Abstract
Aims
To assess toxicity and clinical outcomes of moderately hypofractionated helical tomotherapy (HT) for the curative treatment of localized prostate cancer (PC).
Methods
From December 2012 to May 2018, 170 patients were treated with definitive intent for PC. Thirty-four percent were low risk, 30% intermediate risk (IR) and 36% high risk (HR). All patients received 70 Gy in 28 fractions to the prostate; 61.6 Gy were delivered to the seminal vesicles for IR; pelvic lymph nodes irradiation for a total dose of 50.4 Gy was added in the HR subgroup. Toxicity was assessed using CTCAE V4.0, and biochemical failure was defined following Phoenix criteria. Time-to-event data were analyzed using the Kaplan–Meier method and log-rank test.
Results
The median follow-up was 36 months (range 12–78); acute toxicity was as follows: G1 and G2 in 27.6% and 19.4% for GI; 53% and 24% for GU. No G ≥ 3 event was observed. For late toxicity, G ≥ 3 GI and GU rates were, respectively, 3% and 2.4% at 3 years and 3% and 4.8% at 4 years; no G4 occurred. A statistical correlation between acute or late G3 incidence and clinical or dosimetric parameters was not found. At the time of analysis, 2- and 3-year biochemical relapse-free survival rates were 90% and 87.5% and 2- and 3-year overall survival rates were 96.4% and 90%, respectively. The log-rank test revealed no difference between the risk groups in terms of biochemical control (p = 0.16).
Conclusions
Moderately hypofractionated RT with HT for localized prostate cancer reported excellent outcomes with mild acute and late toxicity incidence, with promising biochemical control rates.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For patients with localized prostate cancer, external beam radiotherapy (EBRT) is a consolidated treatment option in the curative setting. The constant evolution in technology has led to dose-escalated schedules with a remarkable improvement in terms of biochemical control rates [1, 2]. In the last years, the introduction of image-guided intensity-modulated radiotherapy (IG-IMRT) facilitated the adoption of moderately and extremely hypofractionated schedules. The radiobiological rationale for the use of > 2 Gy per fraction lies on the low α/β ratio of prostate cancer (about 1.5 Gy) compared to the nearby healthy structures [3] (i.e., 3 Gy for rectum and 5–10 Gy for bladder); besides the favorable therapeutic ratio of a tumor more sensitive to higher doses per fraction, hypofractionated schedules may be more attractive in terms of patients’ compliance and cost-effectiveness for the shortening of the overall treatment time [4]. Currently, mature data from several phase III randomized trials confirmed that moderately hypofractionated schedules (2.2–4.0 Gy per fraction) reported similar tumor control and toxicity rates compared to conventional fractionation [5], and recent AUA/ASTRO guidelines recommend their routine use [6].
Herein, we report the results of our retrospective study evaluating 170 patients with localized prostate cancer treated with moderate hypofractionation in simultaneous integrated boost (SIB) using helical tomotherapy (HT, Accuray, Inc., Sunnyvale, CA, USA).
Materials and methods
This is a retrospective analysis of 170 patients with biopsy-proven diagnosis of prostate adenocarcinoma who were treated at our center with moderately hypofractionated radiotherapy.
Primary endpoints of the present study were acute and late genitourinary and gastrointestinal toxicities. Secondary endpoints were quality of life and biochemical relapse-free survival and overall survival. Patients’ characteristics are summarized in Table 1.
Pre-treatment evaluation consisted of physical examination including digital rectal examination, blood tests including PSA levels, bone scan and abdominal CT or MRI, if needed for staging. Inclusion criteria were: histologically confirmed diagnosis of prostate cancer, Karnofsky performance status ≥ 60, no history of prior pelvic radiotherapy and absence of active chronic inflammatory bowel disease. Patients with a follow-up less than 12 months were excluded from the current analysis.
