Abstract
Danggui-Shaoyao-San (DSS) is a traditional Chinese medicine, which has long been used for pain treatment and has been demonstrated to possess anti-oxidative, cognitive enhancement, and anti-depressant effects. In the present study, the effects of aqueous extracts of DSS on spontaneous pain behaviors and long-term hyperalgesia were examined to investigate the anti-nociceptive effects and underlying mechanisms. Single pretreatment of DSS dose-dependently reduced spontaneous flinches/licking time in the second, rather than the first, phase after subcutaneous injection of 5 % formalin into one hindpaw, in doses of 2.4 and 9.6 g/kg. DSS also dose-dependently inhibited FOS and cyclooxygenase-2 (COX-2) expression in both superficial and deep layers within the spinal dorsal horn. Further, DSS reduced hypoalgesia in the injected paw from 1 to 3 days and produced anti-hyperalgesic actions in both the injected paw after 3 days and non-injected paw. These data suggest involvement of enhancement of descending pain inhibition by suppression of 5-HTT levels in the spinal dorsal horn and reduction of peripheral long-term inflammation, including paw edema and ulcers. These findings suggest that DSS may be a useful therapeutic agent for short- and long-term inflammation induced pain, through both anti-inflammatory and suppression of central sensitization mechanisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pain is a significant clinical problem worldwide [1]. Clinical pain has multiple origins, symptoms, and signs, associated with tissue or nerve injury resulting in persist spontaneous pain, thermal and mechanical hyperalgesia, or allodynia evoked by different modalities of stimuli [2, 3]. Pain is also a cardinal feature of peripheral inflammation. However, undertreatment of pain is common. The formalin test, an experimental animal model producing both acute spontaneous pain and persistent mechanical and thermal allodynia and hypersensitivity, is produced by subcutaneous (s.c.) injection of formalin into a hindpaw [4]. Long-term peripheral inflammation and central sensitization are involved in the formalin-induced pain, which includes the descending pain modulating system. These associations would allow for more precise clarity as to anti-nociceptive properties mediated by peripheral and/or central-mediated analgesia and inter-model differences. Therefore, the potential role of any novel therapeutic analgesic agent through screening its effects in such an animal model can assist basic and clinical scientists as they seek out new treatment options in different pain states [5].
Danggui-Shaoyao-San (DSS), also called Toki-shakuyaku-san or TJ-23, is a widely used formula of traditional Chinese medicine (TCM) derived from “Jin Kui Yao Lue”, written by Zhong-Jing Zhang in the Eastern Han Dynasty. DSS consists of six Chinese herbs: Radix Paeoniae Alba, Radix Angelica sinensis, Rhizoma Chuanxiong, Poria cocos, Rhizoma Atractylodis macrocephalae, and Rhizoma Alismatis, with a ratio of 16:3:8:4:4:8 [6]. DSS has been used as a blood-activating and stasis-eliminating drug to treat gynecological disorders, such as dysmenorrhea, amenorrhea, and infertility for thousands of years [7, 8]. Recent studies have shown that it also possesses the potential as a therapeutic agent in treating neurocognitive pathogenesis, including depression, senile dementia, memory loss, and other cognitive disorders. Thus, the formula is used as a traditional remedy for Alzheimer’s disease in Japan [9–11]. Previously, our laboratory demonstrated that DSS increased the content of monoamine neuromodulators, such as norepinephrine (NE), dopamine (DA), and 5-hydroxytryptamine (5-HT) in the brains of aged mice and modulated their metabolism [6]. Otherwise, DSS suppresses inflammatory factor production [12], possesses anti-oxidant activity, and anti-apoptosis [13, 14]. Recent study suggests that DSS potentially alleviate pain in a tooth movement animal model, accompanied with neuronal and microglial inhibition within the ipsilateral trigeminal spinal nucleus caudalis [15]. However, the dose-dependent analgesic effects of DSS and peripheral and central mechanisms within the spinal cord remain uncertain.
Therefore, in the present study, we intended to investigate whether DSS produces analgesia in the formalin pain model via an amelioration of peripheral tissue injury and/or inflammation. Since monoamine neuromodulators, especially 5-HT, participates in descending pain inhibition, we hypothesized that potentially, DSS may decrease the levels of serotonin transporter (5-HTT) leading to increased content of 5-HT in the spinal dorsal horn, an integral membrane protein that transports serotonin from synaptic spaces into presynaptic neurons. Hence, the present investigation utilized a formalin model to evaluate possible analgesic effects of oral DSS administration and the potential peripheral and central mechanisms.
Materials and Methods
Animals
Male C57BL/6 mice (8–10 weeks) were housed in a temperature-controlled environment on a 12-h light/dark cycle with access to food and water ad libitum. All experimental procedures received prior approval from the Animal Use and Care Committee for Research and Education of the Fourth Military Medical University (Xi’an, China) and the ethical guidelines to investigate experimental pain in conscious animals.
DSS Preparation
Six herbs were purchased from Nanjing Medicinal Materials Company, Jiangsu Province, China, and identified by Dr. Bo-Yang Yu in the Department of Chinese Compound Prescription of China Pharmaceutical University. Aqueous extract of DSS was prepared following previous investigations [6]. In brief, six medicinal components were mixed in proportion and were macerated for 1 h with eight times (v/w) distilled water, then decocted for 1 h, after which the filtrate was collected and the residue was decocted again for 1 h with six times (v/w) distilled water. The filtrates were mixed and condensed and then dried by a vacuum dryer at 60 °C. The yield of dried powder was 29.0 % according to the original herbs. The doses of DSS were presented as the original crude drugs and the powder was suspended in distilled water. High-performance liquid chromatography (HPLC) fingerprint of DSS was detected according to our previous report [16], in which gallic acid, paeoniflorin, ferulic acid, senkyunolide I, tetra-galloy-glucose (TGG), penta-O-galloy-D-glucose (PGG), and alisol B were well identified.
Experimental Design
Experiment 1 evaluated the analgesic effects of intragastric administration of DSS on formalin-induced spontaneous pain, as well as spinal neuronal activation and underling mechanisms. After a 5-day acclimation period, mice were randomly divided into four groups: (1) Veh group, (2) DSS 0.6 g/kg group, (3) DSS 2.4 g/kg group, (4) DSS 9.6 g/kg group. The mice in the four groups were delivered intragastric administrations with vehicle (1 ml/kg, saline), 0.6, 2.4, and 9.6 g/kg DSS, followed by subcutaneous injection with 25 μl of 5 % formalin 1 h later.
Experiment 2 observed analgesic effects of DSS on formalin-induced long-term mechanical hyperalgesia as well as underlying central mechanisms and anti-inflammatory effects of DSS on the injected paws. The dose of DSS applied in this series was based on analysis of analgesic dosage effects of DSS on formalin-induced spontaneous pain. The mice were randomly assigned to one of the following groups: (1) Veh groups, (2) DSS group. All Veh and DSS group animals were administrated with Vehicle (1 ml/kg, saline) and DSS via a gastric tube from pre-injection 1 h to post-injection on day 10.
Assessment of Spontaneous Pain-Related Behaviors
The formalin test was used to induce mice flinching or licking the injected hindpaw, as described in our previous study [17]. All behavioral observations were performed in a low-illuminated sound-proof room. A sound-attenuated and transparent plexiglas test box (25 × 25 × 40 cm) with a transparent glass floor was placed on a supporting frame of 30 cm high above reverse video cameras to record video for offline behavioral analysis of spontaneous pain behaviors induced by administration of the formalin. After the mice acclimated to the testing chamber for about 30 min, 25 μl of the 5 % formalin solution (dissolved in saline) was s.c. injected into the plantar surface of the right hindpaw, using a microsyringe (Hamilton Co., NV, USA) attached to a 30-G needle. The observer was trained to provide a similar rating measurement for each behavior during the tests of different animals. Pain-related spontaneous responses were determined by counting the number of paw flinches or licking duration of the injected hindpaw occurring during 5 min intervals for 1 h following formalin injection with a stopwatch.
