Abstract
With the rapid increase in the use of thoracic pedicle screws in scoliosis, accurate and safe placement of screw within the pedicle is a crucial step during the scoliosis surgery. To make thoracic pedicle screw placement safer various techniques are used, Patient-specific drill template with pre-planned trajectory has been thought as a promising solution, it is critical to assess the efficacy, safety profile with this technique. In this paper, we develop and validate the accuracy and safety of thoracic transpedicular screw placement with patient-specific drill template technique in scoliosis. Patients with scoliosis requiring instrumentation were recruited. Volumetric CT scan was performed on each desired thoracic vertebra and a 3-D reconstruction model was generated from the CT scan data. The optimal screw size and orientation were determined and a drill template was designed with a surface that is the inverse of the posterior vertebral surface. The drill template and its corresponding vertebra were manufactured using rapid prototyping technique and tested for violations. The navigational template was sterilized and used intraoperatively to assist with the placement of thoracic screws. After surgery, the positions of the pedicle screws were evaluated using CT scan and graded for validation. This method showed its ability to customize the placement and the size of each pedicle screw based on the unique morphology of the thoracic vertebra. In all the cases, it was relatively very easy to manually place the drill template on the lamina of the vertebral body during the surgery. This method significantly reduces the operation time and radiation exposure for the members of the surgical team, making it a practical, simple and safe method. The potential use of such a navigational template to insert thoracic pedicle screws in scoliosis is promising. The use of surgical navigation system successfully reduced the perforation rate and insertion angle errors, demonstrating the clear advantage in safe and accurate pedicle screw placement of scoliosis surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1 Introduction
Pedicles are the strongest part of the vertebra, and pedicle screw fixation affords multidimensional control, providing greater rigidity with an improved fusion rate. In 1995, Suk et al. [39] first described the use of thoracic pedicle screws in the treatment of adolescent idiopathic scoliosis (AIS). More recently, the use of thoracic pedicle screws has become increasingly popular in addressing deformity constructs due to its numerous advantages over other methods of spinal fixation [17, 20, 30]. These advantages include three-column fixation, immediate rigidity, better coronal and sagittal correction, shorter fusion length in scoliosis surgery, lower pseudo arthrosis rates, lower implant failures, and fewer post-operative bracing requirements as compared to conventional hook and wire constructs [9, 14, 22, 41]. However, the use of thoracic screws in scoliosis remains controversial. It is technically difficult with a high risk of potential complications such as neurologic and vascular complications associated with misplaced pedicle screws, which could impair the pull-out strength of the implants and increase the chances for implant failure [7, 8, 18, 19, 23, 36, 40]. Thus, the accurate and safe placement of screws within the pedicle is a crucial step during scoliosis surgery.
Various techniques have been used to facilitate safer thoracic pedicle screw placement. These techniques can be broadly classified into four types: (1) free-hand technique which rely on anatomical landmarks and averaged angular dimensions, (2) techniques with direct exposure of the pedicle such as through laminotomy, (3) CT-based computer-assisted surgery (CAS), and (4) fluoroscopy-based CAS technique.
Most studies have shown that the rates of misplacement for the free-hand technique are usually between 28 and 43%, while only a few studies have shown rates of <5% [3, 11]. Hence, the screw breach rate may be dangerously high when the anatomy is altered as in scoliosis. Lonner et al. [23] suggested that there should be a considerable learning curve for using the pedicle screws in scoliosis surgery to avoid complications. The need for improved accuracy and consistency in the placement of thoracic pedicle screws has led to investigations on the application of computer-navigated spine surgery. Computer-assisted pedicle screw installation allows for an increased accuracy in using screws, thus decreasing the incidence of misplaced screws [10, 15, 16, 29, 35, 43]. Although better results have been uniformly reported with the use of navigation, pre-operative CT scans are usually performed in supine position, and the prone position required for surgery can lead to an alteration in the intervertebral anatomic relationships within the curve. This leads to the need for surface registration of each vertebra, leading to an increase in registration-based errors and surgical time, as well as high equipment cost.
