Abstract
Young black men who have sex with men (YBMSM) and young black transgender women (TGW) have experienced a stark disparity in HIV prevention and care. Resilience, collective resources to adapt stressors or adversities, may improve HIV prevention and care outcomes. The present study investigated the association of resilience-based factors with PrEP uptake and viral suppression from a socioecological perspective among YBMSM and young black TGW. Data were from the baseline cycle of the Neighborhoods and Networks (N2) Study, an ongoing cohort study of 16–34-year-old YBMSM and young black TGW in Chicago (n = 324). Confidant network-level and neighborhood affiliation variables were created to measure the social-environmental context of resilience. All analyses were stratified by participants’ HIV status (184 HIV-negative participants and 140 HIV-positive participants). Among HIV-negative participants, having a parental figure within an individual’s confidant network was significantly associated with a greater likelihood of PrEP use. Among HIV-positive participants, confidant network members’ awareness of an individual’s HIV status was associated with viral suppression. Social support resources from confidant networks could improve HIV prevention and care engagement among YBMSM and young black TGW. Understanding the social and environmental contexts of resilience resource is critical for HIV prevention and care engagement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Young black men who have sex with men (YBMSM) and young black transgender women (TGW) bear a particular high risk for HIV infection. In the United States (US), the Centers for Disease Control and Prevention (CDC) estimates that 1 in 2 young black MSM is expected to be diagnosed with HIV infection within their lifetime [1] and a systematic review published in 2019 estimated that 44% of black TGW are living with HIV infection [2]. Theoretical and empirical work suggests that such high HIV prevalence among these vulnerable populations is not driven by factors at individual level, as black MSM, for example, are often no more likely to engage in behaviors that increase risk of HIV infection (e.g., using drugs during sex, condomless anal intercourse) [3, 4]. Rather, the racial disparity in HIV incidence is produced and perpetuated by more distal factors, including the characteristics of networks and neighborhood environments [3,4,5,6].
Essential to the national goal of zero new HIV infections, public health efforts need to prioritize preventing HIV in vulnerable communities and ensuring that individuals living with HIV infection have sustained access to antiretroviral treatment and maintain an undetectable viral load [7]. Both strategies dramatically decrease the risk of HIV transmission and acquisition. When taken as directed, pre-exposure prophylaxis (PrEP) reduces the risk of HIV acquisition among MSM by more than 92% [8], while people living with HIV infection who have achieved viral load suppression bear no risk of forward HIV transmission to their partners [9]. Past research has often focused separately on HIV prevention among HIV-negative individuals or on HIV treatment among individuals living with HIV infection. Limited research has used an integrated or neutral approach to examine engagement in HIV prevention and care. Such an approach could strengthen our understandings of factors related to a broader spectrum of engagement in the HIV care continuum and may provide insights into similarities and differences in factors that impact engagement in biomedical prevention for HIV-negative and HIV-positive individuals [10].
In addition to the disproportionate burden of HIV among YBMSM and young black TGW, they continue to experience stark racial disparities in HIV prevention and care [3, 11, 12]. Black persons assigned male at birth have different gender identities and expressions, but they often share similar challenges (e.g., stigma, economic deprivation, and violence) and spend time in similar spaces (e.g., isolated black community, ballroom/house communities) [13, 14]. While the CDC recently estimated 61% of the adults with indications for PrEP use in the US were black MSM, a nationwide survey of MSM at high risk for HIV infection shows that about 26% of black MSM used PrEP [15]. A multi-city study shows that only 8% of at-risk TGW had access to PrEP [16]. Based on the National HIV Surveillance System, black MSM had the lowest percentages of retention in care (53%) and viral suppression (52%) among all other races and ethnicities [17].