Immunohistochemistry Staining
After deep anesthesia was induced using pentobarbital (100 mg/kg, i.p.), and perfusion with 30 ml of 0.9 % saline followed by 100 ml of 0.1 M phosphate buffer (PB, pH 7.4) containing 4 % paraformaldehyde, the fifth lumbar spinal cord segments (L5) were removed and post-fixed in the same agent for 2 h and then immersed into 30 % sucrose in 0.1 M PB (pH 7.4) for 48 h at 4 °C. Transverse spinal sections (contralateral side was labeled by piercing on the ventral horn) were cut into 25 μm thickness on a cryostat (Leica CM1800, Heidelberg, Germany) at −20 °C, and sections were collected serially into 6 dishes containing 0.01 M phosphate-buffered saline (PBS, pH 7.4).
Immunohistochemistry staining for FOS or COX-2 was performed with an avidin-biotin-peroxidase complex (ABC) method. The sections in the first dish were rinsed in 0.01 M PBS three times (10 min each) and blocked with 10 % donkey serum in 0.01 M PBS containing 0.3 % Triton X-100 for 0.5 h at room temperature (RT, 20-25 °C), then used for immunohistochemical staining. The sections were incubated overnight at RT with mouse anti-FOS antiserum (1:500; ab11959; Abcam, Cambridge, MA, USA) or rabbit anti-COX-2 antiserum (1:200; ab15191; Abcam) in 0.01 M PBS containing 5 % normal donkey serum, 0.03 % Triton X-100, 0.05 % NaN3 and 0.25 % carrageenan (PBS-NDS, pH 7.4), followed by incubation with biotinylated donkey anti-mouse IgG (1:500; AP192B; Millipore, Billerica, MA, USA) or biotinylated donkey anti-rabbit IgG (1:500; AP182B; Millipore) diluted in PBS-NDS for 5 h. Finally, sections were incubated with ABC-Elite kit (1:100; Vector Laboratories, Burlingame, CA, USA) at RT for 2 h, and then, sections were further incubated in a solution containing 0.05 M Tris-HCl, 0.13 % diaminobenzidine, and 0.005 % hydrogen peroxide for 20 to 30 min in order to complete the diaminobenzidine reaction. Sections were washed completely with 0.01 M PBS between each step. Finally, all sections were mounted onto gelatin-coated glass slides, air dried, dehydrated in a graded series of diluted ethanol, cleared in xylene, and coverslipped.
Measurement of Behavior to Mechanical Stimuli
Mice were habituated to the testing environment for 3 days before baseline testing and then were placed under inverted plastic boxes (7 × 7 × 10 cm) on an elevated mesh floor and allowed to habituate for 30 min before the threshold testing. A logarithmic series of 8 calibrated Semmes-Weinstein monofilaments (von-Frey hairs; Stoelting, Kiel, WI, USA) were applied to the lateral edge on the plantar surface of the injected paw, as well as on the plantar surface of the contralateral paw to determine the stimulus intensity threshold stiffness required to elicit a paw withdrawal response. Log stiffness of the hairs was determined by log10 (milligrams × 10). A von-Frey filament was applied 10 times (3 s for each stimulus) to each testing area. The bending force of the von-Frey filament able to evoke a 50 % occurrence of paw withdrawal reflex was expressed as the paw withdrawal threshold (PWT). The stimulus was stopped if the threshold exceeded 10.0 g (cutoff value). Assessments were made before formalin injection as a baseline value. The behavioral tests were performed on 1, 3, 7, and 10 days after the 5 % formalin injection. The threshold was defined as the minimum pressure required eliciting a withdrawal reflex. The percent change in PWT was determined for the injected paw relative to the contralateral paw, according to the formula: (ipsilateral PWT − contralateral PWT)/contralateral PWT. This index was used as a measure of mechanical hyperalgesia associated with the injected hindpaw relative to the contralateral hindpaw. Positive values indicated a state of hypoalgesia, whereas negative values indicated a state of hyperalgesia associated with the injected hindpaw. All the tests were performed in a double-blind manner.
Measurements of Paw Edema and Areas of Ulcers
Edema and ulceration were produced by subcutaneous injection of formalin into the mice’s hindpaw at the site of injection [4]. Paw edema was assessed by measuring the foot sickness in the dorsal-plantar axis with a caliper. An index of paw edema was calculated as the mean difference of paw thickness (paw thickness of injected side − paw thickness of non-injected side)/paw thickness of non-injected side.
After measuring the thickness of paw, a photo containing the dorsal or plantar surface of hindpaw coupling with a ruler (minimum scale 1 mm) was taken using a camera. Then, one analyst determined the incidence of ulcers, areas of ulcers, and percentage of ulcers healing by using picture software ImageJ (National Institutes of Health, Bethesda, MD, USA). Based on the distance of 1 mm on the ruler, the scale (pixels/mm) can be set by the “set scale” function in the ImageJ. Then, “polygon selections” was used to outline the areas of ulcers, and the results would be calculated through “measure” function.
Western Blot
Mice were sacrificed after inducing deep anesthesia using pentobarbital (100 mg/kg, i.p.), and the L5 dorsal horns were quickly removed. The spinal dorsal horn was then dissected using the “open book” method [18]. Briefly, the L5 spinal cord segment was dissected according to the termination of the L4 and L5 dorsal roots. Then, the spinal segment was cut into a left and right half from the midline. Finally, the left half was further split into the dorsal and ventral horns at the level of the central canal. The dorsal horns were homogenized with a hand-held pestle in sodium dodecyl sulfate (SDS) sample buffer (10 ml/mg tissue), which contained a cocktail of proteinase and phosphatase inhibitors. The electrophoresis samples were heated at 100 °C for 5 min and loaded onto 10 % SDS-polyacrylamide gels with standard Laemmli solutions (Bio-Rad Laboratories, CA, USA). The proteins were electroblotted onto a polyvinylidene difluoride membrane (PVDF, Immobilon-P, Millipore, Billerica, MA, USA). The membrane was placed in a blocking solution, which contained Tris-buffered saline with 0.02 % Tween (TBS-T) and 5 % non-fat dry milk, for 1 h, and incubated overnight under gentle agitation with primary antibody rabbit anti-COX-2 (1:500), rabbit anti-5-HT transporter (1:1000; PC177L; Millipore), and mouse anti-β-actin (1:2000; A1978; Sigma, St Louis, MO, USA), respectively. Bound primary antibodies were detected with a horseradish peroxidase (HRP)-conjugated anti-rabbit or anti-mouse secondary antibody (1:5000; Amersham Pharmacia Biotech Inc., Piscataway, NJ, USA). Between each step, the immunoblots were rinsed with TBS-T.
All reactions were detected by the enhanced chemiluminescence (ECL) detection method (Amersham). The densities of protein blots were analyzed by using Labworks Software (Ultra-Violet Products, UK). The densities of COX-2, 5-HTT, and β-actin immunoreactive bands were quantified with background subtraction. Squares of identical sizes were drawn around each band to measure density, and the background near that band was subtracted. Since β-actin levels did not change significantly after inflammation and nerve injury [19], β-actin levels were used as loading controls, and COX-2 and 5-HTT levels were normalized against β-actin levels.
