Abstract
This paper assessed characteristics associated with awareness of and willingness to take pre-exposure prophylaxis (PrEP) among Baltimore men who have sex with men (MSM). We used data from BESURE-MSM3, a venue-based cross-sectional HIV surveillance study conducted among MSM in 2011. Multivariate regression was used to identify characteristics associated with PrEP knowledge and acceptability among 399 participants. Eleven percent had heard of PrEP, 48% would be willing to use PrEP, and none had previously used it. In multivariable analysis, black race and perceived discrimination against those with HIV were significantly associated with decreased awareness, and those who perceived higher HIV discrimination reported higher acceptability of PrEP. Our findings indicate a need for further education about the potential utility of PrEP in addition to other prevention methods among MSM. HIV prevention efforts should address the link between discrimination and potential PrEP use, especially among men of color.
Resumen
Evaluamos las características asociadas con el conocimiento y la voluntad de hombres que tienen sexo con hombres (HSH) en Baltimore de tomar profilaxis de pre-exposición al VIH (PrEP, por sus siglas en inglés). Utilizamos datos de BESURE-MSM3, un estudio transversal de vigilancia del VIH realizado entre HSH en el año 2011. Se utilizó el método de regresión multivariante para identificar las características asociadas con el conocimiento y aceptabilidad de PrEP entre 399 participantes. El once por ciento habían previamente escuchado de PrEP, el 48% serian dispuestos a utilizar PrEP, y ningún participante había previamente utilizado PrEP. En el análisis multivariante, ser de la raza negra y la percepción de discriminación contra las personas que viven con el VIH fueron asociadas significativamente con la disminución del conocimiento sobre PrEP, aunque los que indicaron más alta percepción de discriminación asociada con el VIH reportaron más alta aceptabilidad de PrEP. Nuestros resultados indican la necesidad de una mayor educación sobre la utilidad potencial de PrEP, además de otros métodos de prevención del VIH entre HSH. Los esfuerzos de prevención del VIH necesitan abordar el vínculo entre la discriminación y el uso potencial de PrEP, especialmente entre HSH negros.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
By the end of 2011 an estimated 1.2 million people over 13 years of age were living with Human Immunodeficiency Virus (HIV) in the United States [1]. While the estimated annual number of new HIV diagnoses has remained stable for the last few years [2], some groups are disproportionately affected [3]. National incident HIV infections attributed to male to male sexual contact increased 12% from 2008 to 2012 (27,315 to 30,695 new cases respectively) [4, 5], and although men who have sex with men (MSM) account for only 4% of the male population, they represent 78% of new HIV infections among males [4]. Maryland ranks third in the estimated rate of HIV diagnoses in the United States [5], and rates in Baltimore city are consistently the highest in the state [6]. HIV cases attributed to male-to-male sexual contact in Baltimore have increased 10% since 1985 and MSM now represent the majority of new cases [6]. With rising MSM infection rates despite availability of behavioral interventions and condoms, new prevention strategies should be explored.
One possible new prevention strategy is pre-exposure prophylaxis (PrEP), an HIV prevention method that involves HIV-negative individuals taking antiretroviral therapy (ART) to reduce the risk of HIV infection if exposed [7]. It contains tenofovir and emitricitabine (TDF–FTC) and can be taken orally (brand name Truvada). PrEP has been proven to be safe and effective in MSM [8, 9]. The iPrEx study, a multi-site randomized control efficacy trial among MSM and transgender women published in 2011, demonstrated 44% efficacy of daily oral TDF/FTC [8]. Expanded case–control studies among iPrEx participants suggested up to a 90% reduction in HIV acquisition with improved drug adherence [9]. Both the IPERGAY randomized placebo trial and the PROUD open label study suggest that PrEP reduces HIV risk among MSM by 86% [10]. Following these results, the Centers for Disease Control and Prevention (CDC) published an interim guidance report in 2011 regarding the use of oral PrEP [11], and in 2012 the Food and Drug Administration (FDA) recommended TDF–FTC combination pill for preventative use among high risk populations, including MSM [12].
