Abstract
Background
Measuring Hounsfield units (HUs) from computed tomography (CT) scans has recently been proposed as a tool for assessing vertebral bone quality, as it has been associated with bone mineral density, compressive strength, and fracture risk. Vertebral bone quality is believed to be an important determinant of outcome and complication rates following spine surgery and potentially influences success of interbody spinal fusion.
Questions/Purposes
The purpose of this study was to investigate the association between HU on CT scans and fusion success in patients with lateral transpsoas surgery for lumbar interbody fusion (LIF).
Methods
The CT scans of 28 patients with a combined 52 levels of stand-alone LIF were evaluated at a minimum of 12 weeks postoperatively. Coronal and sagittal images were evaluated for evidence of fusion, and HU values were collected from axial images. HU measurements were also taken from vertebral bodies proximal to the construct to evaluate global bone quality.
Results
Of the 52 LIF levels, 73% were assessed as fused and 27% were nonunited at the time of evaluation. The successful fusion levels had significantly higher HU measurements than the nonunion levels (203.3 vs. 139.8, p < 0.001). Patients with successful fusion constructs also had higher global bone density when vertebral bodies proximal to the construct were compared (133.7 vs. 107.3, p < 0.05).
Conclusion
With the aging population and increasing prevalence of osteoporosis, preoperative assessment of bone quality prior to spinal fusion deserves special consideration. We found that a successful lumbar fusion was associated with patients with higher bone density, as assessed with HU, both globally and within the fusion construct, as compared to patients with CT evidence of nonunion.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Due to its minimally invasive approach and other proposed advantages, lateral transpsoas surgery for lumbar interbody fusion (LIF) has been gaining popularity in recent years. Results from preliminary reports were encouraging [11, 17], and a growing body of literature on LIF suggests that the technique is safe and effective for achieving lumbar interbody fusion [12, 14]. Among the advantages associated with minimally invasive LIF are its ability to restore disc height and indirectly decompress the neural elements [10], preserve anterior and posterior stabilizing elements, and avoid morbidities [14] associated with other approaches [6, 13]. LIF has successfully been used in an aging spine surgical population, both in a stand-alone fashion as well as with supplemental posterior instrumentation [15].
Since its approval for use in anterior lumbar interbody fusion (ALIF) procedures, recombinant human bone morphogenetic protein-2 (BMP-2; Infuse, Medtronic, Minneapolis, MN) has been used as a biologic adjunct to promote successful fusion in on- and off-label settings, including stand-alone lumbar interbody fusion [1]. Recently, concerns have arisen regarding the safety of BMP-2 as a bone graft substitute in spinal fusion [2], and it has been suggested that an inflammatory response to BMP-2 used in patients with markedly decreased bone health may even contribute to subsidence [9], especially with end plate violation in the course of surgery [18]. Regardless of the graft material used in stand-alone interbody fusion, bone health remains an important determinant of outcome and complication rates [19] and potentially influences fusion success [4].
As such, assessment of bone health in spine surgery patients is an important part of perioperative evaluation, and we suggest that reduced bone mineral density (BMD) deserves special consideration in patient selection, preoperative planning, patient counseling, as well as postoperative management. There is a paucity of data assessing the influence of altered BMD on fusion success in spine surgery. No prior study has been reported on reduced bone density, as assessed by Hounsfield unit (HU) measurement on computed tomography (CT) scans [16], as a possible risk factor for nonunion following stand-alone lumbar interbody fusion. The effect of BMP-2 on HU measurement-derived BMD also remains to be elucidated. Specifically, we aim to document whether there is an association between successful fusion and the patients spinal BMD as measured by quantitative CT and whether or not an additional effect can be documented when BMP-2 is used as an adjunct to promote fusion.
Materials and Methods
Following institutional review board approval, the electronic medical records, radiographs, and CT scans of 28 patients who underwent stand-alone LIF (XLIF, NuVasive, San Diego, CA) at a single institution in a 3-year time period (2008–2010) were reviewed. Preoperative diagnoses included degenerative disc disease, scoliosis, anterior and lateral spondylolisthesis, radiculopathy, and foraminal stenosis. These patients had a combined total of 52 fusion levels. Patient characteristics including age, gender, BMI, fusion level, and available DXA results were recorded (Table 1). Patients with previous spinal instrumentation were excluded as associated artifacts on CT scans affect HU measurements. A minimum of 12 weeks between the LIF surgery and the postoperative CT scan was required for inclusion in the study. A fellowship-trained spine surgeon blinded to HU results assessed all fusions. A successful fusion level was defined as having bridging on both coronal and sagittal reformatted CT images. A successful fusion construct had bridging at all involved levels.
