Abstract
Introduction
Based on radiobiology evidence, hypofractionated radiotherapy has the potential of improving treatment outcome in prostate cancer patients. In this study, we evaluated the safety, in terms of acutetoxicity, of using moderate hypofractionated radiotherapy delivered with Helical Tomotherapy (HT) to treat prostate cancer patients.
Materials and methods
Between December 2012 and April 2014, 42 consecutive patients were treated with hypofractionated radiotherapy using HT. All patients received 70 Gy in 28 fractions to PTV1, which included the prostate. In the intermediate risk group, 61.6 Gy were delivered to PTV2, which included the seminal vesicles. In high risk patients, the pelvic nodes were added (PTV3) and received 50.4 Gy. Acute toxicity was recorded prospectively with RTOG and Common Terminology Criteria for Adverse Events 3.0, retrospectively with CTCAE 4.0. Expanded Prostate Cancer Index Composite (EPIC) was measured at baseline and 3 months after end of treatment, to investigate health related quality of life with regards to bladder and gastrointestinal function.
Results
Acute toxicity was acceptable, independently from the system used to score side effects. Moderate genitourinary toxicity was more frequent than gastrointestinal toxicity. No correlation between acute side effects and patients’ characteristics or physical dose parameters was registered. EPIC evaluation showed a negligible difference in urinary and bowel function post-treatment, that did not reach statistical significance.
Conclusions
Our experience confirms the safety of moderate hypofractionation delivered with HT in prostate cancer patients with low, intermediate and high risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PC) is the most commonly diagnosed non-skin cancer in men and it is estimated as the second leading cause of cancer death [1]. High-energy external beam radiation therapy (EBRT) represents one of the standard definitive treatment options for localized PC. In order to achieve satisfying local and biochemical control with conformal radiation treatment, doses greater than 76 Gy are necessary [2–4]. These doses are usually delivered with standard fractionation schedules using 1.8–2 Gy fractions. With intensity-modulated radiation therapy (IMRT), doses up to 81 Gy can be safely delivered, given that this technique is characterized by a high degree of conformality, which allows dose escalation to the target volume while significantly reducing normal tissue involvement [5]. Another important benefit of IMRT in PC radiotherapy treatment is that it allows delivery of various doses to different volumes in the same number of fractions: this technique, known as simultaneous integrated boost (SIB), is applied to irradiate lymph nodes, seminal vesicles, and prostate concomitantly during the same session [6]. One of the main challenges of IMRT in PC is that the steep dose gradient achieved with this technique introduces the need to take into account prostate interfraction and intrafraction motion to ensure an accurate delivery of the prescribed dose. Different modalities of image-guided radiation therapy (IGRT) are used to reduce variations in the coverage of the planning target volume, allowing at the same time organ at risk sparing [7]. Radiobiology studies estimate a prostate α/β value of 1–3 Gy [8–10], lower than those identified for rectum and bladder. These findings formed the rationale for studies testing the possibility of improving the therapeutic ratio with hypofractionation schedules [11–13]. Various schedules were tested in these studies, from 2.5–3 Gy per fraction (moderate hypofractionation) to 7 Gy per fraction (extreme hypofractionation) [14–18]. Only the data relative to moderate hypofractionation are considered mature for clinical implementation.
We report our preliminary clinical experience with moderate hypofractionation SIB using helical tomotherapy (HT, Accuray, Inc. Sunnyvale, CA, USA), which combines IMRT, delivered by a helical system, and image guidance, based on megavoltage CT scans.
Materials and methods
Between December 2012 and April 2014, 42 consecutive patients with a histologic diagnosis of localized PC were recruited and definitively treated with HT. Diagnosis was performed by ultrasound-guided biopsy or TURP. Patients characteristics are shown in Table 1.
