Abstract
Purpose
We hypothesized that the re-fixation of the deep and superficial fibres of the distal radioulnar ligaments provide improved stability compared to reconstruction of the deep fibres alone.
Methods
Fourteen fresh-frozen cadaver upper extremities were used for biomechanical testing. Transosseous re-fixation of the deep fibres of the distal radioulnar ligaments alone (single mattress suture group; n = 7) was compared to the transosseous re-attachment of the deep and superficial fibres (double mattress suture group; n = 7). Cyclic load application provoked palmar translation of the radius with respect to the rigidly affixed ulna. Creep, stiffness, and hysteresis were obtained from the load-deformation curves, respectively. Testing was done in neutral forearm rotation, 60° pronation, and 60° supination.
Results
The re-fixation techniques did not differ significantly regarding the viscoelastic parameters creep, hysteresis, and stiffness. Several significant differences of one cycle to the consecutive one within each re-fixation group could be detected especially for creep and hysteresis. No significant differences between the different forearm positions could be detected for each viscoelastic parameter.
Conclusions
The re-fixation techniques did not differ significantly regarding creep, hysteresis, and stiffness. This means that the additional re-attachment of the superficial fibres may not provide greater stability to the DRUJ. Bearing in mind that the study was a cadaver examination with a limited number of specimens we may suppose that the re-attachment of the superficial fibres seem to be unnecessary. A gradual decline of creep and hysteresis from first to last loading-unloading cycle is to be expected and typical of ligaments which are viscoelastic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Injuries of the triangular fibrocartilage complex (TFCC) may be detrimental to forearm function since these structures among others are crucial for unrestricted pronation and supination of the forearm and weight-bearing [1–3]. The TFCC is postulated to be in conjunction with the interosseous membrane the most important stabilizer of the distal radioulnar joint (DRUJ) [1, 2, 4–6]. The articular disc of the TFCC is framed by the radioulnar ligaments which attach with their superficial fibres to the base of the ulnar styloid process and with their deep fibres to the ulnar fovea [2, 5, 7, 8]. Both deep and superficial fibres contribute distinctly to DRUJ stability [1, 5, 9, 10]. The centric insertions of the deep fibres at the ulnar fovea and the epicentric insertions of the superficial fibres at the base of the ulnar styloid process enable smooth tension transition between these structures during pronosupination [11]. These kinematic properties guarantee unrestricted forearm rotation while DRUJ stability is preserved [2, 6, 11, 12].
Ulnar-sided triangular fibrocartilage (TFC) tears may cause DRUJ instability with disabling consequences such as persistent pain, limitation of forearm rotation and loss of grip strength [4, 5, 11–13].
To treat these injuries anatomical TFCC re-fixation are increasingly of interest nowadays [7, 14–21].
However, none of these contributions has addressed the centric and epicentric insertions of the radioulnar ligaments specifically even though deep and superficial fibres both contribute to the DRUJ function biomechanically and kinematically [1, 5, 6, 9–11].
This is why we have examined an anatomical transosseous re-fixation technique including both superficial and deep fibres of the radioulnar ligaments in comparison to an established transosseous reconstruction of the deep fibres exclusively [17, 22].
We have tested whether the re-fixation of both deep and superficial fibres of the distal radioulnar ligaments provides greater stability than reconstruction of the deep fibres alone.
Materials and methods
The study design was approved by the institutional ethics committee.
Specimens
Fourteen fresh-frozen cadaver upper extremities amputated at the midportion of the humerus were used for this study (Table 1). The voluntary body donors were 83 years old on average (range: 64–95) at the time of death. Medical records indicated no musculoskeletal injuries or congenital, post-traumatic, and rheumatoid disorders of the upper extremity for any cadaver used. Posteroanterior and lateral radiographs of the wrists and elbow joints were done in order to exclude osseous abnormalities. Inclusion and exclusion criteria are stated in Table 2. The specimens were stored at −20 ° C and thawed completely at room temperature before testing. The skin, muscles, and capsuloligamentous structures below and around the elbow were completely preserved except for the necessary preparation to perform the re-fixation of the TFCC at the wrist. All specimens were moistened continually with saline solution at room temperature during testing.
Surgical technique
In two experimental groups the cut radioulnar ligaments were refixated with either single mattress suture (n = 7 arms) or double mattress suture (n = 7 arms) under direct visualisation using 3.5x loupe magnification.
In order to standardize the ulnar-sided desinsertion and afterwards the re-fixation of the radioulnar ligaments the open approach of Garcia-Elias et al. was used [23].
