Abstract
Real-world medication adherence and healthcare costs of patients with schizophrenia initiating long-acting injectable (LAI) vs. oral antipsychotics were compared. Patients with schizophrenia initiating LAI or oral antipsychotics (index event) were identified from MarketScan Commercial and Medicare claims databases and their medication possession ratios (MPR), pre- and post-index costs for inpatient/outpatient care were compared. Of 3,004 patients, 394 initiated LAI antipsychotics and 2,610 oral antipsychotics. Post-index, the mean MPR was greater for the LAI cohort (0.67 ± 0.34 vs. 0.56 ± 0.35; p < 0.001). Schizophrenia-related hospital costs for LAI users were reduced during the follow-up period in comparison to the pre-index period, but were increased for patients using oral antipsychotics (-$5,981 ± $16,554 vs. 758 ± 14,328, p < 0.001). The change in costs of outpatient care also favored LAI medications ($134 ± 8,280 vs. 658 ± 3,260, p = 0.023). Drug costs of LAI antipsychotics were higher ($4,132 ± 4,533 vs. 2,562 ± 2,714, p < 0.001). Schizophrenia patients initiating LAI antipsychotics incur less healthcare costs in comparison to patients initiating oral antipsychotics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Schizophrenia, is a chronic disabling mental illness that affects approximately 0.7% of the US population (2 million adults).1 Although, relatively uncommon, schizophrenia is associated with a disproportionately large economic burden, estimated at nearly $63 billion in 2002 in the US.2 A primary factor contributing to this large economic burden is that patients with schizophrenia frequently do not adhere to antipsychotic medication therapy for many reasons including, poor disease insight, negative attitude towards medication, previous nonadherence, and inadequate care.3 , 4
Antipsychotic therapy, when used continuously, can provide substantial improvement in the debilitating symptoms of schizophrenia, although approximately 37%, a low estimate in comparison to some studies, of adult patients with schizophrenia in the US experience problems with treatment adherence.5–7 Intermittent antipsychotic therapy compromises disease management and is a strong predictor of increased severity of symptoms, relapses, and rehospitalizations resulting in increased healthcare costs.8 Recently, a study conducted in patients with schizophrenia in the US reported that annual mental health costs of relapsed patients is almost three times higher than for non-relapsed patients ($33,187 ± 47,616 vs. 11,771 ± 10,611, p < 0.01).9 The higher costs were driven mostly by increased hospitalizations and length of stay in hospital, which were also accompanied by higher costs for outpatient services and medications.9
In efforts to improve nonadherence and reduce relapse incidence among patients with schizophrenia, long-acting injectable (LAI) formulations of antipsychotic medications were developed. LAI treatment requires patients to visit clinics to receive treatment every 1 to 6 weeks, eliminating the need for daily oral antipsychotic administration. There is some evidence from clinical trials that LAI antipsychotics may improve adherence to antipsychotic therapy and reduce the incidence of relapses; however, the data are inconsistent.10 , 11 These inconsistencies may be related to the design of clinical trials as patients involved in them have a greater likelihood of adhering to all antipsychotic therapy and are more closely monitored. Consequently, differences in treatment outcomes in patients using LAI antipsychotics versus oral antipsychotics may be difficult to distinguish. Moreover, clinical trial patients frequently have more stable disease and may not adequately represent the patient population with schizophrenia in the real world.12 Studies are needed in the real world where patient monitoring is usually less frequent than that conducted within the setting of a clinical trial. Furthermore, claims data from “real-world” settings would provide more realistic evidence on whether oral- or LAI-formulated antipsychotic medications improve adherence to pharmacotherapy, and thereby reduce relapse incidence, healthcare utilization, and costs among patients suffering with schizophrenia. This study aimed to compare antipsychotic medication adherence and the costs of inpatient and outpatient healthcare among large populations of commercially and Medicare-insured patients with schizophrenia, initiating LAI antipsychotics versus oral antipsychotics.
Methods
Study design
This was a retrospective cohort study with the two cohorts defined by the initiation of LAI or oral antipsychotic agents among schizophrenia patients.