In accordance with NCCN, three risk groups were identified: low risk (clinical stage T1–T2a, Gleason score ≤6, PSA ≤10 ng/ml), intermediate risk (clinical stage T2b–T2c or Gleason score 7 or PSA 10–20 ng/ml T1–T2, Gleason score ≤6, PSA >10 or clinical stage T1–T2, Gleason >6, PSA ≤10 or clinical stage T3, Gleason score <6, PSA <10), and high risk (clinical stage T1–T3a, Gleason score 8–10, PSA >20 ng/ml) [19].
Most patients received neoadjuvant, concomitant, and adjuvant hormonal therapy of variable duration, according to the stage, the risk group, and the physician’s decisions. All patients underwent CT simulation, with a 2.5-mm slice thickness, in the supine position, using vac lock as immobilization devices. To reduce discrepancies in bladder and rectum volumes between simulation and treatment, each patient followed a predefined bladder-filling protocol: patients drank 500 ml of water, 30 min before the CT scan, to achieve a comfortably full bladder, and emptied their bowel by a self-administered enema. Clinical target volumes (CTVs) and organs at risk (OAR) were contoured on the Pinnacle Planning system; rectum, bladder, and femoral heads were contoured as solid organs, small bowel as whole intestinal cavity. The CT datasets were then transferred to the Tomotherapy Treatment Planning system (HT, Accuray Inc. Sunnyvale, CA, USA), where IMRT plans were generated with inverse treatment planning. CTV1 was the prostate gland, CTV2 the seminal vesicles, and CTV3 the pelvic lymph nodes. Planning target volumes (PTV) 1 and 2 were defined, respectively, as CTV 1 and 2 plus a 0.8 cm margin except for the prostate-rectal interface, where a 0.6 cm margin was used; PTV3 was generated adding a 0.5 cm margin to CTV3. The target volume for low-risk patients was PTV1; PTV2 only and PTV2 and PTV3 were added for intermediate and high-risk patients, respectively. Total dose in 28 fractions, using SIB technique, was 70, 61.6, and 50.4 Gy to PTV1, PTV2, and PTV3, respectively. Target dose coverage for PTV1 was evaluated by Homogeneity Index (HI) and Conformity Index (CI) [20, 21].
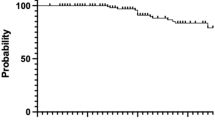
We chose this fractionation schedule based on the results of the largest patient series reporting the safety of HFRT compared to conventional fractionation [22, 23]. Dose-volume constraints for normal tissue were as follows: rectum V56 < 35 %, V60 < 25 %, and V65 < 15 %; bladder V55 < 50 % and V60 < 30 %; femoral head Dmax <50 Gy and V46.2 < 5 %. For the intestinal cavity, the prescription was to reduce the dose as low as possible. Before each fraction, daily megavoltage tomography (MCVT) was performed for set up verification, as shown in Fig. 1. To address the possible under reporting of certain side effects using a single scale, acute toxicity was prospectively recorded according both to RTOG and Common Terminology Criteria for Adverse Events (CTCAE V3.0) [24, 25]. We retrospectively evaluated toxicity also according to CTCAE 4.0 [26]. Patients were monitored every week during treatment, at 1 month from the end of RT and every 3 months for 1 year. Acute genitourinary (GU) and gastrointestinal (GI) toxicity was defined as an increase of any symptom during radiation or within 3 months after the end of treatment. The Expanded Prostate Cancer Index Composite (EPIC-26) questionnaire at baseline and at 3 months follow-up was used to evaluate health-related quality of life (HRQOL) after treatment relatively to bladder and gastrointestinal function [27]. Rectum and bladder dosimetric parameters were retrospectively evaluated for the statistical analysis.
Statistical analysis
Continuous variables were analyzed with descriptive statistics (mean, median, IQR, max, min, range). End points were analyzed using univariate, multiple logistic regression and contingence tables with Fisher’s exact test for the association between GU and GI toxicity, dose-volume, and clinical parameters. p ≤ 0.05 were considered significant. All analyses were performed using R-3.1.0. Responses to the EPIC-26 questionnaire were grouped by physiologic domains and assigned numerical scores. The multi-item scale scores were transformed linearly to a 0–100 scale, as recommended in the scoring instructions for the EPIC-26. We used the Wilcoxon signed-rank test to compare the baseline and the 3 month follow-up EPIC scores.