Although PrEP has been efficacious among MSM, its effectiveness is dependent on uptake, acceptability, and adherence [13]. Research suggests that rates of awareness, use and acceptability in MSM communities vary [14, 15]. Studies estimate awareness of PrEP range from 11 [16] to 66% [13] among sample populations [10, 15–24] and previous use among MSM is reported to be <5%, [15, 17, 18, 20–22, 24–26]. Variation in acceptability ranges from 40 [27] and 86% [28] of sample populations expressing an interest in taking PrEP [13, 16, 18, 19, 21, 25, 29–32]. However, after the publication of the iPrEx study in 2010, PrEP has become a more established option [14, 15]. Given its success, understanding the facilitators and barriers to PrEP uptake is instrumental in creating new HIV prevention programs. Increased likelihood of hearing of PrEP has been associated with race [23], recent HIV test [22, 23, 32], higher education [22, 23], gay identity [10, 22, 23], and condomless anal intercourse (CAI) [18]. Feeling positively about using PrEP to prevent HIV is associated with age [15, 18, 21, 25], education [18, 19, 27, 32], income [19, 21], CAI [17, 18, 25, 27, 32, 33], and having multiple sex partners [15, 17, 27]. A key barrier to PrEP uptake is the stigma surrounding HIV that is prominent in many communities. Studies suggest willingness to use PrEP is influenced by the perception that taking the medication would result in increased discrimination [31, 34, 35].
This is the first study to examine correlates of PrEP awareness and willingness to use PrEP among HIV-negative MSM in Baltimore. The current study examines demographic and behavioral characteristics associated with awareness and consideration of daily oral PrEP for HIV prevention among MSM recruited through the Baltimore site of the National HIV Behavioral Surveillance System (NHBS), a multisite study sponsored by the Centers for Disease Control and Prevention (CDC) in order to provide baseline data and guidance for PrEP initiatives in Baltimore.
Methods
Sampling Design and Recruitment
CDC’s NHBS is a cross-sectional survey implemented every 3 years among venue-recruited MSM to assess HIV prevalence and behavioral risk. The Baltimore arm of the NHBS, BESURE, is implemented by the Johns Hopkins Bloomberg School of Public Health and the Maryland Department of Health and Mental Hygiene. BESURE-MSM3 used venue-based sampling to enroll MSM between June and December in 2011. Study methods have been described previously [36–40].
Eligible participants were males age 18 or older who were residents of the Baltimore–Towson metropolitan area and reported oral or anal sex with at least one male partner in the past year. Of the 1487 attendees approached by interviewers at 31 BESURE–MSM3 events, 592 were screened for eligibility and a total of 498 (33%) were eligible and agreed to participate. For this analysis we restricted our sample to self-reported HIV negative men and excluded 97 (19%) respondents with a previous positive or indeterminate HIV test resulting in a sample size of 399 participants. Informed consent was obtained from all individual participants included in the study.
Measures
The questionnaire assessed socio-demographic characteristics, HIV-related risk behaviors over the lifetime and in the past year, and use of prevention services.
Outcome variables of interest were knowledge of antiretroviral prophylaxis to prevent HIV (PrEP) and willingness to take antiretroviral prophylaxis (PrEP) to prevent HIV. Respondents were asked to respond “yes” or “no” to two questions: (1) “Before today, have you ever heard of people who do not have HIV taking anti-HIV medicines, to keep from getting HIV?” and two) “Would you be willing to take anti-HIV medicines every day to lower your chances of getting HIV?”.
Demographic covariates were informed by PrEP literature and included age, race, education, employment status, household income, sexual identity, and perceived discrimination against people with HIV. Age was operationalized reflecting standard categories for local HIV surveillance. Race/ethnicity categories were non-Hispanic white, non-Hispanic black, Hispanic, Native American, Pacific Islander, Asian-American, or mixed race (i.e., participants who reported being more than one racial/ethnic category). Race/ethnicity was consolidated into three categories (non-Hispanic white, non-Hispanic black, other) due to low prevalence of Native American, Pacific Islander, Asian American, and mixed race participants. Education was recorded as current level attained at the time of the survey and categorized into high school diploma/GED or less and some college or more. Employment status was categorized as working full time, working part time and student, unemployed and other. Annual household income from all sources before taxes was originally collected in 12 categories and then collapsed into $0.00–9999, $10,000–19,999 and $20,000+ based on sample distribution. Health insurance coverage was categorized as public, private or no insurance. HIV stigma was assessed with the question “Most people in Baltimore would discriminate against someone with HIV” and response categories of “strongly agree”, “agree”, “neither agree nor disagree”, “disagree” and “strongly disagree”. A binary discrimination variable was created and responses of “strongly agree” and “agree” were coded as “perceived discrimination”.
Participants answered questions about lifetime and past year sexual and drug-related behaviors. Recent sexual behaviors included CAI with a casual partner, any concurrency, diagnosis with an STD, and number of anal sex partners. CAI was defined as not using a condom during one or more sex acts with a casual partner in the past year. Concurrency was defined as either sexual partner having a sexual relationship with someone else. Participants answered the questions (1) “As far as you know, during the time that you were having a sexual relationship with this partner did he have sex with other people?” with response options of “definitely did not”, “probably did not”, “probably did”, “definitely did” and (2) “During the time that you were having a sexual relationship with this partner, did you have sex with other people?” with “yes” or “no”. Answers were combined into a binary variable of “no concurrency” and “any concurrency”. Self-reported STD diagnosis was categorized as any STD positive diagnosis by a clinician in the last 12 months and was coded as “no STD diagnosis” and “STD diagnosis”.