Statistical Analysis
All results were expressed as mean value ± standard deviation (SD). In the spontaneous behavior test, the area under curve of individual animals for flinching or licking responses were group pooled and used a One-way ANOVA with Dunnett’s post hoc test, which was performed using SPSS® version 16.0 software (SPSS Inc., Chicago, IL, USA). The DSS dosages were transformed into a logarithm dose with GraphPad Prism version 5.01 for Windows (Graph Pad Software, San Diego California USA, www.graphpad.com). The non-line fit was performed as to build a dose-response curve. Based on the dose-response curve, the 90 % effective doses (ED90) of DSS on analgesia were calculated. Differences in changes of values in Western blot over time of each group were tested using Two-way ANOVA, followed by the least significant difference test. Data from the von-Frey test were presented as mean ± SD and were analyzed as the interpolated 50 % threshold (absolute threshold) in the log base 10 of stimulus intensity (monofilament stiffness in milligrams × 10). Two-way ANOVA (with Bonferroni confidence interval adjustment) was used and conducted for analysis.
Results
Effects of Intragastrical DSS on Spontaneous Pain-Related Behaviors Induced by s.c. Formalin Injection
Injection of 5 % formalin s.c. into the plantar surface of the hindpaw produced biphasic pain-related behaviors, consisting of flinching and licking/biting of the injected paw. The first transient phase lasted for the first 10 min post-injection and was followed by the second prolonged phase from 15 to 60 min. There was no difference in the time course of the spontaneous pain-related behaviors between groups with and without i.g. DSS pretreatment (Fig. 1a, b).
Effects of i.g. pretreatment DSS (0.6, 2.4, 9.6 g/kg) or vehicle on formalin-induced spontaneous flinches and licking time of the injected hindpaw. Spontaneous flinches and licking time per 5 min during 60 min after s.c. formalin injection from different groups were shown in (a) and (b), respectively. The AUCs for different groups were calculated to perform statistical analysis on the first and second phases in (c) and (d). The log (dose)-response curves for DSS’s analgesic effects were shown in (e) and (f). n = 8, each group. *P < 0.05, **P < 0.01, ***P < 0.001
Since an obvious biphasic flinch response can be induced by s.c. formalin injection, effects of DSS on the first and second phase flinches were calculated based on the area under the curve (AUC). In comparison with i.g. saline, i.g. pretreatment with DSS significantly reduced the AUC of the second phase but not the first phase (Fig. 1c). By comparing the AUC of flinch behavior, there were no group differences in the first phase flinches (Fig. 1a, c; one-way ANOVA, Kruskal-Wallis test, P = 0.3453). The analgesic effects of DSS on the second phase flinches presented a significant group difference (Fig. 1a, c; one-way ANOVA, Kruskal-Wallis test, P = 0.0008). Dunnett’s post hoc test also revealed difference between DSS 2.4 g/kg (P < 0.05) or DSS 9.6 g/kg (P < 0.001) and vehicle groups. There were no significant differences between DSS 0.6 g/kg and vehicle groups (P > 0.05). The effect of DSS on the second phase flinches was calculated based on the log (dose) vs. response curve (Fig. 1e). The ED90 of DSS on the second phase flinches was 4.1 g/kg.
Since an obvious biphasic licking response with an upper second peak can be induced by s.c. formalin injection, the AUC was also calculated to analyze the analgesic effects of DSS. There were also no group differences in first phase lickings (Fig. 1b, d; one-way ANOVA, Kruskal-Wallis test, P = 0.8278). The analgesic effects of DSS on the second phase lickings presented significant group differences (Fig. 1b, d; one-way ANOVA, Kruskal-Wallis test, P < 0.0001). Dunnett’s post hoc test also revealed differences between DSS 2.4 g/kg (P < 0.001) or DSS 9.6 g/kg (P < 0.0001) and vehicle groups. There were no significant differences between DSS 0.6 g/kg and vehicle groups (P > 0.05). The effects of DSS on the second phase lickings were calculated based on the log (dose) vs. response curve (Fig. 1f). The ED90 of DSS on the second phase lickings was 4.9 g/kg. Considering the difference of ED90 for second phase flinches and lickings, DSS 4.9 g/kg was chosen as the dose of the following consecutive treatment.
Effects of i.g. DSS on Spinal Neuronal Activation and COX-2 Expression Induced by s.c. Formalin Injection
FOS protein has been widely used as a useful marker of neuronal activity that can be used to map functionally related neural pathways involved in specific behaviors including acute and chronic pain [20]. It has been confirmed that spinal neurons were activated after injecting formalin into the hindpaw, which was indicated by nuclei expression of FOS protein [17, 21, 22]. The number of FOS-ir neurons was used to evaluate the degree of the spinal neuronal activation. Therefore, i.g. DSS pretreatments were investigated to ascertain whether it inhibits neuronal activation indicated by decreasing the expression of FOS, correlating with analgesic effects on spontaneous behaviors.
Consistent with the known topographic projection of hindpaw afferents to the spinal cord, FOS-immunoreactive (ir) neurons were most densely observed within the medial half of the ipsilateral spinal dorsal horn, including superficial layers (lamina I-II) and deep layers (lamina III-VI) at 2 h after formalin injection (Fig. 2a). However, there were few FOS-ir neurons distributed in the contralateral spinal dorsal horn (no formalin injection) (Fig. 2b). Compared with the i.g. saline group, the i.g. DSS significantly decreased the total number of FOS-ir positive neurons per section in a dose-dependent manner (Fig. 2f; one-way ANOVA, P < 0.0001). The total number of FOS-ir positive neurons per section in the i.g. saline group, i.g. DSS 0.6, 2.4, and 9.6 g/kg group were 69.6 ± 11.5, 57 ± 9.4, 43 ± 9.0, and 30 ± 7.3, respectively. Dunnett’s post hoc test also revealed significant differences between DSS 0.6 g/kg (P < 0.05) or DSS 2.4 g/kg (P < 0.001) or DSS 9.6 g/kg (P < 0.0001) and vehicle group. Laminar specific counts also revealed that i.g. DSS treatment evoked a statistically significant reduction of FOS-ir positive cells in superficial layers (one-way ANOVA, P < 0.0001) and deep layers (one-way ANOVA, P < 0.0001).
Effects of i.g. pretreatment DSS (0.6, 2.4, 9.6 g/kg) or vehicle on the s.c. injection of formalin-induced FOS protein expression in the spinal cord. Representative photomicrographs demonstrate immunohistochemical staining for FOS in the ipsilateral spinal cord of vehicle (a), 0.6 g/kg (c), 2.4 g/kg (d), 9.6 g/kg (e) DSS treated group and the contralateral spinal cord of the vehicle group (b). There was almost no labeling in the lateral dorsal horn (asterisk). Scale bar = 100 μm. The numbers of FOS-ir cells per section were calculated and compared in these different groups (f). n = 8 sections from 4 animals, each group. *P < 0.05, ***P < 0.001
In the control mice, a relatively low COX-2 immunoreactivity was detected, and there were no significant differences between the two sides. Following formalin injection, increased COX-2 immunoreactivity was detected on the ipsilateral dorsal horn in contrast to the contralateral side (Fig. 3a, b). The DSS effects on COX-2 immunoreactivity were dose-dependent. Following i.g. DSS treatment, the level of COX-2 immunoreactivity was significantly decreased on the superficial layers (Fig. 3f; one-way ANOVA, P < 0.0001) and deep layers (one-way ANOVA, P < 0.0001) of the side ipsilateral to the formalin injection, in comparison to the control group with i.g. normal saline treatment. The expression levels of COX-2 in these groups were also evaluated by Western blot (Fig. 3g). The DSS also dose-dependently decreased the expression levels of COX-2 in the ipisilateral spinal dorsal horn (Fig. 3h; one-way ANOVA, P < 0.0001). These results demonstrated that increased COX-2 expression in the dorsal horn could be partially inhibited by DSS treatment although COX-2 did not return to the control level. In the contralateral side of the dorsal horn, there were no significant differences between the groups.
