Abstract
This study examined the association of housing status over time with unmet physical health care needs and emergency department utilization among homeless and vulnerably housed persons in Canada. Homeless and vulnerably housed individuals completed interviewer-administered surveys on housing, unmet physical health care needs, health care utilization, sociodemographic characteristics, substance use, and health conditions at baseline and annually for 4 years. Generalized logistic mixed effects regression models examined the association of residential stability with unmet physical health care needs and emergency department utilization, adjusting for potential confounders. Participants were from Vancouver (n = 387), Toronto (n = 390), and Ottawa (n = 396). Residential stability was associated with lower odds of having unmet physical health needs (adjusted odds ratio (AOR), 0.82; 95 % confidence interval (CI), 0.67, 0.98) and emergency department utilization (AOR, 0.74; 95 % CI, 0.62, 0.88) over the 4-year follow-up period, after adjusting for potential confounders. Residential stability is associated with fewer unmet physical health care needs and lower emergency department utilization among homeless and vulnerably housed individuals. These findings highlight the need to address access to stable housing as a significant determinant of health disparities.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Homeless and vulnerably housed individuals in high income countries bear a high burden of chronic illness, even in countries with publically funded health care services. In major urban centers, this population experiences higher mortality rates than individuals with stable housing.1 Medical comorbidities including hypertension, arthritis and other musculoskeletal disorders, obstructive lung disease, tuberculosis, respiratory tract infections, human immunodeficiency virus, hepatitis, peripheral vascular disease, and digestive tract disease are common in this population.2 Rates of many of these chronic illnesses and infectious diseases are higher in homeless individuals than age- and gender-matched controls with stable housing.3 Nearly 30 % of homeless or vulnerably housed individuals suffer from at least two medical conditions, and this number doubles among individuals over 50 years of age.2 Poor dental health, visual impairment, exposure-related skin diseases, nutritional deficiency, and trauma are also common.4 , 5 In addition to a high prevalence of chronic disease, homeless and vulnerably housed individuals often experience poorer disease-specific outcomes. For example, among persons living with HIV on antiretroviral therapy, homelessness has been associated with lower rates of HIV virologic suppression, which is mediated by lower levels of antiretroviral adherence.6
Mental health comorbidities, including substance use disorders, depression, anxiety, and posttraumatic stress disorder, are highly prevalent among homeless and vulnerably housed individuals.2 Prevalence of substance use has been found to be 50–85 % among homeless individuals2 , 7 and prevalence of mental health comorbidities has been reported to be as high as 93 % in some urban centers.8 Substance use has been found to be a risk factor for both mortality and unmet care needs in this population.7
Despite high prevalence of chronic physical and mental health comorbidities, homeless and vulnerably housed individuals often experience gaps between care needed and care accessed.9 Approximately half of homeless individuals report unmet medical care needs.10 In one study, fewer than half of homeless individuals surveyed had a family physician and the odds of having a family physician declined with increased time spent homeless.11 A meta-analysis of four national surveys in the USA found worsening housing instability to be associated with postponing needed health care or medication use.12 Predictors of unmet medical care needs include substance use disorders, depression, food insecurity, visual impairment, lack of health insurance, and experiences of violence.13 , 14 Reported barriers to receiving care for homeless and vulnerably housed individuals include prejudice and stigma, wait times and limited after-hour services, lack of health insurance, cost of medications, transportation limitations, stress associated with shelter life, and being poorly connected to social services.8 , 15 , 16
Although ambulatory care is underutilized by homeless and vulnerably housed individuals, higher emergency department and inpatient hospital utilization have been described for this population.1 , 12 , 17 Predictors of emergency department utilization include mood disorders, psychosis, suicide risk, anxiety disorders, and intimate partner violence.18 , 19
Unmet physical health care needs and high rates of emergency department utilization are both frequently observed among homeless and vulnerably housed individuals; however, few studies have explored the effect of residential stability on these markers of health care utilization. This study therefore sought to examine the effect of residential stability among homeless and vulnerably housed individuals on reducing unmet physical health care needs and emergency department utilization using 4 years of longitudinal data from the health and housing in transition study.
