Abstract
This study aims to explore the association of combined exposure to cooking fuel type and ambient ozone (O3) levels with hepatic fibrosis indices among rural adults. A total of 21,010 participants were derived from the Henan Rural Cohort. Information regarding cooking fuel type was collected through a questionnaire, and the concentration of ground-level O3 for each subject was obtained from the Tracking Air Pollution in China (TAP) dataset. A generalized linear model was used to examine the independent association of cooking fuel type or O3 exposure with hepatic fibrosis indices (FIB-4, APRI, and AST/ALT), and their possible interactions with advanced fibrosis were conducted. Compared to clean fuel users, solid fuel users had increased the risk of advanced fibrosis, the adjusted odds ratio (OR) of its assessment by FIB-4 1.240 (1.151, 1.336), by APRI 1.298 (1.185, 1.422), and by AST/ALT 1.135 (1.049, 1.227), respectively. Compared to low O3 exposure, the adjusted ORs of advanced fibrosis assessed by FIB-4, APRI, and AST/ALT in women with high O3 exposure were correspondingly 1.219 (1.138, 1.305), 1.110 (1.017, 1.212), and 0.883 (0.822, 0.949). The adjusted ORs of advanced fibrosis assessed by FIB-4, APRI, and AST/ALT for solid fuel users with high O3 exposure relative to clean fuel users with low O3 exposure in women were 1.557 (1.381, 1.755), 1.427 (1.237, 1.644), and 0.979 (0.863, 1.108), respectively. Significant additive effect of O3 exposure and solid fuel use on FIB-4-defined advanced fibrosis was observed in women, which was quantified by RERI (0.265, 95%CI: 0.052, 0.477), AP (0.170 95%CI: 0.045, 0.295), and SI (1.906, 95%CI: 1.058, 3.432). Solid fuel users with high O3 exposure were significantly associated with elevated hepatic fibrosis indices among rural women, suggesting that poor air quality may induce hepatocellular injury, and women might be more vulnerable to air pollution. The findings indicate that using cleaner fuels in cooking is an effective measure to maintain sustainable development of the environment and gain beneficial effect on human health. Clinical trial registration: The Henan Rural Cohort Study has been registered at the Chinese Clinical Trial Register (registration number: ChiCTR-OOC-15006699). Date of registration: 06 July 2015. http://www.chictr.org.cn/showproj.aspx?proj=11375
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Air pollution is a silent killer of human health and has become a great public concern in past decades (Cohen et al. 2017; Miller 2020). Since the promulgation of the air pollution prevention and control plan has come into act in China from 2013, other air pollutants have significantly improved, but the ozone (O3) level has remained consistently high (Han et al. 2020; Wang et al. 2022). Recently growing evidence suggests that exposure to O3 in association with adverse health effects has extended to multiple organ systems (Theis et al. 2014), such as the respiratory system (Gu et al. 2020) and cardiovascular system (Kazemiparkouhi et al. 2020), but its harmful effect on liver is not neglected and has attracted more attention for research (Alewel et al. 2021). Thus, it is an urgent need to identify the effect of O3 exposure on early biomarkers of liver function, which may give us a chance to take effective action to prevent the occurrence of chronic liver disease.
Non-invasive markers may be valuable and costless to identify individuals who are more likely to develop severe liver events, which may have high ability to predict physician-diagnosed severe liver-related outcomes (Lee et al. 2021). EASL-EASD-EASO clinical practice guidelines have recommended that fibrosis-4 (FIB-4), aspartic aminotransferase (AST)/ platelet count (PLT) ratio index (APRI), and other non-invasive biomarkers can be used to predict fibrosis staging and liver-related events (EASL. et al. 2016; Siddiqui et al. 2019). Liver fibrosis is characterized by abnormal proliferation of connective tissue in the liver (Nah et al. 2021; Toosi 2015), and it is rarely diagnosed before cirrhosis because it is asymptomatic in human. It is well known that liver fibrosis plays a vital role in developing cirrhosis and hepatocellular carcinoma (Watt et al. 2019), and population-based studies have furthermore indicated that hepatic fibrosis is an important predictor of liver-related mortality and all-cause mortality (Long et al. 2021). However, studies of the effects of air pollution on liver damage have been inadequate (Guo et al. 2022; Hou et al. 2022; Pejhan et al. 2019). Since air polltants can interact and permeate with each other to maintain dynamic balance, people are inevitably exposed to indoor and outdoor air pollution in daily life (Chafe et al. 2014). About one-third of indoor air pollution (IAP) was derived from the uncompleted combustion of domestic solid fuel (Li et al. 2017), and it might contribute to increased outdoor air pollution level (Yun et al. 2020). IAP is related to increased risk of chronic diseases such as cancer and chronic liver disease (Yusuf et al. 2020). Moreover, animal studies have found that O3 or fine particulate matter (PM2.5) may cause metabolic disorders, e.g., glucose and lipid metabolism, as well as expression of specific proteins in rats by inducing the same mechanisms of oxidative stress and inflammation in liver cells (Miller 2020; Theis et al. 2014; Xu et al. 2019). It is noted that harmful substances inhaled in air are metabolized in the liver and induce liver injury because the liver is the major detoxifying organ in the body (Ya et al. 2018). The association of O3 exposure with liver dysfunction is little investigated and its interaction with IAP on liver dysfunction is urgently explored, which may provide more accuracy to assess air pollution-related liver dysfunction.