Number of recent sexual partners was ascertained by the questions “In the past 12 months, with how many different men have you had oral or anal sex?” and “Of the men that you’ve had oral or anal sex with in the past 12 months, with how many did you have anal sex with?” Number of anal sex partners was collapsed into four categories to reflect sample distribution.
Drug-related behaviors included injection and non-injection drug use in the past 12 months. Use of injected drugs in the past 12 months was assessed with the question “When was the last time you injected any drug?” and was analyzed as a dichotomous variable of “injected in the last 12 months” and “did not inject in the last 12 months”. Participants were asked about their use of non-injection drugs in the past 12 months including marijuana, crystal meth, crack cocaine, powdered cocaine, downers (such as Valium, Ativan or Xanax), pain killers (such as Oxycontin, Vicodin, Percocet), hallucinogens (such as LSD or mushrooms) ecstasy, heroin that is smoked or snorted, poppers (amyl nitrate) GHB, and ketamine. For this analysis we examined heroin, crack, or cocaine in the past 12 months based on sample substance use prevalence.
Recent access to health prevention services was attained by asking participants about HIV testing practices, participation in one-on-one or group HIV prevention sessions, and availability of free condoms. Respondents indicated ever testing for HIV (coded as a binary variable) and date of most recent test. Using the most recent test date, a new binary variable was created for an HIV test received within the last 12 months. A new binary variable was created to represent access to any prevention services. Participants who reported participation in an organized group session or one-on-one conversation with an outreach worker about ways to prevent HIV, or had received free condoms from a health worker in the past 12 months were coded as receiving HIV prevention services.
Statistical Analysis
We used logistic regression modeling to identify variables associated with awareness of and willingness to take PrEP. For these analyses we report odds ratio and corresponding 95% confidence interval (95% CI). Multivariate models include variables that were statistically significant (P < 0.1) in the bivariate analyses or were a priori considered to be potentially associated with the outcome based on the literature. All statistical analyses were conducted using STATA, version 13.0 and data are presented and analyzed without weights.
Results
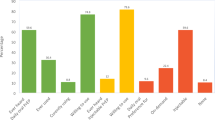
Median participant age was 30 years (range, 18–71 years), 84% were of a minority race, and 44% reported more postsecondary education (Table 1). Fifty-three percent of respondents reported full or part time employment, 29% were unemployed and more than half reported annual household income of less than $20,000 (57%). Sixty percent identified as being gay. About a third indicated they had no health coverage and 40% reported public health insurance. Most reported CAI with a casual partner (68%), and ever getting an HIV test (89%). A majority reported never injecting drugs (68%) and no recent sexually transmitted disease diagnosis (90%). Mean number of anal sexual partners in the past 12 months was 2.9 (range, 0–60 partners) and 72% reported partner concurrency in the past 12 months. Sixty-seven percent of participants perceived discrimination against people with HIV in Baltimore and only 10% reported accessing HIV preventative services. Eleven percent of the respondents had heard of people using PrEP to prevent HIV, and 48% said they would be willing to take PrEP every day to prevent HIV. None had taken PrEP in the prior 12 months.
In bivariate analyses (Table 2), black race (OR 0.24, CI 0.12–0.49) and perceiving discrimination against people with HIV (OR 0.2, CI 0.25–0.90) were associated with decreased awareness of PrEP. At least some college education (OR 3.07, CI 1.57–5.99) and an annual household income of at least $20,000 (OR 2.56 CI 1.15–5.67) were significantly associated with increased awareness of PrEP. Lower educational attainment (OR 0.63 CI 0.42–0.94) was associated with decreased PrEP acceptability. Perceiving discrimination against people with HIV (OR 1.62, CI 1.08–2.43) and having a positive HIV test result (OR 1.59. CI 1.01–2.59) were significantly associated with an increased willingness to use PrEP. Awareness of PrEP did not significantly vary based on age, employment, insurance coverage or sexual identity and acceptability of PrEP was not significantly associated with age, race or household income.
In multivariable analysis (Table 3), black race (AOR 0.48, CI 0.15–0.74) and perceived HIV discrimination (AOR 0.47, CI 0.06–0.81) were associated with decreased awareness of PrEP. After adjusting for other covariates, perceived discrimination was also significantly associated with increased willingness to take PrEP to prevent from getting HIV (AOR 1.5 CI 1.01–2.51) (Table 4).