Methods
The health and housing in transition (HHiT) study was a prospective cohort study of homeless and vulnerably housed single adults in the Canadian cities of Vancouver, Toronto, and Ottawa. The design of the study has been previously described in detail.20
Participants and Recruitment
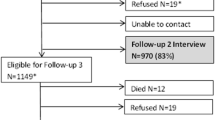
Between January and December 2009, 1190 single adults (18 years or older) were enrolled, of whom 595 were homeless and 595 were vulnerably housed. Homelessness was defined as not living in one’s own home within the last week and living in a shelter, public space, vehicle, abandoned building, or someone else’s home. Vulnerably housed status was defined as living in one’s own room, apartment, or place, but having two or more moves over the past year. Recruitment of homeless adults occurred at shelters and meal programs using sampling methods designed for this population.21 Vulnerably housed individuals were recruited at rooming houses, single room occupancy hotels, which reflect the lowest income housing stock in each of the cities as well as at meal programs. All study participants provided informed consent and were reimbursed $20 CDN for each interview. The Research Ethics Boards at St. Michael’s Hospital, the University of Ottawa, and the University of British Columbia approved this study.
Survey Instrument
Full details of all survey instruments used in the HHiT study have been published elsewhere.20 Immediately following recruitment and informed consent, trained research personnel conducted structured, in-person interviews. Data were collected on housing history using The Residential Time-Line Follow-Back Inventory.22 Additional information was collected on sociodemographic characteristics (age, gender, race/cultural group), lifetime duration of homelessness (months prior to baseline), lifetime prevalence of mental health diagnoses (at baseline) and chronic health conditions. Chronic health conditions were those which were diagnosed by a health professional and had persisted or were expected to persist for at least 6 months. The number of identified chronic health conditions was categorized at baseline (0, 1, 2, and ≥3). Chronic health conditions included hypertension, heart disease, obstructive lung disease, cirrhosis, chronic diarrhea, viral hepatitis, peptic or duodenal ulcers, urinary incontinence, inflammatory bowel disease, arthritis, physical disabilities limiting mobility, human immunodeficiency virus, tuberculosis or exposure to tuberculosis, epilepsy, fetal alcohol syndrome, migraines, traumatic brain injury, stroke, glaucoma, cataracts, hearing impairment, cancer, diabetes, anemia, and dermatologic conditions.
Participants were also asked if they had a primary care provider in the previous 12 months, employment (Did you work in past 12 months? Are you currently working?), and incarceration history (past 12 months). We also used the ten-item Drug Abuse Screening Test (DAST-10)23 to screen for illicit drug use (positive screen ≥3) and defined problematic drug as a DAST-10 score ≥6, which would merit intensive assessment.24 The DAST-10 asks individuals about behaviors related to the use of non-medical drugs as well as prescription and over-the-counter medication use in excess to the recommended amount. The DAST-10 does not specify individual drugs but clarifies that it does not pertain to behaviors related to alcohol and tobacco use. The Alcohol Use Disorders Identification Test (AUDIT),25 a ten-item questionnaire, was used to screen for alcohol use disorder (positive screen ≥8), and we defined problematic alcohol use as an AUDIT score of ≥20.26 These instruments have been validated for use in previous studies of vulnerable populations.25 , 27 Problematic substance use was defined as having an AUDIT score of ≥20 and/or a DAST-10 score of ≥6. Interviews took approximately 60 to 90 minutes to complete. In this study, we report the findings from baseline and four subsequent annual follow-up interviews.
Main Explanatory Variables
We classified the housing history data based on methods adapted from Tsemberis et al.22 Each residence in a participant’s housing history was classified into 1 of 25 types of residence, which were then classified into one of three mutually exclusive residence categories: housed, institution, and homeless. Individuals were considered homeless if they were living with friends or family and not paying rent, or lived in a homeless shelter, on the streets or at a campground. Periods of time spent in institutions were considered periods of being homeless or housed based on a functional classification previously described.28 Participants were considered to have achieved residential stability at each follow-up interview if they were housed and had been living in the same location for 6 months or more.
