Abstract
A number of nutritional supplements containing antioxidants are advertised for better vision health. Do they benefit the average consumer? The literature was examined for the effectiveness of antioxidants for human eye health, and for the intricacies in collection of such evidence. The following diseases were considered: cataract, glaucoma, age-related macular degeneration (AMD), retinopathy, retinitis pigmentosa, eye infections, and uveitis. The literature indicates that antioxidant supplements plus lutein have a reasonable probability of retarding AMD. For glaucoma, such supplements were ineffectual in some studies but useful in others. In some studies, antioxidant rich fruits and vegetables were also useful for protection against glaucoma. For diabetic retinopathy, antioxidant supplements may have a small benefit, if any, but only as an adjunct to glycemic control. In very high-risk premature retinopathy and retinitis pigmentosa, antioxidant supplements may be beneficial but those with excess Vitamin E should be avoided. For cataract, there is no evidence for an advantage of such nutritional supplements. However, lubricant drops containing N-acetylcarnosine may be helpful in initial stages of the disease. For eye infections and other causes of uveitis, antioxidants have not been found useful. We recommend that a diet high in antioxidant rich foods should be developed as a habit from an early age. However, when initial signs of vision health deterioration are observed, the appropriate nutritional supplement products may be recommended but only to augment the primary medical treatments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
When people think about the loss of any of the human senses, loss of sight is often the most feared, even though sight-impaired humans may remain extremely capable. Leonard Euler lost the sight in his right eye in 1735 and then in the left eye in 1766. Yet the great mathematician continued to publish one mathematical paper per week in 1775. To put these publications in perspective, few mathematics professors publish as many papers in their lifetime as the sightless Euler did in the year 1775 alone. The American musicians Stevie Wonder and Ray Charles, the ancient Indian poet Surdas, and Louis Braille who invented Braille writing are further examples that the loss of sight is not in any way connected to loss of other senses. Yet it is scary for us to think of having to find new ways of dealing with everyday life after a potential loss of sight. Vision loss is very prevalent. As of 2002, there were over 131 million people visually impaired (best corrected visual acuity less than 20/40 in the better seeing eye) of which over 30 million were blind (best corrected acuity of less than 20/200 in the better seeing eye) [1, 2]. The major causes for blindness are cataract, glaucoma, macular degeneration, retinoblastoma, and retinopathy (Fig. 2). Infections and accidental damage to the eye also play a role. Some of these factors are inherited but others are preventable.
A small number of individuals are born blind either due to genetic disposition or infections during birth or in early childhood. However, blindness increases with age, globally—under the age of 15 just over a million people are blind but over the age of 50, there are over 30 million [1]. With age there is an increase in the prevalence of cataract, glaucoma, macular degeneration, retinopathy, and other causes of blindness. Recent advances in health care have provided the means to prevent and/or decrease blindness due to several of these causes—either by surgery or by medication. It has been hypothesized that antioxidants may be of benefit in retaining better vision or even reversing vision impairment. There are a number of antioxidant products in the market for systemic or topical use. The advice on their usefulness comes from various types of sources. This information is of variable quality and its availability is not subject to regulation [3]. The objective of this review is to critically examine what, if any, benefits these antioxidants may provide. The approach is to examine each of the major causes of blindness, the rationale for the use of antioxidants associated with each situation, and then examine studies in which such antioxidants were used either as treatment or for prevention. As background, first brief descriptions are provided for the human eye and for reactive oxygen species (ROS).
Human eye
The human eye is a complex structure (Fig. 2, http://www.ncbi.nlm.nih.gov/books/NBK11534/). It photo images objects with the aid of a lens and an adjustable aperture and sends these images to the brain for analysis. Anterior most in the eye are the eyelids, which provide physical protection to it and are followed by the conjunctiva, aqueous humor, iris to control the aperture, a lens that sits on a hyaloid membrane, and is followed by vitreous humor. The inner or nuclear part of the lens contains the mass of crystalline fibers that focus light on the retina. The posterior structures are vitreous humor, choroid and the optic nerve, and the sclera. The exact spatial organization of these structures is paramount and it is maintained by the surrounding epithelial cells. Thus, an eye is a versatile camera, a signal relay system, and image analysis hardware and software—all made up of living structures.
Reactive oxygen species
An atom or a molecule with unpaired electrons in its outermost orbit is termed a free radical—when the atom involved is oxygen, it is called an oxygen free radical [4]. ROS may be free radicals or even oxidizing substances such as peroxide. Typically our body oxidizes substances such as glucose to produce energy needed for our living. During this process, in every cell of the body, oxygen molecules are reduced in a stepwise manner to yield reactive intermediates, such as superoxide, hydrogen peroxide, and hydroxyl radical. The ROS are normally present in very low concentrations (nanomolar to micromolar). For defense purposes, cells such as macrophages may also produce large amounts of superoxide and peroxynitrite. Under normal circumstances, our body uses natural antioxidants, such as vitamin C (ascorbate), vitamin E, glutathione, and naturally occurring enzymes to scavenge these ROS. However, under certain conditions excess accumulation of reactive oxygen may alter the nature of lipids and proteins and ultimately cause cellular dysfunction. Prolonged damage due to accumulated ROS in different tissues of the eye may cause irreversible damage. Another interesting aspect is that oxidative stress increases with age, and vision health decreases with age [5, 6]. Therefore, the question becomes, is there any evidence that such damage can be prevented or repaired using antioxidants.