According to D’Amico classification, patients were stratified in: low risk (T1c or T2a and Gleason score ≤ 6 and PSA < 10 ng/ml), intermediate risk (cT2b and/or Gleason score = 7 and/or PSA = 10–20 ng/ml) and high risk (T2c–T3 and/or Gleason score ≥ 8 and/or PSA > 20 ng/ml). Androgen deprivation therapy was prescribed according to NCCN guidelines for all intermediate- and high-risk patients, respectively, for 6 months and 2–3 years.
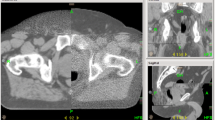
For radiotherapy treatment planning, a 2.5-mm-slice-thick CT scan, from the fourth lumbar vertebra to 2 cm below the femoral neck, was acquired with the patient in supine position with flexed legs and knee–ankle immobilization devices. To obtain a reproducible rectal emptying and bladder filling, patients were required to perform a fleet enema 2 hours prior to the examination and to drink 500 ml of water 30 min before the scan. The same protocol was applied during treatment for each fraction.
Regarding target volume delineation, for low-risk patients only a CTV1 consisting of the prostate gland was contoured. Then, PTV1 was generated by adding a 0.8-cm margin in all directions except posteriorly where a 0.6-cm margin was applied. For intermediate-risk cases, a CTV2 consisting of seminal vesicles was delineated; the same margin of PTV1 was applied for generating PTV2. Only for high-risk patients, pelvic lymph nodes (CTV3) were contoured and subsequently a 0.5-cm margin for PTV3 was added.
We adopted a moderately hypofractionated regimen in order to deliver, using a SIB technique, a total dose of 70, 61.6 and 50.4 Gy to prostate, seminal vesicles and pelvic lymph nodes, respectively. For all the target volumes, the prescription dose was 95% of PTV covered by at least 95% of the prescribed dose.
Rectum, bladder, femoral heads and intestinal loops were delineated as organs at risk (OARs), and the following constraints were applied: V65 < 15% for rectum and V55 < 50% and V60 < 30%; V56 < 35%, V60 < 25% for bladder; Dmax < 50 Gy and V46.2 < 5% for femoral heads; for intestinal loops, the prescription was to reduce the dose as low as reasonably achievable. Treatment planning was performed using the tomotherapy planning system. Radiotherapy was delivered with helical tomotherapy; the image-guided system was based on the daily execution of a MegaVoltage CT scan (MVCT) prior to each fraction in order to verify setup accuracy and rectal and bladder preparation. During the treatment course, a weekly evaluation of the patients was carried out; after RT, follow-up visits were scheduled every three months for the first year and then at biannual intervals.
Acute and late toxicities were prospectively collected and assessed using Common Terminology Criteria for Adverse Events (CTCAE) V4.0, defining acute events as any RT-related symptom occurring within 90 days from the start of treatment. For late adverse events, we considered all the side effects occurring after 90 days. Health-related quality of life (HRQOL) in particular for bladder and gastrointestinal function was assessed with Expanded Prostate Cancer Index Composite (EPIC-26) questionnaire at baseline, at 3-month follow-up and then at annual intervals.
Concerning clinical outcomes, biochemical failure was defined following Phoenix criteria as the identification of the nadir value of PSA + 2 ng/ml after radiotherapy with/without androgen deprivation therapy.
Medians and ranges were calculated for continuous variables. The potential association between toxicity rates and clinical or dosimetric parameters was investigated with a Chi-squared test assuming p ≤ 0.05 as statistically significant. The following clinical parameters were evaluated: age ≥ 75 years, comorbidities (hypertension, diabetes, inflammatory bowel disease, previous abdominal surgery, TURP) and pelvic RT administration; for dosimetric parameters, we investigated: rectal Dmax, V56 Gy, V60 Gy and V65 Gy; bladder Dmax, V55 Gy, V60 Gy, V70 Gy and for PTVs mean, maximum and minimum dose. Using the Wilcoxon signed rank test, we compared the baseline EPIC-26 with the follow-up scores. Time-to-event data were analyzed with the Kaplan–Meier method and log-rank test. All statistical analyses were performed using MedCalc statistical software package v.18.11.3 (Mariakerke, Belgium).