Outcome Variables
We defined unmet physical health care needs as responding yes to the question: “During the past 12 months, was there ever a time when you felt that you needed health care but you didn’t receive it?” This question was based on the definition of unmet health care needs used in other national surveys including the Health Care for the Homeless User Survey,14 the Joint Canada/US Survey of Health,29 and the National Population Health Survey.30 It has also been previously used to assess unmet health care needs among homeless adults.14 , 31 Emergency department (ED) use was defined as receiving health care from a hospital emergency room in the past 12 months. We also asked about the number of times they used the ED in the past 12 months. Adults who experience homelessness are quite accurate reporters of their use of health care, especially for ED visits and hospital admission. Documented sensitivity and specificity of self-report for ED utilization are 80 and 83 %, respectively, in this population when compared with a reference standard of health administrative data.32
Statistical Analysis
Comparisons were made using the chi-square test or Fisher exact test (where appropriate) for categorical variables and one-way ANOVA for continuous variables. For missing data (i.e., participant did not know or refused to answer), the denominators were adjusted accordingly. We excluded 17 transgender participants whose small count would not allow for adjusted analysis by transgender identity. We used a generalized logistic mixed effects regression model to examine the association between residential stability at each follow-up interview and unmet physical health care needs during the prior 12 months where the clusters were the multiple observations collected per participant. We adjusted for the following potential confounding factors, assessed only at baseline, as fixed effects: gender, age, self-identified racial/cultural group, lifetime duration of homelessness, city of recruitment, number of chronic health conditions, and having ever been diagnosed with a mental health problem. We also considered being born in Canada and having children as covariates, but they were not significant independent predictors of ED utilization and were excluded from the final model so that model parsimony could be optimized. We also adjusted for a discrete categorical time-point variable since responses were obtained at each follow-up interview point (years 1, 2, 3, and 4). The following variables were entered as time-varying covariates: problematic substance use, employment, incarceration, and having a primary care provider. We also used generalized logistic mixed effects regression model to explore the association of residential stability with ED use during the prior 12 months at each follow-up interview, adjusting for the same fixed and time-varying variables as the first multivariable model.
Results
Study Participant Demographics
Of the 1173 participants included in this analysis, 387 (33.0 %) were from Vancouver, 390 (33.2 %) from Toronto, and 396 (33.8 %) from Ottawa. Demographic characteristics of participants in each of the three cities are presented in Table 1. Participants in Toronto were less likely to report problematic substance use, have three or more chronic health conditions, or be employed in the past 12 months and more likely to be single or never married or identify as Black/African-Canadian. Participants in Vancouver had a higher monthly income and were more likely to identify as indigenous or to have ≥3 chronic health conditions than participants in Toronto or Ottawa.
Unmet Physical Health Care Needs
At the baseline interview, the proportions of participants in Vancouver who did and did not attain residential stability reporting unmet physical care needs were 43.3 and 40.6 %, respectively. For participants in Toronto, the proportions were 26.7 and 37.0 %, respectively, and for participants in Ottawa, the proportions were 32.7 and 38.6 %, respectively. Over the 4-year follow-up period, the proportion of participants reporting unmet physical health care needs declined for participants in all three cities among participants who did and did not attain residential stability (Fig. 1). However, there was an increment in unmet physical health care needs reported among participants in Ottawa who did not attain residential stability between follow-up years 3 and 4.
A total of 729 participants had non-missing values at baseline and all four follow-up interviews. Of these, 83 (11.4 %) never attained residential stability, 108 (14.8 %) experienced residential stability at one time point, 152 (20.9 %) experienced residential stability at two time points, 178 (24.4 %) experienced residential stability at three time points, 161 (22.1 %) experienced residential stability at four time points, and 47 (6.4 %) always had residential stability. The relative reduction in the proportion reporting unmet physical health care needs was greatest among participants who always had residential stability (Fig. 2).