The deep and superficial fibres of the radioulnar ligaments were divided using a number 11 scalpel blade. With a sweeping "radial to ulnar" motion parallel to the distal surface of the ulnar head the foveal insertion of the deep fibres was completely cut. Then the ulnar styloid process was exposed half-circumferentially in order to section the superficial fibres sufficiently [10]. Prior to disengagement of the ligaments the specimens were tested by using the ballottement test for DRUJ instability [9, 24]. After complete ulnar-sided release of the radioulnar ligaments the TFC was retracted distally using pincers to verify adequate disengagement and the ballottement test was performed to confirm DRUJ instability.
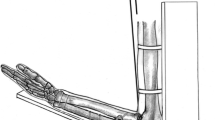
A modified transosseous re-fixation technique described by Iwasaki et al. for anchoring the deep fibres of the radioulnar ligaments by mattress suture served as the single mattress suture group (Fig. 1, left illustration) [17].
The anatomical transosseous re-fixation of the deep and superficial fibres of the radioulnar ligaments served as the double mattress suture group (Fig. 1, right illustration).
The allocation of specimens to both re-fixation techniques is displayed in Table 1.
The technique described by Iwasaki et al. was modified in order to provide secure osseous fixation of the suture. A 2 mm Kirschner wire mounted on a drill created the first oblique osseous tunnel starting from the ulnar neck to the ulnar fovea (Fig. 2). A lasso loop was transferred through the tunnel and the deep fibres of the radioulnar ligaments under direct visualization by using a 20-gauge venipuncture needle. After securing the lasso loop in situ a second parallel osseous tunnel was drilled 5 mm palmar to the first one. A 2–0 nonabsorbable suture (Prolene™ 2–0, Ethicon) was transferred likewise by using a 20-gauge needle through the second tunnel and the deep fibres of the radioulnar ligaments accordingly. The suture was retrieved by the lasso loop from the ulnocarpal compartment into the first osseous tunnel in order to create a horizontal mattress suture for the deep fibres of the radioulnar ligaments (Fig. 1, left illustration). For re-fixation of the superficial fibres of the radioulnar ligaments a third osseous tunnel at the base of the ulnar styloid process was drilled which was oriented almost perpendicular to the long axis of the ulnar shaft. The lasso loop was transferred as described previously and the suture (Prolene™ 2–0, Ethicon) was transferred by using a 20-gauge needle palmar to the styloid process through the soft tissue. The ulnar fibres which corresponded to the styloid base were addressed by the suture to create the second horizontal mattress suture re-fixation by using the lasso loop (Fig. 1, right illustration). The sutures were tightened in neutral forearm rotation after reduction of radius and ulna was achieved [22]. After re-attachment of the ligaments the skin was sutured to protect the underlying tissue from dehydration.
Biomechanical setting
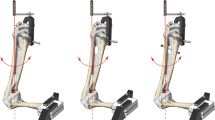
A multidirectional fixation frame has been designed and developed specifically for this study. The ulna and humerus were affixed rigidly with threaded pins to the custom mount, which allowed at least a reliable 120° of forearm rotation without restriction while the elbow was in 90° flexion.
The hand was secured to a wooden plate using screws with washers. The pisiform bone and the proximal pole of scaphoid bone were placed at the rim of the wooden plate in order to guarantee unrestricted DRUJ motion and a rigid fixation of the carpus.
Biomechanical testing was done by using a servo controlled electromechanical testing machine (ZwickRoell Z010; Zwick GmbH & Co. KG, Ulm, Germany) which recorded the force-deformation curves continuously (sampling rate: 10 Hz). Load was applied with a custom-made jig attached to a 5000 N load cell (Zwick GmbH & Co. KG, Ulm, Germany; series K; relative zero point deviation: 0.04 %; relative measurement uncertainty: 0.21 % at 50 N) which allowed precise placement at the Lister tubercle. Prior to load application, the Lister tubercle was prepared surgically. A 3 mm deep hole was drilled on top of the Lister tubercle using a 2 mm Kirschner wire mounted on a drill. Therefore, the jig could engage easily and reliably with the drilled hole upon the radius while the ulna remained attached rigidly.