Discussion
The purpose of this analysis was to describe differences in demographic and behavioral characteristics of Baltimore MSM by their awareness and acceptability of taking daily PrEP. Eleven percent of Baltimore MSM in 2011 reported knowledge of PrEP. While similar results have been reported [16, 17], our results are lower than those reported in other post-iPrEx studies with MSM during the same time period. Rucinski and colleagues found awareness of PrEP to be 38% among MSM in New York city in 2011 [24] and Saberi and colleagues reported 62% of their 2012 San Francisco sample had heard of PrEP [33]. Willingness to take PrEP in our sample was 48%, less than the 55% Golub et al. reported in New York city in 2012 [29] and the 80% Brooks et al. reported in Los Angeles in 2011 [31]. With a majority of participants reporting CAI and partner concurrency in the last 12 months, PrEP is an important biomedical option for MSM in Baltimore. However, the low proportion of respondents aware of PrEP suggests information about PrEP was likely not reaching MSM in Baltimore. Fifty-eight percent of participants (n = 230) reported HIV testing within 12 months, indicating contact with some form of HIV-related counseling. Conversely, 11% indicated awareness of people taking PrEP, suggesting providers in 2011 were missing opportunities for targeted HIV prevention counseling during these clinical interactions.
After adjusting for demographic covariates, being non-Hispanic black was associated with decreased awareness of PrEP, and individuals who perceived discrimination against someone with HIV were less likely to hear of PrEP, but more likely to be willing to take it. Three-quarters of our sample was African-American, and it has been suggested that MSM of minority race endure increased homonegativity [41] and homophobia within their communities [42–44] as well as higher rates of perceived stigma and discrimination around HIV [45–49] HIV-related stigma can negatively impact overall well-being [50] prompting depression, low self-esteem, and lack of social support [51–53].
Perception of HIV intolerance may also be a barrier for MSM, particularly of minority race, to accessing HIV prevention services [54]. Perceived stigma may limit risk prevention education opportunities, and therefore knowledge of PrEP, in communities that may be the most likely to be interested. Fear of rejection due to sexual promiscuity or identity, may discourage accessing social networks with valuable knowledge of risk reduction techniques. HIV literacy and social marketing campaigns that accurately report facts about the risks and benefits of PrEP may be a useful tool for targeting populations uncomfortable with seeking health information from peers.
HIV-related stigma may also influence attitudes about PrEP use. Research cites stigma as a possible barrier for taking PrEP [10] and disclosing its use to others outside one’s social network [55–59], including a healthcare provider. Given public health’s history of mistreating vulnerable racial/ethnic minorities and a pattern of inferior care, it is understandable that patients of minority race may not trust the health care system [60]. Prior research indicates they perceive more discrimination in medical settings, experience more medical mistrust, and deal with poorer provider communication compared with European Americans [61, 62]. Negative feelings about the healthcare system may lead to delayed care or decreased medical adherence and follow up [63]. This is especially problematic because minority MSM would benefit most from HIV-preventative treatment.
Health care providers represent a vital link to PrEP education for MSM populations. Two-thirds of our sample reported health coverage, and a majority had recently tested for HIV, suggesting our population of interest generally has access to providers. In 2011, the iPrEx results were new and clinicians may have been cautious prescribing PrEP [64]. Now that the method has been proven to be safe and effective, HIV providers need to identify potential candidates and initiate a PrEP dialogue. It is imperative that clinicians be cognizant of the perceived barriers to care that minority patients face. Normalizing PrEP use by encouraging honest conversations between sex partners may be beneficial. Greater emphasis should be placed on creating accessible medical systems stressing culturally sensitive messaging and long-term, trusting relationships between provider and patient. Given that PrEP effectiveness depends on awareness and acceptance, strategies to increase uptake of PrEP in Baltimore, especially among black MSM, should examine opportunities to reduce stigma and discrimination surrounding HIV.
It is important to note that providers still face structural barriers prescribing PrEP to patients. Public resources are taxed [64] and access to expensive treatment can be limited by hefty copays or gaps left by assistance programs [65] leading to access disparities. Additional costs of PrEP regimens include routine counseling, HIV/STD testing, renal function monitoring, and surveillance for adverse side effects or resistant viral strains [65]. Even when cost is not problematic, providers face regulatory obstacles to providing PrEP. Many PrEP delivery programs require face-to face consultation or documented HIV-negative test results, and may discontinue prescriptions without follow-up visits [66, 67]. These guidelines are necessary to ensure proper allocation, use and adherence to medication and work effectively for typical patients. However, strict regulations may leave at risk patients without viable options. Clinicians are legally prohibited from providing therapy to ineligible populations such as partners of patients without primary care physicians and those inconsistently retained in care. Further research is needed to fully understand and target barriers to HIV prevention. This will better inform economic and social policies that will ensure all at-risk patients have fair access to medical assistance.