Results
From December 2012 to May 2018, 170 patients with median age 75 years (range 56–88) were treated with definitive hypofractionated helical tomotherapy for prostate cancer. Thirty-four percent were low risk (LR), 30% intermediate risk (IR) and 36% high risk (HR). The median iPSA was 8.79 ng/ml (1.3–170). All patients completed the treatment without any interruption: Acute toxicity was as follows: G1 and G2 in 27.6% and 19.4% of cases for GI; 53% and 24% for GU. No G ≥ 3 event was observed (Table 2 for acute and late toxicity in details).
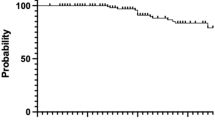
With a median follow-up of 36 months (range 12–78), 3- and 4-year G ≥ 2 late GI and GU adverse events rates were, respectively, 12.4% and 14.3% and 11.8% and 17.1%. Our late G ≥ 3 GI and GU toxicity rates were, respectively, 3% and 2.4% at 3 years and 3% and 4.8% at 4 years (Figs. 1, 2). The highest peak of G3 late adverse events was at 2 years with four GI and three GU cases of G3 toxicity. No G4 event was observed. No statistical correlation between late G3 incidence and clinical or dosimetric parameters was found. Particularly, the addiction of whole pelvis irradiation did not have an impact on GI or GU G ≥ 3 rates (p = 0.30 and p = 0.87). Concerning HRQOL, the EPIC-26 scores reported no statistical differences in terms of urinary or bowel dysfunction between baseline and 4-year data (p = 0.93 and p = 0.45) with a progressive trend to resolution (Fig. 3).
At the time of final assessment, in 12 patients (two low risk, five intermediate risk and five high risk, respectively) a biochemical relapse occurred, resulting in 3- and 4-year biochemical relapse-free survival (bRFS) rates of 88.5% and 87.2%, for the entire population. More specifically, for low-risk patients 3- and 4-year bRFS rates were 96.4% and 93.2%, respectively, for intermediate-risk patients were both 88.1% and for high-risk patients were both 81.8% (Fig. 4).
The log-rank test revealed no difference between the risk groups in terms of biochemical control (p = 0.16). Among these 12 cases, five subjects (one low risk, two intermediate risk and two high risk) developed distant metastases, consisting of three nodal recurrences, successfully treated with stereotactic body radiotherapy, and two bone metastases who underwent palliative treatment. Concerning overall survival (OS), 3- and 4-year OS rates were 88.3% and 82.7%, with only two patients who died by disease progression, respectively, after 16 and 24 months from the end of treatment.
Discussion
This mono-institutional analysis reports moderate hypofractionation with SIB technique by means of helical tomotherapy as a safe and effective treatment option for localized prostate cancer. Our radiotherapy schedule was adopted from the favorable results of the largest series of moderately hypofractionated radiotherapy [7, 8], and we reported excellent rates of acute and late toxicity, similar to other experiences reported in the literature [9,10,11,12,13,14,15,16,17,18] (Table 3); also in terms of biochemical control, our rates are in agreement with previous studies. These data support the routine use of moderate hypofractionation as a more attractive alternative to conventional schedule, as also recommended by recent AUA/ASTRO guidelines. In a previous report, we analyzed acute toxicity in a cohort of 42 patients with no evidence of G3 acute event [19]. This is also confirmed in the current study with mild acute toxicity rates, and no cases of acute G3. Concerning late adverse events, no G4 toxicity occurred, with 3- and 4-year G3 GI and GU toxicity rates of 3% and 2.4%, and 3% and 4.8%, respectively. No clinical or dosimetric parameters were found to be predictive of late toxicity; more specifically, in our series whole pelvis irradiation did not have an impact on GI adverse events incidence. The potential impact of lymph nodes irradiation on GI toxicity was also investigated by Longobardi et al. [20], observing that larger volume of nodal CTV and increased age were predictive factors of acute bowel toxicity.