In this paper, we examined a large-scale health survey data of rural adults in China to explore the associations of ambient O3 exposure, indoor cooking fuel type use, and their possible interaction effects with hepatic fibrosis indices (FIB-4, APRI, and AST/alanine aminotransferase (ALT)). The findings of this study may provide some clues to identify the O3-related liver dysfunction and provide the corresponding effective control measures.
Method
Study population
The study participants were derived from the baseline survey of the Henan Rural Cohort Study, which was carried out between July 2015 and September 2017 in Henan province, China. In brief, a questionnaire was used to collect personal information, socioeconomic status, daily lifestyle, physical health status, etc., and the results of physical examination were recorded for each participant, including anthropometric measurements (such as height, weight, blood pressure, and body fat rate) and blood biochemical test (such as fasting blood glucose, cholesterol, AST, and ALT), and detailed introduction of study design and data collection was described elsewhere (Liu et al. 2019). In this study, after excluding participants with viral hepatitis or without measurement of hepatic fibrosis indices (n=9806), and participants without cooking (n=8378) or partially missing cooking-related information (n=65), a total of 21,010 eligible cooking participants were ultimately included. The characteristics of excluded and included study population are shown in supplementary materials (Table S1). Ethical approval from the Zhengzhou University Life Science Ethics Committee (Code: [2015] MEC (S128)) was received, and the written informed consent from each participant was obtained prior to this study.
Covariates
The covariates included in the analysis are age (continuous), gender (male or female), educational levels (elementary school or below, middle school, and high school or above), marital status (married/cohabitating and unmarried/divorced/widowed), average monthly income (<500RMB, 500-999RMB, and ≥1000RMB), smoking status (never, former, and current smokers), drinking status (never, former, and current drinkers), body mass index (BMI, continuous), physical activity (low, middle, and high) (Tu et al. 2019), and chronic diseases status (type 2 diabetes mellitus (T2DM), coronary heart disease (CHD), and stroke). The diagnostic criteria of T2DM are as follows: participants had fasting blood glucose ≥7.0 mmol/L, or self-reported physician-diagnosed of T2DM and treated with hypoglycemic medications at the same time (Kang et al. 2022). CHD was defined by the self-reported physician diagnosed of CHD (Wang et al. 2019). The information regarding meat fat intake, fruit, and vegetable consumption in the past year was collected by the frequency questionnaire (grams and frequency), which had been confirmed to be suitable for rural adults (Xue et al. 2020b).
Assessment of exposure
The information regarding cooking fuel type was collected by a questionnaire which has been validated in the previous study (Pan et al. 2021). Participants were classified into clean fuel use (natural gas, gas, and electricity) and solid fuel use group (coal and wood) two groups, according to the primary fuel type used for household cooking.
The O3 exposure concentration of each participant was obtained from Tracking Air Pollution in China data set in China (Xue et al. 2020a), which integrated O3 observation data, satellite remote sensing O3 vertical profile, community multi-scale air quality (CMAQ) simulation, weather research and forecasting (WRF) simulation, vegetation index, night light, and population data by using multiple methods including random forest model, elastic net regression model, and the spatiotemporal variance-covariance function. And the spatial resolution of the WRF-CMAQ model is 36 km × 36 km (Xiao et al. 2022), which was verified by using the daily 8-h average surface O3 monitoring data from 1666 stations of the China Environmental Monitoring Center and showed a good prediction ability which indicated by the R2 (R2=70%) and root mean squared errors (RMSE: 29%) of 5-fold cross-validation. Ground-level O3 data for the 3 years prior to the survey date were obtained according to the longitude and latitude of the participant’s residential location, and the average value was calculated and matched as the O3 exposure level of the participant. The O3 exposure was classified into low (<93.07μg/m3) or high (≥ 93.07μg/m3) level by results from restricted cubic spline for subsequent analysis (Fig. S1).
Definition of hepatic fibrosis indices
After at least 8 h of fasting, peripheral venous blood samples were drawn from each participant by a trained nurse using a disposable syringe and stored in a dimethylamine tetraacetic acid tube. Blood routine such as PLT and blood biochemical indexes such as AST and alanine aminotransferase (Dai et al. 2021) were simultaneously detected on the same day by using the XS-500i (SYSMEX, Japan) and Cobas c501 (Roche, Switzerland), respectively. A total of 10% of the samples were measured twice with a coefficient of variation of less than 10% (Yusuf et al. 2020).
Hepatic fibrosis indices were evaluated by using the following formula and classified into low and intermediate-high advanced fibrosis based on previous studies’ reported cutoff values: FIB-4 score = (age (year) × AST (U/L)) / [PLT (109/L) × ALT1/2(U/L)], the cutoff points of low and intermediate-high advanced fibrosis for participants aged <65 years old was 1.3, and ≥65 years old was 2.0 (Hou et al. 2022). APRI = [(AST / the upper limit of normal (ULN)) / PLT (109/L)] × 100 (Pan et al. 2021), the cutoff value of APRI identified participants with low and intermediate-high advanced fibrosis was 0.5 (Dai et al. 2021; Xue et al. 2020a). The cutoff value of AST/ALT identified participants with low and intermediate-high advanced fibrosis was 1.5 (Hou et al. 2022).