Noncontrast CT scan of the spine was performed with a 16-MDCT scanner (MX8000 Philips Healthcare, Andover, MA). HU analysis was performed via a previously described technique using Philips EasyVision Picture Archiving and Communication System (PACS) [16]. This protocol records HU on axial images at three levels within the vertebral body: immediately caudal to the superior end plate, mid-body, and cranial to the inferior end plate (Fig. 1). This technique has been shown to have high reproducibility and correlates with both dual X-ray absorptiometry (DXA)-assessed BMD and compressive strength in an osseous model [16]. Automatic exposure control (AEC) was utilized to obtain quantitative CT assessment without requiring phantoms. AEC uses real-time detector feedback and information from the scout view to adjust exposure time and tube current based on tissue density and patient body habitus. This results in a more homogeneous energy spectrum and increased accuracy of targeted tissue HU readings. A fusion-level HU value was the mean attenuation of cranial and caudal vertebral bodies immediately adjacent to the polyether ether ketone (PEEK) cage. The vertebral bodies, one and two levels cranial to each construct, were also evaluated to assess global HU (Fig. 1).
Technique of obtaining Hounsfield units (HU) values is demonstrated. a A successful lateral lumbar interbody fusion construct is shown to the left. Bridging bone is seen between L4 and L5 on both coronal and sagittal CT images (a (1, 2)). HU readings were made just caudal to the superior end plate, mid-body, and just cranial to the inferior end plate (a (3–5)). The mean of the three readings produced the vertebral body HU score. The mean of L4 and L5 was used to assess the construct bone density. Also apparent is the lack of artifact produced by the interbody PEEK cage. The bone density is visibly increased with higher HU values. b A nonunion patient showing a lack of bridging bone between L4 and L5 is shown to the right. Lower HU values both proximal to and within the construct are observed, and the subsidence of the PEEK cage is apparent. Axial images (b (3–5)) show radiographic signs of osteoporosis including lower attenuation, decreased trabecular density, and apparent cortical thinning.
Statistical analysis was performed using an independent samples Student's t test for continuous variables and Fisher exact test for categorical data, both with two-tailed hypothesis testing. p values equal to or below 0.05 were considered statistically significant.
Results
The average construct was 1.9 levels per patient for a total of 52 levels. Ten patients had single level constructs, 12 had two-level constructs, and 6 patients had three-level constructs. Of the total constructs, a nonunion was present in at least one level in nine patients, and 19 had successful fusion at all levels. Thirty-eight of all included levels were assessed as fused (73.1%), and nonunion was seen in the remaining 14 (26.9%). There were no statistically significant differences between the groups in age, BMI, off-label BMP-2 use, or fusion level. While it is not significant, there was a trend towards female gender and lower BMD (T scores) in the nonunion group. Additionally, there was no difference in average time between the LIF procedure and the date of the CT study between the fused and nonunion groups (226.5 vs. 241.0 days, respectively, p = 0.71) (Table 1).
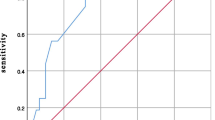
Successful fusion was associated with higher BMD as measured by quantitative CT (p = 0.0009). When fusion levels were individually assessed, the mean results from HU measurement were 203.3 ± 61.4 (95% confidence interval (CI) 183.1–223.5) for the successful fusion levels and 139.8 ± 42.7 (95% CI 115.2–164.5) for the nonunion levels (p = 0.0009) (Fig. 2).
When the complete constructs were assessed for fusion success, HU values were significantly higher within the construct as compared to proximal vertebral bodies both in the 19 patients with complete fusions (200.4 vs. 133.7, p = 0.00001) and in the 9 patients with at least one level of nonunion (142.3 vs. 107.3, p = 0.01) (Fig. 3). As a marker of global bone quality outside of the construct, the successful fusion group had a significantly higher HU in proximal vertebrae (133.7 vs. 107.3, p = 0.048).
Hounsfield units measurements (with standard error bars) of vertebral bodies proximal to the fusion construct compared with HU values within the construct. Both the fusion and nonunion groups showed significantly higher HU values within the BMP-2-augmented LIF construct as compared to proximal levels (p < 0.0001 and p < 0.01, respectively). The global BMD, as assessed by proximal vertebrae HU, was higher in patients with a fused construct as compared to those with a nonunited construct (p < 0.05).
Discussion
In the present study, we utilized a quantitative CT analysis to assess regional bone density following lumbar spine fusion and showed that patients with a successful fusion had higher HU measurements both at the fused levels and throughout the adjacent spine as compared to nonunion controls. We also demonstrate an effect of BMP-2 on increasing local BMD. These data suggest that when a preoperative spinal or abdominal CT scan is available in patients undergoing spinal fusion, HU value measurements may be used to assess BMD and possibly prognosticate fusion success.
