Abstract
Glial cell activation and oxidative stress are important factors in the induction of opioid side effects such as tolerance and dependence. It has been demonstrated that Satureja khuzistanica extract (SKE) has antioxidative, antinociceptive and anti-inflammatory properties; however, its influences on opioid analgesic tolerance have not yet been clarified. Adult male Wistar rats were rendered analgesic-tolerant by injection of 10 mg/kg morphine twice daily for 8 days. To determine the effect of SKE on the development of morphine tolerance, different doses of SKE (25, 50 and 100 mg/kg i.p.) were injected simultaneously with morphine. The tail-flick test was used to assess the nociceptive threshold. The lumbar spinal cord was assayed to determine glial fibrillary acidic protein (GFAP) and tumor necrosis factor alpha (TNFα) levels by the Western blotting method. Our results showed that chronic morphine produced tolerance to the antinociceptive effect of morphine. However, SKE could prevent, in a dose-dependent manner, morphine tolerance development. In tolerant animals, a significant increase in GFAP and TNFα levels was observed in the lumbar spinal cord, and was reversed to control levels by 100 mg/kg SKE. Our data revealed that Satureja khuzistanica had beneficial effects in preventing opioid tolerance and the underlying mechanisms of those effects may be due, at least in part, to reduce spinal glial cell activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The chronic use of opioids such as morphine leads to antinociceptive tolerance, which limits their serviceable and therapeutic effects. Many mechanisms are involved in the induction of analgesic tolerance development [1].
Within the past 20 years evidence has shown that the immune system can alter neuronal function. The effects of immune/glial cells on pain and opioid action occur on multiple levels [2]. Both glial (microglia and astrocyte) activation and enhanced pro-inflammatory cytokine levels were observed following chronic morphine treatment at the lumbar spinal cord of the rats [3]. In addition, following chronic morphine, a marked glial response, astroglial hypertrophy and increased expression of glial fibrillary acidic protein (GFAP) were observed in the spinal cord, posterior cingulated cortex, and hippocampus [4]. The activation of glial cells and enhanced pro-inflammatory cytokine expression has been implicated in the development of morphine tolerance and morphine-induced hyperalgesia [5]. Surprisingly, inhibition of glial activation or antagonizing the activity of pro-inflammatory cytokines interleukin (IL)-1β, IL-6 and tumor necrosis factor alpha (TNFα) attenuated the development of morphine tolerance and withdrawal-induced hyperalgesia in rats [4, 6].
Recently, the demonstration of anti-addictive, anti-tolerance and antinociceptive properties of natural herbal products has attracted intense interest [7]. However, natural products need precise scientific experimental testing as well as clinical trials before they can be used in the management of opioid side effects.
Satureja khuzistanica Jamzad (Marzeh Khuzestani in Persian, family Lamiaceae) is an endemic plant that is widely distributed in the southern part of Iran. It is famous for its medical uses as analgesic and antiseptic in folk medicine [8]. Amanlou and colleagues [9] confirmed that the anti-inflammatory and antinociceptive properties of Satureja khuzistanica are comparable to those of indomethacin and morphine. Furthermore, this plant has anti-hyperalgesic effects in a rat model of diabetic neuropathy [10]. In Persian traditional medicine satureja is used for treating muscle and neuropathic pain as well as withdrawal-induced pain and related side effects.
Based on the fact that glial activation and oxidative stress occur following chronic usage of opioids and those factors play important roles in the induction of opioid tolerance, and that Satureja khuzistanica has antioxidant, antinociceptive and anti-inflammatory properties, the present study was designed to test the hypothesis that its extract could exert effects on the induction of morphine antinociceptive tolerance and also to determine its possible mechanism in that phenomenon.
Materials and methods
Animals
All experiments were carried out on male Wistar rats, weighing 200–250 g, that were housed under a 12 h light/dark cycle in a room with controlled temperature (22 ± 1 °C) and free access to food and water. Animals were handled daily (between 9:00 and 10:00 AM) for 3 days before the experiment days in order to adapt them to manipulation and minimize nonspecific stress responses. Rats were divided randomly into several experimental groups, each comprising 6–8 animals. All experiments followed the guidelines on ethical standards for investigation of experimental pain in animals [11] and were approved by the Animal Experimentation Ethic Committee of Kerman Neuroscience Research Center (EC/KNRC/91).