Results
The median follow-up was 12 months (range 3–20 months). The median age of the population of the study was 75 years (range 62–82 years). Gleason score was ≤6 in 26 (62 %) patients, 7 in 8 (19 %) and ≥8 in 8 (19 %) patients. The median pre-treatment prostate-specific antigen (PSA) was 7.46 ng/ml (range 1.35–90 ng/ml). According to the risk group classification, 16 (38 %), 10 (24 %) and 16 (38 %) patients were classified as low, intermediate, and high risk, respectively. Mean doses to PTV1, PTV2, and PTV3 were 70.2 Gy (range 69.03–70.87), 62.57 Gy (range 61.47–66.04), and 50.79 Gy (range 50.47–51.49), respectively. The CI and HI indices as mean values ± standard deviation were 1.18 ± 0.47 and 0.056 ± 0.02. The median volume of the bladder that received 55 Gy (V55) was 38 % (range 11–61), median V60 was 29 % (range 5–50), and median V70 was 6 % (range 0–19). Median V56, V60, and V65 for the rectum were 31.8 % (range 11–42) 21 % (range 11–32) and 11.5 % (range 4–21), respectively (Table 2).
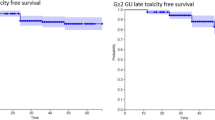
Acute G1, G2, and G3 GI toxicity occurred in 12 (28 %), 3 (7 %), and 1 (2 %) patients, according to the RTOG scale. According to CTCAE3.0., 10 (24 %) and 3 (7 %) patients had G1 and G2 GI toxicity, respectively. Acute G1 and G2 GU toxicity occurred in 27 (64 %) and 2 (4 %) patients according to RTOG and in 23 (55 %) and 6 (14 %) patients according to the CTCAE 3.0 scale. Retrospectively evaluated CTCAE 4.0 showed the same rates of GI toxicity but more frequent GU toxicity compared to the CTCAE 3.0 version (Table 3).
Table 4 shows the specific symptoms events according to CTCAE v 4.0. There was no statistical correlation between acute GU-GI toxicity and physical dose parameters. There was a slight increase in acute toxicity in patients that received radiotherapy to the pelvic lymph nodes, but this correlation did not reach statistical significance. According to the EPIC questionnaire scores, there was no statistical difference in urinary function (p = 0.7735) and bowel function (p = 0.3326) between the baseline and the 3 month evaluation (Table 5).
Discussion
Our preliminary clinical experience with moderate hypofractionation with SIB using helical tomotherapy confirmed that, with this delivery technique, acute toxicities are quite low and similar with other moderate hypofractionation experiences in this setting, as shown in Table 6. Given that scoring side effects with a single scale was associated with under reporting, we used three systems, two prospectively and one retrospectively. Results from all scales showed that toxicity rates were acceptable independently from the system used to score side effects. Our results are also comparable with those of other studies using HT. Similarly to these and other IMRT studies, GU side effects were slightly more frequent than GI ones. In our series, there was no association between toxicity and clinical or dosimetric parameters. Interpretation of these findings in the light of other published data is difficult due to differences in treatment schedules and dishomogeneity of treated populations. Lopez Guerra et al. [28] found that GU toxicity ≥G2 was correlated, in a multivariate analysis, with total radiation dose ≥70 Gy and dose per fraction >2.52 Gy, but not with the percentage of bladder volume receiving a specific dose. Keiler et al. [29] found that increased GU toxicity was correlated with median bladder dose and bladder dose dishomogeneity. Kong et al. [30] registered a relationship between G1 and G2 GU toxicity and bladder V40 and V50, but not with lower or higher bladder dosimetric values. Evaluation of the relationship between GU toxicity and dosimetric parameters is also hampered by possible variations in bladder filling, i.e., bladder volume, throughout radiotherapy treatment. To address this issue, two of the studies cited above used bladder-filling protocols, similarly to our institution. Efficacy of this approach is currently questioned, given that several reports demonstrated that variation in bladder filling throughout radiotherapy treatment is not eliminated, despite the use of various protocols [31–34]. Consistent with these findings are the results of a retrospective analysis we performed on 15 patients from our series, evaluating changes in bladder volume by recontouring this organ in all daily MVCTs: we observed a considerable bladder volume variation, which was significantly correlated with the received dose. With regard to GI side effects, we observed only a single episode of rectal bleeding in one patient, which we scored as G3 according to the RTOG scale and G2 in the other two systems. This favorable toxicity profile confirms the safety of expanding the PTV posteriorly with a margin of 0.6 cm, which was larger than those used in the three studies mentioned above. We chose a 0.6 cm margin based on published data showing that prostate volume varies during the course of radiotherapy treatment and that tighter margins are associated to lower rates of 5-year freedom from biochemical failure [35, 36].