Statistical analysis
The continuous and categorical variables were expressed as mean ± standard deviation (SD) and number (percentage), respectively. Student’s t-test and chi-squared test were used to compare the differences of continuous or categorical variables between low and intermediate-high advanced fibrosis groups, respectively. Generalized linear models were used to estimate β values or odds ratios (ORs) and corresponding 95% confidence intervals (CIs) of independent or combined associations of cooking fuel type and ambient O3 exposure with hepatic fibrosis indices reflected by FIB-4, APRI, and AST/ALT, and the potential additive and multiplicative interaction of the two exposures on advanced fibrosis. The quantitative interactions were indicated by the relative excess risk (RERI) and the attributable proportion (AP) of risk due to interaction and synergy index (SI). Covariates were adjusted in three models: Model 1 was unadjusted; Model 2 was adjusted for age, marital status, educational level, and average monthly income in the group of men or women, and gender was added to the total population; and Model 3 was an additional adjustment for lifestyles (smoking- and drinking status, physical activity, high-fat diet, vegetable, and fruit intake), BMI, and chronic diseases status including T2DM, CHD, and stroke. All data analyses were performed by using the SPSS Software (version 26.0, IBM-SPSS Inc., Armonk, NY) and R software version 4.2.1. Statistical significance was set as a two-tailed P value less than 0.05.
Result
Characteristics of the study population by hepatic fibrosis status
Table 1 presents the characteristics of participants with low and intermediate-high advanced fibrosis. Participants with intermediate-high advanced fibrosis were more likely to be female, be less educated, be married, never smoke or drink alcohol, have less high-fat diet, more fruit and vegetable intake, a small number of participants with T2DM, CHD, and stroke, and use clean fuel on cooking in the total population. When we observed the characteristics of the population grouped by FIB-4, APRI, and AST/ALT, respectively, differences by FIB-4 in the selected variables were observed between the two groups (all P<0.05). Although there were no differences in the distribution of marital status, high-fat diet, and T2DM between two groups of low and intermediate-high advanced fibrosis identified by APRI, the differences in the distributions of the other selected variables between the two groups were significant (all P<0.05). There were no differences in the distributions of physical exercise, CHD, stroke, and O3 level between two groups of low and intermediate-high advanced fibrosis identified by the AST/ALT ratio values, but the differences in the distributions of the other selected variables were significant (all P<0.05).
Independent associations of cooking fuel type or ambient O3 exposure with advanced fibrosis assessed by hepatic fibrosis indices
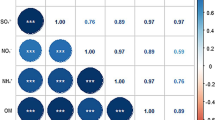
As shown in Fig. 1, the estimated β values for FIB-4, APRI, and AST/ALT in response to solid fuel users versus clean fuel users in all participants were 0.426 (95% CI: 0.372, 0.480), 0.048 (95% CI: 0.031, 0.065), and 0.064 (95% CI: 0.047, 0.081), respectively (Model 1). And the estimated β values for FIB-4, APRI, and AST/ALT in response to solid fuel users versus clean fuel users in women were 0.385 (95% CI: 0.334, 0.436), 0.046 (95% CI: 0.028, 0.064), and 0.038 (95% CI: 0.019, 0.058), respectively (Model 1).
Independent associations of cooking fuel type or ambient O3 exposure with hepatic fibrosis indices. Estimated β values or ORs and 95%CIs in clean fuel, solid fuel, low O3, and high O3 groups were represented by the corresponding black dot (black lines), gray square (gray lines), orange triangle (orange lines), and blue rhombus (blue lines), respectively.
The estimated ORs of advanced fibrosis assessed by FIB-4, APRI, and AST/ALT in response to solid fuel users versus clean fuel users were 1.680 (95% CI: 1.568, 1.799), 1.518 (95% CI: 1.391, 1.654), and 1.284 (95% CI: 1.192, 1.382), respectively (Model 1). The estimated ORs of advanced fibrosis assessed by FIB-4, APRI, and AST/ALT in response to solid fuel users versus clean fuel users in women were 1.605 (95% CI: 1.485, 1.734), 1.502 (95% CI: 1.363, 1.654), and 1.144 (95% CI: 1.052, 1.242), respectively (Model 1). Similar results were observed in Models 2 and 3, which included more covariables for adjustment. The estimated ORs of advanced fibrosis assessed by FIB-4 and APRI in response to high O3 exposure versus low level of O3 exposure in all participants were 1.429 (95% CI: 1.352, 1.511) and 1.309 (95% CI: 1.216, 1.410) (Model 1). The estimated ORs of advanced fibrosis assessed by FIB-4 and APRI in response to solid fuel users versus clean fuel users in women were 1.393 (95% CI: 1.308, 1.485) and 1.310 (95% CI: 1.206, 1.424) (Model 1). Similar results were observed in Models 2 and 3, which included more covariables for adjustment.
Interactive associations of cooking fuel type and ambient O3 exposure with the risk of hepatic fibrosis
Table 2 presents the additive and multiplicative interaction effects of cooking fuel type and ambient O3 exposure with the risk of hepatic fibrosis. Significant multiplicative interaction effect of cooking fuel type and O3 exposure on the risk of hepatic fibrosis reflected by FIB-4 in women was found (P interaction=0.04). Significant additive interaction of cooking fuel type and O3 exposure on the risk of advanced fibrosis reflected by FIB-4 in women was also found, and the matched figures of RERI was 0.265 (95% CI: 0.052, 0.477), indicating that relative excess risks were attributed to the additive synergistic effect of solid fuel use and high O3 exposure on advanced fibrosis risk; of AP was 0.170 (95% CI: 0.045, 0.295), representing that 17.0% additional risk of advanced fibrosis risk may be attributable to the synergistic effect of solid fuel use and high O3 exposure; of SI was 1.906 (95% CI: 1.058, 3.432), indicating the synergistic effect of solid fuel use and high O3 exposure on advanced fibrosis risk.