Unmet physical health care needs over the last 12 months of health and housing in transition participants who achieved or did not achieve residential stability at all five assessment points: Vancouver, Toronto, and Ottawa, 2009–2013. This plot includes only those participants who completed all four follow-up surveys and who either achieved residential stability at all five assessment points (n = 47) or at none of the assessment points (n = 83).
In the bivariate analyses, residential stability (odds ratio (OR), 0.75; 95 % confidence interval (95 % CI), 0.63, 0.90) and having a primary care provider were significantly associated with a lower odds of having unmet physical health needs over time (Table 2). Lifetime history of a mental health problem, having at least three chronic health conditions, having problematic substance use, and incarceration history in the past 12 months were associated with higher odds of having unmet physical health care needs over time. After adjustment for age, gender, race/cultural group, having ever been diagnosed with a mental health problem, having at least three chronic medical conditions, lifetime duration of homelessness, problematic substance use, employment, incarceration history, having a primary health provider, time point, and city of recruitment, residential stability was still significantly associated (adjusted OR, 0.82; 95 % CI, 0.67, 0.98) with lower odds of having unmet physical health care needs. Lifetime history of a mental health problem, having at least three chronic health conditions, having problematic substance use, and incarceration history in the past 12 months remained significant predictors of having unmet physical health care needs in the multivariable model (Table 2).
Emergency Department Utilization
At the baseline interview, the proportions of participants in Vancouver who did and did not attain residential stability who received emergency department care in the past 12 months were similar (58.2 and 58.0 %, respectively). For participants in Toronto, the proportions were 57.6 and 51.5 %, respectively, and for participants in Ottawa, the proportions were 49.1 and 54.5 %, respectively (Fig. 3). Over the 4-year follow-up period, the proportion of participants receiving care in the emergency department decreased among participants who did attain residential stability in all three cities and also among participants from Ottawa who did not attain residential stability (Fig. 3). However, among participants who did not attain residential stability in Vancouver and Toronto, no significant decline in emergency department utilization was observed.
At baseline, 529 (45.2 %), 223 (19.0 %), 202 (17.3 %), 68 (5.8 %), and 149 (12.7 %) participants reported 0, 1, 2, 3, and more than 3 emergency department visits in the preceding 12 months, respectively. Over the 4-year follow-up period, the proportion of participants reporting three and more than three emergency department visits declined over time and were 42 (4.8 %) and 68 (7.7 %) at the 4-year follow-up, respectively (Table 3).
In the bivariate models, residential stability (OR, 0.69; 95 % CI, 0.59, 0.81), age, and time point were significantly associated with a lower odds of emergency department utilization within the last 12 months (Table 4). Lifetime history of mental health problems, having ≥3 chronic health conditions, problematic substance use, incarceration within the last 12 months, and having a primary health provider were associated with increased odds of emergency department utilization within the last 12 months.
After adjustment for age, gender, race/cultural group, lifetime history of mental health problems, having ≥3 chronic medical conditions, lifetime duration of homelessness, problematic substance use, employment, incarceration, having a primary health provider, time point, and city of recruitment, residential stability was still significantly associated (adjusted OR, 0.74; 95 % CI, 0.62, 0.88) with lower odds of emergency department utilization within the last 12 months (Table 4). In the adjusted model, age and time point remained significant negative predictors of emergency department utilization in the past 12 months. Lifetime history of mental health problems, having ≥3 chronic health conditions, problematic substance use, incarceration within the past 12 months, and having a primary health provider remained significant positive predictors of emergency department utilization within the past 12 months.
Discussion
In this study, we found that residential stability was associated with both a reduced risk of having unmet physical health care needs and a decrease in emergency department utilization. These findings remained significant after adjustment for potential confounders.
These findings are consistent with literature describing an association between housing instability and unmet physical health care needs. Kushel et al. found that housing instability was independently associated with postponing needed medical care and medications.17 In Washington State, USA, individuals with insecure housing have reported poorer health status and delaying physician visits due to financial concerns.33 Findings from this study suggest that even when health insurance makes primary care services available, housing insecurity is associated with discrepancies in health care utilization patterns. Although the association between housing instability and unmet physical health care needs has been well documented, most prior studies have been cross-sectional in design. This longitudinal study is unique in that it demonstrates strong associations in a large, multi-city sample that are robust over time.