After preloading at 1 N at a loading rate of 5 mm/minute the specimens were loaded with a crosshead speed of 5 mm/minute so that the distal radius was translated perpendicular to the coronal plane of the radius in palmar direction with respect to the fixed ulna. The specimens were subjected to seven cycles of loading and unloading up to 40 N to determine the viscoelastic properties. The load limit of 40 N was considered to be well within the elastic region of the soft tissue being examined. This limit is in accordance to previous biomechanical studies and was tested experimentally by a pilot study [10, 13].
These cyclic loading-unloading tests were performed in neutral forearm rotation, 60° supination, and 60° pronation, respectively. A recovery time of 30 minutes was respected between each forearm position after testing [13, 20].
Outcome measures
The viscoelastic parameters creep (mm), hysteresis (%), and stiffness (N/mm) were used for evaluation. They are key properties of viscoelastic materials to which connective tissue like ligaments belong to. A material is viscoelastic when its mechanical behaviour varies over time during application of a constant force or deformation.
Hysteresis means energy dissipation during loading and unloading (the unloading curve will not follow the loading curve). This is due to the energy absorbed by the tissue at each loading cycle and dissipated as heat or the drag of fluid being extruded and imbibed during loading and unloading. It is typical for viscoelastic materials (time dependent mechanical behaviour) and is important for normal function and performance of biological tissues.
Creep is defined as the increase of deformation under constant force. In every loading-unloading cycle, there was a shift of the curves to the right. The distance between the start point and the end point of the loading-unloading curves showed an increase of deformation under constant load (40 N) and represented the creep behaviour of the re-fixated ligaments (Fig. 3).
Representative loading-unloading curve from a cyclic test of the double mattress suture: male, 64 years of age; x-axis: deformation in mm; y-axis: load in N. The shift of the 7 loading-unloading curves to the right is typical of viscoelastic tissues. This shift to the right is described as creep. Loading maximum is 40 N for each loading curve followed by unloading. The area between loading and unloading within each cycle is defined as hysteresis
Stiffness was determined for each loading cycle as the slope of the load-deformation curve between 30–35 N and is a measure of elasticity of the material.
Increased creep, increased hysteresis and decreased stiffness are considered to be predictors for instability [25].
Statistical analysis
A two-way (cycle and treatment) analysis of variance (ANOVA) with repeated measurements was used to detect significant differences between the groups (single mattress suture group; double mattress suture group) within the different positions (neutral rotation, 60° supination, and 60° pronation). Duncan’s multiple comparisons test was applied for post hoc analysis. The level of significance was set at a value of p < 0.05. Results are presented as diagrams with standard deviation.
Results
Creep, hysteresis, and stiffness in neutral rotation
While several significant differences were detected between one cycle of loading and unloading to the consecutive one within each group, no significant differences were observed between the single mattress suture group and the double mattress suture group regarding the examined viscoelastic parameters creep, hysteresis, and stiffness (Fig. 4a–c ESM).
Creep, hysteresis, and stiffness in 60° pronation
While stiffness did not decrease significantly from the first to the last cycle of loading and unloading within each group, a few significant differences were observed between one cycle to the consecutive one concerning creep and hysteresis. No significant differences were detected between the single mattress suture group and the double mattress suture group regarding the examined viscoelastic parameters (Fig. 5a–c ESM).
Creep, hysteresis, and stiffness in 60° supination
The viscoelastic parameters creep, hysteresis, and stiffness demonstrated similar results to the aforementioned examination in 60° pronation. No significant differences were detected between the single mattress suture group and the double mattress suture group regarding the examined viscoelastic parameters Fig. 6a–c ESM.
Comparison of forearm positions regarding creep, hysteresis, and stiffness after single mattress suture
There were no significant differences between the different forearm positions for the corresponding cycles of each viscoelastic parameter (Fig. 7a–c ESM).
Comparison of forearm positions regarding creep, hysteresis, and stiffness after double mattress suture
Similar results were observed with no significant differences between the different forearm positions for the corresponding cycles of each viscoelastic parameter (Fig. 8a–c ESM).
Discussion
The study was undertaken in order to examine a re-fixation technique which may enable immediate mobilisation after surgical reconstruction. The importance of both deep and superficial fibres of the radioulnar ligaments were demonstrated clearly by Xu and Tang [5]. They observed length changes of all four ligaments (dorsal and palmar deep radioulnar ligaments; dorsal and palmar superficial radioulnar ligaments) during in vivo pronosupination. During pronation, the dorsal superficial radioulnar ligament and palmar deep radioulnar ligament tighten. They serve as complementary restraints for the DRUJ instability in pronation. During supination, the palmar superficial radioulnar ligament and dorsal deep radioulnar ligament tighten. These ligaments provide stability while functioning as a three point buttress to the DRUJ in supination. Xu and Tang even pointed out that the superficial fibres might be more sensitive restraints for the DRUJ instability since greater length changes of the former ligaments were observed in comparison to the deep fibres [5]. The anatomical configuration of the radioulnar ligaments enables a smooth tension shift within different parts of the fibres in order to guarantee unrestricted forearm rotation while stability is preserved [2, 11, 12, 26].