Combined associations of cooking fuel type and ambient O3 exposure with advanced fibrosis assessed by hepatic fibrosis indices
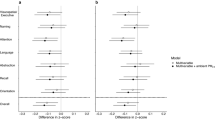
Figure 2 exhibits the combined associations of cooking fuel type and ambient O3 exposure with hepatic fibrosis indices. Compared to clean fuel user with low O3 exposure, the estimated β values of FIB-4 in solid fuel users with low O3 exposure or solid fuel users with high O3 exposure in women were 0.346 (95% CI: 0.276, 0.415) or 0.496 (95% CI: 0.423, 0.570); the matched figures for APRI were 0.034 (95%CI: 0.010, 0.058) or 0.073 (95% CI: 0.047, 0.098) (Model 1). Similar results were observed for FIB-4 and APRI in Models 2–3. Compared to clean fuel users with low O3 exposure, the estimated ORs of advanced fibrosis reflected by FIB-4 in solid fuel users with low O3 or solid fuel users with high O3 exposure in women were 1.514 (95% CI: 1.361, 1.683) or 2.271 (95% CI: 2.031, 2.541), and the matched figures for advanced fibrosis reflected by APRI were 1.498 (95% CI: 1.306, 1.715) or 1.924 (95% CI: 1.677, 2.203) (Model 1). These results were not substantially changed in Models 2–3.
The combined association of ambient O3 exposure and cooking fuel type with hepatic fibrosis indices. Estimated β values or ORs and 95%CIs in low O3 plus clean fuel, low O3 plus solid fuel, high O3 plus clean fuel, and high O3 plus solid fuel groups were represented by the corresponding black dot (black lines), gray square (gray lines), orange triangle (orange lines), and blue rhombus (blue lines), respectively
Discussion
In this study, we observed that high levels of O3 exposure and solid fuel use were associated with elevated hepatic indices or the prevalent intermediate-high advanced fibrosis and their synergistic effects on advanced fibrosis. These were more obviously seen in women, indicating that women might be more vulnerable to the effect of air pollution on liver dysfunction. It revealed the impact of indoor and outdoor air pollution on liver damage, as well as the necessity of cleaner fuel switch and the implementation of effective measures to improve air quality to reduce the risk of liver dysfunction.
The fact that solid fuel use was recognized as a source of IAP is well established. Now, the adverse effect of solid fuel used for cooking on the respiratory and circulatory system has been widely recognized (Lee et al. 2020), while the evidence of solid fuel use–related liver dysfunction is lacking. In fact, the liver, as the major detoxifying organ, is more vulnerable to the adverse effects of air pollutants (Pejhan et al. 2019; Zheng et al. 2015).
It is obvious that numerous pollutants emitted from incomplete combustion of solid fuel, such as PM2.5, polycyclic aromatic hydrocarbons (PAHs), and black carbon (BC) (Ambade et al. 2021a; Ambade et al. 2022) can enter the body through the respiratory tract, and they may also enter the body directly through the skin or other routes when the concentration is high enough. Results from four European cohorts of the ESCAPE project (n=174,770), and the Rome longitudinal cohort (n=1,245,397) showed that exposure to high levels of ambient air pollutants such as PM2.5 and NO was associated with an increased risk of liver cirrhosis or liver cancer (Orioli et al. 2020; Pedersen et al. 2017). Results from the National Health and Nutrition Examination Survey showed that PAH exposure was positively associated with the risk of non-alcoholic fatty liver (Hu et al. 2021). An experimental study showed that PM2.5 was associated with metabolic disorders via inducing oxidative stress and inflammation in liver cells (Ding et al. 2019). Moreover, some evidence showed that air quality had improved for regional closures caused by the COVID-19 pandemic, while the main source of PAHs is still the burning of biomass and coal, which suggests the need to promote the use of cleaner fuels to improve air quality (Ambade et al. 2021b; Kurwadkar et al. 2022).
Currently, epidemiological evidence for ambient O3 exposure–related liver dysfunction is limited. Only one population-based longitudinal study of elderly people showed that short-term (n=545) or long-term (n= 318,911) exposure to O3 was related to a 3.6% increase in AST, and a 4.0% increase in ALT, respectively (Kim et al. 2015; Li et al. 2022). AST and ALT, as the typical liver enzyme in blood samples, are often used to reflect the status of the liver, and our study has also used these liver enzymes to create novel indices to reflect the clinical status of the liver, which can be considered clinically significant and of practical value. However, toxicological studies have been conducted widely to reveal the adverse effect of rats treated with O3. For instance, rats exposed to 0.5 ppm O3 for 10 min per day can cause hepatocellular necrosis in the liver (Cretu et al. 2010), and acetaminophen can attenuate acute exposure to O3 aggravates drug-induced liver injury by delaying liver self-repair in C57BL/6 male mice (Aibo et al. 2010). The abovementioned adverse outcomes may be attributed to the oxidizing air pollutant O3-induced lipid oxidation in the body (Csallany et al. 1985) and irritate the progression of liver fibrosis.