This finding is also reported in a recent study by Jorgo et al. [21] concerning a cohort of 162 patients with intermediate- and high-risk prostate cancer treated with the same schedule of the present series. Notably, unlike the abovementioned study, we did not exclude high-risk patients older than 70 years from the pelvic lymph nodes irradiation, nevertheless reporting late GI toxicity rates comparable to patients not treated with whole pelvis RT (p = 0.30). Among the randomized trials of comparison between moderate hypofractionation and conventional fractionation, only the Fox Chase experience included whole pelvis irradiation, reporting similar GI rates with a negligible impact on quality of life [22].
The controversial role of pelvic lymph nodes irradiation in high-risk disease is also confirmed by three randomized trials [23,24,25] that reported no advantages in terms of biochemical control or OS, and one reporting on the contrary a gain in biochemical relapse-free survival by adding pelvic lymph nodes radiotherapy [26]. Recently, preliminary data from the PIVOTAL trial were published: This trial randomizes patients to prostate only radiotherapy versus prostate + pelvic lymph nodes RT with the aim to address the real impact of whole pelvis irradiation on clinical outcomes for locally advanced disease. Currently, keeping in mind that this trial adopts a higher pelvic dose compared to previously published studies (i.e., 60 Gy in 37 fractions, equivalent dose 2 Gy = 55.4 Gy), only data about acute and late toxicity are available and similar rates between the two cohorts are reported [27].
Concerning genitourinary toxicity, in our cohort no acute G3 adverse events were observed, and G2 rates were comparable to other series; only four cases of G3 late events were observed, with the highest peak after 24 months from the end of RT. We could not identify any predictive factor for acute or late GU toxicity. Despite the lack of a cohort of comparison with conventional fractionation, these data report a mild profile of toxicity, in agreement with a meta-analysis conducted by Carvalho et al. [28], where similar acute and late GU toxicity rates are reported for both conventional and hypofractionated schedules, especially for treatment regimens below 3 Gy per fraction.
Jereczek-Fossa et al. [29] recently published data about 179 patients treated with hypo-RT (70.2 Gy/2.6 Gy per fraction) reporting a small but not statistically significant increase in late GU adverse events in comparison with a cohort of 170 patients treated with conventional non-image-guided radiotherapy. The authors underline the role of IGRT for the safe delivery of moderate hypofractionation, also providing a cost-effectiveness advantage in terms of overall treatment time, and a favorable impact on biochemical control. Nowadays, there is weak evidence that hypofractionation may be superior to conventional treatment in terms of biochemical relapse-free survival, but non-inferiority trials [10,11,12] have demonstrated that moderately hypofractionated schedules are not worse than 2 Gy per fraction regimens, providing an iso-effective and iso-tolerable therapeutic option.
This study has several limitations: The retrospective nature limits the statistical power of the present series, despite toxicity being prospectively collected; in a large part of our population, especially for intermediate-risk patients, ADT has been administered following previous guidelines recommendations that now have changed, so this factor might have an impact on our results in terms of biochemical control; furthermore, we have already mentioned the lack of a cohort of comparison with a conventionally fractionated schedule, and our follow-up time is relatively short, although being comparable to other literature series.
Conclusions
The use of moderate hypofractionation with SIB by means of helical tomotherapy reports mild acute and late toxicity. Our favorable toxicity pattern reflects in a negligible impact in terms of quality of life. Also, we reported promising results in terms of biochemical control providing a shortening of the overall treatment time that may also favorably impact in terms of patients’ compliance and cost-effectiveness.