Considering these difficulties, surgeons must use whatever techniques they find helpful to create a safe environment when placing thoracic pedicle screws into the deformed pediatric spine. We developed a patient-specific navigational template technique which has been proven in cadaver and clinical studies in the cervical and lumbar spine [25–27]. However, there has been no report on its accuracy in the vivo conditions of thoracic pedicle screw insertion in scoliosis. This study, therefore, introduces an ingenious, custom-fit navigational template for the placement of pedicle screws in the deformed thoracic spine and validates it in a clinical setting. Based on this technique, the trajectory of the thoracic pedicle screws was first identified based on the pre-operative CT scan model. The drill template was then specifically designed for the patient so that it can maintain close contact with the postural surface of the thoracic vertebra and provide the best stability for drilling. To the best of our knowledge, there has been no report in the literature on the use of a navigational template for transpedicular screw placement at the deformed thoracic spine.
2 Methods
From June 2006 to September 2009, 16 patients (12 females, 4 males, age 5–18 years) with scoliosis (14 AIS, 2 congenital scoliosis) undergoing spinal deformity correction surgeries using posterior pedicle screw instrumentation of the thoracic spine formed the study group. Titanium implants were used in all patients as they produce less scatter artifact when performing post-operative imaging studies.
2.1 Manufacture of navigational template
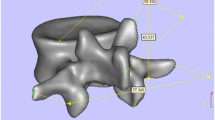
Before the operation, a spiral three-dimensional (3-D) CT scan (LightSpeed VCT, GE, USA) was performed on the thoracic spine of each patient with 0.625 mm slice thickness and 0.35 mm in-plane resolution. The images were stored in DICOM format and transferred to a workstation running MIMICS 10.01 software (Materialise company, Belgium) to generate a 3-D reconstruction model for the desired thoracic vertebra (Fig. 1a). The 3-D vertebral model was then exported in STL format and opened in a workstation running Reverse Engineering (RE) software UG imageware12.0 (EDS, USA) to determine the optimal screw size and orientation. A screw with a diameter of 5 mm was placed virtually into the 3-D spinal model on both sides. The virtual screw’s entry point and the trajectory were placed at the center of the pedicle without violating the cortex (Fig. 1b).
The template surface was created to be the inverse of the spinous, laminar, and transverse process, thus potentially enabling a fit in a lock-and-key fashion similar to a physical casting of the vertebral surface, and specifically avoiding overlap onto adjacent segments (Fig. 1c). The inner diameter of the hollow cylinder was created to accommodate the pre-planned trajectory for drilling. Once these were done, a drill template was constructed with a surface designed to be the inverse of the vertebral surface.
The computer model was then exported into STL format. The biomodel of the corresponding navigational template was produced through acrylate resin (Somos 14120, DSM Desotech Inc, USA) using stereolithography rapid prototyping (RP) technique. The accuracy of the navigational template was examined through visual inspection before the surgery. The biomodel and its corresponding template were placed together, and a standard electric power drill was used to drill the screw trajectory into the biomodel at the pre-defined placement. Visual inspection was conducted to check for violations of the pedicle.
2.2 Pre-operative planning
According to the type of scoliosis, the fusion level is determined, and the instrumentational vertebra is chosen. The design and development of the drill template for each vertebra are also made according to the instrumentational vertebra. The vertebral rotation, axes, length, and diameter of the pedicle were measured from the pre-operative CT scan. Thus, the length and diameter of every pedicle screw were decided upon before operation. The concave periapical (T5–8) pedicles are often deformed and are considered to be the most difficult area to work on during pedicle screw placement [6, 20, 33, 38]. If the pedicle is very narrow, an in-out-in technique can be chosen. (Fig. 2).