Because of the similar pathways of outdoor and indoor air pollution entering the human body, we may consider that the association of IAP from solid fuel burning and ambient O3 exposure with hepatic fibrosis is biologically plausible. One noteworthy finding of this study was that O3 exposure and solid fuel use had a synergistic effect on intermediate-high advanced fibrosis risk. Although the evidence for the combined associations of ambient O3 and solid fuel use with advanced fibrosis risk is lacking, several epidemiological studies have shown that mixed exposure to air pollutants had adverse effects on human health. Zhang et al. (2022) found that the joint effect of multiple air pollutants (PM2.5, PM10, NO2, SO2, O3, and CO) on lipid profiles. Siddika et al. (2019) revealed a synergistic effect of prenatal exposure to PM2.5 and O3 on preterm birth (Siddika et al. 2019). Animal experiments showed that the Wistar rats who inhaled 0.8ppm ozone and PM2.5 successively exhibited inflammatory changes and pathological features in their lungs, indicating that joint exposure to different environmental pollutants may be more toxic to the lungs than exposure to a single pollutant (Wang et al. 2015). It is fact that the volume of air exchange between outdoor and indoor environments is very high in rural China (Carter et al. 2016), which increased their chance for the co-exposure of indoor and outdoor air pollution. In accordance with the abovementioned reasons, we may deduce that it is a reasonable finding that O3 exposure synergist with solid fuel use was related to increased advanced fibrosis risk.
Another notable finding was that women’s liver function was more sensitive to air pollutants, which may be due to factors such as woman’s anatomy, hormone levels, and lifestyle. It is hard to ignore the fact that 66% of the population in low- and middle-income countries are still unable to access the clean energy, and IAP remains a major contributor to indoor particulate matter exposure (Gordon et al. 2014). In fact, women tend to cook at home and are often exposed to oil fuel and the production of fuel combustion for longer time than men (Chen et al. 2020), which had been verified linked to various chronic diseases (Lin et al. 2020). A prospective cohort study of 0.5 million Chinese adults also found a consistent positive association between solid cooking fuel use and chronic digestive diseases (Wen et al. 2023). PAHs derived primarily from solid fuel use (Ambade et al. 2021c) were associated with elevated ALT levels in adolescent females (OR = 2.33, 95%CI: 1.15, 4.72) (Xu et al. 2021), suggesting that PAHs may have toxic effects on the liver. In addition, estrogen has non-reproductive effects as a regulator of the immune system, growth, nervous function, and metabolism. Especially in the liver, impaired estrogen receptor expression and function are closely associated with obesity and liver-related metabolic disorders (Ezhilarasan 2020). As mentioned above, it is reasonable to assume that women are susceptible to IAP.
Although the underlying mechanisms for the association between air pollution and hepatic fibrosis have been not entirely clarified, extensive studies were available to concern the potential mechanisms of involvement in air pollutants such as PM2.5 or O3 associated with liver dysfunction. In vitro experiments on mice have shown that exposure to PM2.5 induced a significant effect on promoting liver fibrosis. PM2.5 may induce increased nicotinamide adenine dinucleotide phosphate (NADPH) oxidases (NOXs) activity and generate excessive reactive oxygen species (ROS) by activating PINK1/parking signaling pathway to cause mitochondrial phagocytosis and ultimately lead to liver fibrosis (Qiu et al. 2019; Zheng et al. 2015). Targeted metabolomics experiments in mice have demonstrated that long-term exposure to PM2.5 aggravates liver metabolic disorders which represents a time-response relationship (Samavat et al. 2021). And PM2.5 and O3 co-exposure induced alteration of key metabolic pathways (glucose, lipids, and amino acids) and activation of oxidative damage and inflammation in the liver (Miller 2020; Samavat et al. 2021; Theis et al. 2014). These phenomena are biologically plausible, and they may be partially explained by that the cytochrome P-450 enzyme plays an important role in detoxifying the xenobiotics which may determine the production of ROS and major source from the liver (Rosen et al. 2001; Tomaru et al. 2007).
Several limitations of the present study should be noted. First, this study cannot establish causal associations between indoor or outdoor air pollution and hepatic fibrosis indices due to the nature of the cross-sectional design. However, we provide some epidemiological clues for subsequent experimental explorations. Second, FIB-4, APRI, and AST/ALT may exist in misclassification in the assessment of the degree of liver fibrosis. However, the sensitivity and specificity of FIB-4 (Kim et al. 2016), APRI (Wai et al. 2003), and AST/ALT (Hou et al. 2022) have been demonstrated to be accepted in previous studies. Third, IAP was assessed by using self-reported data on domestic fuel use in this study. However, results from a large perspective study indicate that self-reported fuel use shows a high agreement between the baseline survey and the re-survey (kappa coefficient=0.61) (Liu et al. 2019). Finally, the type of fuel used for cooking and the air quality of the environments around people may be influenced by their socio-economic status, lifestyle, and traditional customs. However, no substantial change was observed in the results of this study between unadjusted and adjusted factors.
In conclusion, high levels of O3 exposure and solid fuel use had a synergistic effect on the risk of liver dysfunction, and women are more susceptible to air pollutants. Our study may provide scientific evidence for the synergistic effects of co-exposure to indoor and outdoor air pollution on human health. It also suggests that promoting cleaner fuel use is an effective measure to maintain sustainable development of the environment and gain beneficial effect on human health.
Data availability
The data that support the findings of this study are available upon reasonable request from the corresponding authors.