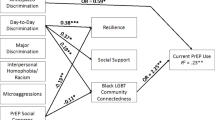
Resilience resources, defined broadly as the collective resources to adapt stressors or adversities, may promote HIV prevention and care behaviors and potentially enable YBMSM and young black TGW to overcome the structural barriers and contextual adversity [18,19,20,21]. Herrick et al. [20] recently proposed a theoretically driven resilience framework for HIV prevention among MSM and emphasized that resilience operated at different levels as the individual resilience characteristics depending on the presence of social-environmental factors to develop and maintain. To date, emerging research has examined how resilience-based factors may influence HIV-related outcomes among MSM [22,23,24,25]. However, these studies overwhelmingly focus on individual-level resilience resources or only measure the cognitive aspect of resilience. Based on McLeroy’s social ecological framework, individual health behaviors are influenced by factors at multiple levels (i.e., individual, interpersonal, community, and policy levels) [26]. Few studies have explored how network or neighborhood resilience resources are associated with HIV-related outcomes from a socioecological perspective among MSM [27,28,29,30,31,32]. Even fewer studies have used this socioecological resilience-based approach to understand HIV prevention and care such as PrEP outcomes and HIV treatment among MSM populations, especially young black MSM and black TGW [29, 30, 33, 34]. Specifically, to our knowledge, only two quantitative studies have examined the association between resilience-based factors and HIV prevention and care among YBMSM and none among YBTGW [33, 34]. One study showed that informal local social affiliation, which may play a key role in distributing HIV health services information, shaped YBMSM’s awareness of PrEP and viral suppression [33]. Another study demonstrated that disclosure of HIV status to networks, which is a way to access support and resources, was positively associated with engagement in care for YBMSM [34]. These findings suggest that social-environmental context may indeed play an important role in facilitating engagement in prevention and care continuums.
While much of the literature has focused on identifying risk factors that may lead to poor HIV prevention and care outcomes among YBMSM [35,36,37] and TGW [2, 16, 38, 39], researchers have only recently begun to shift away from focus solely on risks and deficits and move the field toward identifying new mechanisms for health promotion in HIV prevention and care [18, 20, 40, 41]. The present study examines whether individual-, network-, and neighborhood-level resilience resources are associated with PrEP use and viral suppression among a population-based sample of YBMSM and young black TGW in Chicago.
Methods
Sample and Data Collection
The data for the current analysis were collected through an ongoing baseline assessment in the Neighborhoods and Networks (N2) Cohort Study, a multi-city study which examined the social contexts of HIV prevention and care cross-sectionally and longitudinally among black MSM and young black TGW. The N2 Study is a multi-city study based in Chicago, IL; Jackson, MS; and New Orleans and Baton Rouge, LA, and the current analysis only includes participants enrolled in Chicago where the baseline data began in February 2018. These are baseline data for participants enrolled through July 2019 (n = 354). The methods of N2 have been described in detail elsewhere [42]. In brief, respondent-driven sampling (RDS) was employed to recruit a representative sample of YBMSM and young black TGW who resided in Chicago. Given low numbers of PrEP uptake among these populations, N2 oversampled eligible HIV-negative seed participants from a random sample of PrEP users. Study participants were eligible to be in the study if they (1) were 16–34 years old, (2) identified as African American or black, (3) were assigned male at birth, (4) reported at least one sexual encounter with another man or a transgender woman in the past year, (5) resided in the Chicago metropolitan statistical area (MSA), (6) reported no plan to move outside of the Chicago MSA for 2 years, (7) were willing to wear a global positioning system (GPS) device, and (8) were willing and able to provide informed consent at the time of the study visit.
Measures
HIV Prevention and Care Outcomes
We stratified participants by their HIV status. The N2 Study provided diagnostic testing for HIV to confirm participants’ HIV status. For HIV-negative participants, the health engagement outcome of focus is current PrEP use. Participants were asked “Are you currently taking PrEP to prevent HIV?” For HIV-positive participants, we focused on viral suppression via the confirmatory HIV test or the electronic medical record from Howard Brown Health Center, which is a healthcare center specifically for lesbian, gay, bisexual, transgender, and queer (LGBTQ) population in Chicago [43]. Viral suppression was defined as having a viral load lower than 200 HIV RNA copied/ml.
Network-Level Resilience Resource Characteristics
As in previous work [44], the N2 Study used a personal network inventory to collect the names of both confidants and sex partners over the past 6 months through a face-to-face interview. The current study only focuses on confidants as they represent network-level resources for resilience. Each participant was asked to name up to 5 confidants. To obtain a list of confidants, participants were asked “In this section, we will ask about your close social network, that is, the people with whom you talk about things that are important to you. Please list the names of the people with whom you talk about things that are important to you.” Once the names of the confidants were generated, participants were asked to describe each confidant in terms of demographic characteristics (e.g., age, employment status) and network-level characteristics (e.g., relationship to the participant).