PrEP program planning should be a multi-stakeholder process, drawing on MSM networks to promote informed decision making about PrEP and ensure messages are culturally sensitive with the aim of reducing perceived HIV stigma and discrimination. Social marketing, community engagement and policy analysis may increase PrEP acceptability, reduce stigmatization of use, and expand therapy [68].
These findings are subject to several limitations. Individuals included in the sample are those who agreed to take the BESURE-MSM3 survey and those who chose not to participate may be systematically different. The results also may not be generalizable to MSM who do not frequent recruitment venues, or who live in other US states or cities. Demographic and HIV risk behavior data were self-reported, which may have introduced some validity concerns [69]. Recall or social desirability bias may result in misreported stigmatized behaviors and PrEP acceptability may be overestimated. Due to perceived stigma or concerns about study eligibility, participants who had been previously diagnosed with HIV infection may not have accurately reported their status, resulting in their inclusion in the analysis. This survey measured PrEP willingness by asking people to respond to hypothetical scenarios, which may not correlate well with actual intentions. It is important to note that participants were asked about their willingness to use PrEP after being provided with only a brief description of the method that did not include potential side effects, costs, or efficacy, which may further impact willingness. Furthermore, perceived stigma was measured using a single question as opposed to a validated instrument, which may limit the ability to compare results in the future. Data were not weighted to account for variations in venue attendance or likelihood of recruitment to participate in the survey.
Despite limitations, this study has important implications for HIV prevention programs and PrEP initiatives in Baltimore. Our results suggest disparate access to PrEP information and a general ambivalence regarding PrEP usage among Baltimore MSM in 2011. Race/ethnicity and perceived stigma and discrimination were shown to have a significant impact on PrEP awareness and acceptability. Facilitating sustained relationships emphasizing cultural understanding and trust between MSM and providers may help introduce and normalize PrEP use in high-risk communities. Further research and policy reform is needed to better understand and target barriers to PrEP delivery among Baltimore MSM. PrEP has the potential to reduce HIV incidence in Baltimore City in the context of high background prevalence, sub-optimal prior year HIV testing and sexual risk behaviors [70–72]. Enhancing awareness of and willingness to use PrEP among those most at risk for HIV transmission will be crucial for effective coverage.
References
Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas—2012. HIV surveillance supplemental report 2014. 2014; 19(3). http://www.cdc.gov/hiv/pdf/surveillance_Report_vol_19_no_3.pdf
Centers for Disease Control and Prevention. HIV surveillance report, 2012. 2014. http://www.cdc.gov/hiv/pdf/statistics_2012_HIV_Surveillance_Report_vol_24.pdf
Purcell DW, Johnson CH, Lansky A, et al. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS J. 2012;6:98–107.
Centers for Disease Control and Prevention. Estimated HIV incidence in the United States, 2007– 2010. HIV Surveillance Supplemental Report 2012. 2012; 17(4). http://www.cdc.gov/hiv/pdf/statistics_hssr_vol_17_no_4.pdf.
Centers for Disease Control and Prevention. Diagnoses of HIV infection in the United States and dependent areas, 2012. HIV Surveillance Report. 2012; 24. Available at: http://www.cdc.gov/hiv/pdf/statistics_2012_HIV_Surveillance_Report_vol_24.pdf.
Maryland Department of Health and Mental Hygiene. Maryland annual HIV epidemiological profile 2012. Center for HIV Surveillance, Epidemiology and Evaluation. 2015. http://phpa.dhmh.maryland.gov/OIDEOR/CHSE/SiteAssets/SitePages/statistics/Maryland%20HIV%20AIDS%20Epidemiological%20Profile2.pdf
Kelesidis T, Landovitz RJ. Preexposure prophylaxis for HIV prevention. Curr HIV/AIDS Rep. 2002;8(2):94–103.
Grant RM, Lama JR, Anderson PL, et al. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. NEJM. 2010;363(27):2587–99.
Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):1–5.
Centers for Disease Control and Prevention. CDC statement on IPERGAY trial of Pre- exposure prophylaxis (PrEP) for HIV prevention among men who have sex with men, NCHHSTP Newsroom, 2015. http://www.cdc.gov/nchhstp/newsroom/2015/IPERGAY-2015-Media-Statement.html.
Centers for Disease Control and Prevention. Interim guidance: preexposure prophylaxis for the prevention of HIV infection in men who have sex with men. MMWR Morb Mortal Wkly Rep. 2011;60(3):65–8.
Food and Drug Administration. FDA approves first drug for reducing the risk of sexually acquired HIV infection. FDA News Press Release, July 16, 2012.