New advances in radiation modalities, such as the use of IGRT, resulted in less volume of bladder exposed to the high doses of irradiation, translating into a reduced incidence of toxicity [7]. The acceptable toxicity observed in the current analysis may possibly be explained by more consistent coverage of the target using IGRT with less percentage of OARs radiation exposure. The acute toxicity profile was also favorable in patients that received limphnode irradiation, suggesting that high-risk patients can be treated safely with moderate hypofractionation using HT. The Dmean to the intestinal cavity, contoured as OAR, was 29.12 Gy (range 21.5–39.2), confirming that HT allows delivery of high doses to the target volume while sparing the other organs present in the pelvis. Consistent with these findings, Cozzarini et al. [37] reported a Dmean to the intestinal cavity of 23.37 (range 19–30.6) and low incidence of acute G2 toxicity in patients irradiated to the prostate and pelvic lymphonodes. Keeping in mind the limitations related to the limited sample size, our study shows that delivering moderate hypofractionated radiotherapy with HT is safe, based on the evaluation of side effects using three toxicity scales and a HRQOL questionnaire.
Although the lack of a comparison with conventional fractionation is a limitation of the present study, our findings revealed that toxicity rates were acceptable independently from the system used to score side effects, in a series of radical prostate cancer submitted to moderate hypofractionation and simultaneous integrated boost by helical tomotherapy.
References
Siegel R, Naishadham D, Jemal A (2013) Cancer statistics. CA Cancer J Clin 63(1):11–30. doi:10.3322/caac.21166
Pollack A, Zagars GK, Starkschall G, Antolak JA, Lee JJ, Huang E, von Eschenbach AC, Kuban DA, Rosen I (2002) Prostate cancer radiation dose response: results of the M. D. Anderson phase III randomized trial. Int J Radiat Oncol Biol Phys 53(5):1097–1105
Zietman AL, DeSilvio ML, Slater JD, Rossi CJ Jr, Miller DW, Adams JA, Shipley WU (2005) Comparison of conventional-dose vs high-dose conformal radiation therapy in clinically localized adenocarcinoma of the prostate: a randomized controlled trial. JAMA 294(10):1233
Zelefsky MJ, Fuks Z, Hunt M, Yamada Y, Marion C, Ling CC (2002) High-dose intensity modulated radiation therapy for prostate cancer: early toxicity and biochemical outcome in 772 patients. Int J Radiat Oncol Biol Phys 53:1111–1116
Alongi F, Fiorino C, Cozzarini C, Broggi S, Perna L, Cattaneo GM, Calandrino R, Di Muzio N (2009) IMRT significantly reduces acute toxicity of whole-pelvis irradiation in patients treated with post-operative adjuvant or salvage radiotherapy after radical prostatectomy. Radiother Oncol 93(2):207–212. doi:10.1016/j.radonc.2009.08.042
Fiorino C, Alongi F, Broggi S, Cattaneo GM, Cozzarini C, Di Muzio N, Maggiulli E, Mangili P, Perna L, Valdagni R, Fazio F, Calandrino R (2008) Physics aspects of prostate tomotherapy: planning optimization and image-guidance issues. Acta Oncol 47(7):1309–1316
Zelefsky MJ, Kollmeier M, Cox B, Fidaleo A, Sperling D, Pei X, Carver B, Coleman J, Lovelock M, Hunt M (2012) Improved clinical outcomes with high-dose image guided radiotherapy compared with non-IGRT for the treatment of clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 84(1):125–129