Effects of i.g. pretreatment DSS (0.6, 2.4, 9.6 g/kg) or vehicle on the s.c. injection of formalin-induced COX-2 expression in the spinal cord. Representative photomicrographs demonstrating immunohistochemical staining for COX-2 in the ipsilateral spinal cord of vehicle (a), 0.6 g/kg (c), 2.4 g/kg (d), 9.6 g/kg (e) DSS treated group and the contralateral spinal cord of the vehicle group (b). Scale bar = 100 μm. The relative COX-2 immunoreactivities per section were calculated and compared in these different groups (f). n = 8 sections from 4 animals, each group. ***P < 0.001. Western blot showed the COX-2 expression in the ipsilateral spinal cord of vehicle, 0.6, 2.4, 9.6 g/kg DSS treated group and the contralateral spinal cord of the vehicle group (a). The bar graphs demonstrated the mean levels of 5-HTT normalized to β-actin (b). The relative COX-2 levels were expressed as percentages of the contralateral spinal cord of the vehicle group. n = 3, each group. A number sign was used, when ipsilateral and contralateral spinal cord of vehicle group were compared; an asterisk was used, when DSS treated groups were compared with ipsilateral spinal cord of vehicle group. ### P < 0.001, *P < 0.05, ***P < 0.001
Effects of i.g. DSS on Mechanical Hyposensitivity, or Hypersensitivity and Spinal 5-HTT Levels Induced by s.c. Formalin Injection
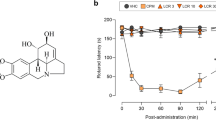
There were no significant differences between the right hindpaw and left hindpaw on baseline paw withdrawal thresholds (PWTs) to mechanical stimulus on the plantar surface. After formalin was injected into the plantar surface of the right hindpaw, PWTs on the plantar surface of the injected paws increased relative to baseline pre-injection values at 1 day (P < 0.001). This hypoalgesic state of the injected hindpaw was evident at 3 days (P = 0.009). Then, PWTs on the plantar surface of the injected paws decreased and presented hyperalgesia after 3 days. So, injection of formalin produced both hypoalgesia and hyperalgesia on the ipsilateral paws. Consecutive i.g. DSS treatment reduced not only hypoalgesia but also hyperalgesia (Fig. 4a; two-way ANOVA, P < 0.05). With regard to differences from the injected paws, hyperalgesic responses to mechanical stimuli were detected on the non-injected paws from 1 to 10 days after formalin injection. The analgesic effects of i.g. DSS on the contralateral paws were also observed (Fig. 4a; two-way ANOVA, P < 0.05). The hypoalgesic state was also observed on 1 day (P = 0.002) and 3 days (P = 0.014) by comparison of the injected paws to non-injected paws (Fig. 4b). Therefore, there was a protective effect of DSS on this formalin-induced hypoalgesic state (two-way ANOVA, P < 0.05).
Effects of consecutive i.g. pretreatment DSS or saline on formalin-induced mechanical hyposensitivity, or hypersensitivity, and edema thickness. Injection of formalin-induced mechanical hypersensitivity in the contralateral hindpaw and mechanical both hyposensitivity and hypersensitivity in the ipsilateral hindpaw from 1 to 10 days after injection (a). The differences in PWTs between the injected and uninjected paw were shown in (b). The percentages of increase in paw thickness were calculated in (c). The representative photographs showed the dorsal and plantar surface of the hindpaw before formalin injection and after formalin injection 2 h and 1 day (d). The minimum scale value is 1 mm in the stainless stain rule. n = 8 for the saline group, n = 12 for the DSS group. *P < 0.05, **P < 0.01, ***P < 0.001
The loss of descending analgesia was considered as a critical contribution to the hypersensitivity of both the injected hindpaw and non-injected hindpaw. Since 5-HTT is the principle means for actively clearing of 5-HT from the extracellular space, we evaluated the expression levels of 5-HTT in both the ipsilateral and contralateral dorsal horn to formalin injection, and this was evaluated by Western blot. The expression levels of 5-HTT increased after formalin injection from 1 to 10 days, both on the ipsilateral side (P < 0.001) and the contralateral side (P < 0.001). Consecutive i.g. DSS treatment reduced the elevated 5-HTT levels, both on the ipsilateral side (Fig. 5a; two-way ANOVA, P < 0.05) and the contralateral side (Fig. 5b; two-way ANOVA, P < 0.05).
Effects of consecutive i.g. pretreatment DSS or saline on the formalin-induced 5-HTT expression in the spinal dorsal horn of ipsilateral and contralateral hindpaws. Western blot showed the time-dependent changes of 5-HTT expression in the ipsilateral (a) and contralateral (b) dorsal horn after formalin injection. The bottom bar graphs demonstrated the mean levels of 5-HTT normalized to β-actin. The relative 5-HTT levels after formalin injection were expressed as percentages of the naïve-saline group. n = 3, each group. A number sign was used, when saline groups were compared with naïve-saline group; an asterisk was used, when DSS groups were compared with saline groups at the same time point. ### P < 0.001, *P < 0.05, ***P < 0.001
Effects of i.g. DSS on Edema Thickness and Areas of Ulcers Induced by s.c. Formalin Injection
Paw edema on the injected side was present at 2 h after s.c. formalin injection (Fig. 4d). There were no significant differences between the right and left hindpaw on the baseline of the thickness of paws. The magnitude of paw edema was calculated by increased percentage of ipsilateral paws relative to the contralateral paws. The magnitude of paw edema increased rapidly over the first hour, peaked on the 3 days (72.6 ± 13.0 %) and elevated at 10 days (54.7 ± 6.2 %) after formalin injection. The paw returned to a pre-injection appearance, approximately 4 weeks after injection. Paw edema was not observed on the contralateral paws. Consecutive i.g. DSS treatment significantly reduced the percentage of ipsilateral paws edema (Fig. 4c; two-way ANOVA, P < 0.05).
Formalin injection also produced ulcers on the plantar surface of the injected paw on 3 days after injection. Most ulcers developed most severely with significant inflammatory exudates at 7 days, with many ulcers gradually healing by 10 days (Fig. 6a). The incidence of ulcers, areas of the ulcers, and incidence of ulcers healing were different among mice. Consecutive i.g. DSS treatment reduced the incidence of paw ulcers at 3 days (75 vs. 44.44 %) and 7 days (87.5 vs. 77.78 %), decreased the areas of ulcers at 3 days (P = 0.019), 7 days (P < 0.001), and 10 days (P = 0.0095) and increased the incidence of ulcers healing at 10 day (14.29 vs. 42.86 %), compared with i.g. saline (Fig. 6b, c).
Effects of consecutive i.g. pretreatment DSS or saline on the formalin-induced incidence of ulcers, percentages of ulcers healing, and areas of ulcers. The representative photographs showed the plantar surface of the hindpaw after formalin injection 3, 7, and 10 days (a). The minimum scale value is 1 mm in the stainless stain rule. The incidence of ulcers and percentages of ulcers healing were calculated in (b). The areas of ulcers in the two groups were compared in (c). n = 8 for the saline group, n = 12 for the DSS group. *P < 0.05, **P < 0.01, ***P < 0.001
Discussion
Our study systemically investigated the potential anti-nociceptive effects of DSS, a traditional Chinese formula containing six herbs, on diverse “phenotypes” of nociception and hypersensitivity relevant to formalin-induced inflammatory pain. Pretreatment with i.g. DSS dose-dependently suppressed spontaneous flinching and licking responses in the second instead of the first phase. The total number of FOS-ir cells in the spinal dorsal horn, including superficial and deep layers, was also dose-dependently reduced after formalin injection at 2 h. These analgesic properties of DSS may result from suppression of COX-2 expression in the spinal cord in addition to the neuronal inhibition. Further, consecutive i.g. DSS protected tissue and nerve endings from formalin-induced inflammation, resulting in reduction of hypoalgesia in the injected paw from 1 to 3 days. Possible mechanisms related to the anti-hyperalgesic or anti-allodynic effects seen in both the injected and non-injected paws might be enhancing descending pain inhibition, by suppressing 5-HTT levels in the spinal dorsal horn and reducing peripheral long-term inflammation, including paw edema and ulcers. These results indicate that DSS may be a useful therapeutic agent for short- and long-term inflammatory pain, through both anti-inflammation and suppression of central sensitization mechanisms.
