Abstract
Based on nationally representative samples from US, we aimed to assess the associations of vitamins with hearing loss, vision disorder and sleep problem. A total of 25,312, 8425 and 24,234 participants were included in this study to investigate the relationship of vitamins with hearing loss, vision disorder and sleep problem from National Health and Nutrition Examination Survey, respectively. Vitamins including niacin, folic acid, vitamin B6, A, C, E and carotenoids were considered in our study. Logistic regression models were used to assess the associations between all included dietary vitamin intake concentrations and the prevalence of specific outcomes. Increased lycopene (odds ratio [OR]: 0.904, 95% confidence interval [CI]: 0.829–0.985) intake was associated with a deceased prevalence of hearing loss. Higher dietary intake of folic acid (OR: 0.637, 95% CI: 0.443–0.904), vitamin B6 (0.667, 0.465–0.947), alpha-carotene (0.695, 0.494–0.968), beta-carotene (0.703, 0.505–0.969) and lutein + zeaxanthin (0.640, 0.455–0.892) were associated with a decreased prevalence of vision disorder. The inversely associations of sleeping problem with niacin (OR: 0.902, 95% CI: 0.826–0.985), folic acid (0.882, 0.811–0.959), vitamin B6 (0.892, 0.818–0.973), vitamin C (0.908, 0.835–0.987), vitamin E (0.885, 0.813–0.963) and lycopene (0.919, 0.845–0.998) were also observed. Our findings provide evidence that increased specific vitamin intake is associated with decreased prevalence of hearing loss, vision disorder and sleep problem.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Good hearing, eyesight and sleep are all essential body functions for living a normal life and ensuring quality of life. In the United States, 23.4 million people (7.2%) have vision impairments or blindness (Rein et al. 2021), 14.5% of adults have sleeping problems (Shieu et al. 2020) and 23% of Americans over the age of 12 years old are directly affected by hearing loss (HL) (Goman and Lin 2016). HL, vision disorder (VD) and sleep problems (SP) have gained widespread public health attention because of their potential effects on quality of life. The three body functions (hearing, vision and sleep) are regulated by a range of internal and external variables, with the nervous system playing a prominent role (Pula 2012, Rémi et al. 2019, Yamasoba et al. 2013). Several factors could affect the neurological system's functions, including age, the accumulation of reactive oxygen species (ROS), and environmental pollutants (Ambade et al. 2022; Ambade and Sethi 2021). Recently, vitamins have been reported to play a unique part in influencing brain function through an anti-oxidation mechanism (Flanagan et al. 2020; Milisav et al. 2018).
With economic development, food production and supply capacity have substantially improved, resulting in a considerable change in the structure of the human diet. Increasingly people prefer Western dietary patterns that are heavy in energy and fat but deficient in dietary vitamins, fiber and minerals (Christ et al. 2019). Vitamins deficiency may motive a series of health damages, inclusive of overweight, neurological dysfunction, diabetes and so on (Diab and Krebs 2018; Thomas-Valdés et al. 2017). Vitamins, essential nutrients, are required to preserve human health and may have an impact on the brain function by taking part in the neurosynthesis (Kennedy 2016). Evidence from relevant clinical research suggested that vitamins were promising for preventing and treating cognitive impairment and dementia (Dysken et al. 2014; Markun et al. 2021; Vlachos and Scarmeas 2019). Meanwhile, some vitamins with anti-oxidant properties can eliminate ROS and slow down aging (Duan et al. 2022; Milisav et al. 2018).
Vitamins may also have impacts on hearing, vision and sleep via the aforementioned or other pathways. Several previous studies have reported the associations of some vitamins with hearing (Ibrahim et al. 2018; Özkırış et al. 2013; Rodrigo et al. 2021), vision (Shalini et al. 2021; Williams et al. 2017) and sleep (Black 2021; Djokic et al. 2019). However, only a few vitamins were included in previous studies (Aspy et al. 2018; Kabagambe et al. 2018; Merle et al. 2016) and their results were inconsistent: some studies reported positive or negative associations of vitamins with HL, VD and SP (Çakir et al. 2020; Curhan et al. 2015; Dziedziak et al. 2021), but others showed no significant association (Merle et al. 2016; Shargorodsky et al. 2010). Furthermore, vitamin consumption has drawn a lot of attention recently as a helpful and easily modifiable factor in the prevention and treatment of a variety of clinical and subclinical diseases; however, the current research evidence is insufficient to assess whether additional supplementation is beneficial.
Therefore, we carried out the present cross-sectional analysis to evaluate the associations of various vitamins (including niacin, folic acid, vitamin B6, A, C, E and carotenoids) with HL, VD and SP from the National Health and Nutrition Examination Survey (NHANES). Exploring the association between multivitamins and various body functions could provide evidence for people to boost vitamin intake adequately for overall health, better hearing, vision and sleep, etc. Moreover, our study may provide clues for future research on the dual use of multivitamins for disease prevention and therapy.
Material and methods
Study population
Data for this study were sourced from NHANES, which has been conducted by the National Center for Health Statistics since 1999 (https://wwwn.cdc.gov/Nchs/Nhanes/). Briefly, NHANES combines interviews with physical and laboratory examinations in a nationwide chosen representative group of adults and children in the United States over a two-year cycle.
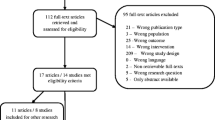
The data available for estimating the associations between vitamins and HL (NHANES 2000–2012, 2015–2018), VD (2001–2008) and SP (2005–2018) were included in this study. Following the exclusion of participants who had no data on the corresponding outcome variables, 77,493, 21,777 and 44,669 were included in the study of vitamins in relation to HL, VD and SP, respectively. Pregnant women, participants under 18 years old, those who lacked detailed dietary intake information, and those who lacked data on covariates and important demographic variables were further excluded. Finally, a total of 25,312, 8425 and 24,234 participants were included to investigate the associations of vitamins with HL, VD and SP, respectively (Fig. S1).