Yang D, Chariyalertsak C, Wongthanee A, et al. Acceptability of pre-exposure prophylaxis among men who have sex with men and transgender women in northern thailand. PLoS ONE. 2013;8(10):e76650.
Al-Tayyib AA, Thrun MW, Haukoos JS, Walls NE. Knowledge of pre-exposure prophylaxis (PrEP) for HIV prevention among men who have sex with men in denver, colorado. AIDS Behav. 2014;18(3):340–7.
Krakower DS, Mimiaga MJ, Rosenberger JG, et al. Limited awareness and low immediate uptake of pre-exposure prophylaxis among men who have sex with men using an internet social networking site. PLoS ONE. 2012;7(3):e33119.
Zhou F, Gao L, Li S, et al. Willingness to accept HIV pre-exposure prophylaxis among chinese men who have sex with men. PLoS ONE. 2012;7(3):e32329.
Leonardi M, Lee E, Tan DH. Awareness of, usage of and willingness to use HIV-pre-exposure prophylaxis among men in downtown Toronto, Canada. Int J STD AIDS. 2011;22(12):738–41.
Liu A, Kittredge PV, Vittinghoff E, et al. Limited knowledge and use of HIV post- and pre-exposure prophylaxis among gay and bisexual men. J AIDS. 2008;47(2):241–7.
Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J AIDS. 2009;50(1):77–83.
Voetsch AC, Heffelfinger JD, Begley EB, Jafa-Bhushan K, Sullivan PS. Knowledge and use of preexposure and postexposure prophylaxis among attendees of minority gay pride events, 2005 through 2006. J AIDS. 2007;46(3):378–80.
Barash EA, Golden M. Awareness and use of HIV pre-exposure prophylaxis among attendees of a seattle gay pride event and sexually transmitted disease clinic. AIDS Patient Care STDS. 2011;24(11):689–91.
Kellerman SE, Hutchinson AB, Begley EB, Boyett BC, Clark HA, Sullivan P. Knowledge and use of HIV pre-exposure prophylaxis among attendees of minority gay pride events, 2004. J AIDS. 2006;43(3):376–7.
Mehta SA, Silvera R, Bernstein K, Holzman RS, Aberg JA, Daskalakis DC. Awareness of post-exposure HIV prophylaxis in high-risk men who have sex with men in New York city. Sex Transm Infect. 2011;87(4):344–8.
Rucinski KB, Mensah NP, Sepkowitz KA, Cutler BH, Sweeney MM, Myers JE. Knowledge and use of pre-exposure prophylaxis among an online sample of young men who have sex with men in New York city. AIDS Behav. 2013;17(6):2180–4.
Aghaizu A, Mercey D, Copas A, Johnson AM, Hart G, Nardone A. Who would use PrEP? Factors associated with intention to use among MSM in London: a community survey. Sex Transm Infect. 2013;89(3):207–2011.
Mansergh G, Koblin BA, Colfax GN, McKirnan DJ, Flores SA, Hudson SM. Preefficacy use and sharing of antiretroviral medications to prevent sexually-transmitted HIV infection among US men who have sex with men. J AIDS. 2010;55(2):e14–6.
Lorente N, Fugon L, Carrieri MP, et al. Acceptability of an “on-demand” pre-exposure HIV prophylaxis trial among men who have sex with men living in france. AIDS Care. 2012;24(4):468–77.
Schneider J, Kumar R, Dandona R, et al. Social network and risk-taking behavior most associated with rapid HIV testing, circumcision, and preexposure prophylaxis acceptability among high-risk indian men. AIDS Patient Care STDS. 2012;26(10):631–40.
Golub SA, Gamarel KE, Rendina HJ, Surace A, Lelutiu-Weinberger CL. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in new york city. AIDS Patient Care STDS. 2013;27(4):248–54.
Golub SA, Kowalczyk W, Weinberger CL, Parsons JT. Pre-exposure Prophylaxis and predicted condom use among high-risk men who have sex with men. J AIDS. 2010;54(5):548–55.
Brooks RA, Landovitz RJ, Kaplan RL, Lieber E, Lee SJ, Barkley TW. Sexual risk behaviors and acceptability of HIV pre-exposure prophylaxis among HIV-negative gay and bisexual men in serodiscordant relationships: a mixed methods study. AIDS Patient Care STDS. 2012;26(2):87–94.
Young I, Li J, McDaid L. Awareness and willingness to use HIV pre-exposure prophylaxis amongst gay and bisexual men in scotland: implications for biomedical HIV prevention. PLoS ONE. 2013;8(5):e64038.
Saberi P, Gamarel KE, Neilands TB, et al. Ambiguity, ambivalence, and apprehensions of taking HIV-1 pre-exposure prophylaxis among male couples in san francisco: A mixed methods study. PLoS One. 2012;7(11):e50061.