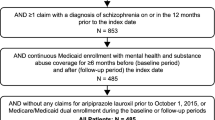
Study populations
Patients with schizophrenia who initiated the use of LAI and oral antipsychotics were identified from the Thomson Reuters MarketScan® Research Databases between 1 January 2005 and 30 September 2010. The date at which LAI or oral antipsychotic treatment was initiated was defined as the index event with the associated date as the index date. Commercially insured patients with schizophrenia were identified, and their data extracted from the Commercial Claims and Encounters Database, which contains the inpatient, outpatient, and outpatient prescription drug experience of employees and their dependents, covered under a variety of fee-for-service and capitated health plans. Medicare-insured patients were identified, and their data extracted from the Medicare Supplemental Database, which contains the healthcare experience of individuals with Medicare supplemental insurance paid for by employers.
Inclusion in either study population required that patients be ≥13 years of age at the year of index date, that they had at least one inpatient or two outpatient visits on separate dates with a primary or secondary diagnosis of ICD-9-CM code 295.X prior to the index event, and that they had at least 12 months of continuous medical and prescription drug coverage prior to the index event (baseline period), and at least 12 months of continuous medical and prescription drug coverage after the index event (follow-up period). Each of the commercially and Medicare-insured study populations were then separated into two study cohorts consisting of patients who initiated LAI antipsychotics (LAI cohort) and those who initiated oral antipsychotics (Oral cohort). Since this study did not involve “identifiable human subjects,” it was exempt from Institutional Review Board overview under the Common Rule (45 CFR §46.101(b)(4)).13
Baseline measurements
Baseline demographics, consisting of age, geographic region, health plan type, and index antipsychotic medication use when available and clinical characteristics, including Charlson Comorbidity Index (CCI) and comorbid conditions, were evaluated during the baseline period for each LAI and Oral cohort within the study populations.
Endpoint measurements
Medication adherence, inpatient, and outpatient costs, with breakdowns for all-cause and schizophrenia related were evaluated during the baseline and follow-up time periods. Inpatient and outpatient costs reflected the health plan payments for the respective medical services as reported in the claims database. A patient’s medication possession ratio (MPR) was used to describe a patient's medication adherence. The MPR was calculated as the total number of days of drug supply during the study time period, divided by the total number of days in the baseline or follow-up periods, and reported as the mean ± standard deviation. The mean costs ± standard deviation of inpatient treatment and outpatient services for all-cause- and schizophrenia-related treatment and antipsychotic medication costs, were determined for the baseline and follow-up periods and compared within each cohort of the study populations. The differences between inpatient and outpatient costs between the follow-up and baseline time periods were also compared among the LAI and Oral cohorts within each study population at both the unadjusted and adjusted levels.
Statistical analyses
Descriptive statistics were used to evaluate differences in patient demographics and clinical characteristics, with p values provided by Chi-square and t tests when appropriate. Descriptive statistics were also used to determine significant differences between follow-up and baseline healthcare costs of LAI and Oral cohorts and whether these differences significantly differed among the LAI and Oral cohorts by t test. A generalized linear model was used to carry out multivariate regression to evaluate the impact of initiating LAI versus oral antipsychotics on hospitalization costs between follow-up and baseline periods. The analysis accounted for the following covariates: age, gender, region, health plan type, CCI, and index antipsychotic drug. A p value of 0.05 was used to determine the level of statistical significance. All statistical analyses were carried out using SAS 9.2.
Results
Study populations
For the commercially insured study population, 3,004 patients with schizophrenia were identified who started treatment with an oral or LAI antipsychotic; 394 (13%) initiated LAI antipsychotics and 2,610 (87%) initiated oral antipsychotics. For the Medicare-insured study population, 665 patients with schizophrenia were similarly identified of whom 147 (22%) initiated LAI antipsychotics and 518 (78%) initiated oral antipsychotics.