Preparation of satureja extract
An ethanolic Satureja khuzistanica extract (SKE) was prepared in Razi Herbal Medicines Research Center (Lorestan, Iran). The healthy leaves were dried in shade conditions, and to avoid decomposition of chemical constituents dried leaves were powdered and stored in clean and dry airtight containers for further studies. A sample was deposited at the herbarium of Razi Herbal Medicines Research Center. Two hundred grams of the air-dried leaves were ground into fine powder. The powder was extracted twice, on each occasion with 1 L of 80 % ethyl alcohol. The collective ethanol extract was filtered, and the filtrate was concentrated to dryness under reduced pressure in a rotary evaporator; the resulting ethanol extract was freeze-dried. Gas chromatography–mass spectroscopy (GC-MS) analysis of the extract showed that carvacrol (78.3 %), 9-octadecenoic acid (13.5 %), hexadecanoic acid (6.7 %), bis(2-ethylhexyl)phthalate (1.0 %) and beta-bisabolene (0.5 %) were the main components of the SKE [10].
Drugs
Aliquot portions of the crude SKE were weighed and dissolved in warm physiological saline for use on each day of our experiments. Morphine hydrochloride (TEMAD, Iran) was also dissolved in physiological saline. SKE was given intragastrically (i.g.) by gavage and morphine was injected intraperitoneally (i.p.). These drugs were given in 1 ml/kg volumes (i.g. and i.p.). Control animals received saline in an equal volume (1 ml/kg).
Antinociceptive test
Antinociception was assessed by the tail-flick test [12]. Radiant heat (power intensity = 7) was focused on 4–7 cm from the tail distal end. The tail-flick latency for each rat was determined three times and the mean was designated as baseline latency before drug injection. The intensity of the beam was adjusted to produce a mean control reaction time between 2 and 4 s. The cut-off time was fixed at 10 s in order to avoid any damage to the tail. The percentage of antinociception was determined with the following formula:
Morphine tolerance
To induce analgesic tolerance, morphine at a daily dose of 20 mg/kg in two equally divided doses was administrated at 8.00 AM and 6.00 PM from day 1 to day 8. SKE or vehicle was given according to the same schedule as control groups. Nociceptive testing was performed both before and 30 min after morphine administration on days 1, 3, 6 and 8 [13, 14]. To determine the effect of satureja on the development of morphine tolerance, SKE (25, 50 and 100 mg/kg i.g.) was injected simultaneously with morphine but on days that nociceptive testing was measured, morphine was injected first and antinociception was measured 30 min after morphine administration and then SKE was given. With such a method, compounds with antinociceptive properties cannot produce a false-positive anti-tolerance effect.
Tissue extraction and preparation
Rats were anesthetized (exposed to a CO2 atmosphere) and decapitated. The spinal column was cut through the pelvic girdle. Hydraulic extrusion was performed by inserting a 16-gauge needle into the sacral vertebral canal and expelling with ice-cold saline. The spinal cord was immediately placed on ice in a glass petri dish, and the dorsal half of the lumbar cord was dissected. Tissue samples were weighed and immediately frozen in liquid nitrogen and stored at −70 °C until assay.
Western blot analysis
The dissected spinal tissues were homogenized in ice-cold buffer containing 10 mM Tris–HCl (pH 7.4), 1 mM EDTA, 0.1 % SDS, 0.1 % Na-deoxycholate, 1 % NP-40 with protease inhibitors (1 mM phenylmethylsulfonyl fluoride, 2.5 μg/ml leupeptin, 10 μg/ml aprotinin) and 1 mM sodium orthovanadate. The homogenate was centrifuged at 14,000 g for 15 min at 4 °C. The resulting supernatant was retained as the whole cell fraction. Equal amounts of protein were electrophoresed on 9 % SDS-PAGE gel and transferred to nitrocellulose membranes (Hybond ECL, GE Healthcare Bio-Sciences Corporation, NJ, USA). After blocking (overnight at 4 °C) with 5 % non-fat dried milk in Tris-buffered saline with Tween 20 (blocking buffer, TBS-T, 150 mM NaCl, 20 mM Tris–HCl, pH 7.5, 0.1 % Tween 20), the membranes were probed with primary antibodies (1:1000 GFAP and TNFα, Santa Cruz Biotechnology, USA) for 2 h at room temperature. After washing in TBS-T (three times for 5 min), the blots were incubated for 60 min at room temperature with a horseradish peroxidase-conjugated secondary antibody (1:15000, Santa Cruz Biotechnology). All antibodies were diluted in blocking buffer. The antibody–antigen complexes were detected using the ECL system and exposed to Lumi-Film chemiluminescent detection film (Roche, Germany). LabWorks software (UVP, UK) was used to analyze the intensity of the expression. β-Actin immunoblotting (antibody from Cell Signaling Technology, Inc., Beverly, MA, USA; 1:1000) was used to control for loading.