Ascertainment of vitamin intake
Vitamins were divided into fat-soluble vitamins (vitamin A, D, E and K) and water-soluble vitamins (vitamin B and C) (Chawla and Kvarnberg 2014; Yuan et al. 2020). Vitamin A and E, as representatives of fat-soluble vitamins, were included in our study instead of vitamin D and K due to their ability to be synthesized by the body (Yuan et al. 2020). Vitamin B3 (niacin), B6 and B9 (folic acid) were included in our study as representatives of group B vitamins as they played crucial roles in neuronal functions, redox reactions, as well as catabolism and anabolism (Meyer-Ficca et al. 2016; Ratajczak et al. 2021). Additionally, carotenoids were considered in our study since they were broadly located in diets and provided numerous health advantages via acting as antioxidants and provitamin A. Alpha-carotene, beta-carotene, beta-cryptoxanthin, lycopene and lutein + zeaxanthin were included in our study as they were the principal carotenoids present in human plasma and tissue (Jomova and Valko 2013; Brewczyński et al. 2021).
Dietary niacin, folic acid, carotenoids, vitamin B6, A, C and E intakes were estimated using 24-h dietary recall interviews, which were conducted by the automated multiple-pass method developed by the United States Department of Agriculture. And for each dietary recall interview release, the nutritional value of the foods and drinks ingested by participants was calculated using data from the relevant Food and Nutrient Database for Dietary Studies, which included information on food descriptions, food quantities and weights and nutrients (Raper et al. 2004). The types and quantities of foods and beverages ingested by the participants up to 24 h before the interview were recorded. Energy, nutrients (e.g., vitamins, minerals) and other food component intakes were estimated via multiplying the quantity of each nutrient in each food by its daily consumption and then adding the sum of all food sources of that nutrient. Units of measurement for vitamins vary: microgram (mcg) units for folic acid and carotenoids, milligram (mg) units for niacin, vitamin B6, C, and E, and retinol activity equivalent (RAE) units for vitamin A. Every diet surveyor and coder had completed initial training and passed certification exams.
Ascertainment of outcome
The definitions of HL, VD and SP were based on hearing, vision and sleep status questionnaires, respectively. Participants were questioned about their general hearing condition without assistance from any assistive listening devices. Answering “excellent” or “good” was classified as normal hearing, while “a little trouble”, “moderate hearing trouble”, “a lot of trouble” or “deaf” was classified as HL (Goshtasbi et al. 2021). Participants were questioned about their general condition of eyesight in the questionnaire section devoted to vision. Answering “excellent”, “good” or “fair” was distinguished as normal eyesight, while “poor” or “very poor” was distinguished as VD (Shiue 2013). Furthermore, participants were asked in the sleep habits and disorders questionnaire: Have you ever told a doctor or other health professional that you had trouble sleeping? There were two options: yes or no. Participants were considered to suffer from SP if their responses were “yes”, and a “no” response indicated normal sleep.
Covariates
Age, gender, body mass index (BMI), race-ethnicity (Mexican American, Other Hispanic, Non-Hispanic White, Non-Hispanic Black and other races), education levels, family income-poverty ratio (PIR), smoking, alcohol use, physical activity, waist circumference and diabetes were obtained through interviews and physical exams. Age was coded as < 60 years old and ≥ 60 years old. BMI was calculated as weight (in kilograms) divided by the square of height (in meters). There were three divisions for educational levels: less than high school, high school or equivalent and college or above. PIR was calculated via dividing family (or individual) income by the poverty guidelines specific to the survey year, which varied according to the household size and the locality (Fadeyev et al. 2021). A ratio of one indicated the same income and poverty level, while a lower PIR denoted a higher degree of poverty (Okosun et al. 2014). Our study grouped PIR into three categories: 0–1.0, 1.0–3.0 and > 3.0. Smokers were those who had consumed at least 100 cigarettes throughout their lifetime. Current drinkers were recognized as those who had consumed one or more alcoholic beverages in the previous 12 months. Physical activity levels were classified as 0, 1–2 or ≥ 3 times per week. Those who met one of the following criteria were deemed to have diabetes: being told by a doctor that they have diabetes, using antidiabetic medicine, glycated hemoglobin level ≥ 6.5%, fasting plasma glucose ≥ 7.0 mmol/L, random plasma glucose ≥ 11.1 mmol/L or plasma glucose ≥ 11.1 mmol/L two hours after a 75 g glucose load (Lee and Colagiuri 2018).
Statistical analysis
Continuous variables were reported as mean ± standard deviation (SD) and categorical variables were presented as numbers (percentages). Logistic regression models were used to assess the associations of all included dietary vitamin intake concentrations [continuous and categorical (across quartiles)] and the prevalence of HL, VD and SP. The linear trend was created via allocating each category's median value to every participant in that group. In addition, stratification analyses by gender, age, BMI, smoking, drinking and physical activity were conducted. The combined effects of vitamins with stratified variables were assessed using a likelihood ratio test for interaction. Meanwhile, the dose–response relationships were performed using restricted cubic splines with four knots at percentiles 5, 35, 65 and 95% of the distribution (Li et al. 2022). R version 4.2.0 was used for all statistical analyses, and statistical significance was identified as a two-sided P < 0.05.
Results
A total of 25,312 participants were finally included in the study to examine the relationship between dietary vitamin intake and HL (Table 1). Among them, 54.4% were male, 31.4% were found to be equal and more than 60 years old, 16.5% were diabetic patients, and 6327 (25.0%) people were classified as HL. 8425 participants were included to investigate the association between dietary vitamin intake and VD. Among them, 304 (3.62%) participants had VD. And 24,234 participants were eventually enrolled to investigate the association between dietary vitamin intake and SP. There were 6509 (26.86%) participants who had SP.
Association between dietary vitamin intake and HL
Compared with the lowest quartile (quartile 1, Q1), the second (quartile 2, Q2) and third (quartile 3, Q3) quartiles of beta-carotene and the Q3 of alpha-carotene had a lower prevalence of HL, and their multivariate-adjusted ORs (95% CIs) were 0.911 (0.836–0.992), 0.917 (0.841–0.999) and 0.912 (0.837–0.995), respectively (Table 2). Additionally, the OR for HL was lower in the highest quartile (quartile 4, Q4) (OR: 0.904, 95% CI: 0.829–0.985) than that in the Q1 of lycopene intake (P-trend < 0.05) (Table 2). No significantly nonlinear dose–response association between vitamin and hearing loss was found in our study (Fig S2). Furthermore, the interaction terms between folic acid and age (P for interaction = 0.028), vitamin E and drinking (P for interaction = 0.044), as well as lycopene and BMI (P for interaction = 0.040) were statistically significant (Table S1).