3D reconstruction of a single vertebra and the biomodel of the drill template a The best trajectory of the pedicle screw and measurement of the length of the pedicle; b In–out-in technique in the concave side; c The navigational template fits the vertebra perfectly; d The template can show the location, diameter, and length of the pedicle screw; e The navigational template fits the RP model of the vertebra very well
2.3 Operation procedure
The spine was exposed subperiosteally on both sides, up to the tips of the transverse processes. For the thoracic spine, the soft tissues on the facet joints were thoroughly cleaned off to ensure better visualization of the bony landmarks. The drill template was then placed on the spinous, lamina, and transverse processes. The drill template and the corresponding spinous process were fitted well. A high-speed drill was used along the navigational channel to drill the trajectory of each pedicle screw. Using a hand drill, the trajectory of the pedicle screw was carefully drilled to a depth in accordance with the pre-operation plan. The pedicle screw, the diameter and length of which had been chosen pre-operatively, was carefully inserted along the same trajectory. After screw placement and correction of deformity, all exposed laminar surfaces were decorticated, and the autologous iliac crest bone was grafted.
2.4 Accuracy of the pedicle screw
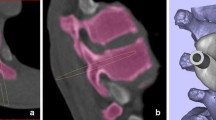
In each case, post-operative CT scans were obtained to assess the accuracy of screw placement in all patients by an independent observer (Dr. Yu B. Chen). The radiographs and CT scans were analyzed with respect to the breach of the pedicle wall by the screw either medially, laterally, inferiorly, or superiorly. Screw placement was graded on CT as follows: grade 0, no pedicle perforation; grade 1, only the threads outside the pedicle (less than 2 mm); grade 2, core screw diameter outside the pedicle (2–4 mm); grade 3, screw entirely outside the pedicle [24]. The time taken for the insertion of each screw was then measured Fig. 3.
A 12-year-old male with a 62° pre-operative curve; thoracic pedicle screw was inserted using the drill template; a AP X-ray; b 3-D model of the spine; c pedicle screw trajectory and design of the navigational template; d RP model of the navigational template, e The navigational template fits the posterior part of the thoracic perfectly in the operation; f drill the trajectory by a power drill. g, h, i, j X ray and CT scan show that the screws were fully contained within the pedicle and body; corrected to 11° 1 year after surgery, giving 82.3% correction of the major curve
3 Results
Using a virtual 3-D model, the optimal entry point for the drill can be chosen, thus determining the entry point and direction for the thoracic pedicle screw. The accuracy of the drill template was examined by drilling a K wire trajectory into the vertebra biomodel before operation. During the operation, the best fit for positioning the template can easily be found manually because no significantly free motion of the template occured when it was pressed slightly against the postal part of the thoracic spine. Therefore, the navigational template was used as in situ drill guide. To achieve this, exact preparation of the bone surface was essential, including meticulous exposure of the posterior elements through removal of the attached muscle and fat tissue without damage to the bony surface. The individual navigational template technique had the capability to customize the placement and size of each screw based on the unique morphology of each patient’s pedicle and to pre-operatively prepare the surgical plan.
The diameter of the screws used ranged from 4.0 to 6.5 mm. The length of screws was 30–50 mm. The average blood loss was 700 ml (range 500–1,200). In this study, the average pre-operative and post-operative Cobb’s angle measured was 54.2° (range 45°–82°) and 15.3(4°–41°), respectively, with 71.7% correction rate. The average screw insertion time was 1.24 min (range 1.16–2.5 min) per screw.
3.1 Accuracy of the pedicle screw
A total of 168 screws were placed from T2 to T12 in the 16 cases, and post-operative CT scans were obtained in all 16 patients. About 157 screws were considered intrapedicular, while 11 screws were considered to have a 0–2 mm breach (1 medial, 10 lateral in which 8 belonged to the planned in-out-in screws, the misplacement of pedicle screw is 1.8%). No pedicle screw breached more than 2 mm, and the overall screw accuracy (<2 mm breach is safe) was 100%. No screws penetrated the inferior or superior cortex in the sagittal plane.