Effects of i.g. DSS on Short-Term Inflammatory Pain and Possible Mechanisms Following s.c. Formalin Injection
In order to confirm the analgesic effects of DSS on formalin-induced spontaneous pain, flinching and licking behaviors were doubly examined and indicate that DSS pretreatment decreases the pain responses in the second phase greater than those in the first phase. Previous studies have demonstrated the analgesic effects of paeoniflorin, which is one of the active chemical compounds identified from the DSS, in several pain models including formalin-induced pain model, [5, 23–25]. It has been shown that intracerebroventricular pretreatment with paeoniflorin suppressed licking responses in both the first and second phases of the formalin test [24]. They concluded that this anti-nociception from paeoniflorin on the first phase was mediated by activating central κ opioid receptor. However, it has been clarified that the first phase is related to chemical activation of nociceptive primary afferent fibers via direct activation of transient receptor potential ankyrin 1 (TRPA1) receptors [26, 27], while the second phase response is the consequence of central sensitization which largely involves primary sensory neurons [28], spinal cord neurons [17, 29], or descending modulation [30–32], in addition to direct activation of TRPA1.
Another approach to investigate the analgesic properties of DSS involves the FOS expression. FOS expression has been widely utilized as an index of analgesia, demonstrating anti-nociceptive actions for many analgesics [17, 21, 22]. Injection of formalin significantly increased neuronal activation, indicated by the nuclei expression of FOS, and such neuronal activation reaches a peak at 2 h after formalin injection [17, 33]. Consistent with previous studies showing that primary afferents which innervate distal extremities terminate in the medial superficial dorsal horn and that input from proximal extremities is represented more laterally, our results also showed that FOS-ir neurons were concentrated in the medial part of the spinal dorsal horn [21, 22, 34, 35]. FOS expression in the deep layers was much more sensitive to DSS administration than that in the superficial layers, and a similar phenomenon has already been reported in previous studies [21, 29, 36, 37]. The two phases of the formalin test contribute equally to FOS expression in the superficial dorsal horn but differentially to the neuronal activation in the deep layers [29]. The second phase is associated with a predominant increase of FOS expression in the deep layers. Blockade of the second phase could produce a greater suppression of FOS expression in deep layers. Besides, many FOS-ir neurons in the superficial dorsal horn may be inhibitory interneurons [38–40].
Non-steroidal anti-inflammatory drugs (NSAIDs) are commonly used medications targeting different types of pain, especially inflammatory pain. NSAIDs exhibit anti-pyretic, anti-inflammatory, and analgesic activities attributed to inhibition of prostaglandins biosynthesis [41, 42]. Prostaglandins are produced after induction of COX-2, which is an inducible enzyme and contributes to both inflammation and pain hypersensitivity. Marked increases in COX-2 expression occur not only locally at the site of inflammation [43] but also in neurons, glia, and endothelial cells in the spinal cord and brain [43, 44]. COX-2 is increased in neurons after peripheral inflammation, where it aids in developing a central component of inflammatory pain hypersensitivity by increasing neuronal excitation and reducing inhibition. After induction of paw inflammation with zymosan, COX-2 immunoreactivity increases dramatically in dorsal horn neurons of lamina I-VI and X, paralleled by a significant increase in prostaglandin E2 release from spinal cord [45]. Similarly, spinal COX-2 mRNA and protein are raised significantly after peripheral inflammatory stimuli [46, 47]. Importantly, there was no change in formalin-induced spontaneous pain behavior during the first phase and significant differences in the second phase between nCOX-2−/− mice and their control littermates [47]. Moreover, constitutive spinal COX-2 is an important contributor to immediate hyperalgesia induced by peripheral inflammation, intrathecal SP, and NMDA [48]. It has been demonstrated that DSS can inhibit COX-2 by inhibiting COX-2 activity and reducing COX-2 expression, not only at the level of transcription but also at the translation level [12]. Thus, the inhibitory expressions of COX-2 by DSS contribute to suppression of spontaneous pain behaviors and FOS expression.
Effects of i.g. DSS on Long-Term Inflammatory Pain and Possible Mechanisms Following s.c. Formalin Injection
It is interesting that the injected hindpaw presented hypoalgesia from 1 to 3 days after formalin injection presumably because nerve endings and local nociceptive receptors were damaged by formalin leading to desensitization. Hyperalgesic responses to mechanical stimuli were observed on the injected paw after 3 days and the contralateral paw. Although the mechanisms that mediate the ipsilateral hyperalgesic responses have not been clearly established, there have been several supporting studies. Spinal microglial activation and peripheral inflammation might contribute to the long-lasting, persistent pain states [4, 49, 50]. Meanwhile, the time course of hyperalgesic responses from 1 day to 4 weeks matches the time course of spinal microglial activation. However, this microglial activation was not observed in another study [51]. Peripheral and spinal Ca2+-activated chloride channels, chloride-bicarbonate anion exchanger 3, TRPV1, and ASIC3 might also participate in the long-term mechanical hyperalgesia induced by formalin [52–54]. In addition to the above mechanisms, progressive tactile hypersensitivity that repetitive touch stimuli results in a progressively increased spontaneous activity, touch, pinch, and Aβ afferent-evoked responses of hamstring flexor motor neurons may also explain the development of hyperalgesia [55].
At present, little is known related to the mechanism underlying the phenomenon of bilateral hyperalgesia after unilateral tissue inflammation or nerve injury. Because the contralateral hyperalgesia does not appear to be caused by direct inflammation, central sensitization is likely a contributor to the long-lasting hyperalgesia. It has been suggested that this might involve the release of immune substances and proinflammatory cytokines from glia [56, 57] and the bilateral signaling via commissural interneurons [58] which might induce this mirror-image pain. It also may be reflective of adaptive changes in the inhibitory and/or excitatory descending pathways in response to inflammation-facilitated spinal nociception. Our previous studies have shown that descending 5-HT and 5-HT receptors in the spinal cord play critical roles in the inflammatory pain [59, 60]. Others also showed that 5-HT2A/2B/2C receptors, 5-HT3 receptors, and 5-HT4/6/7 receptors participate in the development and maintenance of formalin-induced bilateral long-term hyperalgesia [61–63].