These in vivo observations and cadaver studies performed by Haugstvedt et al. and Moriya et al. demonstrated that both deep and superficial fibres are important contributors to DRUJ stability. Based on these conclusions the re-fixation of both fibre structures was evaluated in comparison to the re-attachment of the deep fibres alone [5, 9, 10].
Our results do not show significant differences between both re-fixation techniques regarding the measured biomechanical parameters. The additional re-attachment of the superficial fibres may not provide greater stability to the DRUJ than suture of the deep fibres on its own. Bearing in mind that the study was a cadaver examination with a limited number of specimens we may suppose that the re-attachment of the superficial fibres seem to be unnecessary. A gradual decline of creep and hysteresis from first to last loading-unloading cycle is to be expected and typical of ligaments which are viscoelastic because the tissue gradually stabilizes (steady-state) with continued cyclic loading. Therefore, significant differences between cycles were to be expected. No significant differences were detected between the different forearm positions for each viscoelastic parameter. This may support the fact that the radioulnar ligaments were attached adequately and that they stabilised the DRUJ sufficiently.
Biomechanical testing of intact radioulnar ligaments exhibited a fivefold higher stiffness throughout pronosupination than the re-fixation techniques evaluated [6, 27]. Therefore, immobilization after surgical repair is advisable. Early active mobilisation might compromise the re-fixation. Since an established re-fixation technique served as control we did not examine the intact radioulnar ligaments additionally [16, 17].
The biomechanical testing was performed using a highly standardised setup. We examined the structures within an arc of 120° from pronation to supination. Soft tissue around forearm and hand was deliberately preserved to avoid lesions which might have interfered with data collection. The open approach that was utilized is established and does not compromise crucial stabilising structures of the DRUJ since the dorsal capsule was incised at the fifth extensor compartment only [12, 23]. Furthermore, it was chosen deliberately to evaluate the integrity of the radioulnar ligaments and to guarantee safe and reliable desinsertion of the former structures before re-fixation. Load application provoked translation between radius and ulna which is the defining clinical entity in order to diagnose DRUJ instability [28]. Hysteresis, energy dissipation or internal dampening of ligaments, creep and stiffness were measured since they characterise the ligaments' viscoelasticity accurately.
Even though drilling an osseous tunnel at the base of the styloid process might cause fracture of the latter, the risk was deliberately reduced using direct visualisation and proper selection of Kirschner wires.
Our cadaver study used seven specimens per group and was based on specific loading rates and loading maximums. It entails all limitations inherent in a design trying to simulate living tissue. Furthermore, the experimental setup allowed palmar translation of the radius with respect to the fixed ulna only. This deliberate design is owed to the observation that palmar instability of the radius with respect to the ulna is much more common than dorsal instability [29].
Another drawback is the decrease in biomechanical performance due to aging, but in our work this is consistent across all tissues, so that relative mechanical behaviour is constant regardless of age. The age-related or simply inter-individual heterogeneity among the specimens was mostly addressed by creating matched pairs of the two different re-fixation techniques separating both arms of the same cadaver for the two experimental groups. The values presented in this study were likely influenced by changes in soft tissue elasticity and lack of muscle tone and may therefore not reflect values in vivo.
The arc of 120° from pronation to supination does not resemble full range of motion and therefore may not simulate sufficient forearm mobility which is necessary to tackle certain activities of daily living.
Further studies should focus particularly on the kinematic properties of the superficial fibres to assess their function. Moreover, an experimental setup which evaluates the anatomical transosseous re-fixation of the deep and superficial fibres in comparison to re-attachment of the superficial fibres alone might provide additional information regarding the relevance of the latter structure.
In summary, further studies are required to answer the relevance of additional re-attachment of the superficial fibres.