4 Discussion
More recently, some authors have reported on the use of pedicle screws in the thoracic spine to enhance the correction rate and to minimize the fusion area despite potential risks, including pedicle dimension and vertebral rotation. Screw malposition increases the risk of injury to neural, vascular, and visceral structures [7, 28, 42]. In scoliosis patients, several unique morphometric characteristics such as an intravertebral asymmetry of the vertebra, smaller diameter of the concave side pedicle around the apex, and significant vertebral rotations appear. On the other hand, in severe deformities, the pedicles are frequently thinner, sclerosed, and waisted, allowing easy canal perforation and thereby significantly increasing perforation risk [21, 31, 37]. In particular, the concave apex carries the highest risk of spinal cord injury with medially placed screws [5, 7]. Pedicle morphology in patients with AIS was studied by O’Brien et al. [31] using radiographs and CT scans. A total of 512 pedicles from T1 to T12 were analyzed. The mean concave pedicle diameters ranged from 5.2 (T7) to 8.5 (T12) mm. The single smallest diameter was 3.4 mm at T7. Parent et al. [33] analyzed the vertebrae in 30 scoliotic specimens where the vertebrae were all separate, thus not allowing information on the curve size to be known. These were compared with 30 matched but nonscoliotic specimens. A three-dimensional digitizing protocol was used for the reconstructions. The minimal width for both scoliotic and control specimens was found in the T4–T7 region. The mean concave width was 2.60 mm at T4, 3.64 mm at T5, 3.78 mm at T6, and 4.00 mm at T7. Gilbert et al. [12] confirmed the findings of other authors that the concave pedicles can be so small that pedicle screw insertion is impossible. We also found that these findings can be confirmed pre-operatively through thin-section CT scanning. In such situations, extrapedicular screw placement should be considered.
Belmont et al. [2] reported on the clinical accuracy of thoracic pedicle screws in 40 scoliosis and kyphosis patients, demonstrating 43% screw perforation rate at T1–T12. In this study, the medial and lateral perforation rates of 14 and 29% were demonstrated without neurologic and vascular complications; however, two screws were subsequently removed due to their proximity to the aorta. Liljenqvist et al. [21] reported on 33 patients with thoracic pedicle screw insertion in idiopathic scoliosis, demonstrating 25% perforation rate without neurovascular and pulmonary complications; however, one screw was replaced due to its direct proximity to the thoracic aorta. In terms of serious complications, Minor et al. [28] reported on an iatrogenic aortic injury at T5, in which the thoracic pedicle screw penetrated the descending aortic wall without a hemodynamically unstable condition. The endovascular treatment was successfully conducted in association with simultaneous implant removal without any consequences. Papin et al. [7] reported a case of spinal cord complication associated with the thoracic pedicle screw in posterior scoliosis surgery. In this case, the medially perforated screw caused persistent abdominal pain and tremors in the legs, requiring removal after 6 months and thus proving that the pedicle screw could be dangerous for deformed spines.
At present, various techniques are being used to insert the thoracic pedicle screw in scoliosis, including the free hand technique, intraoperative C-arm image intensifier, direct visualization of the medial wall after laminotomy, 3D fluoroscopy, and CT-based computer-assisted navigational systems. Some surgeons opt for intraoperative fluoroscopic guidance. This requires the fluoroscope tube to be tilted and rotated to obtain an axial view of the concerned pedicle. It may even be impossible in a few cases where the pedicle may be severely deformed. Image-guided techniques result in the use of expensive equipment and prolonged operating time, as well as radiation exposure to both the surgical personnel and the patient. Another important factor during the operation was the inaccuracy of the fluoroscopic lateral spine images. The significant vertebral tilt in scoliosis disturbed the clear visualization of lateral vertebral images, causing possible misdirection of screws in the cephalad and caudal directions.