Galea JT, Kinsler JJ, Salazar X, et al. Acceptability of pre-exposure prophylaxis as an HIV prevention strategy: barriers and facilitators to pre-exposure prophylaxis uptake among at-risk peruvian populations. Int J STD AIDS. 2011;22(5):256–62.
Jackson T, Huang A, Gao X, Zhong X, Zhang Y. Cognitive. Psychosocial, and Sociodemographic Predictors of Willingness to use HIV pre-exposure prophylaxis among Chinese men who have sex with men, AIDS Behav. 2012;16(7):1853–61.
Ferreira LO, de Oliveira ES, Raymond HF, Chen SY, McFarland W. Use of time-location sampling for systematic behavioral surveillance of truck drivers in Brazil. AIDS Behav. 2008;12(4 Suppl):S32–8.
MacKellar DA, Gallagher KM, Finlayson T, Sanchez T, Lansky A, Sullivan P. Surveillance of HIV risk and prevention behaviors of men who have sex with men: a national application of venue-based, time-space sampling. Public Health Rep. 2007;122(Suppl 1):39–47.
Raymond HF, McFarland W. Racial mixing and HIV risk among men who have sex with men. AIDS Behav. 2009;13(4):630–7.
Centers for Disease Control and Prevention. Prevalence and awareness of HIV infection among men who have sex with men—21 cities, United States, 2008. MMWR Morb Mortal Wkly Rep. 2010;59(37):1201–7.
German D, Sifakis F, Maulsby C, et al. Persistently high prevalence and unrecognized HIV infection among men who have sex with men in Baltimore: the BESURE Study. J Acquir Immune Defic Syndr. 2011;57(1):77–87.
Shoptaw S, Weiss RE, Munjas B, et al. Homonegativity, substance use, sexual risk behaviors, and HIV status in poor and ethnic men who have sex with men in Los Angeles. J Urban Health. 2009;86(Suppl. 1):77–92.
Icard L. Gay black men and conflicting social identities: sexual orientation versus racial identity. J Soc Work Hum Sex. 1986;4:83–93.
Operario D, Smith CD, Kegeles S. Social and psychological context for HIV risk in non-gay-identified African American men who have sex with men. AIDS Educ Prev. 2008;20:347–59.
Williams JK, Wyatt GE, Resell J, Peterson J, Asuan-O’Brien A. Psychosocial issues among gay- and non-gay-identifying HIV-seropositive African American and Latino MSM. Cult Divers Ethn Minor Psychol. 2004;10:268–86.
Dodge B, Jeffries WL, Sandfort TG. Beyond the down low: sexual risk, protection, and disclosure among at-risk black men who have sex with both men and women (MSMW). Arch Sex Behav. 2008;37(5):683–96.
Miller M, Serner M, Wagner M. Drug-using men who have sex with men as bridges for HIV and other sexually transmitted infections: sexual diversity among black men who have sex with men in an inner-city community. J Urban Health. 2005;82(1):i26–34.
Radcliffe J, Doty N, Hawkins LA, Gaskins CS, Beidas R, Rudy BJ. Stigma and sexual health risk in HIV-positive African American young men who have sex with men. AIDS Patient Care STDS. 2010;24(8):493–9.
Woodyard JL, Peterson JL, Stokes JP. ‘‘Let us go into the house of the lord’’: participation in African American churches among young African American men who have sex with men. J Pastor Care. 2000;54(4):451–60.
Miller RL Jr. Legacy denied: African American gay men, AIDS, and the black church. Soc Work. 2007;52(1):51–61.
Radcliffe J, Doty N, Hawkins LA, et al. Stigma and sexual health risk in HIV-positive African American young men who have sex with men. AIDS Patient Care STDS. 2010;24(8):493–9.
Downshen N, Binns H, Garafalo R. Experiences of HIV-related stigma among young men who have sex with men. AIDS Patient Care STDS. 2009;23:371–6.
Wright K, Naar-King S, Lam P, et al. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV + youth. J Adol Health. 2007;40:96–8.
Johnson M, Carrico A, Chesney M, et al. Internalized heterosexism among HIV-positive, gay-identified men: implications for HIV prevention and care. J Consult Clin Psych. 2008;76:829–39.
Glick SN, Golden MR. Persistence of racial differences in attitudes toward homosexuality in the United States. J AIDS. 2010;55(4):516–23.
Abbas UL, Anderson RM, Mellors JW. Potential impact of antiretroviral chemoprophylaxis on HIV-1 transmission in resource-limited settings. PLoS ONE. 2007;2(9):e875.