Demographics of patient cohorts in study populations
Commercially insured patients with schizophrenia who initiated LAI antipsychotics were older (41.7 vs. 37.1 years, p < 0.001), and a greater proportion had comprehensive healthcare coverage (18.8 vs. 9.8%, p < 0.001) in comparison to those who initiated oral antipsychotics (see Table 1). Also, a smaller proportion of the LAI cohort had Health Maintenance Organization (17.8 vs. 26.1%, p < 0.001) or Point-of-Service (9.6 vs. 13.0%, p < 0.001) health plan coverage. The majority of patients in the LAI cohort lived in North Central USA (47.0 vs. 29.5%, p < 0.001) while more patients initiating oral antipsychotics were located in Western USA (24.9 vs. 9.4%, p < 0.001). Among those who were Medicare insured, patients who initiated oral antipsychotic medications were older (73.2 vs. 67.2 years, p < 0.001), but similar to the commercially insured patient population, the majority of patients in the LAI cohort lived in North Central USA (66.7 vs. 44.8%, p < 0.001) while more patients initiating oral antipsychotic medications were located in Western USA (15.6 vs. 2.7%, p < 0.001). All evaluated demographics for both the commercially insured and Medicare insured study populations are reported in Table 1.
Clinical characteristics of patient cohorts in study populations (see Table 2)
The mean CCI score was greater, but nonsignificantly so for the LAI cohort versus the Oral cohort of the commercially insured study population (0.58 ± 1.10 vs. 0.47 ± 1.08, p = 0.056). Also, a larger proportion of patients initiating LAI antipsychotics were diagnosed with diabetes (15.0 vs. 9.7%, p = 0.001) or peripheral vascular disease (2.3 vs. 1.0%, p = 0.026) in comparison to patients initiating oral antipsychotics. Chronic pulmonary disease was a common comorbidity of patients in both the LAI and Oral cohorts (12.2 vs. 11.5%, p = 0.707).
In contrast to the commercially insured study population, patients within the Medicare-insured study population who initiated oral antipsychotics had significantly higher CCI scores (1.83 vs. 1.24, p < 0.001). Also, they more often had peripheral vascular disease (11.6 vs. 5.4%, p = 0.0301), cerebrovascular disease (24.5 vs. 12.9%, p = 0.003), dementia (19.7 vs. 11.6%, p = 0.023), and cancer (9.1 vs. 2.7%, p = 0.011) in comparison to patients in the LAI cohort. Similar to the commercially insured study population, the most common comorbid conditions among both LAI and Oral patient cohorts insured by Medicare were diabetes (27.9 vs. 26.1%, p = 0.657) and chronic pulmonary disease (21.8 vs. 23.8%, p = 0.617). All evaluated clinical characteristics for both the commercially and Medicare-insured study populations are reported in Table 2.
Medication adherence of patient cohorts in study populations
During the follow-up period, medication adherence was significantly greater than during the baseline period among patients who initiated LAI antipsychotics for both the commercially- (0.67 ± 0.34 vs. 0.40 ± 0.37, p < 0.001) and Medicare-insured (0.68 ± 0.34 vs. 0.42 ± 0.39, p < 0.001) study populations (Table 3). Also, when comparing medication adherence of LAI cohorts versus Oral cohorts during the follow-up period, adherence was found to be greater among the LAI cohorts of both the commercially- (0.67 ± 0.34 vs. 0.56 ± 0.35, p < 0.001) and Medicare-insured study populations (0.68 ± 0.34 vs. 0.59 ± 0.36, p = 0.005).
Differences between follow-up and baseline healthcare costs of LAI and Oral cohorts (see Table 3)
The mean costs for inpatient care for any cause ($7,518 ± 24,510 vs. 14,976 ± 18,976, p < 0.001) and schizophrenia related ($4,109 ± 10,788 vs. 10,089 ± 14,346, p < 0.001) were significantly reduced during the follow-up period in comparison to the baseline period for commercially insured LAI patients. Mean costs for outpatient services, all-cause ($6,329 ± 10,988 vs. 6,364 ± 12,112 p = 0.966) and schizophrenia related ($2,002 ± 5,606 vs. 1,868 ± 9,811, p = 0.814) did not significantly differ between the follow-up and baseline periods for commercially insured LAI patients. Similarly, a significant reduction in inpatient healthcare costs was observed from the follow-up to baseline time period, but not for outpatient cost differences, among Medicare-insured patients who initiated LAI antipsychotics. The mean costs of antipsychotic prescriptions ($4,132 ± 4,533 vs. 1,885 ± 2,618, p < 0.001) significantly increased during the follow-up period in comparison to the baseline period for commercially insured patients in the LAI cohort, a trend also observed for Medicare insured patients within the LAI cohort.