Statistical analysis
The results are expressed as mean ± SEM. The difference in % MPE (antinociception) between groups over the time course of study was determined by two- or one-way analysis of variance (ANOVA) followed by the Newman–Keuls test. The values of protein band density obtained from gel analysis and band densitometry were calculated. These values were expressed as GFAP or TNFα subunit/β-actin ratio for each sample. The averages for different groups were compared using ANOVA followed by the Newman–Keuls test. P < 0.05 was considered significant.
Results
Effect of SKE on development of tolerance to analgesic effect of morphine.
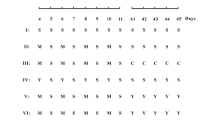
As shown in Fig. 1, chronic administration of 10 mg/kg morphine (twice daily for 8 days), induced a significant decrease in its analgesic effect (tolerance). Simultaneous treatment with morphine and SKE in doses of 50 and 100 mg/kg could significantly prevent the development of tolerance to the analgesic effect of morphine. 25 mg/kg of SKE had a moderate anti-tolerance effect. However, vehicle treatment (saline) had no anti-tolerance effect (data not shown).
The effect of different doses (25, 50 and 100 mg/kg, i.g.) of Satureja khuzestanica extract (SKE) on the development of tolerance to the analgesic effect of morphine (Mor) in rats. Values represent mean ± SEM (n = 6–8). *P < 0.05, ***P < 0.001 significantly different versus antinociception values on the first day in the same group. + P < 0.01, +++ P < 0.001 significantly different versus morphine-injected rats at the same time
As shown in Fig. 2, on day 8 of the experiment, the analgesic effect of 10 mg/kg morphine in animals that received different doses of SKE plus morphine was significantly greater than that of chronic morphine-injected rats.
The antinociceptive effect of 10 mg/kg (i.p.) morphine (Mor) on day 8 in groups that received morphine (10 mg/kg twice daily, i.p.) and morphine concurrently with 50 and 100 mg/kg SKE (i.g.) for 7 days. Each bar represents mean ± SEM (n = 6–8). ***P < 0.001 significantly different versus control saline-treated group (Cont). +++ P < 0.001 significantly different versus morphine-treated animals
Effect of morphine and morphine plus SKE on levels of GFAP and TNFα.
Immunoblotting data revealed that chronic morphine resulted in elevation of GFAP in the dorsal portion of rat lumbar spinal cord. Administration of an effective anti-tolerance dose of SKE (100 mg/kg i.g.) prevented chronic morphine-induced GFAP activation (Fig. 3).
The levels of GFAP in dorsal portion of lumbar spinal cord in control, chronic morphine-treated (10 mg/kg, i.p.) and morphine + SKE (10 mg/kg, i.p. + 100 mg/kg, i.g.) treated rats. Each value in the graph represents the mean ± SEM band density ratio for each group (n = 5–6). β-Actin was used as an internal control. **P < 0.01 significantly different versus control group (Cont). + P<0.05 significantly different versus morphine-treated group (Mor)
In addition, under morphine-tolerant conditions an increase in TNFα protein levels was induced. The increased TNFα level was reversed in the rats that received morphine plus 100 mg/kg SKE (Fig. 4).
Western blot analysis of TNFα in dorsal portion of lumbar spinal cord of animals that received morphine (10 mg/kg, i.p.) alone and morphine concurrently with 100 mg/kg SKE (i.g.) for 7 days. Each value in the graph represents the mean ± SEM band density ratio for each group (n = 5–6). ***P < 0.001 compared to control animals (Cont); + P < 0.05 compared to morphine-treated group (Mor)
Discussion
In the present study, chronic morphine injection induced significant increases in the spinal levels of GFAP and TNFα which were accompanied by a dramatic decrease in morphine analgesia. SKE (100 mg/kg i.g.) not only attenuated the morphine-induced GFAP and TNFα expression but also prevented the induction of tolerance to the antinociceptive effect of morphine.