An analysis of health care utilization data in Toronto, Canada, which has a universal health insurance system, found homeless individuals to have significantly higher rates of emergency department utilization and hospital admission compared with low-income-matched controls.34 Similarly, an analysis of the Veterans Affairs administrative database found that homeless veterans had four times higher odds of using the emergency department than non-homeless veterans.35 These studies suggest that even when homeless individuals have free access to primary care services, emergency department utilization is higher. This may be due to additional barriers to primary health care access, such as transportation barriers and stigma; however, more research is needed to better understand causes for increased emergency department utilization among homeless and vulnerable housed individuals. Flexible models of low-barrier delivery of interdisciplinary primary health care services such as community outreach, after-hour clinics should be further explored.
Our findings are consistent with existing literature that has described increased emergency department utilization among vulnerably housed individuals. Residential instability, and in particular, shelter use, has been associated with increased reliance on emergency department services to meet the healthcare needs of women of low socioeconomic status in New York, USA.36 A recent systematic review of housing status and health outcomes among people living with HIV found that housing instability was strongly correlated to acute care utilization, including both hospital-based emergency department care and inpatient care. In addition, an apparent dose effect was observed with increased rates of acute care utilization with increasing degree of housing instability.37 Similarly, less stable housing among homeless and vulnerably housed individuals has been associated with increased emergency department utilization.38
Interestingly, in this observational cohort, participants experienced fewer unmet physical health care needs and had decreased emergency department use over time. This may in part be due to attrition bias whereby participants with more active health problems may have been more likely to be lost to follow-up.
These findings have supported the existing literature by recognizing housing instability as a determinant of health that affects both unmet physical health care needs and emergency department utilization. This highlights the need to improve access to stable and affordable housing, particularly for individuals with many medical and mental health comorbidities. Housing first strategies, which provide immediate access to independent housing along with mental health supports for people with mental health comorbidities, have been demonstrated to improve housing stability in several Canadian urban settings.39 Implementation of expanded housing first programs should be considered an evidence-based strategy to address housing insecurity as a determinant of health. However, studies on supportive housing programs have had conflicting results in their impact on decreasing emergency department utilization and cost efficacy.40 , 41 Many housing intervention studies have been underpowered, and longer duration of follow-up may be required to detect significant differences.
In addition, lower rates of emergency department utilization were observed in Ottawa compared with Toronto. These cities have a similar climate and health care is provided through the same provincial single-payer system. Differences in service delivery and accessibility in these two cities may account for this observed difference in emergency department utilization and warrants further exploration.
Limitations of this study are that it only focused on unmet physical health care needs and emergency department utilization as outcomes. A more holistic model of health and wellness for homeless and vulnerably housed individuals, including mental health and quality-of-life outcomes, may identify further benefits of housing stability. In addition, future studies should further evaluate predictors of residential stability to identify supportive factors that may enable individuals to achieve residential stability.
An additional limitation is the use of self-report for the outcome of unmet physical health need. This outcome has been widely used and is likely to accurately represent perceived health status, but future studies including linkage to health administrative data could correlate this measure with hospitalization for preventable and ambulatory-sensitive conditions. Other self-reported measures of health status have been found to be robust predictors of health care utilization and can be even stronger predictors than validated comorbidity indices.42
Strengths of this study include sampling from three major Canadian cities, which differ in their geographic region, available services, and climate, allowing for increased generalizability of the findings. Additional strengths are the large sample size of homeless and vulnerably housed individuals, the longitudinal follow-up over 4 years, the use of time-varying covariates, and an attrition rate of less than 25 % over 4 years.