Association between dietary vitamin intake and VD
Compared with the Q1, the Q4 of folic acid (OR: 0.637, 95% CI: 0.443–0.904), vitamin B6 (0.667, 0.465–0.947), alpha-carotene (0.695, 0.494–0.968) and beta-cryptoxanthin (0.703, 0.505–0.969) were negatively associated with the prevalence of VD (Table 3). Regarding lutein + zeaxanthin, the prevalence of VD was significantly decreased in Q3 (OR: 0.640, 95% CI: 0.455–0.892). We found significant negatively dose-dependent associations of folic acid and vitamin B6 with VD in categorical models across quartiles of vitamin intake concentrations (both P-trend < 0.05) (Table 3). In addition, the nonlinear dose–response associations of vitamin B6 (P nonlinear = 0.0051), alpha-carotene (P nonlinear = 0.0464), beta-carotene (P nonlinear = 0.0041) and lutein + zeaxanthin (P nonlinear = 0.0056) with VD were found too (Fig S3). Meanwhile, the associations of niacin and vitamin C with VD were significant in different smoking groups, and their P for interaction were 0.038 and 0.029, respectively (Table S2). Besides, the interaction term between vitamin B6 and physical activity (P for interaction = 0.012) was also statistically significant.
Association between dietary vitamin intake and SP
The Q4 of niacin (OR: 0.902, 95% CI: 0.826–0.985) and vitamin B6 (OR: 0.892, 95% CI: 0.818–0.973) were associated with a decreased prevalence of SP (Table 4). Q2 (OR: 0.869, 95% CI: 0.801–0.943) and Q3 (OR: 0.882, 95% CI:0.811–0.959) quartiles of folic acid were associated with a significantly decreased prevalence of SP when compared with the Q1. Additionally, the Q3 of vitamin C, E and lycopene had a lower prevalence of SP, and the multivariate-adjusted ORs (95% CIs) were 0.908 (0.835–0.987), 0.885 (0.813–0.963) and 0.919 (0.845–0.998), respectively. In categorical models, the significant dose–response relationships of SP with vitamin intake concentrations were also found to be negative for niacin and vitamin B6 (both P-trend < 0.05) (Table 4). Besides, there were nonlinear dose–response associations of niacin, folic acid, vitamin B6, vitamin C and vitamin E with SP (all P nonlinear < 0.05) (Fig S4). Meanwhile, the likelihood ratio test for interaction showed that the interaction terms between vitamin B6 and age (P for interaction = 0.002), vitamin A and gender (P for interaction = 0.015), vitamin C and drinking (P for interaction = 0.014), as well as alpha-carotene and physical activity (P for interaction = 0.042) were statistically significant (Table S3).
Discussion
Our study found that increased lycopene intake was associated with a decreased prevalence of HL. Folic acid and vitamin B6 may have a protective effect on both VD and SP. In addition, higher dietary intake of alpha-carotene, beta-carotene and lutein + zeaxanthin were associated with a decreased prevalence of VD. The associations of increased niacin, vitamin C, vitamin E and lycopene with decreased prevalence of SP were also observed. Meanwhile, the interaction effects of vitamins with gender, age, BMI, smoking, drinking and physical activity were found in our study, which was in line with previous studies (Choi et al. 2014; Sarris et al. 2012).
The results of our study carry noteworthy implications for public health. HL, VD and SP, as public health issues of widespread concern, have been proven to be associated with difficulty in daily interactions, impaired physical and mental health, as well as increased risks of cognitive impairment and death. Additionally, vitamin consumption has drawn a lot of attention recently as a helpful and easily modifiable factor in the prevention and treatment of HL, VD and SP. The associations between vitamins and HL, VD, and SP had been studied in several animal and population research; however, there were discrepancies in their results (Abbasi et al. 2021; Gopinath et al. 2013; Nunes et al. 2018; Ongan and Yuksel 2017; Rodrigo et al. 2021). The present study explored these associations using representative samples of the US general population, which enabled the generalization of our findings. And the results of our study implied that proper vitamin intake might be helpful for the prevention of HL, VD and SP.
Possible mechanisms
Vitamins are a group of regulatory substances that play a vital role in the metabolism process. As well as their involvement in neurochemical synthesis and antioxidant, they could thus be perceived as having a specific impact on numerous organs, including the brain, ear, eye, etc. (Berger et al. 2012; Kennedy 2016; Thomas-Valdés et al. 2017). An overabundance of ROS has adverse effects on vision, hearing and sleep by inducing oxidative stress, which can cause cochlea damage, reduce blood flow and affect the normal function of the vascular, endothelial and nervous systems (Çakir et al. 2020; Choi et al. 2021; Curhan et al. 2015; Evans and Lawrenson 2017). Hence, vitamins can function as antioxidants to guard against HL, VD and SP. On the other hand, vitamin actively participate in the metabolism of homocysteine; increased serum homocysteine concentrations could also contribute to a higher prevalence of HL, VD and SP (Aspy et al. 2018; Martínez-Vega et al. 2016; Tawfik et al. 2021). Additionally, vitamins play an essential role in the synthesis of several neurotransmitters (Peters et al. 2015) and can regulate the release of melatonin, thus having an effect on sleep (Peuhkuri et al. 2012). Several prior studies have reported the associations of some vitamins with hearing, vision and sleep, and a summary of previous studies is shown in Table S4.
Vitamin and HL
Although animal research has revealed some protective effects of vitamins on HL and associated mechanisms (Gi et al. 2018; Le Prell et al. 2011; Martínez-Vega et al. 2015), population studies have yielded inconsistent results. Our research found that intakes of alpha-carotene, beta-carotene and lycopene were associated with decreased prevalence of HL, which was in line with the previous studies (Curhan et al. 2015; Özkırış et al. 2013; Spankovich et al. 2011; Yu et al. 2011). Antioxidant vitamins (such as carotenoids, vitamin A, C and E) function as free radical scavengers to ward off oxidative stress, which can damage lipids, proteins, RNA and DNA and lead to disease (Berger et al. 2012). The associations between the prevalence of HL and beta-cryptoxanthin, lutein + zeaxanthin, vitamin A, C and E were not significant in our study; however, their protective effects on HL have been reported in previous research (Gopinath et al. 2011; Ibrahim et al. 2018; Rodrigo et al. 2021), but not all (Shargorodsky et al. 2010). A prospective cohort study following 65,521 female nurses found no association between HL and vitamin A or vitamin E and higher vitamin C intake was associated with a higher risk of HL (Curhan et al. 2015). The discrepancies could be explained by differences in the study population, reporting methods for HL and dietary evaluation techniques.