We included confidant network members’ sociodemographic characteristics, including educational attainment, employment status, and whether confidants were also MSM. We also measured several confidants’ characteristics that would act as a resilience resource for participants at dyadic level, including whether confidants knew participants’ MSM status, confidants knew participant’s HIV status, confidants frequently communicated with participants about their sex life (i.e., more than once a week vs. less than once a week), confidants frequently talked with participants about avoiding acquisition of HIV or other sexually transmitted disease (i.e., more than once a week vs. less than once a week), and whether confidants were also parental figures of participants. All of these confidant variables were originally obtained at the dyadic level. We then transformed each of these dyadic-level variables into a summary proportion variable for each participant. Each of the summary proportion variables was further categorized into a 3-level categorical variable to represent the level of each confidant characteristic for a participant (i.e., 0%, greater than 0% and lower than 100%, and 100%). We collapsed two of the categories if any of the 3-level categories had less than 10 participants to ensure the stability of the analyses.
Neighborhood Affiliations
We measured two neighborhood affiliations for the access to local resources: healthcare affiliation location and socialization affiliation location. Each participant was asked to report up to the top 3 Chicago neighborhoods where they most often went for healthcare and socialized in the past 6 months. Due to the large amount of missing data in the top 2 and top 3 Chicago neighborhood variables, we only retained the top 1 Chicago neighborhood where participants went for healthcare and socialization. Based on past research that found that informal social affiliation with the black community in Chicago has a beneficial effect on HIV prevention and care outcomes [33, 45] we defined social and healthcare affiliation with the south side Chicago, which is the largest black community in the US, as a neighborhood-level resilience resource factor for HIV prevention and care.
Individual-Level Resilience Resource and Covariates
We included participants’ characteristics that could enhance individuals’ resilience resource, including higher level of educational attainment, being employed, greater annual income, and housing stability. Housing stability was measured by two items: (1) living in stable housing that participants own, rent, or stay in as part of a household in the past 6 months and (2) number of moves in the past 6 months. Stable housing was defined as living in stable housing and had moved less than 2 times in the past 6 months. We include participants’ age (recoded based on quartiles), gender identity, and sexual orientation as covariates.
Analyses
All analyses excluded participants if their HIV testing results were unavailable (n = 9) or if HIV-positive participants were missing viral load information (n = 17). Descriptive statistics of each neighborhood-level affiliation, network-level characteristics, and individual-level characteristics were summarized. Bivariate analyses were conducted to explore characteristics associated with the HIV prevention and care outcomes. Multivariable analyses were conducted to determine the adjusted association of the neighborhood-level affiliation, network-level, and individual-level resilience-based characteristics with the outcomes. Logistic regression models were used to estimate the associations. Unadjusted and adjusted odds ratios with 95% confidence intervals were computed, and statistical significance was assessed at p < 0.05. Assessment for collinearity was conducted through variance inflation factor (VIF) values for each predictor and indicated minimal evidence of multicollinearity (VIF < 5 for all variables). All analyses were performed using STATA 14.2 (StataCorp LP, Texas).
Results
Our study sample included 281 YBMSM and 47 young black TGW from the baseline cycle of N2 in Chicago. Within the study sample, there were 184 HIV-negative and 140 HIV-positive YBMSM and young black TGW. Specific to this sample, overall, 58% self-identified as gay, 33% had annual income equal or greater than $USD 20,000, and 70% reported having stable housing in the past 6 months (see Table 1). For HIV-negative participants, the distribution of several individual-level and network-level resilience-based variables significantly differed between current PrEP users and those who did not use PrEP. Compared with those not currently using PrEP, current PrEP users were more commonly employed, reported higher number of confidants, had greater proportions of confidants who were employed, and more frequently talked about their sex lives and methods to avoid HIV acquisition with their confidant networks. The distributions of all resilience-based variables did not significantly differ between participants who were and were not virally suppressed.
Table 2 shows the unadjusted and adjusted associations of neighborhood affiliation, network-level, and individual-level resilience-based variables with PrEP use and viral suppression. After adjusting for individual-level covariates, participants were more likely to use PrEP currently if any of their confidants were a parental figure (AOR 3.51 [1.21, 10.14]). For HIV-positive participants, if all confidants knew participants’ HIV status, participants were more likely to be virally suppressed (AOR 4.76 [1.09, 20.73]). The neighborhood affiliations for socialization and healthcare were not significant in both univariate and multivariable analyses.