Our observations on spinal expression of 5-HTT appear to support this hypothesis since the adaptive changes were located bilaterally to inflammation, which means that these changes could also be related to the onset of the bilateral hyperalgesia. 5-HTT is an integral membrane protein which transports serotonin from synaptic spaces into presynaptic neurons and thus plays an essential role in determining the duration and intensity of 5-HT communication with its receptors [64, 65]. 5-HTT is highly expressed in the spinal cord, and its distribution parallels the innervations by serotoninergic fibers [66]. This protein is the therapeutic target of many anti-depressant medications, including those of selective serotonin reuptake inhibitors (SSRIs), which also possess analgesic properties [31]. In human studies, 5-HTT gene polymorphisms have been associated with heat pain perception in adults with chronic pain [67]. Mice with 5-HTT deficiency have attenuated thermal hyperalgesia in pain models of chronic constriction injury of the sciatic nerve and hindpaw inflammation induced by complete Freund’s adjuvant [68, 69]. It has also been demonstrated that 5-HTT−/− genotype protects mice from mechanical allodynia and heat hyperalgesia in vincristine neuropathy [70]. No difference in thermal nociception has been found between 5-HTT−/− and wild type mice, suggesting that the loss of 5-HTT does not lead to altered thermal pain sensation [71]. The development of mechanical hyperalgesia depends on the central sensitization which appears to be related to the loss of descending inhibition [72], though an increase in descending facilitation at the spinal cord level through 5-HT pathway is another plausible explanation [73]. Therefore, it is not clear whether an increase in the expression of spinal 5-HTT may contribute to mechanical hypersensitivity, or conversely, it may be a compensatory mechanism to reduce 5-HT level in synaptic spaces.
DSS can increase the contents of NE, DA, and 5-HT, as to modulate metabolism of monoamine neurotransmitters [6]. It has also been demonstrated that DSS decreases activity of acetylcholinesterase as to enhance cholinergic-mediated pathways [74]. Antagonists of 5-HT receptors reverse the effect of ferulic acid, and the combination of SSRIs and ferulic acid also produces a synergic anti-depressant-like effect, which is one of the most important properties of DSS [75]. In addition, paeoniflorin stimulates the release of 5-HT and NE from synaptosomes [76].
Effects of i.g. DSS on Peripheral Inflammation Induced by s.c. Formalin Injection
Formalin-induced paw inflammation developed quickly and reached its peak in several hours, then began to decrease from 8 h to 1 day after injection. Formalin injection subcutaneously into the hindpaw produced significant inflammation characterized by accumulation of neutrophils and macrophages observed at 6 h and day 3. These findings are representative of acute and chronic inflammation, characterized by fibrosis and infiltration of mononuclear cells [77]. Inflammatory cells were strongly stained with COX-2. The suppression of COX-2 from DSS might be linked to this peripheral anti-inflammatory effect. Treatment of PC12 cells with DSS has been shown to inhibit H2O2-induced apoptosis by the regulation of Bcl-2 family members, as well as suppression of cytochrome c release and caspase cascade activation [14]. This protective effect of DSS might be a reason for the decreasing incidence of ulcers and increasing incidence of ulcer healing.
In summary, the present study provided initial evidence demonstrating that systemic application of DSS dose-dependently inhibits pain behaviors in the second phase in the formalin model, likely attributed to the suppression of FOS and COX-2 expression in the spinal dorsal horn. Furthermore, consecutive application of DSS reduced both hypoalgesia and hyperalgesia, which might represent the involvement of suppression of 5-HTT levels in the spinal dorsal horn and reduction of peripheral inflammation, including paw edema and ulcers. These new findings related to the anti-nociceptive and anti-inflammatory actions of DSS may open new therapeutic investigations into the development of novel strategies in the treatment of clinical pain.
References
De Leon-Casasola OA (2013) Opioids for chronic pain: new evidence, new strategies, safe prescribing. Am J Med 126:S3–11
Merskey M, Bogduk N (eds) (1994) Classification of chronic pain. IASP press, Seattle
Yin JB, Cui GB, Mi MS, Du YX, Wu SX, Li YQ, Wang W (2014) Local infiltration analgesia for postoperative pain after hip arthroplasty: a systematic review and meta-analysis. J Pain 15:781–799
Fu KY, Light AR, Maixner W (2001) Long-lasting inflammation and long-term hyperalgesia after subcutaneous formalin injection into the rat hindpaw. J Pain 2:2–11
Yu HY, Liu MG, Liu DN, Shang GW, Wang Y, Qi C, Zhang KP, Song ZJ et al (2007) Antinociceptive effects of systemic paeoniflorin on bee venom-induced various ‘phenotypes’ of nociception and hypersensitivity. Pharmacol Biochem Behav 88:131–140
Kou J, Zhu D, Yan Y (2005) Neuroprotective effects of the aqueous extract of the Chinese medicine Danggui-Shaoyao-san on aged mice. J Ethnopharmacol 97:313–318
Jiang H, Shen Y, Wang XG (2010) Current progress of Chinese medicinal treatment of endometriosis. Chin J Integr Med 16:283–288
Kotani N, Oyama T, Sakai I, Hashimoto H, Muraoka M, Ogawa Y, Matsuki A (1997) Analgesic effect of a herbal medicine for treatment of primary dysmenorrhea—a double-blind study. Am J Chin Med 25:205–212
Hatip-Al-Khatib I, Egashira N, Mishima K, Iwasaki K, Kurauchi K, Inui K, Ikeda T, Fujiwara M (2004) Determination of the effectiveness of components of the herbal medicine Toki-Shakuyaku-San and fractions of Angelica acutiloba in improving the scopolamine-induced impairment of rat’s spatial cognition in eight-armed radial maze test. J Pharmacol Sci 96:33–41
Kano Y, Takaguchi S, Nohno T, Hiragami F, Kawamura K, Iwama MK, Miyamoto K, Takehara M (2002) Chinese medicine induces neurite outgrowth in PC12 mutant cells incapable of differentiation. Am J Chin Med 30:287–295
Zhou K, Jia N, Jiang N, Wang F, and Kou J (2015) Beneficial effect of Danggui-Shaoyao-san, a Traditional Chinese Medicine, on drowsiness induced by chronic restraint stress. Neurosci Lett
Hua YQ, Su SL, Duan JA, Wang QJ, Lu Y, Chen L (2008) Danggui-Shaoyao-San, a traditional Chinese prescription, suppresses PGF2alpha production in endometrial epithelial cells by inhibiting COX-2 expression and activity. Phytomedicine 15:1046–1052
Liu IM, Tzeng TF, Liou SS, Chang CJ (2012) Beneficial effect of traditional Chinese medicinal formula danggui-shaoyao-san on advanced glycation end-product-mediated renal injury in streptozotocin-diabetic rats. Evid Based Complement Alternat Med 2012:140103
Qian YF, Wang H, Yao WB, Gao XD (2008) Aqueous extract of the Chinese medicine, Danggui-Shaoyao-San, inhibits apoptosis in hydrogen peroxide-induced PC12 cells by preventing cytochrome c release and inactivating of caspase cascade. Cell Biol Int 32:304–311