The use of computer-assisted navigation has emerged in an attempt to obviate the chance of pedicle screw malpositioning in difficult deformity correction surgeries. Rajasekaran et al. [35] compared the accuracy of non-navigation and Iso-C-based navigation in pedicle screw fixation in thoracic spine deformities. They reported that there were 54 (23%) pedicle breaches in the non-navigation group compared with only 5 (2%) in the navigation group. Iso-C navigation increases accuracy and reduces surgical time and radiation in thoracic deformity correction surgeries. Amiot and Poulin [1] analyzed and compared the results of CT-based navigation-guided thoracic, lumbar, and sacral pedicle screws with those of the control group treated surgically with conventional techniques. The historical controls had no pedicle screws placed in the upper thoracic spine. Post-operative screw placement was measured using MRI in both study groups. They found that computer navigation could significantly reduce the incidence of incorrectly positioned pedicle screws. The time required to insert the pedicle screws was significantly shorter in the navigation group as compared to the non-navigation group. Computer-assisted navigation surgery is superior to the use of the fluoroscopic technique alone in thoracic deformity correction surgeries using pedicle screw instrumentation as it reduces radiation exposure and pedicle perforations, and it increases accuracy. However, the increased set-up time and registration-related errors are the drawbacks of CT-based navigation systems, which rely on acquired data before surgery. The change in intervertebral anatomic relationship in unstable situations was also reported with navigation systems using pre-operative CT scans. In navigation, the surgeon can be away from the operating field while screening the spine using a surgical fluoroscope; this increases surgical time as well as the risk of infection.
The use of drill templates was initially demonstrated in hip and knee surgeries [34]. Several studies have also described their use in spine surgeries including the cervical spine [13, 32]. Berry et al. [4] used a three V-shaped knife design to support the drill template. Goffin et al. [13] designed a template with clamps to interface with the posterior course of the cervical vertebra. More recently, Owen et al. [32] introduced a drill template which was designed to match the posterior surface of the cervical vertebra around the entry point, providing a greater contact area with the vertebra and thus offering better stability. Compared with other template designs, this study successfully introduced a novel, custom-fit navigational template for the placement of pedicle screws in the scoliosis thoracic spine and further validated the technique in a clinical setting by applying it to 16 patients requiring cervical pedicle screw insertion. The clinical application of this technique demonstrated its high accuracy. A pre-operative CT scan was also obtained in this study to customize the placement of each screw based on the unique morphology of the patient’s thoracic vertebra. The use of a high-resolution CT scanner and advanced technologies facilitated the high geometric accuracy of the drill template. The Mimics software used in this study to reconstruct the 3-D model of the vertebra from the CT scan data provided fast, easy, and powerful 3D image processing and editing. Moreover, rapid prototyping technology, which is based on building the model by stacking thin layers, was also used. Rapid prototyping can reproduce more complex designs due to its high accuracy and versatility. The resolution of the rapid prototyping machine is well above the 0.35 mm resolution of the template model and thus the accuracy of reproduction is not a limiting factor.
There are several advantages in using a patient-specific drill template design. First, the surgeon can decide on the location, orientation, and size of each screw based on the unique morphology of the deformed thoracic vertebra even before going to the operating table. The observations in this study have demonstrated that the pedicle may differ widely from patient to patient. Therefore, pre-operative CT evaluation is suggested as a mandatory step for precise planning of the surgical procedure. The diameter of the screw should be appropriately selected for the individual pedicle. The use of patient-specific drill templates has helped us in the successful handling of even abnormal cases by helping us choose the right screws and decide on the best orientation of the screw insertion for each pedicle. Second, the technique is simple to use because it does not require much expertise on the surgeon’s part, and the pre-operatively prepared drill template can be used intra-operatively to assist in the surgical navigation and precise placement of the instrumentation. Third, in contrast to the image-guided technique, the use of a patient-specific drill template design eliminates the need for complex equipment and time-consuming procedures in the operation, thereby reducing the duration of the surgical procedure. Fourth, the accuracy of screw placement can be accomplished without perforating the spinal canal or the blood vessels. In abnormal cases with very narrow pedicles, this technique also allows for flexibility to examine the accuracy of the drill templates by inserting the screws into the biomodel of the vertebra. Thus, the technique has a potential role to play in scoliosis surgery where the radiographic landmarks can look distorted and obscured. Finally, the need for fluoroscopy during screw insertion is eliminated, which considerably reduces the radiation exposure to the members of the surgical team.
However, there are also some potential sources of errors for this technique. First, it requires clean preparation of the bone surface, including thorough removal of the attached muscle and fat tissue without causing damage to the bony surface structure to ensure proper fit of the drill template on the lamina. Second, in the clinical setting, a template should be capable of being used as an in situ drill guide, and any movement between the bone and the template due to vibration while drilling will greatly affect accuracy. Therefore, the template has to be firmly placed in position by the surgeon while drilling.