Discussion
Our study contributes to the literature by using a socioecological approach to explore how network- and neighborhood-level sources of resilience may be associated with greater HIV prevention and care engagement among YBMSM and young black TGW, which are the populations experiencing profound sexual health disparities and similar socioeconomic disadvantages. At the network-level, we found that YBMSM and young black TGW who were employed and who reported having a parental figure in their confidant network significantly reported higher likelihood of uptake of PrEP. We also found that YBMSM and young black TGW who reported all of their confidants were aware of their HIV status were significantly more likely to be virally suppressed. These results indicate a strong potential for scaling up PrEP uptake and treatment as prevention (TasP) through enhancing network-based social support resources that alleviate sources of stress that may impede engagement with effective HIV prevention and treatment services.
At the network-level, we found several confidant network factors that were associated with PrEP uptake. The result of the protective effect of having a parental figure within one’s confidant network on PrEP uptake contributes a new insight in the literature on PrEP uptake. Our previous work has shown that having two or more family members in YBMSM’s close networks was associated with a lower risk for HIV infection (e.g., less sex-drug use) and a greater HIV intravention (e.g., having more friends who discourage group sex) [46]. Another Chicago-based cohort also found that more than half of participants who were on PrEP reported that they disclosed their PrEP use to their maternal figures; however, sub-group analysis by race was not conducted [47]. Our finding indicates a strong potential of a family-based social capital or social support intervention for improving PrEP uptake among YBMSM and young black TGW that could leverage both families of origin and chosen families.
Among participants living with HIV infection, we found that confidants’ awareness of participants’ HIV status was positively associated with being virally suppressed. To date, most studies that examine HIV serostatus disclosure among MSM only focus on disclosure within sexual partnerships [48,49,50]. Our finding further extends the understanding of HIV status disclosure within close personal networks. A recent study that examined HIV status disclosure to sex partners, family, and friends among YBMSM found that only disclosure to sex partners was associated with better viral suppression, but the authors did not find a significant effect of disclosure to family or friends on viral suppression and other HIV care engagement outcomes [34]. Disclosure of HIV serostatus to individuals’ close network may help with increasing one’s social support, navigation of HIV care services, and the initiation and adherence of HIV treatment. We suggest that interventions promoting disclosure of HIV serostatus should also consider one’s close personal network in addition to one’s sex partners.
At the neighborhood-level, we did not find significant associations of neighborhood affiliation with PrEP use and viral suppression. The lack of significance could have been attributed to factors that were not measured in the baseline data collection in N2 Study such as stigma, transportation access, or medical mistrust, which could directly or indirectly affect both neighborhood affiliation and engagement in prevention and care in complex ways. For example, where YBMSM and TGW spend time to socialize and go for healthcare may be influenced by their perceived stigma regarding their race, gender identity, or sexual orientation from the community or from health providers [30]. Stigma has also been shown to be associated with delayed HIV prevention and care appointments which may limit the effectiveness of biomedical prevention and treatment among black MSM [51, 52]. Nevertheless, as high-quality healthcare services for YBMSM and TGW have recently been introduced in Chicago, it is important that future research examines how healthcare proximity and the affiliation with local social venues are associated with PrEP uptake and HIV treatment and how they are affected by other socio-environmental factors such as stigma and medical mistrust.
The study has a few limitations. First, PrEP uptake in the current study was based on self-report and responses could be subject to social desirability bias. However, social desirability bias for PrEP use in routine care has not been demonstrated in the US. Further interviews were conducted by highly trained interviewers from a professional survey center at the University of Chicago using techniques to minimize reporting of socially desirable responses. Second, the construction of the neighborhood affiliations for socialization and healthcare affiliation relies on the self-report of neighborhoods most commonly visited for socialization and health care. It is likely that some YBMSM and young black TGW spend time in several different areas in the city and there is thus potential for misclassification of neighborhood affiliation. Use of global positioning systems (GPS) may help to better characterize the activity space of our participants and create a more nuanced understanding of their neighborhood affiliation. Third, 26 participants were dropped from the analysis because of lack of HIV testing results or viral load information, though there was no significant difference in terms of the demographics, neighborhood affiliation, and confidant characteristics between participants included and not included in the current analysis. Fourth, although the N2 Chicago site utilizes respondent-driven sampling approach to generate a population-based sample of YBMSM and young black TGW, the results may not be generated to YBMSM and young black TGW in other regions outside Chicago. Lastly, the sample size for HIV-negative and HIV-positive YBMSM was relatively low and thus the analysis may have been underpowered. Future research is warranted to replicate the findings in larger samples.