References
Zietman AL, DeSilvio ML, Slater JD, Rossi CJ Jr, Miller DW, Adams JA, Shipley WU (2005) Comparison of conventional-dose vs high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial. JAMA 294(10):1233–1239 (erratum in: JAMA. 2008 Feb 27;299(8):899–900)
Dearnaley DP, Jovic G, Syndikus I, Khoo V, Cowan RA, Graham JD, Aird EG, Bottomley D, Huddart RA, Jose CC, Matthews JH, Millar JL, Murphy C, Russell JM, Scrase CD, Parmar MK, Sydes MR (2014) Escalated-dose versus control-dose conformal radiotherapy for prostate cancer: long-term results from the MRC RT01 randomised controlled trial. Lancet Oncol 15(4):464–473. https://doi.org/10.1016/S1470-2045(14)70040-3
Dasu A, Toma-Dasu I (2012) Prostate α/β revisited: an analysis of clinical results from 14168 patients. Acta Oncol 51:963–974
Voong KR, Lal LS, Kuban DA, Pugh TJ, Swint JM, Godby J, Choi S, Lee AK, Schlembach PJ, Frank SJ, McGuire SE, Hoffman KE (2017) Long-term economic value of hypofractionated prostate radiation: secondary analysis of a randomized trial. Adv Radiat Oncol 2(3):249–258. https://doi.org/10.1016/j.adro.2017.07.010
Lee WR, Koontz BF (2018) Moderate hypofractionation for prostate cancer. Transl Androl Urol 7(3):321–329. https://doi.org/10.21037/tau.2017.12.07
Morgan SC, Hoffman K, Loblaw DA, Buyyounouski MK, Patton C, Barocas D, Bentzen S, Chang M, Efstathiou J, Greany P, Halvorsen P, Koontz BF, Lawton C, Leyrer CM, Lin D, Ray M, Sandler H (2019) Hypofractionated radiation therapy for localized prostate cancer: executive summary of an ASTRO, ASCO and AUA evidence-based guideline. J Urol 201(3):528–534. https://doi.org/10.1097/JU.0000000000000071
Kupelian PA, Willoughby TR, Reddy CA, Klein EA, Mahadevan A (2007) Hypofractionated intensity-modulated radiotherapy (70 Gy at 2.5 Gy per fraction) for localized prostate cancer: Cleveland clinic experience. Int J Radiat Oncol Biol Phys 68(5):1424–1430
Kotecha R, Marwaha G, Hearn JW, Weller MA, Kupelian P, Reddy CA, Ciezki JP, Stephans K, Tendulkar RD (2014) A comparison of long-term treatment-related toxicities between moderately hypofractionated and conventionally fractionated radiation therapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 90(1, Supplement):S423–S424
Pollack A, Walker G, Horwitz EM, Price R, Feigenberg S, Konski AA, Stoyanova R, Movsas B, Greenberg RE, Uzzo RG, Ma C, Buyyounouski MK (2013) Randomized trial of hypofractionated external beam radiotherapy for prostate cancer. J Clin Oncol 31:3860–3868
Lee WR, Dignam JJ, Amin MB, Bruner DW, Low D, Swanson GP, Shah AB, D’Souza DP, Michalski JM, Dayes IS, Seaward SA, Hall WA, Nguyen PL, Pisansky TM, Faria SL, Chen Y, Koontz BF, Paulus R, Sandler HM (2016) Randomized phase III noninferiority study comparing two radiotherapy fractionation schedules in patients with low-risk prostate cancer. J Clin Oncol 34:2325–2332
Catton CN, Lukka H, Gu CS, Martin JM, Supiot S, Chung PWM, Bauman GS, Bahary JP, Ahmed S, Cheung P, Tai KH, Wu JS, Parliament MB, Tsakiridis T, Corbett TB, Tang C, Dayes IS, Warde P, Craig TK, Julian JA, Levine MN (2017) Randomized trial of a hypofractionated radiation regimen for the treatment of localized prostate cancer. J Clin Oncol 35:1884–1890
