Fujioka H, et al. Evaluation of an interference screw for tendon reattachment to small bones. J Orthop Trauma. 2002;16:418–21. doi:10.1097/00005131-200207000-00009.
Ward LD, Ambrose CG, Masson MV, et al. The role of the distal radioulnar ligaments, interosseous membrane, and joint capsule in distal radioulnar joint stability. J Hand Surg [Am]. 2000;25:341–51. doi:10.1053/jhsu.2000.jhsu25a0341.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Kalson, N.S., Charalambous, C.P., Powell, E.S. et al. Tendon Graft—Ulna Fixation in Distal Radio-Ulnar Joint Stabilisation; Biomechanical Comparison of Three Graft-Bone Fixation Methods. HAND 4, 279–282 (2009). https://doi.org/10.1007/s11552-009-9165-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11552-009-9165-z