References
Hagert CG (1994) Distal radius fracture and the distal radioulnar joint--anatomical considerations. Handchir Mikrochir Plast Chir 26:22–26
Kleinman WB (2007) Stability of the distal radioulna joint: biomechanics, pathophysiology, physical diagnosis, and restoration of function what we have learned in 25 years. J Hand Surg [Am] 32:1086–1106. doi:10.1016/j.jhsa.2007.06.014
Spies CK, Müller LP, Oppermann J et al (2014) Instability of the distal radioulnar joint - an overview of clinical and radiological procedures regarding their efficacies. Handchir Mikrochir Plast Chir 46:137–150. doi:10.1055/s-0033-1363662
Haugstvedt J, Berger RA, Nakamura T et al (2006) Relative contributions of the ulnar attachments of the triangular fibrocartilage complex to the dynamic stability of the distal radioulnar joint. J Hand Surg [Am] 31:445–451. doi:10.1016/j.jhsa.2005.11.008
Xu J, Tang JB (2009) In vivo changes in lengths of the ligaments stabilizing the distal radioulnar joint. J Hand Surg [Am] 34:40–45. doi:10.1016/j.jhsa.2008.08.006
Schuind F, An KN, Berglund L et al (1991) The distal radioulnar ligaments: a biomechanical study. J Hand Surg [Am] 16:1106–1114
Moritomo H (2015) Open repair of the triangular fibrocartilage complex from palmar aspect. J Wrist Surg 4:2–8. doi:10.1055/s-0034-1398474
Nakamura T, Takayama S, Horiuchi Y et al (2001) Origins and insertions of the triangular fibrocartilage complex: a histological study. J Hand Surg (Br) 26:446–454. doi:10.1054/jhsb.2001.0562
Moriya T, Aoki M, Iba K et al (2009) Effect of triangular ligament tears on distal radioulnar joint instability and evaluation of three clinical tests: a biomechanical study. J Hand Surg Eur Vol 34:219–223. doi:10.1177/1753193408098482
Haugstvedt J, Berger RA, Berglund LJ et al (2002) An analysis of the constraint properties of the distal radioulnar ligament attachments to the ulna. J Hand Surg [Am] 27:61–67
Hagert E, Hagert C (2010) Understanding stability of the distal radioulnar joint through an understanding of its anatomy. Hand Clin 26:459–466. doi:10.1016/j.hcl.2010.05.002
Gofton WT, Gordon KD, Dunning CE et al (2004) Soft-tissue stabilizers of the distal radioulnar joint: an in vitro kinematic study. J Hand Surg [Am] 29:423–431. doi:10.1016/j.jhsa.2004.01.020
Petersen MS, Adams BD (1993) Biomechanical evaluation of distal radioulnar reconstructions. J Hand Surg [Am] 18:328–334. doi:10.1016/0363-5023(93)90370-I
Atzei A, Luchetti R, Braidotti F (2015) Arthroscopic foveal repair of the triangular fibrocartilage complex. J Wrist Surg 4:22–30. doi:10.1055/s-0035-1544226
Farr S, Zechmann U, Ganger R et al (2015) Clinical experience with arthroscopically-assisted repair of peripheral triangular fibrocartilage complex tears in adolescents-technique and results. Int Orthop. doi:10.1007/s00264-015-2795-6
Iwasaki N, Nishida K, Motomiya M et al (2011) Arthroscopic-assisted repair of avulsed triangular fibrocartilage complex to the fovea of the ulnar head: a 2- to 4-year follow-up study. Arthroscopy 27:1371–1378. doi:10.1016/j.arthro.2011.05.020
Iwasaki N, Minami A (2009) Arthroscopically assisted re-attachment of avulsed triangular fibrocartilage complex to the fovea of the ulnar head. J Hand Surg [Am] 34:1323–1326. doi:10.1016/j.jhsa.2009.02.026
Atzei A (2009) New trends in arthroscopic management of type 1-B TFCC injuries with DRUJ instability. J Hand Surg Eur Vol 34:582–591. doi:10.1177/1753193409100120
Nakamura T, Nakao Y, Ikegami H et al (2004) Open repair of the ulnar disruption of the triangular fibrocartilage complex with double three-dimensional mattress suturing technique. Tech Hand Up Extrem Surg 8:116–123. doi:10.1097/01.bth.0000126573.05697.29
Martineau PA, Bergeron S, Beckman L et al (2005) Reconstructive procedure for unstable radial-sided triangular fibrocartilage complex avulsions. J Hand Surg [Am] 30:727–732. doi:10.1016/j.jhsa.2005.01.006
Chou KH, Sarris IK, Sotereanos DG (2003) Suture anchor repair of ulnar-sided triangular fibrocartilage complex tears. J Hand Surg (Br) 28:546–550
Spies CK, Müller LP, Unglaub F et al (2014) Anatomical transosseous fixation of the deep and superficial fibres of the radioulnar ligaments. Arch Orthop Trauma Surg 134:1783–1788. doi:10.1007/s00402-014-2103-8.