No significant association between HL and niacin, folic acid or vitamin B6 was found in our current investigation, which was reconcilable with previous studies (Choi et al. 2021; Dawes et al. 2020). Although some studies showed that higher niacin, folic acid and vitamin B6 intakes were associated with a lower risk of HL (Curhan et al. 2015; Kabagambe et al. 2018; Kim and Chung 2019), others have reported no significant association or increased risk (Dawes et al. 2020; Park et al. 2019). Perhaps the larger size of the study population in our study allowed for a better ability to support our findings. In addition, individual differences among study participants and different methods for outcome assessment may explain the disparities in results.
Vitamin and VD
Human vision creation is a complex and sensitive process, which can be harmed by the accumulation of reactive oxygen species, ultraviolet radiation, diseases, old age, environmental pollutants and other things (Ambade et al. 2021a; Grover and Samson 2014). Because of the eye's features (excessive oxygen consumption, high content of polyunsaturated fatty acids, chronic exposure to high-energy visible light and so on), oxidative stress was assumed to be a prevalent pathogenic mechanism in VD (Grover and Samson 2014; Lawrenson and Downie 2019). Thus, antioxidant vitamins may have a protective effect on decreasing the risk of VD. However, investigations into the associations between vitamins and VD have shown conflicting findings. For example, clinical studies and cohort studies discovered that antioxidant supplements (including beta-carotene, vitamins C and E) did not slow the advancement of cataracts(Mathew et al. 2012; Ramdas et al. 2012) but not all (Giaconi et al. 2012). Several carotenoids (alpha-carotene, beta-carotene, lutein + zeaxanthin) were found to have inverse associations with the prevalence of VD in our study; however, neither vitamin A, C nor E were associated with VD in our study. Carotenoids (alpha-carotene, beta-carotene and lutein + zeaxanthin) might protect eyesight by lowering the apoptosis of retinal ganglion cells and regulating ocular vascular function via their antioxidant action (Bungau et al. 2019; Dziedziak et al. 2021). It has also been reported in other studies that carotenoids have a decreased impact on the risk of VD (Wu et al. 2015; Shalini et al. 2021).
Niacin, folic acid and vitamin B6 are group B vitamins, and a lack of either one might result in mitochondrial failure (Huang-Link et al. 2021), elevated plasma homocysteine levels (Zampatti et al. 2014) and vascular endothelial damage (Tawfik et al. 2021). VD can be caused via the aforementioned pathways. In our study, folic acid and vitamin B6 were associated with decreased risk of VD, which is consistent with previous studies (Gopinath et al. 2013; Tan et al. 2014). According to a study that used data from the Age-Related Eye Disease Study, high folate intake was linked to a lower risk of progression to geographic atrophy, whereas vitamin B6 had no impact; and age-related macular degeneration was not substantially associated with folate or other B vitamins (Merle et al. 2016). However, several studies have also noted that niacin and vitamin B6 have protective effects against VD (Evans and Lawrenson 2017; Williams et al. 2017). Varied study populations, different research methodologies, various approaches to assessing exposures and results, as well as different types of visual issues may have contributed to variances in study findings.
Vitamin and SP
The association between dietary intake and sleep has gotten a lot of attention in recent years. Existing evidence has revealed that diet structure, eating behaviors, chemicals contained in drinking water and food, as well as the amount and/or percentage of specific nutrients taken all have an impact on sleep performance (Dashti et al. 2015; Ghani et al. 2022; Hasan et al. 2021; St-Onge et al. 2016). The sleep–wake cycle is linked to a number of neurotransmitters (Halson 2014). Dietary nutrients, particularly vitamins and minerals, alter hormone levels, biological rhythms and mood in the body via regulating the synthesis and release of these neurotransmitters (Frank et al. 2017; Peuhkuri et al. 2012; Sarris et al. 2012). Our study found that lycopene, vitamin C and vitamin E were associated with decreased SP prevalence, and their benefits for sleep have been documented in several previous studies (Black 2021; Carrasco et al. 2022; Dadashpour et al. 2018; Monfared et al. 2017). Additionally, vitamin A and several carotenoids (alpha-carotene, beta-carotene, beta-cryptoxanthin and lutein + zeaxanthin) were not significantly associated with SP, which has been found in our study and other research (Çakir et al. 2020; Komada et al. 2017). But other studies reported their benefits for sleep (Beydoun et al. 2014; Grandner et al. 2014).
Our findings showed antagonistic associations between B vitamins (vitamin B6, folic acid and niacin) intake and SP. B vitamins have a protective effect on sleep because they are crucial for synthesizing a variety of neurotransmitters (Peters et al. 2015) and can regulate the release of melatonin (Peuhkuri et al. 2012). Animal studies have shown that niacin can greatly increase non-rapid-eye movement sleep by activating niacin receptors GPR109A (Szentirmai and Kapás 2019). Clinical trials have reported that B vitamins are associated with more excellent sleep (Sarris et al. 2012) and might be effective in treating insomnia (Djokic et al. 2019). In contrast, another RCT including 100 participants from across Australia found that B vitamins were significantly linked to lower self-rated sleep quality and greater fatigue upon waking (Aspy et al. 2018). Insufficient sample size, discrepancies in the study population's baseline characteristics and the duration of the intervention may contribute to differences in study results.
Strengths and limitations
This study has some strengths. First, based on sizable and nationally representative samples from a well-established nationwide survey in the US, this study explored the associations of vitamins with HL, VD and SP. Second, our study explored potential associations of multivitamins with various body functions and conducted stratification analyses based on several confounders, allowing for a more thorough knowledge of the roles of vitamins on body functions.
Several limitations need to be acknowledged. First, we cannot examine the causality because of the cross-sectional study design, but it also has significant public health implications. Second, the outcomes of the present study were based on self-reported information with possible recall bias. However, it has been discovered that self-reported assessments of HL, VD and SP are generally reliable (Gomez et al. 2001; Rein et al. 2021; Komada et al. 2017). Third, although we have adjusted for confounders like smoking, drinking and diabetes, there may still be some other confounding factors that may have impacts, such as drug use, family history of disease and other contaminants in food or drinking water (Ambade et al. 2021b; Kurwadkar et al. 2022).