For patients in the commercially insured Oral cohort, the mean costs for inpatient care for any cause remained similar during the follow-up period in comparison to the baseline period; however, there was a significant increase in cost for schizophrenia-related hospitalizations during the follow-up period ($4,149 ± 11,586 vs. 3,391 ± 8,545, p = 0.007). Mean costs for all-cause- ($6,866 ± 10,291 vs. 5,077 ± 8,416, p < 0.001) and schizophrenia-related outpatient services ($988 ± 2,977 vs. 331 ± 1,380, p < 0.001) were higher during the follow-period in comparison to the baseline period for commercially insured patients in the Oral cohort as well. Medicare-insured patients within the Oral cohort did not have significant differences in healthcare costs between the follow-up and baseline time periods.
Differences in mean costs for healthcare between follow-up and baseline time periods for LAI versus Oral cohorts
For patients initiating LAI antipsychotics versus oral antipsychotics, the mean costs of antipsychotic prescriptions ($4,132 ± 4,533 vs. 2,562 ± 2,714, p < 0.001) were greater by $1,570 during the follow-up period. Reported in Figure 1 are the differences in mean costs for (a) hospitalizations and (b) outpatient services, all-cause and schizophrenia related for the study populations between the follow-up and baseline time periods. Among the commercially insured population, differences in mean costs between the follow-up and baseline periods for hospitalizations for any cause- (-$7,458 ± 29,774 vs. 623 ± 24,190, p < 0.001) and schizophrenia-related hospitalizations (-$5,981 ± 16,554 vs. 758 ± 14,328, p < 0.001) were substantially greater for patients in the LAI cohort versus Oral cohort. Also, while patients within the LAI cohort had reductions in inpatient costs, patients within the Oral cohort had increased inpatient costs during the follow-up period in comparison to baseline. The greater reductions in costs for inpatient care from the baseline to follow-up periods were also significant for Medicare-insured patients initiating LAI versus oral antipsychotic medications.
Among the commercially insured population, patients within the LAI cohort had a small reduction in their mean cost for outpatient services for any cause incurred during the follow-up period compared with baseline (-$35 ± 12,868 vs. 1,789 ± 9,970, p = 0.001), while this cost increased for patients within the Oral cohort. The difference in outpatient cost of schizophrenia-related services from the follow-up to baseline time periods were also significantly less for commercially insured patients initiating LAI versus oral antipsychotics ($134 ± 8,280 vs. 658 ± 3,260, p = 0.023).
Differences in hospitalization costs based on multivariate regression analysis
After control for patient characteristics, the differences in hospitalization costs were confirmed for both the Commercial and Medicare populations. The estimated cost difference (follow-up − baseline) for all-cause hospitalization between the commercially insured LAI and Oral cohorts was −$8,207 (95% CI upper and lower, −$4,971 and −11,443, p < 0.001) and for schizophrenia-related hospitalization was −$6,566 (95% CI, −$4,669 and −8,463, p < 0.001). The estimated cost difference for all-cause hospitalization for the Medicare-insured LAI and Oral cohorts was −$11,485 (95% CI, -$4,236 and -18,734, p = 0.002) and for schizophrenia-related hospitalization was −$5,468 (95% CI, −$2,136 and -8,800, p = 0.001).
Discussion
The present study shows that real-world patients with schizophrenia, who initiated LAI antipsychotic medications versus oral antipsychotic medications, independent of whether they were commercially insured or Medicare insured, had better adherence to antipsychotic medications, and a greater reduction in healthcare costs 12 months after initiation of treatment in comparison to 12 months before treatment initiation. Also, there were important differences in patient characteristics among those who received LAI antipsychotics versus oral antipsychotics between commercially and Medicare-insured populations.