The underlying mechanisms involved in the induction of opioid tolerance are a very complex issue. They include modulation of intracellular adenylyl cyclase and cyclic adenosine monophosphate-dependent protein kinase A, G protein uncoupling, increased binding of β-arrestin to opioid receptors, and μ-opioid receptor internalization [15]. In addition, activation of N-methyl-d-aspartate receptor, downregulation of glutamate transporters, upregulation of L-type calcium channels, and glial cell activation with increasing pro-inflammatory cytokine expression and apoptosis have also been observed in tolerance situations [16–19].
Glial cell activation and increased cytokine (TNFα, IL-1β, and IL-6) expression have important roles in the pathogenesis of morphine tolerance and suppression of such events could be helpful in the prevention of analgesic tolerance [20, 21].
It is well known that Satureja khuzestanica has a potent anti-inflammatory effect in an animal model of inflammatory pain [9]. The results of this study demonstrated that SKE attenuates morphine-induced elevation in TNFα level. The increase in TNFα expression in the spinal cord of morphine-treated rats contributed to cytokine-mediated neuroinflammation and the subsequent neuronal plasticity [22]. Therefore, it seems that the attenuation of morphine-induced TNFα over-expression by SKE is a possible mechanism for its anti-tolerance effect.
Glial fibrillary acidic protein is expressed in the central nervous system in astrocyte cells and is involved in many important processes. Previous evidence demonstrated that increased expression of GFAP is observed in the central nervous system of chronic morphine-treated animals and this phenomenon plays a fundamental role in the development of opioid complications and side effects, i.e., tolerance and dependence [4]. It has been shown that glia have a central role in the development of morphine tolerance and that administration of a glial modulating agent attenuated tolerance formation [23].
Recently, Jin and colleagues [24] showed that LXA4ME, a lipoxin A4 analogue, attenuates morphine analgesic tolerance and inhibits the activation of microglia and astrocytes through the reduction of pro-inflammatory cytokines (IL-1β, IL-6, and TNFα) at the lumbar spinal cord. Furthermore, it has been reported that inhibition of ceramide biosynthesis with various pharmacological inhibitors significantly blocks the development of morphine antinociceptive tolerance through attenuation of spinal glial activation, IL-1β, IL-6, and TNFα [25].
It is well known that such pro-inflammatory cytokines can enhance excitatory synaptic transmission and potentiate NMDA- and AMPA-induced currents in the spinal cord [26]. In addition, the activation of AMPA and/or NMDA receptor is correlated with morphine tolerance and hyperalgesia [27].
Previous reports indicated that free radicals play important roles in the development of opioid analgesic tolerance and radical scavenging agents could be potential tools in the prevention of morphine tolerance [28, 29].
High antioxidant activity of Satureja khuzestanica has been demonstrated in numerous reports. Abdollahi and colleagues [30] showed that satureja efficiently decreases the normal blood lipid peroxidation level and increases total antioxidant power in rats. It has been shown that 60 days’ treatment of diabetic type-2 patients with Satureja khuzestanica significantly decreases serum lipids and increases total antioxidant power [31]. Rezvanfar and colleagues [32] reported that satureja protects the rat reproductive system from cyclophosphamide-induced toxicity through its antioxidant potential and androgenic activity. Therefore, it seems that the antioxidant property of satureja can be, at least in part, responsible for such an inhibiting response (anti-tolerance) in this study. However, this possible mechanism needs to be clarified by further complementary investigation.
However, for evaluating the pharmacological effects of natural products and indicating the validity of the methods used, a standard drug must be simultaneously evaluated as a positive control group, but in this case it is difficult to choose a positive control because of the lack of appropriate standard drugs for morphine tolerance.
In conclusion, this study shows that the ethanolic extract of Satureja khuzestanica has significant inhibitory effect against morphine antinociceptive tolerance in rats. Thus, satureja may attenuate morphine-induced analgesic tolerance through its ability to decrease spinal cord glia activation. Investigations of the pharmacology of natural products are necessary to gain evidence concerning the usefulness of medicinal plants in phytotherapy. Our experiments therefore contribute to our knowledge of the pharmacology of Satureja khuzestanica.