Li H, Gu Z, Wu L, Xia L, Zhou K, E L, Wang D, Kou J et al (2014) Danggui-shaoyao-san, a traditional Chinese medicine prescription, alleviates the orthodontic pain and inhibits neuronal and microglia activation. Chin Med J (Engl) 127:3630–3637
Chen L, Qi J, Chang YX, Zhu D, Yu B (2009) Identification and determination of the major constituents in Traditional Chinese Medicinal formula Danggui-Shaoyao-San by HPLC-DAD-ESI-MS/MS. J Pharm Biomed Anal 50:127–137
Bai L, Wang W, Dong YL, Huang J, Wang XY, Wang LY, Li YQ, Wu SX (2012) Attenuation of mouse somatic and emotional inflammatory pain by hydralazine through scavenging acrolein and inhibiting neuronal activation. Pain Physician 15:311–326
Zhuang ZY, Gerner P, Woolf CJ, Ji RR (2005) ERK is sequentially activated in neurons, microglia, and astrocytes by spinal nerve ligation and contributes to mechanical allodynia in this neuropathic pain model. Pain 114:149–159
Guo W, Wang H, Watanabe M, Shimizu K, Zou S, Lagraize SC, Wei F, Dubner R et al (2007) Glial-cytokine-neuronal interactions underlying the mechanisms of persistent pain. J Neurosci 27:6006–6018
Guzowski JF, Timlin JA, Roysam B, Mcnaughton BL, Worley PF, Barnes CA (2005) Mapping behaviorally relevant neural circuits with immediate-early gene expression. Curr Opin Neurobiol 15:599–606
Presley RW, Menetrey D, Levine JD, Basbaum AI (1990) Systemic morphine suppresses noxious stimulus-evoked Fos protein-like immunoreactivity in the rat spinal cord. J Neurosci 10:323–335
Roussy G, Dansereau MA, Dore-Savard L, Belleville K, Beaudet N, Richelson E, Sarret P (2008) Spinal NTS1 receptors regulate nociceptive signaling in a rat formalin tonic pain model. J Neurochem 105:1100–1114
Lee KK, Omiya Y, Yuzurihara M, Kase Y, Kobayashi H (2011) Antinociceptive effect of paeoniflorin via spinal alpha(2)-adrenoceptor activation in diabetic mice. Eur J Pain 15:1035–1039
Tsai HY, Lin YT, Tsai CH, Chen YF (2001) Effects of paeoniflorin on the formalin-induced nociceptive behaviour in mice. J Ethnopharmacol 75:267–271
Zhang XJ, Chen HL, Li Z, Zhang HQ, Xu HX, Sung JJ, Bian ZX (2009) Analgesic effect of paeoniflorin in rats with neonatal maternal separation-induced visceral hyperalgesia is mediated through adenosine A(1) receptor by inhibiting the extracellular signal-regulated protein kinase (ERK) pathway. Pharmacol Biochem Behav 94:88–97
Macpherson LJ, Xiao B, Kwan KY, Petrus MJ, Dubin AE, Hwang S, Cravatt B, Corey DP et al (2007) An ion channel essential for sensing chemical damage. J Neurosci 27:11412–11415
Mcnamara CR, Mandel-Brehm J, Bautista DM, Siemens J, Deranian KL, Zhao M, Hayward NJ, Chong JA et al (2007) TRPA1 mediates formalin-induced pain. Proc Natl Acad Sci U S A 104:13525–13530
Mcroberts JA, Ennes HS, Marvizon JC, Fanselow MS, Mayer EA, Vissel B (2011) Selective knockdown of NMDA receptors in primary afferent neurons decreases pain during phase 2 of the formalin test. Neuroscience 172:474–482
Abbadie C, Taylor BK, Peterson MA, Basbaum AI (1997) Differential contribution of the two phases of the formalin test to the pattern of c-fos expression in the rat spinal cord: studies with remifentanil and lidocaine. Pain 69:101–110
Chen HS, Li MM, Shi J, Chen J (2003) Supraspinal contribution to development of both tonic nociception and referred mirror hyperalgesia: a comparative study between formalin test and bee venom test in the rat. Anesthesiology 98:1231–1236
Sun YH, Dong YL, Wang YT, Zhao GL, Lu GJ, Yang J, Wu SX, Gu ZX et al (2013) Synergistic analgesia of duloxetine and celecoxib in the mouse formalin test: a combination analysis. PLoS ONE 8, e76603
Yin JB, Wu HH, Dong YL, Zhang T, Wang J, Zhang Y, Wei YY, Lu YC et al (2014) Neurochemical properties of BDNF-containing neurons projecting to rostral ventromedial medulla in the ventrolateral periaqueductal gray. Front Neural Circ 8:137
Liu CR, Duan QZ, Wang W, Wei YY, Zhang H, Li YQ, Wu SX, Xu LX (2011) Effects of intrathecal isoflurane administration on nociception and Fos expression in the rat spinal cord. Eur J Anaesthesiol 28:112–119
Molander C, Grant G (1985) Cutaneous projections from the rat hindlimb foot to the substantia gelatinosa of the spinal cord studied by transganglionic transport of WGA-HRP conjugate. J Comp Neurol 237:476–484
Sugiura Y, Lee CL, Perl ER (1986) Central projections of identified, unmyelinated (C) afferent fibers innervating mammalian skin. Science 234:358–361
Jasmin L, Wang H, Tarczy-Hornoch K, Levine JD, Basbaum AI (1994) Differential effects of morphine on noxious stimulus-evoked fos-like immunoreactivity in subpopulations of spinoparabrachial neurons. J Neurosci 14:7252–7260
Luo C, Chen J, Li HL, Li JS (1998) Spatial and temporal expression of c-Fos protein in the spinal cord of anesthetized rat induced by subcutaneous bee venom injection. Brain Res 806:175–185
Dickenson AH, Sullivan AF (1986) Electrophysiological studies on the effects of intrathecal morphine on nociceptive neurones in the rat dorsal horn. Pain 24:211–222
Sastry BR, Goh JW (1983) Actions of morphine and met-enkephalin-amide on nociceptor driven neurones in substantia gelatinosa and deeper dorsal horn. Neuropharmacology 22:119–122
Willis WD, Coggeshall RE (1991) Mechanisms of the spinal cord. Plenum, New York
Bovill JG (1997) Mechanisms of actions of opioids and non-steroidal anti-inflammatory drugs. Eur J Anaesthesiol Suppl 15:9–15
Burian M, Geisslinger G (2005) COX-dependent mechanisms involved in the antinociceptive action of NSAIDs at central and peripheral sites. Pharmacol Ther 107:139–154
Samad TA, Moore KA, Sapirstein A, Billet S, Allchorne A, Poole S, Bonventre JV, Woolf CJ (2001) Interleukin-1beta-mediated induction of Cox-2 in the CNS contributes to inflammatory pain hypersensitivity. Nature 410:471–475
Laflamme N, Lacroix S, Rivest S (1999) An essential role of interleukin-1beta in mediating NF-kappaB activity and COX-2 transcription in cells of the blood–brain barrier in response to a systemic and localized inflammation but not during endotoxemia. J Neurosci 19:10923–10930
Maihofner C, Tegeder I, Euchenhofer C, Dewitt D, Brune K, Bang R, Neuhuber W, Geisslinger G (2000) Localization and regulation of cyclo-oxygenase-1 and −2 and neuronal nitric oxide synthase in mouse spinal cord. Neuroscience 101:1093–1108
Beiche F, Scheuerer S, Brune K, Geisslinger G, Goppelt-Struebe M (1996) Up-regulation of cyclooxygenase-2 mRNA in the rat spinal cord following peripheral inflammation. FEBS Lett 390:165–169
Vardeh D, Wang D, Costigan M, Lazarus M, Saper CB, Woolf CJ, Fitzgerald GA, Samad TA (2009) COX2 in CNS neural cells mediates mechanical inflammatory pain hypersensitivity in mice. J Clin Invest 119:287–294
Yaksh TL, Dirig DM, Conway CM, Svensson C, Luo ZD, Isakson PC (2001) The acute antihyperalgesic action of nonsteroidal, anti-inflammatory drugs and release of spinal prostaglandin E2 is mediated by the inhibition of constitutive spinal cyclooxygenase-2 (COX-2) but not COX-1. J Neurosci 21:5847–5853
Fu KY, Light AR, Maixner W (2000) Relationship between nociceptor activity, peripheral edema, spinal microglial activation and long-term hyperalgesia induced by formalin. Neuroscience 101:1127–1135