Siegel K, Raveis V. Perceptions of access to HIV-related information, care, and services among infected minority men. Qual Health Res. 1997;7(1):9–31.
Malebranche DJ, Peterson JL, Fullilove RE, Stackhouse RW. Race and sexual identity: perceptions about medical culture and healthcare among black men who have sex with men. J Natl Med Assoc. 2004;96(1):97–107.
Halkitis PN, Parsons JT, Wolitski RJ, Remien RH. Characteristics of HIV antiretroviral treatments, access and adherence in an ethnically diverse sample of men who have sex with men. AIDS Care. 2003;15(1):89–102.
Clark JL, Long CM, Giron JM. Partner notification for sexually transmitted diseases in Peru: knowledge, attitudes, and practices in a high risk community. Sex Transm Dis. 2007;34:309–13.
Bauermesiter JA, Meanley S, Pingel E, et al. PrEP awareness and perceived barriers among single young men who have sex aith men in the United States. Cur HIV Res. 2014;11(7):520–7.
Cuevas AG, O’Brien K, Saha S. African American experiences in healthcare: “I always feel like I’m getting skipping over”. Health Psychol. 2016;35(9):987–95.
Boulware LE, Cooper LA, Ratner LE, et al. Race and trust in the health care system. Public Health Rep. 2003;118(4):358–65.
Sorkin DH, Ngo-Metzger Q, De Alba I. Racial/ethnic discrimination in health care: impact on perceived quality of care. J Gen Intern Med. 2010;25(5):390–6.
Leibowitz AA, Parker KB, Rotheram-Borus MJ. A US Policy perspective on oral preexposure prophylaxis for HIV. Am J Public Health. 2011;101:982–5.
Mayer KH, Hosek S, Cohen S, Liu A, Pickett J, Warren M, Krakower D, Grant R. Antiretroviral pre-exposure prophylaxis implementation in the United States: a work in progress. J Int AIDS Soc. 2015;18(4Suppl 3):19980.
Centers for Disease control and Prevention. Preexopsure prophylaxis for the prevention of HIV infection in the United Stated—2014: a clinical practice guideline. http://www.cdc.gov/hiv/pdf/guidelines/PrEPguidelines2014.pdf
NYS guidelines: HIV Clinical Resource. New York state guidance for the use of pre-exposure prophylaxis (PrEP) to prevent HIV transmission. 2015. http://www.hivguidelines.org/wp-content/uploads/2016/02/PrEP-Guidance_10-14-15.pdf
Underhill K, Operario D, Mayer KH. Implementation science of pre-exposure prophylaxis: preparing for public use. Curr HIV/AIDS Rep. 2010;7(4):210–9.
Lewontin RC. Sex, lies and social science. NY Rev Books. 1995;20:24–9.
Desai K, Sansom SL, Ackers ML, et al. Modeling the impact of HIV chemoprophylaxis strategies among men who have sex with men in the United States: HIV infections prevented and cost-effectiveness. Aids. 2008;22(14):1829–39.
Paltiel AD, Freedberg KA, Scott CA, et al. HIV preexposure prophylaxis in the United States: impact on lifetime infection risk, clinical outcomes, and cost effectiveness. Clin Infect Dis. 2009;48(6):806–15.
Vissers DC, Voeten HA, Nagelkerke NJ, Habbema JD, de Vlas SJ. The impact of pre-exposure prophylaxis (PrEP) on HIV epidemics in Africa and India: a simulation study. PLoS ONE. 2008;3(5):e0277.
Acknowledgements
The authors wish to acknowledge and thank the many participants in NHBS Baltimore (BESURE) as well as the many dedicated BESURE team members for their invaluable contributions over time.
Funding
This study was funded by contracts to the Johns Hopkins University from the Maryland Department of Health and Mental Hygiene and by cooperative agreements between the Maryland Department of Health and Mental Hygiene and the Centers for Disease Control and Prevention (CDC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Susan Fallon and Dr. Colin Flynn do not receive any external funding and have no conflicts of interest to report. Dr. Danielle German receives funding from Johns Hopkins CFAR, the National Institutes of Health, PCORI, and from CDC via the Maryland Department of Health and Mental Hygiene to implement National HIV Behavioral Surveillance for this study. The CFAR, NIH, and PCORI played no role in the current study. The CDC provided the study protocol and technical support for project implementation. CDC played no role in analysis, interpretation of data, report writing, or the decision to submit the report for publication.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Fallon, S.A., Park, J.N., Ogbue, C.P. et al. Awareness and Acceptability of Pre-exposure HIV Prophylaxis Among Men Who have Sex with Men in Baltimore. AIDS Behav 21, 1268–1277 (2017). https://doi.org/10.1007/s10461-016-1619-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-016-1619-z