In conclusion, residential stability is associated with fewer unmet physical health care needs and lower emergency department utilization among homeless and vulnerably housed individuals. Strategies to improve the health of homeless and vulnerably housed individuals need to address access to stable housing as a significant determinant of underlying health disparities. Improved provision of supportive housing services, increased availability of affordable housing, and better integration of health and housing services may be helpful in facilitating residential stability among homeless and vulnerable housed individuals, and this may translate into improved health care utilization for this population.
References
LePage JP, Bradshaw LD, Cipher DJ, Crawford AM, Hoosyhar D. The effects of homelessness on Veterans’ health care service use: an evaluation of independence from comorbidities. Public Health. 2014; 128(11): 985–92. doi:10.1016/j.puhe.2014.07.004.
Garibaldi B, Conde-Martel A, O’Toole TP. Self-reported comorbidities, perceived needs, and sources for usual care for older and younger homeless adults. J Gen Intern Med. 2005; 20(8): 726–30. doi:10.1111/j.1525-1497.2005.0142.x.
Wagner J, Diehl K, Mutsch L, Loffler W, Burkert N, Freidl W. Health status and utilisation of the healthcare system by homeless and non-homeless people in Vienna. Health Soc Care Community. 2014; 22(3): 300–7. doi:10.1111/hsc.12083.
Stratigos AJ, Katsambas AD. Medical and cutaneous disorders associated with homelessness. Skinmed. 2003; 2(3): 168–72.
Grossberg AL, Carranza D, Lamp K, Chiu MW, Lee C, Craft N. Dermatologic care in the homeless and underserved populations: observations from the Venice Family Clinic. Cutis. 2012; 89(1): 25–32.
Milloy MJ, Kerr T, Bangsberg DR, Buxton J, Parashar S, Guillemi S, et al. Homelessness as a structural barrier to effective antiretroviral therapy among HIV-seropositive illicit drug users in a Canadian setting. AIDS Patient Care STDS. 2012; 26(1): 60–7. doi:10.1089/apc.2011.0169.
Palepu A, Gadermann A, Hubley AM, Farrell S, Gogosis E, Aubry T, et al. Substance use and access to health care and addiction treatment among homeless and vulnerably housed persons in three Canadian cities. PLoS ONE. 2013; 8(10): e75133. doi:10.1371/journal.pone.0075133.
Krausz RM, Clarkson AF, Strehlau V, Torchalla I, Li K, Schuetz CG. Mental disorder, service use, and barriers to care among 500 homeless people in 3 different urban settings. Soc Psychiatry Psychiatr Epidemiol. 2013; 48(8): 1235–43. doi:10.1007/s00127-012-0649-8.
Lebrun-Harris LA, Baggett TP, Jenkins DM, Sripipatana A, Sharma R, Hayashi AS, et al. Health status and health care experiences among homeless patients in federally supported health centers: findings from the 2009 patient survey. Health Serv Res. 2013; 48(3): 992–1017. doi:10.1111/1475-6773.12009.
Kertesz SG, McNeil W, Cash JJ, Desmond R, McGwin G Jr, Kelly J, et al. Unmet need for medical care and safety net accessibility among Birmingham’s homeless. J Urban Health. 2014; 91(1): 33–45. doi:10.1007/s11524-013-9801-3.
Khandor E, Mason K, Chambers C, Rossiter K, Cowan L, Hwang SW. Access to primary health care among homeless adults in Toronto, Canada: results from the Street Health survey. Open Med. 2011; 5(2): e94–103.
Reid KW, Vittinghoff E, Kushel MB. Association between the level of housing instability, economic standing and health care access: a meta-regression. J Care Poor Underserved. 2008; 19(4): 1212–28. doi:10.1353/hpu.0.0068.
Teruya C, Longshore D, Andersen RM, Arangua L, Nyamathi A, Leake B, et al. Health and health care disparities among homeless women. Women Health. 2010; 50(8): 719–36. doi:10.1080/03630242.2010.532754.
Baggett TP, O’Connell JJ, Singer DE, Rigotti NA. The unmet health care needs of homeless adults: a national study. Am J Public Health. 2010; 100(7): 1326–33. doi:10.2105/AJPH.2009.180109.