Conclusions
Our findings emphasize the broader role of social-environmental resilience-based factors in improving HIV prevention and care outcomes. The social resources and support from close personal network of YBMSM and young black TGW can increase PrEP uptake and viral suppression. Neighborhood affiliations for socialization and healthcare were not significantly associated with PrEP uptake and viral suppression in our preliminary results. Future research is warranted to understand how social and environmental contexts of resilience may be impactful to improve HIV prevention and care engagement among most impacted populations.
References
CDC. Lifetime risk of HIV diagnosis in the United States [press release]. Available at: https://www.cdc.gov/nchhstp/newsroom/2016/croi-press-release-risk.html.
Becasen JS, Denard CL, Mullins MM, Higa DH, Sipe TA. Estimating the prevalence of HIV and sexual behaviors among the US transgender population: a systematic review and meta-analysis, 2006-2017. Am J Public Health. 2019:e1–8. https://doi.org/10.2105/AJPH.2018.304727
Millett GA, Peterson JL, Flores SA, Hart TA, 4th Jeffries WL, Wilson PA, et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. Lancet. 2012;380(9839):341–8.
Sullivan PS, Rosenberg ES, Sanchez TH, Kelley CF, Luisi N, Cooper HL, et al. Explaining racial disparities in HIV incidence in black and white men who have sex with men in Atlanta, GA: a prospective observational cohort study. Ann Epidemiol. 2015;25(6):445–54.
Bauermeister JA, Connochie D, Eaton L, Demers M, Stephenson R. Geospatial indicators of space and place: a review of multilevel studies of HIV prevention and care outcomes among young men who have sex with men in the United States. J Sex Res. 2017;54(4–5):446–64.
Tieu H-V, Koblin BA, Latkin C, et al. Neighborhood and network characteristics and the HIV care continuum among gay, bisexual, and other men who have sex with men. J Urban Health. 2018. https://doi.org/10.1007/s11524-018-0266-2.
Katz I, Jha AK. HIV in the United States: getting to zero transmissions by 2030. JAMA. 2019;321(12):1153–4.
Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. N Engl J Med. 2010;363(27):2587–99.
Cohen MS, McCauley M, Gamble TR. HIV treatment as prevention and HPTN 052. Curr Opin HIV AIDS. 2012;7(2):99–105.
Myers JE, Braunstein SL, Xia Q, et al. Redefining prevention and care: a status-neutral approach to HIV. Open Forum Infect Dis. 2018;5(6). https://doi.org/10.1093/ofid/ofy097.
Fallon SA, Park JN, Ogbue CP, Flynn C, German D. Awareness and acceptability of pre-exposure HIV proylaxis among men wo have sex with men in Baltimore. AIDS Behav. 2017;21(5):1268–77.
Eaton LA, Driffin DD, Bauermeister J, Smith H, Conway-Washington C. Minimal awareness and stalled uptake of pre-exposure prophylaxis (PrEP) among at risk, HIV-negative, black men who have sex with men. AIDS Patient Care STDs. 2015;29(8):423–9.
Arrington-Sanders R, Fields E, Greenberg L, Henry-Reid L, Stines Pehoua S, Korelitz J, … Boyer CB. Does venue type matter for HIV-related risk behavior in urban adolescent and young adult men who have sex with men? Youth Soc. 2017:51(8);1081–1103. https://doi.org/10.1177/0044118X17723655.
Ezell JM, Ferreira MJ, Duncan DT, Schneider JA. The social and sexual networks of black transgender women and black men who have sex with men: results from a representative sample. Transgend Health. 2018;3(1):201–9.
Finlayson T, Cha S, Xia M, et al. Changes in HIV preexposure prophylaxis awareness and use among men who have sex with men — 20 urban areas, 2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68(27):597. https://doi.org/10.15585/mmwr.mm6827a1.
Reisner SL, Jadwin-Cakmak L, White Hughto JM, Martinez M, Salomon L, Harper GW. Characterizing the HIV prevention and care continua in a sample of transgender youth in the U.S. AIDS Behav. 2017;21(12):3312–27.