Conclusions
In conclusion, our study shows that specific vitamin intake is associated with decreased prevalence of HL, VD and SP. Dietary intake of alpha-carotene, beta-carotene and lycopene are negatively associated with the prevalence of HL. Increased intake of folic acid, vitamin B6, lutein + zeaxanthin, and alpha- and beta-carotene are associated with a decreased probability of VD. Besides that, properly increasing niacin, folic acid, lycopene, vitamin B6, C and E intakes may contribute to sleep. Future research is required to fully illustrate the biological pathways before forming definite conclusions about these associations.
Data availability
All data generated or analyzed during our study are extracted from the NHANES (https://wwwn.cdc.gov/Nchs/Nhanes/).
References
Abbasi M, Pourrajab B, Tokhi MO (2021) Protective effects of vitamins/antioxidants on occupational noise-induced hearing loss: A systematic review. J Occup Health 63:e12217. https://doi.org/10.1002/1348-9585.12217
Ambade B, Sethi SS (2021) Health Risk Assessment and Characterization of Polycyclic Aromatic Hydrocarbon from the Hydrosphere. J Hazard Toxic Radioact Waste 25:05020008. https://doi.org/10.1061/(ASCE)HZ.2153-5515.0000586
Ambade B, Kumar A, Sahu LK (2021a) Characterization and health risk assessment of particulate bound polycyclic aromatic hydrocarbons (PAHs) in indoor and outdoor atmosphere of Central East India. Environ Sci Pollut Res Int 28:56269–56280. https://doi.org/10.1007/s11356-021-14606-x
Ambade B, Sethi SS, Kumar A et al (2021b) Health Risk Assessment, Composition, and Distribution of Polycyclic Aromatic Hydrocarbons (PAHs) in Drinking Water of Southern Jharkhand, East India. Arch Environ Contam Toxicol 80:120–133. https://doi.org/10.1007/s00244-020-00779-y
Ambade B, Sethi SS, Giri B et al (2022) Characterization, Behavior, and Risk Assessment of Polycyclic Aromatic Hydrocarbons (PAHs) in the Estuary Sediments. Bull Environ Contam Toxicol 108:243–252. https://doi.org/10.1007/s00128-021-03393-3
Aspy DJ, Madden NA, Delfabbro P (2018) Effects of Vitamin B6 (Pyridoxine) and a B Complex Preparation on Dreaming and Sleep. Percept Mot Skills 125:451–462. https://doi.org/10.1177/0031512518770326
Berger RG, Lunkenbein S, Ströhle A, Hahn A (2012) Antioxidants in food: mere myth or magic medicine? Crit Rev Food Sci Nutr 52:162–171. https://doi.org/10.1080/10408398.2010.499481
Beydoun MA, Gamaldo AA, Canas JA et al (2014) Serum nutritional biomarkers and their associations with sleep among US adults in recent national surveys. PLoS One 9:e103490. https://doi.org/10.1371/journal.pone.0103490
Black D (2021) P011 Effect size of vitamin-C on indices of sleep-quality, fatigue, endothelial-function, circulating HIF-1alpha and patient mortality: a systematic review. SLEEP Adv 2:A25. https://doi.org/10.1093/sleepadvances/zpab014.059
Brewczyński A, Jabłońska B, Kentnowski M et al (2021) The Association between Carotenoids and Head and Neck Cancer Risk. Nutrients 14:88. https://doi.org/10.3390/nu14010088
Bungau S, Abdel-Daim MM, Tit DM et al (2019) Health Benefits of Polyphenols and Carotenoids in Age-Related Eye Diseases. Oxid Med Cell Longev 2019:9783429. https://doi.org/10.1155/2019/9783429
Çakir B, Nişancı Kılınç F, Özata Uyar G et al (2020) The relationship between sleep duration, sleep quality and dietary intake in adults. Sleep Biol Rhythms 18:49–57. https://doi.org/10.1007/s41105-019-00244-x
Carrasco C, Blanco L, Abengozar Á, Rodríguez AB (2022) Effects of Lycopene-enriched, Organic, Extra Virgin Olive Oil on Benign Prostatic Hyperplasia: A Pilot Study. Altern Ther Health Med 28:8–15
Chawla J, Kvarnberg D (2014) Hydrosoluble vitamins. Handb Clin Neurol 120:891–914. https://doi.org/10.1016/B978-0-7020-4087-0.00059-0
Choi Y-H, Miller JM, Tucker KL et al (2014) Antioxidant vitamins and magnesium and the risk of hearing loss in the US general population1234. Am J Clin Nutr 99:148–155. https://doi.org/10.3945/ajcn.113.068437
Choi JE, Ahn J, Moon IJ (2021) Associations between Age-Related Hearing Loss and DietaryAssessment Using Data from Korean National Health andNutrition Examination Survey. Nutrients 13:1230. https://doi.org/10.3390/nu13041230
Christ A, Lauterbach M, Latz E (2019) Western Diet and the Immune System: An Inflammatory Connection. Immunity 51:794–811. https://doi.org/10.1016/j.immuni.2019.09.020
Curhan SG, Stankovic KM, Eavey RD et al (2015) Carotenoids, vitamin A, vitamin C, vitamin E, and folate and risk of self-reported hearing loss in women12. Am J Clin Nutr 102:1167–1175. https://doi.org/10.3945/ajcn.115.109314
Dadashpour S, Hajmiri MS, Roshani D (2018) Effect of intravenous vitamin C supplementation on the quality of sleep, itching and restless leg syndrome in patients undergoing hemodialysis; A double-blind randomized clinical trial. J Nephropharmacol 7:131–136
Dashti HS, Scheer FA, Jacques PF et al (2015) Short sleep duration and dietary intake: epidemiologic evidence, mechanisms, and health implications. Adv Nutr 6:648–659. https://doi.org/10.3945/an.115.008623
Dawes P, Cruickshanks KJ, Marsden A et al (2020) Relationship Between Diet, Tinnitus, and Hearing Difficulties. Ear Hear 41:289–299. https://doi.org/10.1097/AUD.0000000000000765
Diab L, Krebs NF (2018) Vitamin Excess and Deficiency. Pediatr Rev 39:161–179. https://doi.org/10.1542/pir.2016-0068