Commercially insured patients using LAI antipsychotics were older, and there was a trend for having increased comorbidity, represented by CCI score in comparison with patients using oral antipsychotics. In contrast, Medicare-insured patients using LAI antipsychotics were younger and had significantly less comorbid conditions than patients using oral antipsychotics. The differences in demographics and clinical characteristics between commercially and Medicare-insured users of the different formulations of antipsychotic medications suggests different incentives may be required for increasing antipsychotic adherence among patients with schizophrenia who are commercially insured, versus those who are publicly insured. Among the commercially insured study population, initiation of LAI antipsychotics is potentially later in the course of schizophrenia, whereas, in the Medicare population, the use of LAIs could be related to the presence or absence of comorbid conditions.
LAI antipsychotics were only initiated by 13% of commercially insured patients in comparison to 22% of Medicare-insured patients with schizophrenia. As in this study, public insurance has been previously associated with greater LAI antipsychotic usage, suggesting that socioeconomic status may be one factor contributing to drug/prescribing choice.14 Another potential factor may be that commercial insurance places more emphasis on price than public insurance and based on drug price alone there is less incentive to prescribe LAI antipsychotics to those who are commercially insured. Similar to previous studies, commercially and Medicare-insured patients who initiated LAI antipsychotics had less stable disease as indicated by their higher costs for schizophrenia-related care prior to initiating antipsychotic medication.15 , 16 For patients initiating LAI antipsychotics adherence to oral antipsychotic therapy was low (mean baseline MPR = 0.40) providing more evidence that nonadherence is strongly associated with increased risk for relapses and hospitalizations and greater cost for care.8 LAI antipsychotics are recommended for patients with schizophrenia who have a history of nonadherence, which as mentioned is widespread among patients with schizophrenia, as up to 80% of patients will experience problems adhering to antipsychotic therapy at some period during their illness.7 , 17 , 18 However, it appears from this study, alongside others that LAI antipsychotics are underused in current clinical practice, despite evidence-based recommendations for patients with a history of nonadherence.14 , 18 , 19
During the follow-up period medication, adherence increased nearly 1.7-fold from that during the baseline period for both commercially and Medicare-insured patients who initiated LAI antipsychotics. Moreover, medication adherence was between 15 and 20% greater for patients using LAI antipsychotics in comparison to those using oral antipsychotics. Likely associated with improved adherence to antipsychotic therapy, the costs for inpatient care, all-cause and schizophrenia related were markedly less during the follow-up period in contrast to before-treatment initiation for patients using LAI antipsychotics. Thus, patients with greater schizophrenia severity may have a greater benefit if initiation of LAI antipsychotics occurred earlier in disease progression given their increased adherence and observed scale of healthcare resource and relapse reduction, as represented by healthcare costs. According to the results presented herein, for every 5,000 patients who initiate LAI versus oral antipsychotics who are covered by private insurance there would be a hospital savings of over $18 million annually and for those covered by Medicare over $15 million annually for schizophrenia-related hospitalizations when taking into account the higher cost of LAI antipsychotic medications.
Hospital care of patients with any mental illness declined from 1992 to 2002, but rehospitalization rates remained the same for patients with schizophrenia.20 A review of seven studies addressing the economic impact of nonadherence among patients with schizophrenia who are covered by Medicaid estimated US rehospitalization costs in 2005 at $1.5 billion.8 It is important to address this enormous societal burden of schizophrenia by improving medication adherence using multiple strategies on many fronts, such as implementing better ways of administering antipsychotic therapy for high risk patient populations, increasing patient monitoring, improving access to outpatient mental health centers, and increasing the emphasis on community-based social therapy.