Proust-Lima C, Taylor JM, Sécher S, Sandler H, Kestin L, Pickles T, Bae K, Allison R, Williams S (2011) Confirmation of a low α/β ratio for prostate cancer treated by external beam radiation therapy alone using a post-treatment repeated-measures model for PSA dynamics. Int J Radiat Oncol Biol Phys 79(1):195–201. doi:10.1016/j.ijrobp.2009.10.008
Miralbell R, Roberts SA, Zubizarreta E, Hendry JH (2012) Dose-fractionation sensitivity of prostate cancer deduced from radiotherapy outcomes of 5,969 patients in seven international institutional datasets: α/β = 1.4 (0.9 − 2.2) Gy. Int J Radiat Oncol Biol Phys 82(1):e17–e24
Leborgne F, Fowler J, Leborgne JH, Mezzera J (2012) Later outcomes and alpha/beta estimate from hypofractionated conformal three-dimensional radiotherapy versus standard fractionation for localized prostate cancer. Int J Radiat Oncol Biol Phys 82(3):1200–1207
Arcangeli G, Saracino B, Gomellini S, Petrongari MG, Arcangeli S, Sentinelli S, Marzi S, Landoni V, Fowler J, Strigari L (2010) A prospective phase III randomized trial of hypofractionation versus conventional fractionation in patients with high-risk prostate cancer. Int J Radiat Oncol Biol Phys 78(1):11–18. doi:10.1016/j.ijrobp.2009.07.169112
Soete G, Arcangeli S, De Meerleer G, Landoni V, Fonteyne V, Arcangeli G, De Neve W, Storme G (2006) Phase II study of a four-week hypofractionated external beam radiotherapy regimen for prostate cancer: report on acute toxicity. Radiother Oncol 80(1):78–81
Di Muzio N, Fiorino C, Cozzarini C, Alongi F, Broggi S, Mangili P, Guazzoni G, Valdagni R, Calandrino R, Fazio F (2009) Phase I-II study of hypofractionated simultaneous integrated boost with tomotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 74(2):392–398. doi:10.1016/j.ijrobp.2008.08.038
Lukka H, Hayter C, Julian JA, Warde P, Morris WJ, Gospodarowicz M, Levine M, Sathya J, Choo R, Prichard H, Brundage M, Kwan W (2005) Randomized trial comparing two fractionation schedules for patients with localized prostate cancer. J Clin Oncol 23(25):6132–6138
Pollack A, Hanlon AL, Horwitz EM, Feigenberg SJ, Konski AA, Movsas B, Greenberg RE, Uzzo RG, Ma CM, McNeeley SW, Buyyounouski MK, Price RA Jr (2006) Dosimetry and preliminary acute toxicity in the first 100 men treated for prostate cancer on a randomized hypofractionation dose escalation trial. Int J Radiat Oncol Biol Phys 64(2):518–526
Dearnaley D, Syndikus I, Sumo G, Bidmead M, Bloomfield D, Clark C, Gao A, Hassan S, Horwich A, Huddart R, Khoo V, Kirkbride P, Mayles H, Mayles P, Naismith O, Parker C, Patterson H, Russell M, Scrase C, South C, Staffurth J, Hall E (2012) Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: preliminary safety results from the CHHiP randomised controlled trial. Lancet Oncol 13(1):43–54. doi:10.1016/S1470-2045(11)70293-5
Katz AJ, Kang J (2014) Quality of life and toxicity after SBRT for organ-confined prostate cancer, a 7-year study. Front Oncol 28(4):301. doi:10.3389/fonc.2014.00301
Arcangeli S, Scorsetti M, Alongi F (2012) Will SBRT replace conventional radiotherapy in patients with low-intermediate risk prostate cancer? A review. Crit Rev Oncol Hematol 84(1):101–108. doi:10.1016/j.critrevonc.2011.11.009