Dearnaley D, Syndikus I, Mossop H, Khoo V, Birtle A, Bloomfield D, Graham J, Kirkbride P, Logue J, Malik Z, Money-Kyrle J, O’Sullivan JM, Panades M, Parker C, Patterson H, Scrase C, Staffurth J, Stockdale A, Tremlett J, Bidmead M, Mayles H, Naismith O, South C, Gao A, Cruickshank C, Hassan S, Pugh J, Griffin C, Hall E, CHHiP Investigators (2016) Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5-year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol 17(8):1047–1060. https://doi.org/10.1016/s1470-2045(16)30102-4(Erratum in: Lancet Oncol. 2016 Aug;17 (8):e321)
Di Muzio NG, Fodor A, Noris Chiorda B, Broggi S, Mangili P, Valdagni R, Dell’Oca I, Pasetti M, Deantoni CL, Chiara A, Berardi G, Briganti A, Calandrino R, Cozzarini C, Fiorino C (2016) Moderate hypofractionation with simultaneous integrated boost in prostate cancer: long-term results of a phase I–II study. Clin Oncol (R Coll Radiol) 28(8):490–500. https://doi.org/10.1016/j.clon.2016.02.005
Magli A, Moretti E, Tullio A, Giannarini G, Tonetto F, Urpis M, Crespi M, Foti C, Prisco A, Polsinelli M, De Giorgi G, Bravo G, Scalchi P, Trovò M (2018) Hypofractionated simultaneous integrated boost (IMRT-SIB) with pelvic nodal irradiation and concurrent androgen deprivation therapy for high-risk prostate cancer: results of a prospective phase II trial. Prostate Cancer Prostatic Dis 21(2):269–276. https://doi.org/10.1038/s41391-018-0034-0
Chang MG, Mukhopadhyay N, Holdford D, Skinner V, Saraiya S, Moghanaki D, Anscher MS (2018) Phase 1/2 study of hypofractionated intensity-modulated radiation therapy for prostate cancer including simultaneously integrated boost. Pract Radiat Oncol 8(3):e149–e157. https://doi.org/10.1016/j.prro.2017.09.007
Alongi F, Fogliata A, Navarria P, Tozzi A, Mancosu P, Lobefalo F, Reggiori G, Clivio A, Cozzi L, Scorsetti M (2012) Moderate hypofractionation and simultaneous integrated boost with volumetric modulated arc therapy (RapidArc) for prostate cancer. Report of feasibility and acute toxicity. Strahlenther Onkol 188(11):990–996. https://doi.org/10.1007/s00066-012-0171-7
Aluwini S, Pos F, Schimmel E, Krol S, van der Toorn PP, de Jager H et al (2016) Hypofractionated versus conventionally fractionated radiotherapy for patients with prostate cancer (HYPRO): late toxicity results from a randomised, non-inferiority, phase 3 trial. Lancet Oncol 17(4):464–474
Franzese C, Fogliata A, D’Agostino GR, Di Brina L, Comito T, Navarria P, Cozzi L, Scorsetti M (2017) Moderate hypofractionated radiotherapy with volumetric modulated arc therapy and simultaneous integrated boost for pelvic irradiation in prostate cancer. J Cancer Res Clin Oncol 143(7):1301–1309. https://doi.org/10.1007/s00432-017-2375-9
Ferrera G, Mortellaro G, Mannino M, Caminiti G, Spera A, Figlia V, Iacoviello G, Di Paola G, Mazzola R, Lo Casto A, Alongi F, Pappalardo MP, Lagalla R (2015) Moderate hypofractionation and simultaneous integrated boost by helical tomotherapy in prostate cancer: monoinstitutional report of acute tolerability assessment with different toxicity scales. Radiol Med 120(12):1170–1176. https://doi.org/10.1007/s11547-015-0555-8
Longobardi B, Berardi G, Fiorino C, Alongi F, Cozzarini C, Deli A, La Macchia M, Perna L, Di Muzio NG, Calandrino R (2011) Anatomical and clinical predictors of acute bowel toxicity in whole pelvis irradiation for prostate cancer with tomotherapy. Radiother Oncol 101(3):460–464. https://doi.org/10.1016/j.radonc.2011.07.014
Jorgo K, Polgar C, Major T, Stelczer G, Herein A, Pocza T, Gesztesi L, Agoston P (2019) Acute and late toxicity after moderate hypofractionation with simultaneous integrated boost (SIB) radiation therapy for prostate cancer. A single institution, prospective study. Pathol Oncol Res. https://doi.org/10.1007/s12253-019-00623-2