Garcia-Elias M, Smith DE, Llusá M (2003) Surgical approach to the triangular fibrocartilage complex. Tech Hand Up Extrem Surg 7:134–140
Garcia-Elias M (2012) Clinical examination of the ulnar-sided painful wrist. In: del Piñal F (ed) Arthroscopic management of ulnar pain. Springer Berlin Heidelberg; Imprint: Springer, Berlin, Heidelberg, pp 25–44
Dy CJ, Ouellette EA, Makowski AH et al (2012) Peripheral triangular fibrocartilage complex tears cause ulnocarpal instability: a biomechanical pilot study. Clin Orthop Relat Res 470:2771–2775. doi:10.1007/s11999-012-2399-z
af Ekenstam F, Hagert CG (1985) Anatomical studies on the geometry and stability of the distal radio ulnar joint. Scand J Plast Reconstr Surg 19:17–25
Werner FW, Taormina JL, Sutton LG et al (2011) Structural properties of 6 forearm ligaments. J Hand Surg [Am] 36:1981–1987. doi:10.1016/j.jhsa.2011.09.026
Pirela-Cruz MA, Goll SR, Klug M et al (1991) Stress computed tomography analysis of the distal radioulnar joint: a diagnostic tool for determining translational motion. J Hand Surg [Am] 16:75–82
Moritomo H, Kataoka T (2014) Palmar reconstruction of the triangular fibrocartilage complex for static instability of the distal radioulnar joint. Tech Hand Up Extrem Surg 18:110–115. doi:10.1097/BTH.0000000000000047
Acknowledgments
We thank Mr. Thomas Bruckner, PhD, Department of Medical Biometry and Informatics, Heidelberg, Germany for his statistical advice.
We thank Mrs. Jutta Knifka, Department of Orthopaedics and Traumatology, University Hospital Cologne, Germany, for her relentless support.
Special thanks to Mr. Martin Külser-Feldker, Institute of Biomechanics and Orthopaedics, German Sport University Cologne, Germany, for his great expertise.
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional ethics committee and with the 1964 Helsinki declaration.
Funding
The study was supported by a grant of the Richard and Annemarie Wolf Foundation. The first author appreciates the financial support kindly.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. 4
a-b *Significantly (p < 0.05) different from the preceding cycle within the group (both groups: n = 7). c *Significantly (p < 0.05) different from the preceding cycle within the group (single mattress suture group: n = 7; double mattress suture group: n = 6) (DOCX 14 kb)
ESM 2
(DOCX 12 kb)
ESM 3
(DOCX 14 kb)
Fig. 5
a *Significantly (p < 0.05) different from the preceding cycle within the group (single mattress suture group: n = 7; double mattress suture group: n = 6). b-c *Significantly (p < 0.05) different from the preceding cycle within the group (both groups: n = 7) (DOCX 14 kb)
ESM 5
(DOCX 14 kb)
ESM 6
(DOCX 12 kb)
Fig. 6
a-c *Significantly (p < 0.05) different from the preceding cycle within the group (both groups: n = 7) (DOCX 14 kb)
ESM 8
(DOCX 14 kb)
ESM 9
(DOCX 12 kb)
Fig. 7
a-c *Significantly (p < 0.05) different from the preceding cycle within the group (all groups: n = 7) (DOCX 16 kb)
ESM 11
(DOCX 16 kb)
ESM 12
(DOCX 16 kb)
Fig. 8
a *Significantly (p < 0.05) different from the preceding cycle within the group (neutral: n = 7; pronation: n = 6; supination: n = 7). b *Significantly (p < 0.05) different from the preceding cycle within the group (all groups: n = 7). c *Significantly (p < 0.05) different from the preceding cycle within the group (neutral: n = 6; pronation: n = 7; supination: n = 7) (DOCX 16 kb)
ESM 14
(DOCX 16 kb)
ESM 15
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Spies, C.K., Niehoff, A., Unglaub, F. et al. Biomechanical comparison of transosseous re-fixation of the deep fibres of the distal radioulnar ligaments versus deep and superficial fibres: a cadaver study. International Orthopaedics (SICOT) 40, 315–321 (2016). https://doi.org/10.1007/s00264-015-2986-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2986-1