NCCN Clinical Practice Guidelines in Oncology (NCCNGuidelines®) prostate cancer2014version4. http://www.nccn.org/professionals/physician_gls/f_guidelines.asp#prostate
ICRU Report 83. 3 (2010) Special considerations regarding absorbed-dose and dose–volume prescribing and reporting in IMRT. J ICRU 10:14
ICRU Report 62 (1999) Prescribing, recording and reporting photon beam therapy. Bethesda (MD): International Commission on Radiation Units and Measurements
Kupelian PA, Willoughby TR, Reddy CA, Klein EA, Mahadevan A (2007) Hypofractionated intensity-modulated radiotherapy (70 Gy at 2.5 Gy per fraction) for localized prostate cancer: Cleveland Clinic experience. Int J Radiat Oncol Biol Phys 68(5):1424–1430
Kotecha R, Marwaha G, Hearn JW, Weller MA, Kupelian P, Reddy CA, Ciezki JP, Stephans K, Tendulkar RD (2014) A comparison of long-term treatment-related toxicities between moderately hypofractionated and conventionally fractionated radiation therapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 90(1, Supplement):S423–S424
Acute Radiation Morbidity Scoring Criteria RTOG. http://www.rtog.org/ResearchAssociates/AdverseEventReporting/AcuteRadiationMorbidityScoringCriteria.aspx
Common Terminology Criteria for Adverse Events,Version 3.0: http://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcaev3.pdf
Common Terminology Criteria for Adverse Events,Version 4.0 http://evs.nci.nih.gov/ftp1/CTCAE/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf
Sanda MG, Rl Dunn, Michalski J et al (2008) Qaulity of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med 358:1250–1261
Lopez Guerra JL, Isa N, Matute R, Russo M, Puebla F, Kim MM, Sanchez-Reyes A, Beltran C, Jaen J, Bourgier C, Marsiglia H (2013) Hypofractionated helical tomotherapy using 2.5-2.6 Gy daily fractions for localized prostate cancer. Clin Transl Oncol 15(4):271–277. doi:10.1007/s12094-012-0907-y
Keiler L, Dobbins D, Kulasekere R, Einstein D (2007) Tomotherapy for prostate adenocarcinoma: a report on acute toxicity. Radiother Oncol 84(2):171–176
Kong M, Hong SE, Chang SG (2014) Hypofractionated helical tomotherapy (75 Gy at 2.5 Gy per fraction) for localized prostate cancer: long-term analysis of gastrointestinal and genitourinary toxicity. Onco Target Ther 7:553–566. doi:10.2147/OTT.S61465
Nakamura N, Shikama N, Takahashi O, Ito M, Hashimoto M, Uematsu M, Hama Y, Sekiguchi K, Nakagawa K (2010) Variability in bladder volumes of full bladders in definitive radiotherapy for cases of localized prostate cancer. Strahlenther Onkol 186(11):637–642. doi:10.1007/s00066-010-2105-6
O’Doherty UM, McNair HA, Norman AR, Miles E, Hooper S, Davies M, Lincoln N, Balyckyi J, Childs P, Dearnaley DP, Huddart RA (2006) Variability of bladder filling in patients receiving radical radiotherapy to the prostate. Radiother Oncol 79(3):335–340
Stam MR, van Lin EN, van der Vight LP, Kaanders JH, Visser AG (2006) Bladder filling variation during radiation treatment of prostate cancer: can the use of a bladder ultrasound scanner and biofeedback optimize bladder filling? Int J Radiat Oncol Biol Phys 65(2):371–377