LAI antipsychotics cost more than oral antipsychotics when only drug costs are considered, and for this reason among others, such as psychiatrist presumption of sufficient adherence among their patient populations are prescribed to a much lesser extent than oral antipsychotics.21 Medical costs, predominately inpatient costs associated with relapses are far greater than drug costs for patients with schizophrenia and their avoidance is a priority of healthcare reform.22 When comparing the cost effectiveness of therapeutics it is important to consider whether medical costs are avoided, especially in a real-world setting where drugs associated with greater medical cost reductions have the potential to improve healthcare delivery while controlling cost. The present study did not include indirect costs, which will need to be studied further as improved medication adherence and a reduction in the incidence of relapses will likely allow for patients who choose LAI antipsychotic medications to function better socially, maintain a job with less absenteeism, abuse substances to a lesser degree and be involved in less violence, all of which could potentially contribute towards a large reduction in the indirect costs of schizophrenia, which in 2002 were estimated at $32.4 billion in the US.2
While the present study provides valuable insight into the real-world healthcare impact of initiating LAI versus oral antipsychotic medications for the treatment of schizophrenia, as with all studies utilizing healthcare databases, there are inherent limitations. The MarketScan databases consist of claims submitted by healthcare providers to insurance companies or the government for reimbursement and such claims are subject to possible coding errors, coding for the purpose of rule-out rather than actual disease, and undercoding, either by the healthcare provider or due to limitations imposed by the database. Changes in employment status or employer can limit the amount of continuous data available and consequently, constrain the study sample sizes available for analysis. In addition, the MarketScan claims databases are based on large convenience samples. Because the samples are not random, they may contain biases or fail to generalize well to other populations, particularly those who have alternate healthcare coverage such as Medicaid or those who are uninsured. Additionally, the demographics and clinical characteristics of the patients recorded in the MarketScan databases may not match with the overall US population. Another limitation of these databases are that the drug claims data reflect only that a patient has a prescription and administration cannot be verified. Therefore, MPR may overestimate patient adherence as it reflects drug availability and not actual drug administration. Although, the MPR does have a time component and is a widely used method of estimating medication adherence for database studies. Other limitations of this study are that it did not address cost-wise some of the concerns associated with LAI antipsychotics, such as delayed onset of action, short-term oral antipsychotic co-administration, the facilities and skills required for injectable administration, or how best to accomplish switching from oral antipsychotics to LAI antipsychotics. Lastly, in comparisons between LAI and Oral cohorts, treatment assignment was not achieved by randomization, but selected based on real-world treatment initiation. Patients initiating LAI antipsychotics were likely switching from an oral agent, whereas patients initiating oral antipsychotics were likely newly diagnosed with schizophrenia. This was viewed as a conservative comparison as newly schizophrenia diagnosis usually follows acute decompensated disease, a more severe state than the reasons for switching medications.
Implications for Behavioral Health
In real-world patients with schizophrenia, regardless of whether they have private or public health insurance, those who initiate LAI versus oral antipsychotic medications have better adherence to antipsychotic therapy and a greater reduction in healthcare expenditures after initiation of treatment versus before treatment initiation. The substantial savings for hospitals provides a strong economic rationale for using LAI antipsychotics, already an evidence-based practice, as an alternative therapy for nonadherent patients with schizophrenia.
References
Horvitz-Lennon M, Donohue JM, Domino ME, et al. Improving quality and diffusing best practices: the case of schizophrenia. Health Affairs 2009;28(3):701–12.
Wu EQ, Birnbaum HG, Shi L, et al. The economic burden of schizophrenia in the United States in 2002. The Journal of Clinical Psychiatry 2005;66(9):1122–9.
Lambert T, Olivares JM, Peuskens J, et al. Effectiveness of injectable risperidone long-acting therapy for schizophrenia: data from the US, Spain, Australia, and Belgium. Annals of General Psychiatry 2011;10:10.
Lacro JP, Dunn LB, Dolder CR, et al. Prevalence of and risk factors for medication nonadherence in patients with schizophrenia: a comprehensive review of recent literature. The Journal of Clinical Psychiatry 2002;63(10):892–909.
West JC, Wilk JE, Olfson M, et al. Patterns and quality of treatment for patients with schizophrenia in routine psychiatric practice. Psychiatric Services 2005;56(3):283–91.
Valenstein M, Copeland LA, Owen R, et al. Adherence assessments and the use of depot antipsychotics in patients with schizophrenia. The Journal of Clinical Psychiatry 2001;62(7):545–51.