References
Stefano GB, Kream RM, Esch T (2009) Revisiting tolerance from the endogenous morphine perspective. Med Sci Monit 15:189–198
Watkins LR, Hutchinson MR, Milligan ED, Maier SF (2007) “Listening” and “talking” to neurons: implications of immune activation for pain control and increasing the efficacy of opioids. Brain Res Rev 56:148–169
Raghavendra V, Rutkowski MD, DeLeo JA (2002) The role of spinal neuroimmune activation in morphine tolerance/hyperalgesia in neuropathic and sham-operated rats. J Neurosci 22:9980–9989
Song P, Zhao ZQ (2001) The involvement of glial cells in the development of morphine tolerance. Neurosci Res 39:281–286
DeLeo JA, Tanga FY, Tawfik VL (2004) Neuroimmune activation and neuroinflammation in chronic pain and opioid tolerance/hyperalgesia. Neuroscientist 10:40–52
Raghavendra V, Tanga FY, DeLeo JA (2004) Attenuation of morphine tolerance, withdrawal-induced hyperalgesia, and associated spinal inflammatory immune responses by propentofylline in rats. Neuropsychopharmacology 29:327–334
Ward J, Rosenbaum C, Hernon C, McCurdy CR, Boyer EW (2011) Herbal medicines for the management of opioid addiction: safe and effective alternatives to conventional pharmacotherapy? CNS Drugs 25:999–1007
Zargari A (1990) Medicinal plants. Tehran University Publications, Tehran, pp 42–45
Amanlou M, Dadkhah F, Salehnia A, Farsam H, Dehpour AR (2005) An anti-inflammatory and anti-nociceptive effects of hydroalcoholic extract of Satureja khuzestanica Jamzad extract. J Pharm Pharmaceut Sci 8:102–106
Kaeidi A, Esmaeili-Mahani S, Abbasnejad M, Sheibani V, Rasoulian B, Hajializadeh Z, Pasban-Aliabadi H (2013) Satureja khuzestanica attenuates apoptosis in hyperglycemic PC12 cells and spinal cord of diabetic rats. J Nat Med 67:61–69
Zimmermann M (1983) Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16:109–110
D’Amour FE, Smith DL (1941) A method of determining loss of pain sensation. J Pharmacol Exp Ther 27:74–79
Darvishzadeh-Mahani F, Esmaeili-Mahani S, Komeili G, Sheibani V, Zare L (2012) Ginger (Zingiber officinale Roscoe) prevents the development of morphine analgesic tolerance and physical dependence in rats. J Ethnopharmacol 141:901–907
Zare L, Esmaeili-Mahani S, Abbasnejad M, Rasoulian B, Sheibani V, Sahraei H, Kaeidi A (2012) Oleuropein, chief constituent of olive leaf extract, prevents the development of morphine antinociceptive tolerance through inhibition of morphine-induced L-type calcium channel overexpression. Phytother Res 26:1731–1737
Zhao J, Xin X, Xie GX, Palmer PP, Huang YG (2012) Molecular and cellular mechanisms of the age-dependency of opioid analgesia and tolerance. Mol Pain 8:38
Esmaeili Mahani S, Motamedi F, Javan M, Ahmadiani A (2005) Involvement of hypothalamic pituitary adrenal axis on the effects of nifedipine in the development of morphine tolerance in rats. Pharmacol Biochem Behav 81:152–157
Bryant L, Doyle T, Chen Z, Cuzzocrea S, Masini E, Vinci MC, Esposito E, Mazzon E, Petrusca DN, Petrache I, Salvemini D (2009) Spinal ceramide and neuronal apoptosis in morphine antinociceptive tolerance. Neurosci Lett 463:49–53
Ueda H, Ueda M (2009) Mechanisms underlying morphine analgesic tolerance and dependence. Front Biosci 14:5260–5272
Wen YR, Tan PH, Cheng JK, Liu YC, Ji RR (2011) Microglia: a promising target for treating neuropathic and postoperative pain, and morphine tolerance. J Formos Med Assoc 110:487–494
Tai YH, Wang YH, Wang JJ, Tao PL, Tung CS, Wong CS (2006) Amitriptyline suppresses neuroinflammation and up-regulates glutamate transporters in morphine-tolerant rats. Pain 124:77–86