Nevertheless, the template design is unique in that it is created based on computer-assisted design and thus can match the postural surface of the thoracic vertebra perfectly. After the preparation of the bone surface with thorough removal of the attached muscle and fat tissue without damaging the bony surface structure, all our templates can be easily and securely held in place by the surgeon’s free hand. The drill template can avoid registration-related errors and shorten the surgical time. As proof of its effectiveness, there have been increasing reports on the simplicity of navigated spine surgery owing to the use of the patient-specific drill template design.
This study has introduced a novel navigational template for use in scoliosis thoracic pedicle screw placement and has clinically validated its viability in 16 patients. The preliminary clinical trials have demonstrated that this design can improve the accuracy and safety of pedicle screw placement in the deformed spine. With its wide applicability, high accuracy, and cost-effectiveness, this design is expected to enjoy widespread use in the future.
References
Amiot LP, Poulin F (2004) Computed tomography-based navigation for hip, knee, and spine surgery. Clin Orthop Relat Res 421:77–86
Belmont PJ, Klemme WR, Dhawan A et al (2001) In vivo accuracy of thoracic pedicle screws. Spine 26:2340–2346
Belmont PJ Jr, Klemme WR, Robinson M et al (2002) Accuracy of thoracic pedicle screws in patients with and without coronal plane spinal deformities. Spine 27:1558–1566
Berry E, Cuppone M, Porada S et al (2005) Personalised image-based templates for intra-operative guidance. Proc Inst Mech Eng H 219:111–118
Bridwell KH, Lenke LG, Baldus C et al (1998) Major intraoperative neurologic deficits in pediatric and adult spinal deformity patients: incidence and etiology at one institution. Spine 23:324–331
Catan H, Buluc L, Anik Y et al (2007) Pedicle morphology of the thoracic spine in preadolescent idiopathic scoliosis: magnetic resonance supported analysis. Eur Spine J 16:1203–1208
Clin J, Aubin CÉ, Lalonde N et al (2011) A new method to include the gravitational forces in a finite element model of the scoliotic spine. Med Biol Eng Comput 49:967–977
Di Silvestre M, Parisini P, Lolli F et al (2007) Complications of thoracic pedicle screws in scoliosis treatment. Spine 32:1655–1661
Driscoll M, Aubin CE, Moreau A et al (2011) Biomechanical comparison of fusionless growth modulation corrective techniques in pediatric scoliosis. Med Biol Eng Comput 49(12):1437–1445
Foley KT, Simon DA, Rampersaud YA (2001) Virtual fluoroscopy: computer assisted fluoroscopic navigation. Spine 26:347–351
Gertzbein SD, Robbins SE (1990) Accuracy of pedicle screw placement in vivo. Spine 15:11–15
Gilbert TJ Jr, Winter RB (2005) Pedicle anatomy in a patient with severe early-onset scoliosis: can pedicle screws be safely inserted? J Spinal Disord Tech 18:360–363
Goffin J, Van Brussel K, Martens K et al (2001) Three-dimensional computed tomography-based, personalized drill guide for posterior cervical stabilization at C1-C2. Spine 26:1343–1347
Hamill C, Lenke L, Bridwell K et al (1996) The use of pedicle screw fixation to improve correction in the lumbar spine patients with idiopathic scoliosis: is it warranted? Spine 21:1241–1249
Hott JS, Theodore N, Klopfenstein JD et al (2004) Image guidance in spinal surgery for trauma: Iso-C 3D. Oper Tech Neurosurg 7:42–47
Kim KD, Patrick Johnson J, Bloch BSO et al (2001) Computer-assisted thoracic pedicle screw placement: an in vitro feasibility study. Spine 26:360–364
Kim YJ, Lenke LG, Bridwell KH et al (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29:333–342
Kim YJ, Lenke LG, Bridwell KH et al (2004) Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 29:333–342
Kuklo TR, Lenke LG, O’Brien MF et al (2005) Accuracy and efficacy of thoracic pedicle screws in curve more than 90°. Spine 20:222–226