Djokic G, Vojvodić P, Korcok D et al (2019) The Effects of Magnesium - Melatonin - Vit B Complex Supplementation in Treatment of Insomnia. Open Access Maced J Med Sci 7:3101–3105. https://doi.org/10.3889/oamjms.2019.771
Duan H, Pan J, Guo M et al (2022) Dietary strategies with anti-aging potential: Dietary patterns and supplements. Food Res Int 158:111501. https://doi.org/10.1016/j.foodres.2022.111501
Dysken MW, Sano M, Asthana S et al (2014) Effect of vitamin E and memantine on functional decline in Alzheimer disease: the TEAM-AD VA cooperative randomized trial. JAMA 311:33–44. https://doi.org/10.1001/jama.2013.282834
Dziedziak J, Kasarełło K, Cudnoch-Jędrzejewska A (2021) Dietary Antioxidants in Age-Related Macular Degeneration and Glaucoma. Antioxidants (basel) 10:1743. https://doi.org/10.3390/antiox10111743
Evans JR, Lawrenson JG (2017) Antioxidant vitamin and mineral supplements for slowing the progression of age-related macular degeneration. Cochrane Database Syst Rev 7:CD000254. https://doi.org/10.1002/14651858.CD000254.pub4
Fadeyev K, Nagao-Sato S, Reicks M (2021) Nutrient and Food Group Intakes among U.S. Children (2–5 Years) Differ by Family Income to Poverty Ratio, NHANES 2011–2018. Int J Environ Res Public Health 18:11938. https://doi.org/10.3390/ijerph182211938
Flanagan EW, Most J, Mey JT, Redman LM (2020) Calorie Restriction and Aging in Humans. Annu Rev Nutr 40:105–133. https://doi.org/10.1146/annurev-nutr-122319-034601
Frank S, Gonzalez K, Lee-Ang L et al (2017) Diet and Sleep Physiology: Public Health and Clinical Implications. Front Neurol 8:393. https://doi.org/10.3389/fneur.2017.00393
Ghani SB, Delgadillo ME, Granados K et al (2022) Patterns of Eating Associated with Sleep Characteristics: A Pilot Study among Individuals of Mexican Descent at the US-Mexico Border. Behav Sleep Med 20:212–223. https://doi.org/10.1080/15402002.2021.1902814
Gi M, Shim DB, Wu L et al (2018) Progressive hearing loss in vitamin A-deficient mice which may be protected by the activation of cochlear melanocyte. Sci Rep 8:16415. https://doi.org/10.1038/s41598-018-34653-8
Giaconi JA, Yu F, Stone KL et al (2012) The association of consumption of fruits/vegetables with decreased risk of glaucoma among older African-American women in the study of osteoporotic fractures. Am J Ophthalmol 154:635–644. https://doi.org/10.1016/j.ajo.2012.03.048
Goman AM, Lin FR (2016) Prevalence of Hearing Loss by Severity in the United States. Am J Public Health 106:1820–1822. https://doi.org/10.2105/AJPH.2016.303299
Gomez MI, Hwang SA, Sobotova L et al (2001) A comparison of self-reported hearing loss and audiometry in a cohort of New York farmers. J Speech Lang Hear Res 44:1201–1208. https://doi.org/10.1044/1092-4388(2001/093)
Gopinath B, Flood VM, McMahon CM et al (2011) Dietary antioxidant intake is associated with the prevalence but not incidence of age-related hearing loss. J Nutr Health Aging 15:896–900. https://doi.org/10.1007/s12603-011-0119-0
Gopinath B, Flood VM, Rochtchina E et al (2013) Homocysteine, folate, vitamin B-12, and 10-y incidence of age-related macular degeneration. Am J Clin Nutr 98:129–135. https://doi.org/10.3945/ajcn.112.057091
Goshtasbi K, Abouzari M, Risbud A et al (2021) Tinnitus and Subjective Hearing Loss are More Common in Migraine: A Cross-Sectional NHANES Analysis. Otol Neurotol 42:1329–1333. https://doi.org/10.1097/MAO.0000000000003247
Grandner MA, Jackson N, Gerstner JR, Knutson KL (2014) Sleep symptoms associated with intake of specific dietary nutrients. J Sleep Res 23:22–34. https://doi.org/10.1111/jsr.12084
Grover AK, Samson SE (2014) Antioxidants and vision health: facts and fiction. Mol Cell Biochem 388:173–183. https://doi.org/10.1007/s11010-013-1908-z
Halson SL (2014) Sleep in elite athletes and nutritional interventions to enhance sleep. Sports Med 44(Suppl 1):S13-23. https://doi.org/10.1007/s40279-014-0147-0
Hasan MF, Nur-E-Alam M, Salam MA et al (2021) Health Risk and Water Quality Assessment of Surface Water in an Urban River of Bangladesh. Sustainability 13:6832. https://doi.org/10.3390/su13126832
Huang-Link Y, Mirabelli P, Lindehammar H, Link H (2021) Retinal changes associated with multivitamin deficiency before and after supplementation. Acta Neurol Scand 144:209–215. https://doi.org/10.1111/ane.13438
Ibrahim I, Zeitouni A, da Silva SD (2018) Effect of Antioxidant Vitamins as Adjuvant Therapy for Sudden Sensorineural Hearing Loss: Systematic Review Study. Audiol Neurootol 23:1–7. https://doi.org/10.1159/000486274
Jomova K, Valko M (2013) Health protective effects of carotenoids and their interactions with other biological antioxidants. Eur J Med Chem 70:102–110. https://doi.org/10.1016/j.ejmech.2013.09.054
Kabagambe EK, Lipworth L, Labadie RF et al (2018) Erythrocyte folate, serum vitamin B12, and hearing loss in the 2003–2004 National Health And Nutrition Examination Survey (NHANES). Eur J Clin Nutr 72:720–727. https://doi.org/10.1038/s41430-018-0101-6
Kennedy DO (2016) B Vitamins and the Brain: Mechanisms, Dose and Efficacy–A Review. Nutrients 8:68. https://doi.org/10.3390/nu8020068
Kim TS, Chung JW (2019) Associations of Dietary Riboflavin, Niacin, and Retinol with Age-related Hearing Loss: An Analysis of Korean National Health and Nutrition Examination Survey Data. Nutrients 11:E896. https://doi.org/10.3390/nu11040896
Komada Y, Narisawa H, Ueda F et al (2017) Relationship between Self-Reported Dietary Nutrient Intake and Self-Reported Sleep Duration among Japanese Adults. Nutrients 9:134. https://doi.org/10.3390/nu9020134