Canavan R, Barry MM, Matanov A, Barros H, Gabor E, Greacen T, et al. Service provision and barriers to care for homeless people with mental health problems across 14 European capital cities. BMC Health Serv Res. 2012; 12: 222. doi:10.1186/1472-6963-12-222.
Martens WH. Vulnerable categories of homeless patients in Western societies: experience serious barriers to health care access. Med Law. 2009; 28(2): 221–39.
Kushel MB, Gupta R, Gee L, Haas JS. Housing instability and food insecurity as barriers to health care among low-income Americans. J Gen Intern Med. 2006; 21(1): 71–7. doi:10.1111/j.1525-1497.2005.00278.x.
Hodgson KJ, Shelton KH, van den Bree MB. Mental health problems in young people with experiences of homelessness and the relationship with health service use: a follow-up study. Evid Based Ment Health. 2014; 17(3): 76–80. doi:10.1136/ebmental-2014-101810.
Vijayaraghavan M, Tochterman A, Hsu E, Johnson K, Marcus S, Caton CL. Health, access to health care, and health care use among homeless women with a history of intimate partner violence. J Community Health. 2012; 37(5): 1032–9. doi:10.1007/s10900-011-9527-7.
Hwang SW, Aubry T, Palepu A, Farrell S, Nisenbaum R, Hubley AM, et al. The health and housing in transition study: a longitudinal study of the health of homeless and vulnerably housed adults in three Canadian cities. Int J Public Health. 2011; 56(6): 609–23. doi:10.1007/s00038-011-0283-3.
Ardilly P, Le Blanc D. Sampling and weighting a survey of homeless persons: a French example. Surv Methodol. 2001; 27(1): 109–18.
Tsemberis S, McHugo G, Williams V, Hanrahan P, Stefancic A. Measuring homelessness and residential stability: the residential time-line follow-back inventory. J Community Psychol. 2007; 35(1): 29–42. doi:10.1002/jcop.20132.
French MT, Roebuck MC, McGeary KA, Chitwood DD, McCoy CB. Using the drug abuse screening test (DAST-10) to analyze health services utilization and cost for substance users in a community-based setting. Subst Use Misuse. 2001; 36(6–7): 927–46.
Yudko E, Lozhkina O, Fouts A. A comprehensive review of the psychometric properties of the drug abuse screening test. J Subst Abuse Treat. 2007; 32(2): 189–98. doi:10.1016/j.jsat.2006.08.002.
Maisto SA, Carey MP, Carey KB, Gordon CM, Gleason JR. Use of the AUDIT and the DAST-10 to identify alcohol and drug use disorders among adults with a severe and persistent mental illness. Psychol Assess. 2000; 12(2): 186–92. doi:10.1037/1040-3590.12.2.186.
Barbor TF, de la Fuente JR, Saunders J, Grant M. AUDIT: the alcohol use disorders identification test: guidelines for use in primary health care. Geneva, Switzerland: World Health Organization; 1992.
Donovan DM, Kivlahan DR, Doyle SR, Longabaugh R, Greenfield SF. Concurrent validity of the Alcohol Use Disorders Identification Test (AUDIT) and AUDIT zones in defining levels of severity among out-patients with alcohol dependence in the COMBINE study. Addiction. 2006; 101(12): 1696–704. doi:10.1111/j.1360-0443.2006.01606.x.
The Health and Housing in Transition (HHiT) Study Team. Housing definitions and housing variables. University of Toronto TSpace. https://tspace.library.utoronto.ca/handle/1807/69938. Published 2015. Accessed 12 Feb 2016.
Lasser KE, Himmelstein DU, Woolhandler S. Access to care, health status, and health disparities in the United States and Canada: results of a cross-national population-based survey. Am J Public Health. 2006; 96(7): 1300–7. doi:10.2105/AJPH.2004.059402.
Sanmartin C, Houle C, Tremblay S, Berthelot JM. Changes in unmet health care needs. Health Rep. 2002; 13(3): 15–21.