Lijenqvist UR, Link TM, Halm FH (2000) Morphometric analysis of thoracic and lumbar vertebrae in idiopathic scoliosis. Spine 25:1247–1253
Liljenqvist UR, Halm HF, Link TM (1997) Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine 19:2239–2245
Liljenqvist UR, Lepsien U, Hackeberg L et al (2002) Comparative analysis of pedicle idiopathic thoracic scoliosis. Eur Spine J 11:336–343
Lonner BS, Auerbach JD, Estreicher MB et al (2009) Thoracic pedicle screw instrumentation: the learning curve and evolution in technique in the treatment of adolescent idiopathic scoliosis. Spine 34:2158–2164
Lonstein JE, Denis F, Perra JH et al (1999) Complications associated with pedicle screws. J Bone Joint Surg Am 81:1519–1528
Lu S, Xu YQ, Zhang YZ et al (2009) A novel computer-assisted drill guide template for lumbar pedicle screw placement: a cadaveric and clinical study. Int J Med Robot Comput Assist Surg 5:184–191
Lu S, Xu YQ, Zhang YZ et al (2009) A novel computer-assisted drill guide template for placement of C2 laminar screws. Eur Spine J 18:1379–1385
Lu S, Xu YQ, Lu WW et al (2009) A novel patient-specific navigational template for cervical pedicle screw placement. Spine 34:E959–E964
Minor ME, Morrissey NJ, Peress R et al (2004) Endovascular treatment of an iatrogenic thoracic aortic injury after spinal instrumentation: case report. J Vasc Surg 39:893–896
Nolte LP, Beutler T (2004) Basic principles of CAOS. Injury 35:S–A6–16
O’Brien MF, Lenke LG, Mardjetko S et al (2000) Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine 25:2285–2293
O’Brien MF, Lenke LG, Mardjetko S et al (2000) Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine 25:228–293
Owen BD, Christensen GE, Reinhardt JM et al (2007) Rapid prototype patient-specific drill template for cervical pedicle screw placement. Comput Aided Surg 12:303–308
Parent S, Labelle H, Skalli W et al (2004) Thoracic pedicle morphometry in vertebrae from scoliotic spines. Spine 29:239–248
Radermacher K, Portheine F, Anton M et al (1998) Computer assisted orthopaedic surgery with image based individual templates. Clin Orthop Relat Res 354:28–38
Rajasekaran S, Vidyadhara S, Ramesh P et al (2007) Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine 32:E56–E64
Sarlak AY, Tosun B, Atmaca H et al (2009) Evaluation of thoracic pedicle screw placement in adolescent idiopathic scoliosis. Eur Spine J 18:1892–1897
Smith RM, Pool RD, Butt WP et al (1991) The transverse plane deformity of structural scoliosis. Spine 16:1126–1129
Smorgick Y, Millgram MA, Anekstein Y et al (2005) Accuracy and safety of thoracic pedicle screw placement in spinal deformities. J Spinal Disord Tech 18:522–526
Suk SI, Lee CK, Kim WJ et al (1995) Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 20:1399–1405
Suk S, Kim WJ, Lee SM et al (2001) Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine 26:2049–2057
Suk SI, Lee SM, Chung ER et al (2003) Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine 28:484–491
West JL, Ogilvie JW, Bradford DS (1991) Complications of the variable screw plate pedicle screw fixation. Spine 16:576–579
Wu H, Ronsky JL, Cheriet F et al (2010) Prediction of scoliosis progression with serial three-dimensional spinal curves and the artificial progression surface technique. Med Biol Eng Comput 48:1065–1075
Acknowledgments
The authors would like to thank Dr. You-hua Cheng for his assistance with the CT data collection. This work was supported by Yunnan Natural Science Foundation (2010ZC183 and 2011CA015).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lu, S., Zhang, Y.Z., Wang, Z. et al. Accuracy and efficacy of thoracic pedicle screws in scoliosis with patient-specific drill template. Med Biol Eng Comput 50, 751–758 (2012). https://doi.org/10.1007/s11517-012-0900-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-012-0900-1