Singh S, Mitsch A, Wu B. HIV care outcomes among men who have sex with men with diagnosed HIV infection — United States, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:69–974.
Dulin AJ, Dale SK, Earnshaw VA, et al. Resilience and HIV: a review of the definition and study of resilience. AIDS Care. 2018;30(sup5):S6–S17.
Ransome Y, Thurber KA, Swen M, Crawford ND, German D, Dean LT. Social capital and HIV/AIDS in the United States: knowledge, gaps, and future directions. SSM-Population Health. 2018;5:73–85.
Herrick AL, Stall R, Goldhammer H, Egan JE, Mayer KH. Resilience as a research framework and as a cornerstone of prevention research for gay and bisexual men: theory and evidence. AIDS Behav. 2014;18(1):1–9.
Buttram ME. The social environmental elements of resilience among vulnerable African American/Black men who have sex with men. J Hum Behav Soc Environ. 2015;25(8):923–33.
Kunzweiler CP, Bailey RC, Mehta SD, et al. Factors associated with viral suppression among HIV-positive Kenyan gay and bisexual men who have sex with men. AIDS Care. 2018;30(sup5):S76–88.
McNair OS, Gipson JA, Denson D, Thompson DV, Sutton MY, Hickson DA. The associations of resilience and HIV risk behaviors among black gay, bisexual, other men who have sex with men (MSM) in the deep south: the MARI study. AIDS Behav. 2018;22(5):1679–87.
Meanley S, Tingler R, Chittamuru D, Bauermeister JA. Applying resilience theory models to contextualize economic-dependent partnerships as a risk factor for HIV among young men who have sex with men. AIDS Care. 2018;30(sup4):42–50.
Storholm ED, Huang W, Siconolfi DE, et al. Sources of resilience as mediators of the effect of minority stress on stimulant use and sexual risk behavior among young black men who have sex with men. AIDS Behav. 2019;23:3384–3395. https://doi.org/10.1007/s10461-019-02572-y.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15(4):351–77.
Ransome Y, Zarwell M, Robinson WT. Participation in community groups increases the likelihood of PrEP awareness: New Orleans NHBS-MSM Cycle, 2014. PLoS One. 2019;14(3):e0213022.
Zarwell M, Robinson WT. Development of a social capital scale for constructed families of gay, bisexual, and other men who have sex with men. PLoS One. 2018;13(12):e0208781.
Buttram ME. The social environmental context of resilience among substance-using African American/Black men who have sex with men. J Homosex. 67;6:816–832. https://doi.org/10.1080/00918369.2018.1557952.
Graham SM, Micheni M, Secor A, et al. HIV care engagement and ART adherence among Kenyan gay, bisexual, and other men who have sex with men: a multi-level model informed by qualitative research. AIDS Care. 2018;30(sup5):S97–S105.
O’Leary A, Jemmott JB, Stevens R, Rutledge SE, Icard LD. Optimism and education buffer the effects of syndemic conditions on HIV status among African American men who have sex with men. AIDS Behav. 2014;18(11):2080–8.
Kubicek K, McNeeley M, Holloway IW, Weiss G, Kipke MD. “It’s like our own little world”: resilience as a factor in participating in the ballroom community subculture. AIDS Behav. 2013;17(4):1524–39.
Behler RL, Cornwell BT, Schneider JA. Patterns of social affiliations and healthcare engagement among young, black, men who have sex with men. AIDS Behav. 2018;22:806–818. https://doi.org/10.1007/s10461-016-1668-3.
Hightow-Weidman L, LeGrand S, Choi SK, Egger J, Hurt CB, Muessig KE. Exploring the HIV continuum of care among young black MSM. PLoS One. 2017;12(6):e0179688.
Schneider JA, Kozloski M, Michaels S, Skaathun B, Voisin D, Lancki N, et al. Criminal justice involvement history is associated with better HIV care continuum metrics among a population-based sample of young black MSM. AIDS. 2017;31(1):159–65.
Morgan E, Skaathun B, Michaels S, Young L, Khanna A, Friedman SR, et al. Marijuana use as a sex-drug is associated with HIV risk among black MSM and their network. AIDS Behav. 2016;20(3):600–7.