There are several limitations to this study. The retrospective nature resulted in a very limited number of preoperative CT scans, so while correlative HU data suggest an association with fusion success, we cannot definitively claim causative effects of BMD on fusion. We also cannot exclude the possibility that a successful fusion results in local bone changes that would increase density measurements. While it is possible that increased HU is a marker for higher quality bone that facilitates fusion, it is also possible that the elevated HU values were the result of an increased response to BMP-2. However, the successful fusion group also showed globally higher HU values when vertebral bodies proximal to the construct were evaluated. Another limitation is that a single postoperative CT scan was evaluated and that this was not standardized throughout the patient cohort. It is possible that some of the patients with a nonunion at a mean of 241 days eventually went on to a successful fusion. If so, HU may be a more accurate prognosticator of time to fusion rather than overall fusion rate.
Further exploration of the association between bone mineral density and successful spinal fusion outcomes deserved attention. Osteoporosis is an increasingly prevalent disease, with recent estimations of 10 million individuals affected and 41 million at risk in the USA [7]. In patients undergoing spine surgery, over half of all females and one in six males are osteoporotic on DXA by the World Health Organization definitions [3]. Unfortunately, a recent survey of spine surgeons revealed that only 22% obtained DXA and 11% checked metabolic laboratories prior to noninstrumented fusion [5].
HU was recently shown to correlate with BMD on DXA scans as well as compressive strength based on osseous models [16]. A subsequent study showed that HU was significantly lower both at the fracture level and, globally, in patients with adjacent segment fractures following spinal fusion as compared with matched controls [8]. When CT scans are available, HU assessments can easily be obtained by the practitioner to provide additional information on global and regional bone density with minimal effort and no additional cost. The far-reaching implications of HU quantification include bone quality assessment, fracture risk, and possibly the capacity to develop a successful spinal fusion. It could also be utilized to suggest metabolic bone disease, the need for further imaging or laboratory assessments, and the necessity for initiating pharmacologic treatment. Other advantages include the fact that it can be obtained throughout the entire spine, where DXA standards have not been defined.
The HU reported here is consistent with previously published normative values [16]. When stratified by success of fusion, the HU values proximal to the construct in the nonunion patients (107.3) were consistent with osteopenia (95% CI range 93.1–108.8), while the values in patients with a successful fusion (133.7) were in the normal range (95% CI range 118.4–147.5) [16]. This data, along with the increased preoperative T scores in the successful fusion group (−0.54 vs. −1.55), suggest that patients with higher BMD may have an increased likelihood of fusion following LIF.
It was previously shown that HU values are typically consistent through all levels of the lumbar spine [16]. However, in this study, both the fusion and nonunion groups had significantly higher HU in the LIF construct as compared to proximal levels (Fig. 3). While preoperative HU values are unknown, we believe that this is likely secondary to the high percentage of patients receiving BMP-2 to augment fusion and its effect on local bone density.
Stand-alone LIF provides a unique opportunity for evaluating postoperative fusion and HU values on the same CT scan images. Posterior instrumentation or the use of pedicle screws results in artifact that modifies beam attenuation and produces significant increases in HU measurements. The use of PEEK cages in isolation does not appear to produce these changes (Fig. 1) and so allows accurate HU measurements and fusion evaluation on the same study. Our stand-alone fusion rate of 71% at a mean of 230 days is similar to that of a previous investigation by Sharma et al., who reported a stand-alone fusion rate of 75% at 1 year and an overall fusion rate of 94% [17].
In summary, we showed that in patients with a successful fusion following stand-alone LIF, the vertebral bodies within the construct had significantly higher bone mineral density, as assessed with HU, as compared to patients with CT evidence of nonunion. Additionally, the patients with a successful fusion had higher global bone density when HU measurements of proximal vertebrae were evaluated. Future prospective evaluations are certainly indicated to explore the effect of bone quality on fusion rates, and the ability of HU to prognosticate successful surgical outcomes.
References
Burkus JK, Gornet MF, Schuler TC, Kleeman TJ, Zdeblick TA. Six-year outcomes of anterior lumbar interbody arthrodesis with use of interbody fusion cages and recombinant human bone morphogenetic protein-2. The Journal of Bone and Joint Surgery, American Volume. 2009; 91(5): 1181-1189.
Carragee EJ, Hurwitz EL, Weiner BK. A critical review of recombinant human bone morphogenetic protein-2 trials in spinal surgery: emerging safety concerns and lessons learned. The Spine Journal: official journal of the North American Spine Society. 2011; 11(6): 471-491.
Chin DK, Park JY, Yoon YS, et al. Prevalence of osteoporosis in patients requiring spine surgery: incidence and significance of osteoporosis in spine disease. Osteoporosis International: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2007; 18(9): 1219-1224.
DeWald CJ, Stanley T. Instrumentation-related complications of multilevel fusions for adult spinal deformity patients over age 65: surgical considerations and treatment options in patients with poor bone quality. Spine. 2006; 31(19 Suppl): S144-151.