Hwang SW, Ueng JJ, Chiu S, Kiss A, Tolomiczenko G, Cowan L, et al. Universal health insurance and health care access for homeless persons. Am J Public Health. 2010; 100(8): 1454–61. doi:10.2105/AJPH.2009.182022.
Hwang SW, Chambers C, Katic M. Accuracy of self-reported health care use in a population-based sample of homeless adults. Health Serv Res. 2016; 51(1): 282–301. doi:10.1111/1475-6773.12329.
Stahre M, VanEenwyk J, Siegel P, Njai R. Housing insecurity and the association with health outcomes and unhealthy behaviors, Washington State, 2011. Prev Chronic Dis. 2015; 12, E109. doi:10.5888/pcd12.140511.
Hwang SW, Chambers C, Chiu S, Katic M, Kiss A, Redelmeier DA, et al. A comprehensive assessment of health care utilization among homeless adults under a system of universal health insurance. Am J Public Health. 2013; 103(Suppl 2): S294–301. doi:10.2105/AJPH.2013.301369.
Tsai J, Doran KM, Rosenheck RA. When health insurance is not a factor: national comparison of homeless and nonhomeless US veterans who use Veterans Affairs Emergency Departments. Am J Public Health. 2013; 103(Suppl 2): S225–31. doi:10.2105/AJPH.2013.301307.
Duchon LM, Weitzman BC, Shinn M. The relationship of residential instability to medical care utilization among poor mothers in New York City. Med Care. 1999; 37(12): 1282–93.
Aidala AA, Wilson MG, Shubert V, Gogolishvili D, Globerman J, Rueda S, et al. Housing status, medical care, and health outcomes among people living with HIV/AIDS: a systematic review. Am J Public Health. 2016; 106(1): 95. doi:10.2105/AJPH.2015.302905a.
Kushel MB, Perry S, Bangsberg D, Clark R, Moss AR. Emergency department use among the homeless and marginally housed: results from a community-based study. Am J Public Health. 2002; 92(5): 778–84.
Aubry T, Tsemberis S, Adair CE, Veldhuizen S, Streiner D, Latimer E, et al. One-year outcomes of a randomized controlled trial of housing first with ACT in five Canadian cities. Psychiatr Serv. 2015; 66(5): 463–9. doi:10.1176/appi.ps.201400167.
Kessell ER, Bhatia R, Bamberger JD, Kushel MB. Public health care utilization in a cohort of homeless adult applicants to a supportive housing program. J Urban Health. 2006; 83(5): 860–73. doi:10.1007/s11524-006-9083-0.
Raven MC, Doran KM, Kostrowski S, Gillespie CC, Elbel BD. An intervention to improve care and reduce costs for high-risk patients with frequent hospital admissions: a pilot study. BMC Health Serv Res. 2011; 11: 270. doi:10.1186/1472-6963-11-270.
Rosella LC, Fitzpatrick T, Wodchis WP, Calzavara A, Manson H, Goel V. High-cost health care users in Ontario, Canada: demographic, socio-economic, and health status characteristics. BMC Health Serv Res. 2014; 14: 532. doi:10.1186/s12913-014-0532-2.
Acknowledgments
This study was funded by the Canadian Institutes for Health Research. We would like to acknowledge the following individuals from our community partner organizations: Street Health (Laura Cowan, Erika Khandor, Stephanie Gee), PHS Community Services Society (Liz Evans, Clare Hacksel), and Ottawa Inner City Health (Wendy Muckle). The authors also thank the study coordinators and interviewers in each of the three cities as well as the shelter, drop-in, and municipal and provincial staff for their assistance with participant recruitment and follow-up. We also thank Dr. Hubert Wong for his guidance on the statistical analyses. We are especially grateful to the health and housing in transition study participants for their contribution to these data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jaworsky, D., Gadermann, A., Duhoux, A. et al. Residential Stability Reduces Unmet Health Care Needs and Emergency Department Utilization among a Cohort of Homeless and Vulnerably Housed Persons in Canada. J Urban Health 93, 666–681 (2016). https://doi.org/10.1007/s11524-016-0065-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-016-0065-6