Hynds S, McGarry CK, Mitchell DM, Early S, Shum L, Stewart DP, Harney JA, Cardwell CR, O’Sullivan JM (2011) Assessing the daily consistency of bladder filling using an ultrasonic Bladderscan device in men receiving radical conformal radiotherapy for prostate cancer. Br J Radiol 84(1005):813–818. doi:10.1259/bjr/50048151
King BL, Butler WM, Merrick GS, Kurko BS, Reed JL, Murray BC, Wallner KE (2011) Electromagnetic transponders indicate prostate size increase followed by decrease during the course of external beam radiation therapy. Int J Radiat Oncol Biol Phys 79(5):1350–1357. doi:10.1016/j.ijrobp.2009.12.053
Engels B, Soete G, Gevaert T, Storme G, Michielsen D, De Ridder M (2014) Impact of planning target volume margins and rectal distention on biochemical failure in image-guided radiotherapy of prostate cancer. Radiother Oncol 111(1):106–109. doi:10.1016/j.radonc.2014.02.009
Cozzarini C, Fiorino C, Di Muzio N, Alongi F, Broggi S, Cattaneo M, Montorsi F, Rigatti P, Calandrino R, Fazio F (2007) Significant reduction of acute toxicity following pelvic irradiation with helical tomotherapy in patients withlocalized prostate cancer. Radiother Oncol 84(2):164–170
Barra S, Vagge S, Marcenaro M, Blandino G, Timon G, Vidano G, Agnese D, Gusinu M, Cavagnetto F, Corvò R (2014) Image guided hypofractionated radiotherapy by helical tomotherapy for prostate carcinoma: toxicity and impact on Nadir PSA. Biomed Res Int 2014:541847. doi:10.1155/2014/541847
Alongi F, Fogliata A, Navarria P, Tozzi A, Mancosu P, Lobefalo F, Reggiori G, Clivio A, Cozzi L, Scorsetti M (2012) Moderate hypofractionation and simultaneous integrated boost with volumetric modulated arc therapy (RapidArc) for prostate cancer. Report of feasibility and acute toxicity. Strahlenther Onkol 188(11):990–996. doi:10.1007/s00066-012-0171-7
Geier M, Astner ST, Duma MN, Jacob V, Nieder C, Putzhammer J, Winkler C, Molls M, Geinitz H (2012) Dose-escalated simultaneous integrated-boost treatment of prostate cancer patients via helical tomotherapy. Strahlenther Onkol 188(5):410–416. doi:10.1007/s00066-012-0081-8
Jereczek-Fossa BA, Santoro L, Zerini D, Fodor C, Vischioni B, Dispinzieri M, Bossi-Zanetti I, Gherardi F, Bonora M, Caputo M, Vavassori A, Cambria R, Garibaldi C, Cattani F, Matei DV, Musi G, De Cobelli O, Orecchia R (2013) Image-guided hypofractionated radiotherapy and quality of life in localized prostate cancer: prospective longitudinal study on 337 patients. J Urol
Martin JM, Rosewall T, Bayley A, Bristow R, Chung P, Crook J, Gospodarowicz M, McLean M, Menard C, Milosevic M, Warde P, Catton C (2007) Phase II trial of hypofractionated image-guided intensity-modulated radiotherapy for localized prostate adenocarcinoma. Int J Radiat Oncol Biol Phys 69:1084–1089
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standards
This article does not contain any studies with human participants or animals performed by any of the authors.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrera, G., Mortellaro, G., Mannino, M. et al. Moderate hypofractionation and simultaneous integrated boost by helical tomotherapy in prostate cancer: monoinstitutional report of acute tolerability assessment with different toxicity scales. Radiol med 120, 1170–1176 (2015). https://doi.org/10.1007/s11547-015-0555-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-015-0555-8