Kurwadkar S, Dane J, Kanel SR et al (2022) Per- and polyfluoroalkyl substances in water and wastewater: A critical review of their global occurrence and distribution. Sci Total Environ 809:151003. https://doi.org/10.1016/j.scitotenv.2021.151003
Lawrenson JG, Downie LE (2019) Nutrition and Eye Health. Nutrients 11:E2123. https://doi.org/10.3390/nu11092123
Le Prell CG, Gagnon PM, Bennett DC, Ohlemiller KK (2011) Nutrient-enhanced diet reduces noise-induced damage to the inner ear and hearing loss. Transl Res 158:38–53. https://doi.org/10.1016/j.trsl.2011.02.006
Lee CMY, Colagiuri S (2018) Diagnostic Criteria and Classification. In: Bonora E, DeFronzo R (eds) Diabetes. Epidemiology, Genetics, Pathogenesis, Diagnosis, Prevention, and Treatment. Springer International Publishing, Cham, pp 1–17
Li W, Ruan W, Cui X et al (2022) Blood volatile organic aromatic compounds concentrations across adulthood in relation to total and cause specific mortality: A prospective cohort study. Chemosphere 286:131590. https://doi.org/10.1016/j.chemosphere.2021.131590
Markun S, Gravestock I, Jäger L et al (2021) Effects of Vitamin B12 Supplementation on Cognitive Function, Depressive Symptoms, and Fatigue: A Systematic Review, Meta-Analysis, and Meta-Regression. Nutrients 13:923. https://doi.org/10.3390/nu13030923
Martínez-Vega R, Garrido F, Partearroyo T et al (2015) Folic acid deficiency induces premature hearing loss through mechanisms involving cochlear oxidative stress and impairment of homocysteine metabolism. FASEB J 29:418–432. https://doi.org/10.1096/fj.14-259283
Martínez-Vega R, Murillo-Cuesta S, Partearroyo T et al (2016) Long-Term Dietary Folate Deficiency Accelerates Progressive Hearing Loss on CBA/Ca Mice. Front Aging Neurosci 8:209. https://doi.org/10.3389/fnagi.2016.00209
Mathew MC, Ervin A-M, Tao J, Davis RM (2012) Antioxidant vitamin supplementation for preventing and slowing the progression of age-related cataract. Cochrane Database Syst Rev CD004567. https://doi.org/10.1002/14651858.CD004567.pub2
Merle BMJ, Silver RE, Rosner B, Seddon JM (2016) Dietary folate, B vitamins, genetic susceptibility and progression to advanced nonexudative age-related macular degeneration with geographic atrophy: a prospective cohort study. Am J Clin Nutr 103:1135–1144. https://doi.org/10.3945/ajcn.115.117606
Meyer-Ficca M, Kirkland JB (2016) Niacin. Adv Nutr 7:556–558. https://doi.org/10.3945/an.115.011239
Milisav I, Ribarič S, Poljsak B (2018) Antioxidant Vitamins and Ageing. In: Harris JR, Korolchuk VI (eds) Biochemistry and Cell Biology of Ageing: Part I Biomedical Science. Springer, Singapore, pp 1–23
Monfared M, Sadegh M, Gohari Z (2017) Effect of melatonin and vitamin E on EEG, sleep quality and quality of life of shift-working nurses in Arak Hospitals. (Majallah-i dānishgāh-i ̒ulūm-i pizishkī-i Arāk}. Arak Med Univ J 19:1–11
Nunes S, Alves D, Barreto P et al (2018) Adherence to a Mediterranean diet and its association with age-related macular degeneration. The Coimbra Eye Study-Report 4. Nutrition (burbank, Los Angeles County, Calif) 51–52:6–12. https://doi.org/10.1016/j.nut.2017.12.010
Okosun IS, Annor FB, Seale JP, Eriksen MP (2014) Abdominal adiposity and family income-to-poverty ratio in American women. Obes Res Clin Pract 8:e201–e211. https://doi.org/10.1016/j.orcp.2012.12.002
Ongan D, Yuksel A (2017) What to eat for a better sleep in haemodialysis patients: Potential role of B vitamins intake and appetite. Pak J Med Sci 33:417–424. https://doi.org/10.12669/pjms.332.11838
Özkırış M, Kapusuz Z, Karaçavuş S, Saydam L (2013) The effects of lycopene on cisplatin-induced ototoxicity. Eur Arch Otorhinolaryngol 270:3027–3033. https://doi.org/10.1007/s00405-013-2352-0
Park C, Lim H, Moon SK, Park R (2019) Pyridoxine Preferentially Induces Auditory Neuropathy Through Mitochondrial Dysfunction and Endoplasmic Reticulum Stress-Mediated Apoptosis. Ann Otol Rhinol Laryngol 128:117S-124S. https://doi.org/10.1177/0003489419836116
Peters L, Fernstrand AM, Garssen J, Verster JC (2015) P.8.b.002 The effect of dietary intake of vitamin B6 on sleep quality and insomnia. Eur Neuropsychopharmacol 25:S654–S655. https://doi.org/10.1016/S0924-977X(15)30930-5
Peuhkuri K, Sihvola N, Korpela R (2012) Diet promotes sleep duration and quality. Nutr Res 32:309–319. https://doi.org/10.1016/j.nutres.2012.03.009
Pula J (2012) Functional vision loss. Curr Opin Ophthalmol 23:460–465. https://doi.org/10.1097/ICU.0b013e328358c6dc
Ramdas WD, Wolfs RCW, Kiefte-de Jong JC et al (2012) Nutrient intake and risk of open-angle glaucoma: the Rotterdam Study. Eur J Epidemiol 27:385–393. https://doi.org/10.1007/s10654-012-9672-z
Raper N, Perloff B, Ingwersen L et al (2004) An overview of USDA’s Dietary Intake Data System. J Food Compos Anal 17:545–555. https://doi.org/10.1016/j.jfca.2004.02.013
Ratajczak AE, Szymczak-Tomczak A, Rychter AM et al (2021) Does Folic Acid Protect Patients with Inflammatory Bowel Disease from Complications? Nutrients 13:4036. https://doi.org/10.3390/nu13114036
Rein DB, Lamuda PA, Wittenborn JS et al (2021) Vision Impairment and Blindness Prevalence in the United States: Variability of Vision Health Responses across Multiple National Surveys. Ophthalmology 128:15–27. https://doi.org/10.1016/j.ophtha.2020.06.064
Rémi J, Pollmächer T, Spiegelhalder K et al (2019) Sleep-Related Disorders in Neurology and Psychiatry. Dtsch Arztebl Int 116:681–688. https://doi.org/10.3238/arztebl.2019.0681