Liu CH, Cherng CH, Lin SL, Yeh CC, Wu CT, Tai YH, Wong CS (2011) N-Methyl-d-aspartate receptor antagonist MK-801 suppresses glial pro-inflammatory cytokine expression in morphine-tolerant rats. Pharmacol Biochem Behav 99:371–380
Shen CH, Tsai RY, Shih MS, Lin SL, Tai YH, Chien CC, Wong CS (2011) Etanercept restores the antinociceptive effect of morphine and suppresses spinal neuroinflammation in morphine-tolerant rats. Anesth Analg 112:454–459
Horvath RJ, Romero-Sandoval EA, De Leo JA (2010) Inhibition of microglial P2X4 receptors attenuates morphine tolerance, Iba1, GFAP and mu opioid receptor protein expression while enhancing perivascular microglial ED2. Pain 150:401–413
Jin H, Li YH, Xu JS, Guo GQ, Chen DL, Bo Y (2012) Lipoxin A4 analog attenuates morphine antinociceptive tolerance, withdrawal-induced hyperalgesia, and glial reaction and cytokine expression in the spinal cord of rat. Neuroscience 208:1–10
Ndengele MM, Cuzzocrea S, Masini E, Vinci MC, Esposito E, Muscoli C, Petrusca DN, Mollace V, Mazzon E, Li D, Petrache I, Matuschak GM, Salvemini D (2009) Spinal ceramide modulates the development of morphine antinociceptive tolerance via peroxynitrite-mediated nitroxidative stress and neuroimmune activation. J Pharmacol Exp Ther 329:64–75
Ren K, Dubner R (2010) Interactions between the immune and nervous systems in pain. Nat Med 16:1267–1276
Guo RX, Zhang M, Liu W, Zhao CM, Cui Y, Wang CH, Feng JQ, Chen PX (2009) NMDA receptors are involved in upstream of the spinal JNK activation in morphine antinociceptive tolerance. Neurosci Lett 467:95–99
Doyle T, Bryant L, Batinic-Haberle I, Little J, Cuzzocrea S, Masini E, Spasojevic I, Salvemini D (2009) Supraspinal inactivation of mitochondrial superoxide dismutase is a source of peroxynitrite in the development of morphine antinociceptive tolerance. Neuroscience 164:702–710
Abdel-Zaher AO, Abdel-Rahman MS, ELwasei FM (2010) Blockade of nitric oxide overproduction and oxidative stress by Nigella sativa oil attenuates morphine-induced tolerance and dependence in mice. Neurochem Res 35:1557–1565
Abdollahi M, Salehnia A, Mortazavi SH, Ebrahimi M, Shafiee A, Fouladian F, Keshavarz K, Sorouri S, Khorasani R, Kazemi A (2003) Antioxidant, antidiabetic, antihyperlipidemic, reproduction stimulatory properties and safety of essential oil of Satureja khuzestanica in rat in vivo: a oxicopharmacological study. Med Sci Monit 9:331–335
Vosough-Ghanbari S, Rahimi R, Kharabaf S, Zeinali S, Mohammadirad A, Amini S, Yasa N, Salehnia A, Toliat T, Nikfar S, Larijani B, Abdollahi M (2010) Effects of Satureja khuzestanica on serum glucose, lipids and markers of oxidative stress in patients with type 2 diabetes mellitus: a double-blind randomized controlled trial. Evid Based Complement Altern Med 7:465–470
Rezvanfar M, Sadrkhanlou R, Ahmadi A, Shojaei-Sadee H, Rezvanfar M, Mohammadirad A, Salehnia A, Abdollahi M (2008) Protection of cyclophosphamide-induced toxicity in reproductive tract histology, sperm characteristics, and DNA damage by an herbal source; evidence for role of free-radical toxic stress. Hum Exp Toxicol 27:901–910
Acknowledgments
This work was supported by funds from Razi Herbal Medicines Research Center, Lorestan University of Medical Sciences and Kerman Neuroscience Research Center, Kerman University of Medical Sciences.
Conflict of interest
The authors declare that there are no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Esmaeili-Mahani, S., Ebrahimi, B., Abbasnejad, M. et al. Satureja khuzestanica prevents the development of morphine analgesic tolerance through suppression of spinal glial cell activation in rats. J Nat Med 69, 165–170 (2015). https://doi.org/10.1007/s11418-013-0796-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11418-013-0796-6