Dipaola CP, Bible JE, Biswas D, Dipaola M, Grauer JN, Rechtine GR. Survey of spine surgeons on attitudes regarding osteoporosis and osteomalacia screening and treatment for fractures, fusion surgery, and pseudoarthrosis. The Spine Journal: official journal of the North American Spine Society. 2009; 9(7): 537-544.
Fantini GA, Pappou IP, Girardi FP, Sandhu HS, Cammisa FP Jr. Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine. 2007; 32(24): 2751-2758.
Hart RA, Prendergast MA. Spine surgery for lumbar degenerative disease in elderly and osteoporotic patients. Instructional Course Lectures. 2007; 56: 257-272.
Meredith DS, Schreiber JJ, Taher F, Cammisa FP Jr, Girardi FP. Lower Preoperative Hounsfield Unit Measurements are Associated With Adjacent Segment Fracture Following Spinal Fusion. Spine. 2012; 38(5): 415-418.
Mroz TE, Wang JC, Hashimoto R, Norvell DC. Complications related to osteobiologics use in spine surgery: a systematic review. Spine. 2010; 35(9 Suppl): S86-104.
Oliveira L, Marchi L, Coutinho E, Pimenta L. A radiographic assessment of the ability of the extreme lateral interbody fusion procedure to indirectly decompress the neural elements. Spine. 2010; 35(26 Suppl): S331-337.
Ozgur BM, Aryan HE, Pimenta L, Taylor WR. Extreme Lateral Interbody Fusion (XLIF): a novel surgical technique for anterior lumbar interbody fusion. The Spine Journal: official journal of the North American Spine Society. 2006; 6(4): 435-443.
Pumberger M, Hughes AP, Huang RR, Sama AA, Cammisa FP, Girardi FP. Neurologic deficit following lateral lumbar interbody fusion. European Spine Journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society. 2012; 21(6): 1192-1199.
Rajaraman V, Vingan R, Roth P, Heary RF, Conklin L, Jacobs GB. Visceral and vascular complications resulting from anterior lumbar interbody fusion. Journal of Neurosurgery. 1999; 91(1 Suppl): 60-64.
Rodgers WB, Gerber EJ, Patterson J. Intraoperative and early postoperative complications in extreme lateral interbody fusion: an analysis of 600 cases. Spine. 2011; 36(1): 26-32.
Rodgers WB, Gerber EJ, Rodgers JA. Lumbar fusion in octogenarians: the promise of minimally invasive surgery. Spine. 2010; 35(26 Suppl): S355-360.
Schreiber JJ, Anderson PA, Rosas HG, Buchholz AL, Au AG. Hounsfield units for assessing bone mineral density and strength: a tool for osteoporosis management. The Journal of Bone and Joint Surgery, American Volume. 2011; 93(11): 1057-1063.
Sharma AK, Kepler CK, Girardi FP, Cammisa FP, Huang RC, Sama AA. Lateral lumbar interbody fusion: clinical and radiographic outcomes at 1 year: a preliminary report. Journal of Spinal Disorders & Techniques. 2011; 24(4): 242-250.
Smith WD, Huntington CF. Letter to the editor regarding: Dua K, Kepler CK, Huang RC, Marchenko A. Vertebral body fracture after anterolateral instrumentation and interbody fusion in two osteoporotic patients. Spine J 2010;10:e11-5. The Spine Journal: official journal of the North American Spine Society. 2011; 11(2): 166-167. author reply 167.
Toyone T, Ozawa T, Kamikawa K, et al. Subsequent vertebral fractures following spinal fusion surgery for degenerative lumbar disease: a mean ten-year follow-up. Spine. 2010; 35(21): 1915-1918.
Disclosures
ᅟ
Conflict of Interest:
Joseph J. Schreiber, MD and Fadi Taher, MD have declared that they have no conflict of interest. Alexander P. Hughes, MD receives personal fees from NuVasive, outside the work. Federico P. Girardi, MD receives personal fees from DePuy Spine, LifeSpine, NuVasive, Ortho Development Corp., Centinel Spine, Healthpoint Capital, Paradigm Spine, Small Bone Innovations, Spinal Kinetics, LANX Spine, SpineArt, Wenzel Spine, LDR Spine, and Ethicon, outside the work.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 [5].
Informed Consent:
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Level of Evidence: Prognostic Study Level III: See Levels of Evidence for a complete description.
Rights and permissions
About this article
Cite this article
Schreiber, J.J., Hughes, A.P., Taher, F. et al. An Association Can Be Found Between Hounsfield Units and Success of Lumbar Spine Fusion. HSS Jrnl 10, 25–29 (2014). https://doi.org/10.1007/s11420-013-9367-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11420-013-9367-3