Kelin K, Lambert T, Brnabic AJ, et al. Treatment discontinuation and clinical outcomes in the 1-year naturalistic treatment of patients with schizophrenia at risk of treatment nonadherence. Patient Preference and Adherence 2011;5:213–22.
Sun SX, Liu GG, Christensen DB, et al. Review and analysis of hospitalization costs associated with antipsychotic nonadherence in the treatment of schizophrenia in the United States. Current Medical Research and Opinion 2007;23(10):2305–12.
Ascher-Svanum H, Zhu B, Faries DE, et al. The cost of relapse and the predictors of relapse in the treatment of schizophrenia. BMC psychiatry 2010;10:2.
Adams C E, Fenton MKP, Quraishi S, et al. Systematic meta-review of depot antipsychotic drugs for people with schizophrenia. The British Journal of Psychiatry 2001;179(4):290–299.
Gaebel W, Schreiner A, Bergmans P, et al. Relapse prevention in schizophrenia and schizoaffective disorder with risperidone long-acting injectable vs quetiapine: results of a long-term, open-label, randomized clinical trial. Neuropsychopharmacology 2010;35(12):2367–77.
Rosenheck RA, Krystal JH, Lew R, et al. Long-acting risperidone and oral antipsychotics in unstable schizophrenia. The New England Journal of Medicine 2011;364(9):842–51.
US Department of Health and Human Services. Code of Federal Regulations. Human Subjects Research (45 CFR 46).
West JC, Marcus SC, Wilk J, et al. Use of depot antipsychotic medications for medication nonadherence in schizophrenia. Schizophrenia Bulletin 2008;34(5):995–1001.
Shi L, Ascher-Svanum H, Zhu B, et al. Characteristics and use patterns of patients taking first-generation depot antipsychotics or oral antipsychotics for schizophrenia. Psychiatric Services 2007;58(4):482–8.
Bernardo M, San L, Olivares JM, et al. Treatment patterns and health care resource utilization in a 1-year observational cohort study of outpatients with schizophrenia at risk of nonadherence treated with long-acting injectable antipsychotics. Patient Preference and Adherence 2011;5:601–10..
Lehman AF, Kreyenbuhl J, Buchanan RW, et al. The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophrenia Bulletin 2004;30(2):193–217.
Lehman AF, Steinwachs DM. Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 1998;24(1):1–10.
Ascher-Svanum H, Peng X, Faries D, et al. Treatment patterns and clinical characteristics prior to initiating depot typical antipsychotics for nonadherent schizophrenia patients. BMC Psychiatry 2009;9:46.
Akincigil A, Hoover DR, Walkup JT, et al. Hospitalization for psychiatric illness among community-dwelling elderly persons in 1992 and 2002. Psychiatric Services 2008;59(9):1046–8.
Heres S, Hamann J, Kissling W, et al. Attitudes of psychiatrists toward antipsychotic depot medication. The Journal of Clinical Psychiatry 2006;67(12):1948–53.
Yu AP, Atanasov P, Ben-Hamadi R, et al. Resource utilization and costs of schizophrenia patients treated with olanzapine versus quetiapine in a Medicaid population. Value in Health: the Journal of the International Society for Pharmacoeconomics and Outcomes Research 2009;12(5):708–15.
Conflict of Interest
Declaration of funding—this research was supported by Otsuka America Pharmaceutical, Inc. and H. Lundbeck A/S. Declaration of financial/other relationships—Jay Lin is an employee of Novosys Health, which has received research funds from Otsuka America Pharmaceutical, Inc. in connection with conducting this study and development of this manuscript. Bruce Wong is a paid consultant for Otsuka America Pharmaceutical, Inc. in connection with conducting this study and development of this manuscript. Steve Offord and Dario Mirski are employees of Otsuka America Pharmaceutical, Inc.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, J., Wong, B., Offord, S. et al. Healthcare Cost Reductions Associated with the Use of LAI Formulations of Antipsychotic Medications Versus Oral Among Patients with Schizophrenia. J Behav Health Serv Res 40, 355–366 (2013). https://doi.org/10.1007/s11414-013-9329-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11414-013-9329-z