Fu KY, Light AR, Matsushima GK, Maixner W (1999) Microglial reactions after subcutaneous formalin injection into the rat hind paw. Brain Res 825:59–67
Sweitzer SM, Colburn RW, Rutkowski M, Deleo JA (1999) Acute peripheral inflammation induces moderate glial activation and spinal IL-1beta expression that correlates with pain behavior in the rat. Brain Res 829:209–221
Barragan-Iglesias P, Rocha-Gonzalez HI, Pineda-Farias JB, Murbartian J, Godinez-Chaparro B, Reinach PS, Cunha TM, Cunha FQ et al (2014) Inhibition of peripheral anion exchanger 3 decreases formalin-induced pain. Eur J Pharmacol 738:91–100
Garcia G, Martinez-Rojas VA, Rocha-Gonzalez HI, Granados-Soto V, Murbartian J (2014) Evidence for the participation of Ca(2+)-activated chloride channels in formalin-induced acute and chronic nociception. Brain Res 1579:35–44
Martinez-Rojas VA, Barragan-Iglesias P, Rocha-Gonzalez HI, Murbartian J, Granados-Soto V (2014) Role of TRPV1 and ASIC3 in formalin-induced secondary allodynia and hyperalgesia. Pharmacol Rep 66:964–971
Ma QP, Woolf CJ (1996) Progressive tactile hypersensitivity: an inflammation-induced incremental increase in the excitability of the spinal cord. Pain 67:97–106
Twining CM, Sloane EM, Milligan ED, Chacur M, Martin D, Poole S, Marsh H, Maier SF et al (2004) Peri-sciatic proinflammatory cytokines, reactive oxygen species, and complement induce mirror-image neuropathic pain in rats. Pain 110:299–309
Watkins LR, Milligan ED, Maier SF (2001) Spinal cord glia: new players in pain. Pain 93:201–205
Koltzenburg M, Wall PD, Mcmahon SB (1999) Does the right side know what the left is doing? Trends Neurosci 22:122–127
Wang W, Wu SX, Wang YY, Liu XY, Li YQ (2003) 5-hydroxytryptamine1A receptor is involved in the bee venom induced inflammatory pain. Pain 106:135–142
Wu SX, Wang W, Li H, Wang YY, Feng YP, Li YQ (2010) The synaptic connectivity that underlies the noxious transmission and modulation within the superficial dorsal horn of the spinal cord. Prog Neurobiol 91:38–54
Bravo-Hernandez M, Cervantes-Duran C, Pineda-Farias JB, Barragan-Iglesias P, Lopez-Sanchez P, Granados-Soto V (2012) Role of peripheral and spinal 5-HT(3) receptors in development and maintenance of formalin-induced long-term secondary allodynia and hyperalgesia. Pharmacol Biochem Behav 101:246–257
Cervantes-Duran C, Pineda-Farias JB, Bravo-Hernandez M, Quinonez-Bastidas GN, Vidal-Cantu GC, Barragan-Iglesias P, Granados-Soto V (2013) Evidence for the participation of peripheral 5-HT(2)A, 5-HT(2)B, and 5-HT(2)C receptors in formalin-induced secondary mechanical allodynia and hyperalgesia. Neuroscience 232:169–181
Godinez-Chaparro B, Barragan-Iglesias P, Castaneda-Corral G, Rocha-Gonzalez HI, Granados-Soto V (2011) Role of peripheral 5-HT(4), 5-HT(6), and 5-HT(7) receptors in development and maintenance of secondary mechanical allodynia and hyperalgesia. Pain 152:687–697
Blakely RD, Berson HE, Fremeau RT Jr, Caron MG, Peek MM, Prince HK, Bradley CC (1991) Cloning and expression of a functional serotonin transporter from rat brain. Nature 354:66–70
Hariri AR, Holmes A (2006) Genetics of emotional regulation: the role of the serotonin transporter in neural function. Trends Cogn Sci 10:182–191
Bowker RM, Westlund KN, Coulter JD (1981) Origins of serotonergic projections to the spinal cord in rat: an immunocytochemical-retrograde transport study. Brain Res 226:187–199
Hooten WM, Hartman WR, Black JL 3rd, Laures HJ, Walker DL (2013) Associations between serotonin transporter gene polymorphisms and heat pain perception in adults with chronic pain. BMC Med Genet 14:78
Palm F, Mossner R, Chen Y, He L, Gerlach M, Bischofs S, Riederer P, Lesch KP et al (2008) Reduced thermal hyperalgesia and enhanced peripheral nerve injury after hind paw inflammation in mice lacking the serotonin-transporter. Eur J Pain 12:790–797
Vogel C, Mossner R, Gerlach M, Heinemann T, Murphy DL, Riederer P, Lesch KP, Sommer C (2003) Absence of thermal hyperalgesia in serotonin transporter-deficient mice. J Neurosci 23:708–715
Hansen N, Uceyler N, Palm F, Zelenka M, Biko L, Lesch KP, Gerlach M, Sommer C (2011) Serotonin transporter deficiency protects mice from mechanical allodynia and heat hyperalgesia in vincristine neuropathy. Neurosci Lett 495:93–97
Kayser V, Elfassi IE, Aubel B, Melfort M, Julius D, Gingrich JA, Hamon M, Bourgoin S (2007) Mechanical, thermal and formalin-induced nociception is differentially altered in 5-HT1A−/−, 5-HT1B−/−, 5-HT2A−/−, 5-HT3A−/− and 5-HTT−/− knock-out male mice. Pain 130:235–248
Millan MJ (2002) Descending control of pain. Prog Neurobiol 66:355–474
Suzuki R, Rygh LJ, Dickenson AH (2004) Bad news from the brain: descending 5-HT pathways that control spinal pain processing. Trends Pharmacol Sci 25:613–617
Kou JP, Jin WF, Hua M, Yan YQ (2002) Effect of Danggui-Shaoyao-san (DSS) on three models of memory dysfunction. Chin Tradit Paten Med 24:191–193
Zeni AL, Zomkowski AD, Maraschin M, Rodrigues AL, Tasca CI (2012) Ferulic acid exerts antidepressant-like effect in the tail suspension test in mice: evidence for the involvement of the serotonergic system. Eur J Pharmacol 679:68–74
Qiu F, Zhong X, Mao Q, Huang Z (2013) The antidepressant-like effects of paeoniflorin in mouse models. Exp Ther Med 5:1113–1116
Lin T, Li K, Zhang FY, Zhang ZK, Light AR, Fu KY (2007) Dissociation of spinal microglia morphological activation and peripheral inflammation in inflammatory pain models. J Neuroimmunol 192:40–48
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This work was supported by the Natural Science Foundation of China (NO. 81271230), the intramural grant of form Open Project of the State Key Laboratory of Natural Medicines, China Pharmaceutical University (SKLNMKF201214) and the Natural Science Foundation of Shaanxi Province (NO. 2012JM4040).
Conflict of Interest
All the authors have viewed and agreed with this submission. The authors declare that they have no competing interests.
Ethical Approval
All experimental procedures received prior approval from the Animal Use and Care Committee for Research and Education of the Fourth Military Medical University (Xi’an, China) and the ethical guidelines to investigate experimental pain in conscious animals.
Additional information
Jun-Bin Yin, Ke-Cheng Zhou, Huang-Hui Wu and Wei Hu contributed equally to this work.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Figure 1
Fluorescent photomicrographs show neuron could express FOS, but astrocyte or microglia. (A-A2) Colocalization of NeuN (green) and FOS (red), NeuN can be seen the marker for neurons. (B-B2) Expression of GFAP (green) and FOS (red), GFAP can be seen the marker for astrocytes. (C-C2) Expression of Iba1 (green) and FOS (red), Iba1 can be seen the marker for microglias. Scale bar = 20 μm in C2 (applies A-A2, B-B2, C-C1). (GIF 207 kb)
Rights and permissions
About this article
Cite this article
Yin, JB., Zhou, KC., Wu, HH. et al. Analgesic Effects of Danggui-Shaoyao-San on Various “Phenotypes” of Nociception and Inflammation in a Formalin Pain Model. Mol Neurobiol 53, 6835–6848 (2016). https://doi.org/10.1007/s12035-015-9606-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-015-9606-3