Abbreviations
- IAP:
-
indoor air pollution
- O3 :
-
ozone
- PAHs:
-
polycyclic aromatic hydrocarbons
- T2DM:
-
type 2 diabetes mellitus
- CHD:
-
coronary heart disease
- APRI:
-
aspartate-to-platelet-ratio index
- AST:
-
aspartate aminotransferase
- ALT:
-
alanine aminotransferase
- FIB-4:
-
fibrosis-4 score
- BMI:
-
body mass index
- CI:
-
confidence interval
- OR:
-
odds ratio
- RERI:
-
relative excess risk due to interaction
- AP:
-
the attributable proportion due to interaction
- SI:
-
synergy index
References
Aibo DI, Birmingham NP, Lewandowski R, Maddox JF, Roth RA, Ganey PE et al (2010) Acute exposure to ozone exacerbates acetaminophen-induced liver injury in mice. Toxicol Sci 115:267–285
Alewel DI, Henriquez AR, Colonna CH, Snow SJ, Schladweiler MC, Miller CN et al (2021) Ozone-induced acute phase response in lung versus liver: the role of adrenal-derived stress hormones. J Toxicol Environ Health A 84:235–248
Ambade B, Kurwadkar S, Sankar TK, Kumar A (2021a) Emission reduction of black carbon and polycyclic aromatic hydrocarbons during COVID-19 pandemic lockdown. Air Qual Atmos Health 14:1081–1095
Ambade B, Sankar TK, Kumar A, Gautam AS, Gautam S (2021b) COVID-19 lockdowns reduce the black carbon and polycyclic aromatic hydrocarbons of the Asian atmosphere: source apportionment and health hazard evaluation. Environ Dev Sustain 23:12252–12271
Ambade B, Sethi SS, Kumar A, Sankar TK, Kurwadkar S (2021c) Health risk assessment, composition, and distribution of polycyclic aromatic hydrocarbons (pahs) in drinking water of southern Jharkhand, East India. Arch Environ Contam Toxicol 80:120–133
Ambade B, Sethi SS, Kurwadkar S, Mishra P, Tripathee L (2022) Accumulation of polycyclic aromatic hydrocarbons (pahs) in surface sediment residues of Mahanadi River Estuary: abundance, source, and risk assessment. Mar Pollut Bull 183:114073
Carter E, Archer-Nicholls S, Ni K, Lai AM, Niu H, Secrest MH et al (2016) Seasonal and diurnal air pollution from residential cooking and space heating in the eastern Tibetan Plateau. Environ Sci Technol 50:8353–8361
Chafe ZA, Brauer M, Klimont Z, Van Dingenen R, Mehta S, Rao S et al (2014) Household cooking with solid fuels contributes to ambient PM2.5 air pollution and the burden of disease. Environ Health Perspect 122:1314–1320
Chen TY, Fang YH, Chen HL, Chang CH, Huang H, Chen YS et al (2020) Impact of cooking oil fume exposure and fume extractor use on lung cancer risk in non-smoking Han Chinese women. Sci Rep 10:6774
Cohen AJ, Brauer M, Burnett R, Anderson HR, Frostad J, Estep K et al (2017) Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the global burden of diseases study 2015. Lancet 389:1907–1918
Cretu DI, Sovrea A, Ignat RM, Filip A, Bidian C, Cretu A (2010) Morpho-pathological and physiological changes of the brain and liver after ozone exposure. Rom J Morphol Embryol 51:701–706
Csallany AS, Manwaring JD, Menken BZ (1985) Ozone-related fluorescent compounds in mouse liver and lung. Environ Res 37:320–326
Dai X, Bui DS, Perret JL, Lowe AJ, Frith PA, Bowatte G et al (2021) Exposure to household air pollution over 10 years is related to asthma and lung function decline. Eur Respir J 57
Ding S, Yuan C, Si B, Wang M, Da S, Bai L et al (2019) Combined effects of ambient particulate matter exposure and a high-fat diet on oxidative stress and steatohepatitis in mice. PLoS One 14:e0214680
EASL, EASD, EASO (2016) EASL-EASD-EASO clinical practice guidelines for the management of non-alcoholic fatty liver disease. Diabetologia 59:1121–1140
Ezhilarasan D (2020) Critical role of estrogen in the progression of chronic liver diseases. Hepatobiliary Pancreat Dis Int 19:429–434
Gordon SB, Bruce NG, Grigg J, Hibberd PL, Kurmi OP, Lam KB et al (2014) Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med 2:823–860
Gu J, Shi Y, Zhu Y, Chen N, Wang H, Zhang Z et al (2020) Ambient air pollution and cause-specific risk of hospital admission in China: a nationwide time-series study. PLoS Med 17:e1003188
Guo B, Guo Y, Nima Q, Feng Y, Wang Z, Lu R et al (2022) Exposure to air pollution is associated with an increased risk of metabolic dysfunction-associated fatty liver disease. J Hepatol 76:518–525
Han L, Sun Z, Gong T, Zhang X, He J, Xing Q et al (2020) Assessment of the short-term mortality effect of the national action plan on air pollution in Beijing. China. Environmental Research Letters 15:034052
Hou J, Liu X, Zuo T, Tu R, Dong X, Li R et al (2022) Residential greenness attenuated associations of long-term exposure to air pollution with biomarkers of advanced fibrosis. Environ Sci Pollut Res Int 29:977–988
Hu Z, Li Y, Yang Y, Yu W, Xie W, Song G et al (2021) Serum lipids mediate the relationship of multiple polyaromatic hydrocarbons on non-alcoholic fatty liver disease: a population-based study. Sci Total Environ 780:146563
Kang N, Chen G, Tu R, Liao W, Liu X, Dong X et al (2022) Adverse associations of different obesity measures and the interactions with long-term exposure to air pollutants with prevalent type 2 diabetes mellitus: the Henan rural cohort study. Environ Res 207:112640