Shaikh T, Li T, Handorf EA, Johnson ME, Wang LS, Hallman MA, Greenberg RE, Price RA Jr, Uzzo RG, Ma C, Chen D, Geynisman DM, Pollack A, Horwitz EM (2017) Long-term patient-reported outcomes from a phase 3 randomized prospective trial of conventional versus hypofractionated radiation therapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 97(4):722–731. https://doi.org/10.1016/j.ijrobp.2016.12.034
Leibel SA, Fuks Z, Zelefsky MJ, Whitmore WF Jr (1994) The effects of local and regional treatment on the metastatic outcome in prostatic carcinoma with pelvic lymph node involvement. Int J Radiat Oncol Biol Phys 28(1):7–16
Asbell SO, Krall JM, Pilepich MV, Baerwald H, Sause WT, Hanks GE, Perez CA (1988) Elective pelvic irradiation in stage A2, B carcinoma of the prostate: analysis of RTOG 77-06. Int J Radiat Oncol Biol Phys 15(6):1307–1316
Pommier P, Chabaud S, Lagrange JL, Richaud P, Lesaunier F, Le Prise E, Wagner JP, Hay MH, Beckendorf V, Suchaud JP, Pabot du Chatelard PM, Bernier V, Voirin N, Perol D, Carrie C (2007) Is there a role for pelvic irradiation in localized prostate adenocarcinoma? Preliminary results of GETUG-01. J Clin Oncol 25(34):5366–5373
Lawton CA, DeSilvio M, Roach M 3rd et al (2007) An update of the phase III trial comparing whole pelvic to prostate only radiotherapy and neoadjuvant to adjuvant total androgen suppression: updated analysis of RTOG 94-13, with emphasis on unexpected hormone/radiation interactions. Int J Radiat Oncol Biol Phys 69:646–655
Dearnaley D, Griffin CL, Lewis R, Mayles P, Mayles H, Naismith OF, Harris V, Scrase CD, Staffurth J, Syndikus I, Zarkar A, Ford DR, Rimmer YL, Horan G, Khoo V, Frew J, Venkitaraman R, Hall E (2019) Toxicity and patient-reported outcomes of a phase 2 randomized trial of prostate and pelvic lymph node versus prostate only radiotherapy in advanced localised prostate cancer (PIVOTAL). Int J Radiat Oncol Biol Phys 103(3):605–617. https://doi.org/10.1016/j.ijrobp.2018.10.003
Carvalho ÍT, Baccaglini W, Claros OR, Chen FK, Kayano PP, Lemos GC, Weltman E, Kuban DA, Carneiro A (2018) Genitourinary and gastrointestinal toxicity among patients with localized prostate cancer treated with conventional versus moderately hypofractionated radiation therapy: systematic review and meta-analysis. Acta Oncol 57(8):1003–1010. https://doi.org/10.1080/0284186X.2018.1478126
Jereczek-Fossa BA, Surgo A, Maisonneuve P, Maucieri A, Gerardi MA, Zerini D, Marvaso G, Ciardo D, Volpe S, Rojas DP, Riva G, Alessandro O, Dicuonzo S, Fanetti G, Romanelli P, Starzyńska A, Cattani F, Cambria R, Fodor C, Garibaldi C, Romanò C, De Cobelli O, Orecchia R (2019) Late toxicity of image-guided hypofractionated radiotherapy for prostate: non-randomized comparison with conventional fractionation. Radiol Med 124(1):65–78. https://doi.org/10.1007/s11547-018-0937-9
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflict of interests.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cuccia, F., Mortellaro, G., Trapani, G. et al. Acute and late toxicity and preliminary outcomes report of moderately hypofractionated helical tomotherapy for localized prostate cancer: a mono-institutional analysis. Radiol med 125, 220–227 (2020). https://doi.org/10.1007/s11547-019-01095-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-019-01095-9