Eaton LA, Driffin DD, Kegler C, Smith H, Conway-Washington C, White D, et al. The role of stigma and medical mistrust in the routine health care engagement of black men who have sex with men. Am J Public Health. 2015;105(2):e75–82.
Reback CJ, Rünger D, Fletcher JB. Drug use is associated with delayed advancement along the HIV care continuum among transgender women of color. AIDS Behav. 2019. https://doi.org/10.1007/s10461-019-02555-z.
Jin H, Restar A, Biello K, Kuhns L, Reisner S, Garofalo R, et al. Burden of HIV among young transgender women: factors associated with HIV infection and HIV treatment engagement. AIDS Care. 2019;31(1):125–30.
Earnshaw VA, Bogart LM, Dovidio JF, Williams DR. Stigma and racial/ethnic HIV disparities: moving toward resilience. Am Psychol. 2013;68(4):225–36.
Gahagan J, Colpitts E. Understanding and measuring LGBTQ pathways to health: a scoping review of strengths-based health promotion approaches in LGBTQ health research. J Homosex. 2017;64(1):95–121.
Duncan TD, Hickson AD, Goedel CW, et al. The social context of HIV prevention and care among black men who have sex with men in three U.S. Cities: the neighborhoods and networks (N2) cohort study. Int J Environ Res Public Health. 2019;16:1922.
Howard Brown Health Center. Available at: https://howardbrown.org/. Accessed 28 Aug 2019.
Schneider J, Cornwell B, Jonas A, et al. Network dynamics of HIV risk and prevention in a population-based cohort of young Black men who have sex with men. Netw Sci. 2017:1–29. https://doi.org/10.1017/nws.2016.27.
Dehlin JM, Issema R, Eavou R, et al. The motivational PrEP cascade guides interpretation of early PrEP linkage to care for young black men who have sex with men: the case of Chicago’s PrEPLine. AIDS Educ Prev. 2019;31(6):491–504. https://doi.org/10.1521/aeap.2019.31.6.491.
Schneider J, Michaels S, Bouris A. Family network proportion and HIV risk among black men who have sex with men. J Acquir Immune Defic Syndr. 2012;61(5):627–35.
Phillips G, Raman A, Felt D, Han Y, Mustanski B. Factors associated with PrEP support and disclosure among YMSM and transgender individuals assigned male at birth in Chicago. AIDS Behav. 2019;23:2749–2760. https://doi.org/10.1007/s10461-019-02561-1.
Cook CL, Staras SA, Zhou Z, Chichetto N, Cook RL. Disclosure of HIV serostatus and condomless sex among men living with HIV/AIDS in Florida. PLoS One. 2018;13(12):e0207838.
Serovich JM, Laschober TC, Brown MJ, Kimberly JA. Evaluation of HIV disclosure behavior following a randomized controlled disclosure intervention for men who have sex with men living with HIV. Arch Sex Behav. 2018;47(7):2051–9.
Cao W, Wong HM, Chang C, Agudile EP, Ekström AM. Behavioral interventions promoting HIV serostatus disclosure to sex partners among HIV-positive men who have sex with men: a systematic review. Int J Public Health. 2019;64(7):985–98.
Eaton LA, Earnshaw VA, Maksut JL, Thorson KR, Watson RJ, Bauermeister JA. Experiences of stigma and health care engagement among Black MSM newly diagnosed with HIV/STI. J Behav Med. 2018;41(4):458–66.
Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston, Massachusetts. AIDS Care. 2017;29(11):1351–8.
Acknowledgments
The Neighborhoods and Networks (N2) Cohort Study is funded through a grant from the National Institute on Mental Health (Grant Number: R01MH112406) and a cooperative agreement with the Centers for Disease Control and Prevention under the Minority HIV/AIDS Research Initiative (Grant Number: U01PS005122). Mr. Goedel is supported by the Brown University Clinical and Community-Based HIV/AIDS Research Training Fellowship, funded by the National Institute of Mental Health (Grant Number: R25MH083620). We thank the participants for engaging in this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, YT., Duncan, D.T., Issema, R. et al. Social-Environmental Resilience, PrEP Uptake, and Viral Suppression among Young Black Men Who Have Sex with Men and Young Black Transgender Women: the Neighborhoods and Networks (N2) Study in Chicago. J Urban Health 97, 728–738 (2020). https://doi.org/10.1007/s11524-020-00425-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-020-00425-x