Kazemiparkouhi F, Eum KD, Wang B, Manjourides J, Suh HH (2020) Long-term ozone exposures and cause-specific mortality in a US Medicare cohort. J Expo Sci Environ Epidemiol 30:650–658
Kim KN, Lee H, Kim JH, Jung K, Lim YH, Hong YC (2015) Physical activity- and alcohol-dependent association between air pollution exposure and elevated liver enzyme levels: an elderly panel study. J Prev Med Public Health 48:151–169
Kim WR, Berg T, Asselah T, Flisiak R, Fung S, Gordon SC et al (2016) Evaluation of apri and fib-4 scoring systems for non-invasive assessment of hepatic fibrosis in chronic hepatitis B patients. J Hepatol 64:773–780
Kurwadkar S, Sethi SS, Mishra P, Ambade B (2022) Unregulated discharge of wastewater in the Mahanadi River basin: risk evaluation due to occurrence of polycyclic aromatic hydrocarbon in surface water and sediments. Mar Pollut Bull 179:113686
Lee J, Vali Y, Boursier J, Spijker R, Anstee QM, Bossuyt PM et al (2021) Prognostic accuracy of FIB-4, NAFLD fibrosis score and APRI for NAFLD-related events: a systematic review. Liver Int 41:261–270
Lee KK, Bing R, Kiang J, Bashir S, Spath N, Stelzle D et al (2020) Adverse health effects associated with household air pollution: a systematic review, meta-analysis, and burden estimation study. Lancet Glob Health 8:e1427–e1434
Li W, Dorans KS, Wilker EH, Rice MB, Long MT, Schwartz J et al (2017) Residential proximity to major roadways, fine particulate matter, and hepatic steatosis: the Framingham Heart Study. Am J Epidemiol 186:857–865
Li Y, Yuan X, Wei J, Sun Y, Ni W, Zhang H et al (2022) Long-term exposure to ambient air pollution and serum liver enzymes in older adults: a population-based longitudinal study. Ann Epidemiol 74:1–7
Lin J, Ni S, Shi Q, Xiong Z, Kang J, Sun X et al (2020) Environmental exposure to cooking oil fumes and fatty liver disease. Ann Palliat Med 9:3810–3817
Liu X, Mao Z, Li Y, Wu W, Zhang X, Huo W et al (2019) Cohort profile: the Henan rural cohort: a prospective study of chronic non-communicable diseases. Int J Epidemiol 48:1756–1756j
Long MT, Zhang X, Xu H, Liu CT, Corey KE, Chung RT et al (2021) Hepatic fibrosis associates with multiple cardiometabolic disease risk factors: the Framingham Heart Study. Hepatology 73:548–559
Miller MR (2020) Oxidative stress and the cardiovascular effects of air pollution. Free Radic Biol Med 151:69–87
Nah EH, Cho S, Kim S, Chu J, Kwon E, Cho HI (2021) Prevalence of liver fibrosis and associated risk factors in the Korean general population: a retrospective cross-sectional study. BMJ Open 11:e046529
Orioli R, Solimini AG, Michelozzi P, Forastiere F, Davoli M, Cesaroni G (2020) A cohort study on long-term exposure to air pollution and incidence of liver cirrhosis. Environ Epidemiol 4:e109
Pan M, Li S, Tu R, Li R, Liu X, Chen R et al (2021) Associations of solid fuel use and ambient air pollution with estimated 10-year atherosclerotic cardiovascular disease risk. Environ Int 157:106865
Pedersen M, Andersen ZJ, Stafoggia M, Weinmayr G, Galassi C, Sorensen M et al (2017) Ambient air pollution and primary liver cancer incidence in four European cohorts within the escape project. Environ Res 154:226–233
Pejhan A, Agah J, Adli A, Mehrabadi S, Raoufinia R, Mokamel A et al (2019) Exposure to air pollution during pregnancy and newborn liver function. Chemosphere 226:447–453
Qiu YN, Wang GH, Zhou F, Hao JJ, Tian L, Guan LF et al (2019) PM2.5 induces liver fibrosis via triggering ros-mediated mitophagy. Ecotoxicol Environ Saf 167:178–187
Rosen P, Nawroth PP, King G, Moller W, Tritschler HJ, Packer L (2001) The role of oxidative stress in the onset and progression of diabetes and its complications: a summary of a congress series sponsored by UNESCO-MCBN, the American Diabetes Association and the German Diabetes Society. Diabetes Metab Res Rev 17:189–212
Samavat H, Luu HN, Beckman KB, Jin A, Wang R, Koh WP et al (2021) Leukocyte telomere length, cancer incidence and all-cause mortality among Chinese adults: Singapore Chinese health study. Int J Cancer 148:352–362
Siddika N, Rantala AK, Antikainen H, Balogun H, Amegah AK, Ryti NRI et al (2019) Synergistic effects of prenatal exposure to fine particulate matter (PM2.5) and ozone (O3) on the risk of preterm birth: a population-based cohort study. Environ Res 176:108549
Siddiqui MS, Yamada G, Vuppalanchi R, Van Natta M, Loomba R, Guy C et al (2019) Diagnostic accuracy of noninvasive fibrosis models to detect change in fibrosis stage. Clin Gastroenterol Hepatol 17(1877-1885):e1875
Theis WS, Andringa KK, Millender-Swain T, Dickinson DA, Postlethwait EM, Bailey SM (2014) Ozone inhalation modifies the rat liver proteome. Redox Biol 2:52–60
Tomaru M, Takano H, Inoue K, Yanagisawa R, Osakabe N, Yasuda A et al (2007) Pulmonary exposure to diesel exhaust particles enhances fatty change of the liver in obese diabetic mice. Int J Mol Med 19:17–22
Toosi AE (2015) Liver fibrosis: causes and methods of assessment, a review. Rom J Intern Med 53:304–314
Tu R, Li Y, Shen L, Yuan H, Mao Z, Liu X et al (2019) The prevalence and influencing factors of physical activity and sedentary behaviour in the rural population in China: the Henan rural cohort study. BMJ Open 9:e029590
Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS et al (2003) A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis c. Hepatology 38:518–526
Wang G, Zhao J, Jiang R, Song W (2015) Rat lung response to ozone and fine particulate matter (PM2.5) exposures. Environ Toxicol 30:343–356
Wang Y, Li Y, Liu X, Zhang H, Abdulai T, Tu R et al (2019) Prevalence and influencing factors of coronary heart disease and stroke in Chinese rural adults: the Henan rural cohort study. Front Public Health 7:411
Wang Y, Cao R, Xu Z, Jin J, Wang J, Yang T et al (2022) Long-term exposure to ozone and diabetes incidence: a longitudinal cohort study in China. Sci Total Environ 816:151634
Watt GP, Lee M, Pan JJ, Fallon MB, Loomba R, Beretta L et al (2019) High prevalence of hepatic fibrosis, measured by elastography, in a population-based study of Mexican Americans. Clin Gastroenterol Hepatol 17(968-975):e965
Wen Q, Liu T, Yu Y, Zhang Y, Yang Y, Zheng R et al (2023) Self-reported primary cooking fuels use and risk of chronic digestive diseases: a prospective cohort study of 0.5 million Chinese adults. Environ Health Perspect 131:47002
Xiao Q, Geng G, Xue T, Liu S, Cai C, He K et al (2022) Tracking PM2.5 and O3 pollution and the related health burden in China 2013-2020. Environ Sci Technol 56:6922–6932
Xu C, Liu Q, Liang J, Weng Z, Xu J, Jiang Z et al (2021) Urinary biomarkers of polycyclic aromatic hydrocarbons and their associations with liver function in adolescents. Environ Pollut 278:116842
Xu MX, Ge CX, Qin YT, Gu TT, Lou DS, Li Q et al (2019) Prolonged PM2.5 exposure elevates risk of oxidative stress-driven nonalcoholic fatty liver disease by triggering increase of dyslipidemia. Free Radic Biol Med 130:542–556
Xue T, Zheng Y, Geng G, Xiao Q, Meng X, Wang M et al (2020a) Estimating spatiotemporal variation in ambient ozone exposure during 2013-2017 using a data-fusion model. Environ Sci Technol 54:14877–14888
Xue Y, Yang K, Wang B, Liu C, Mao Z, Yu S et al (2020b) Reproducibility and validity of an FFQ in the Henan rural cohort study. Public Health Nutr 23:34–40
Ya P, Xu H, Ma Y, Fang M, Yan X, Zhou J et al (2018) Liver injury induced in Balb/c mice by PM2.5 exposure and its alleviation by compound essential oils. Biomed Pharmacother 105:590–598
Yun X, Shen G, Shen H, Meng W, Chen Y, Xu H et al (2020) Residential solid fuel emissions contribute significantly to air pollution and associated health impacts in China. Sci Adv 6
Yusuf S, Joseph P, Rangarajan S, Islam S, Mente A, Hystad P et al (2020) Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (pure): a prospective cohort study. Lancet 395:795–808
Zhang W, Liu J, Hu D, Li L, Cui L, Xu J et al (2022) Joint effect of multiple air pollutants on lipid profiles in obese and normal-weight young adults: the key role of ozone. Environ Pollut 292:118247
Zheng Z, Zhang X, Wang J, Dandekar A, Kim H, Qiu Y et al (2015) Exposure to fine airborne particulate matters induces hepatic fibrosis in murine models. J Hepatol 63:1397–1404
Acknowledgements
We thank all participants, coordinators, and administrators who provided their support and help during the research.
Funding
This research was supported by the Foundation of National Key Program of Research and Development of China (Grant No: 2016YFC0900803), the Science and Technology Innovation Team Support Plan of Colleges and Universities in Henan Province (Grant No: 21IRTSTHN029), the Science and Technique Foundation of Henan Province (Grant NO: 222102320029), the open project of Key Laboratory of Environment and health, ministry of Education (Grant No: 2020GWFJJ01), and the Discipline Key Research and Development Program of Zhengzhou University (Grant No: XKZDQY202008, XKZDQY202002). The funders had no role in the study design, data collection, and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
X. Hou: investigation, data curation, methodology, formal analysis, visualization, writing—original draft. Z. Mao: investigation, writing—review & editing. R. Li, W. Liao, N. Kang, X. Liu, and W. Huo: investigation, writing—review & editing. X. Song, C. Zhang, and R. Chen: formal analysis, writing—review & editing. Chongjian Wang and Jian Hou: conceptualization, methodology, investigation, validation, supervision, writing—reviewing and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Zhengzhou University Life Science Ethics Committee (Code: [2015] MEC (S128)), and informed consent was acquired from each participant before this survey.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Non-invasive hepatic fibrosis indices are novel biomarkers in the field of liver.
• High ozone exposure and solid fuel use are related to increased FIB-4 and APRI values.
• There is a synergic effect of ozone exposure and solid fuel use on advanced fibrosis.
• Women tend to be more vulnerable to air pollutants and the synergy effect.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hou, X., Mao, Z., Song, X. et al. Synergistic association of long-term ozone exposure and solid fuel use with biomarkers of advanced fibrosis. Environ Sci Pollut Res 30, 85318–85329 (2023). https://doi.org/10.1007/s11356-023-28337-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-28337-8