Rodrigo L, Campos-Asensio C, Rodríguez MÁ et al (2021) Role of nutrition in the development and prevention of age-related hearing loss: A scoping review. J Formos Med Assoc 120:107–120. https://doi.org/10.1016/j.jfma.2020.05.011
Sarris J, Cox KHM, Camfield DA et al (2012) Participant experiences from chronic administration of a multivitamin versus placebo on subjective health and wellbeing: a double-blind qualitative analysis of a randomised controlled trial. Nutr J 11:110. https://doi.org/10.1186/1475-2891-11-110
Shalini T, Jose SS, Prasanthi PS et al (2021) Carotenoid status in type 2 diabetes patients with and without retinopathy. Food Funct 12:4402–4410. https://doi.org/10.1039/d0fo03321a
Shargorodsky J, Curhan SG, Eavey R, Curhan GC (2010) A prospective study of vitamin intake and the risk of hearing loss in men. Otolaryngol Head Neck Surg 142:231–236. https://doi.org/10.1016/j.otohns.2009.10.049
Shieu M, Morgenstern H, Bragg-Gresham J et al (2020) US Trends in Prevalence of Sleep Problems and Associations with Chronic Kidney Disease and Mortality. Kidney 360(1):458–468. https://doi.org/10.34067/KID.0000862019
Shiue I (2013) Urinary environmental chemical concentrations and vitamin D are associated with vision, hearing, and balance disorders in the elderly. Environ Int 53:41–46. https://doi.org/10.1016/j.envint.2012.12.006
Spankovich C, Hood LJ, Silver HJ et al (2011) Associations between diet and both high and low pure tone averages and transient evoked otoacoustic emissions in an older adult population-based study. J Am Acad Audiol 22:49–58. https://doi.org/10.3766/jaaa.22.1.6
St-Onge M-P, Mikic A, Pietrolungo CE (2016) Effects of Diet on Sleep Quality12. Adv Nutr 7:938–949. https://doi.org/10.3945/an.116.012336
Szentirmai É, Kapás L (2019) Nicotinic acid promotes sleep through prostaglandin synthesis in mice. Sci Rep 9:17084. https://doi.org/10.1038/s41598-019-53648-7
Tan AG, Mitchell P, Rochtchina E et al (2014) Serum homocysteine, vitamin B12, and folate, and the prevalence and incidence of posterior subcapsular cataract. Invest Ophthalmol vis Sci 56:216–220. https://doi.org/10.1167/iovs.14-15531
Tawfik A, Elsherbiny NM, Zaidi Y, Rajpurohit P (2021) Homocysteine and Age-Related Central Nervous System Diseases: Role of Inflammation. Int J Mol Sci 22:6259. https://doi.org/10.3390/ijms22126259
Thomas-Valdés S, das Tostes MGV, Anunciação PC et al (2017) Association between vitamin deficiency and metabolic disorders related to obesity. Crit Rev Food Sci Nutr 57:3332–3343. https://doi.org/10.1080/10408398.2015.1117413
Vlachos GS, Scarmeas N (2019) Dietary interventions in mild cognitive impairment and dementia. Dialogues Clin Neurosci 21:69–82
Williams PA, Harder JM, Foxworth NE et al (2017) Vitamin B3 modulates mitochondrial vulnerability and prevents glaucoma in aged mice. Science (american Association for the Advancement of Science) 355:756–760. https://doi.org/10.1126/science.aal0092
Wu J, Cho E, Willett WC et al (2015) Intakes of Lutein, Zeaxanthin, and Other Carotenoids and Age-Related Macular Degeneration During 2 Decades of Prospective Follow-up. JAMA Ophthalmol 133:1415–1424. https://doi.org/10.1001/jamaophthalmol.2015.3590
Yamasoba T, Lin FR, Someya S et al (2013) Current concepts in age-related hearing loss: epidemiology and mechanistic pathways. Hear Res 303:30–38. https://doi.org/10.1016/j.heares.2013.01.021
Yu F, Hao S, Zhao Y et al (2011) In utero and lactational β-carotene supplementation attenuates D-galactose-induced hearing loss in newborn rats. Food Chem Toxicol 49:1697–1704. https://doi.org/10.1016/j.fct.2011.04.009
Yuan P, Cui S, Liu Y et al (2020) Metabolic engineering for the production of fat-soluble vitamins: advances and perspectives. Appl Microbiol Biotechnol 104:935–951. https://doi.org/10.1007/s00253-019-10157-x
Zampatti S, Ricci F, Cusumano A et al (2014) Review of nutrient actions on age-related macular degeneration. Nutr Res 34:95–105. https://doi.org/10.1016/j.nutres.2013.10.011
Acknowledgements
We thank the study group of the National Health and Nutrition Examination Survey.
Funding
The study was supported by the Fundamental Research Funds for the Central Universities (2021XXJS017), Health Commission of Hubei Province scientific research project (WJ2023M002), and National key research and development program of China (2022YFC2503203). The funder did not play any role in the study design; in the collection, analysis, and interpretation of data; in the writing of the report; nor in the preparation, review, or approval of the manuscript.
Author information
Authors and Affiliations
Contributions
ZMC wrote the manuscript and performed statistical analysis. ZMC, LLY and DMW conceived and designed the study, and interpreted data. WHC, DMW, LLY, WZL, HZZ, XZH critically revised the manuscript and approved the final version. ZMC, LLY and DMW are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhaomin Chen and Linling Yu are contributed equally to this work and should be considered co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, Z., Yu, L., Li, W. et al. Association of vitamins with hearing loss, vision disorder and sleep problem in the US general population. Environ Sci Pollut Res 30, 53876–53886 (2023). https://doi.org/10.1007/s11356-023-26164-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-26164-5