Eye diseases
Cataract
Normally, the eye lens is transparent but it becomes opaque in a cataract because of hereditary factors, exposure to ultraviolet radiation or chemicals, or risk factors associated with diseases such as diabetes mellitus. In general, cataract formation increases with age and is more prevalent in females than in males. It is more common in countries near the equator than in USA, Canada, or Northern Europe [1]. This exposure has been associated with damage caused by ROS formed due to ultraviolet radiation. When opaque, the natural lens can be replaced with a plastic transparent lens in routine cataract surgery. However, it has been reported that the natural lens exports the antioxidant glutathione to the fluids bathing it [7]. Consequently, the cataract surgery using a synthetic lens may deplete the eye of this resource. The scientific rationale for the use of antioxidants in prophylaxis and treatment of cataract has recently been reviewed [7]. Several products have been used to preserve eyes against cataract.
A double blind study was conducted over 2 years for treatment of cataract with drops containing N-acetylcarnosine with 75 patients and 72 control subjects [8]. The patients received lubricant drops containing 1 % N-acetylcarnosine or placebo drops with the same formulation but without this antioxidant. The vision improved with the drug after 9 months as determined by glare test and visual acuity test. Even control patients reported some improvement in their vision. The work in this study was supported by the manufacturer of the drops—Innovative Vision Product and hence a conflict of interest cannot be overlooked. Another study conducted by the same company is titled “N-acetylcarnosine lubricant eye drops possess all-in-one universal antioxidant protective effects of L-carnosine in aqueous and lipid membrane environments, aldehyde scavenging, and transglycation activities inherent to cataracts: a clinical study of the new vision-saving drug N-acetylcarnosine eyedrop therapy in a database population of over 50,500 patients” [9]. These findings are supported by a case study on a 72 year old male [10] (no conflict of interest). However, the mode of action of these drops may not be an antioxidant effect. The role of the N-acetylcarnosine in preventing oxidative damage to crystalline lens in mammalian eye has been investigated using Radical Probe Mass Spectrometry but the antioxidant did not directly have a significant effect on the oxidation of the most abundant lens crystallins, α and β-crystallin [11]. The study concluded that the therapeutic benefit observed in the clinical trials may be associated with other ingredients in the formulation of the topical solution and/or that the mode of action of N-acetylcarnosine as an antioxidant is not a direct one.
In a double blind study, the effect of nutritional supplementation with antioxidants was examined on the progression of cataract in 798 subjects (35–50 years old) over a 5 year period [12, 13]. Three times weekly, the subjects received tablets containing 500 mg vitamin C, 15 mg vitamin A and 15 mg vitamin E or identical appearing placebo tablets. There was no significant difference between the treatment and the placebo groups in nuclear opalescence and color of the lens, cataract (cortical or posterior subcapsular), or mean spherical equivalent refractive error of the lens. Scrutiny of the data suggests that there may have been some age dependence of the effects, and hence there was a need for inclusion of older subjects. However, a multicenter study with a cohort of 55–80 year old 4,757 relatively well-nourished patients showed that a high-dose formulation of vitamin C, vitamin E, and beta-carotene did not significantly affect the risk of development or progression of the age-related lens opacities or visual acuity loss over a 7 year period [14]. This observation has been confirmed in meta-analysis studies and reviews [14–17].
Glaucoma
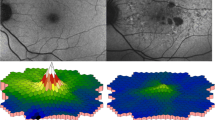
Glaucoma is characterized by an increased narrowing of the field of vision (Fig. 1) resulting from damage to the optic nerve over time [18]. It is the second major cause of blindness. In the USA alone, over two million people suffer from glaucoma [2]. There are two major forms of glaucoma—closed and open angle. The angle pertains to the area between the iris and cornea, through which aqueous fluid must flow to escape via the trabecular meshwork in the eye. The closed angle glaucoma is less common but very painful and hence it is detected more rapidly due to an extremely high ocular pressure. The open-angle glaucoma develops gradually and often goes unnoticed except in eye tests. High intraocular pressure is the main risk factor in glaucoma but exceptions exist: some patients with the high pressure may never develop the disease and some glaucoma patients may not develop high intraocular pressure [18]. Additional risk factors are age, family history, diabetes, hypertension, thin corneas, and the use of corticosteroids or cholesterol lowering drugs. Intraocular pressure is controlled by the rate of filtration of aqueous humor from the trabecular meshwork. The rate of filtration is regulated by changes in the ionic conductances of chloride and potassium channels that regulate the volume of the trabecular meshwork cells. Defects in such conductance have been associated with glaucoma [19]. Endothelin has also been implicated in the optical nerve damage in glaucoma. In normal pressure glaucoma, endothelin-1 may produce systemic and local vascular dysregulation while in the high pressure glaucoma, its effect may be localized to the ocular tissue [20]. Tests for glaucoma include intraocular pressure measurements, stereoscopic dilated eye exam, visual field tests, measurement of the angle where iris meets the cornea, measurement of corneal thickness and monitoring optic nerve damage by imaging. The treatments for management include lowering the intraocular pressure by pharmacological and surgical (including laser surgery) means [18, 21]. The pharmacological treatments not only inhibit the secretion of the aqueous humor but may also stimulate chronic its outflow through the uveoscleral pathway.
Major causes of blindness as percent total. Figure is based on data on global blindness from [1]. Pictures showing how the vision is affected by each type of blindness are from the websites given in the Acknowledgments section
There are several studies associating deficiency in antioxidant levels to glaucoma. The transporter, SLC23A2, plays a major role in delivering vitamin C to various cells. A single nucleotide polymorphism in the gene related to this vitamin C transporter has been significantly associated with a higher risk of primary open-angle glaucoma [22]. In one study, 47 patients with glaucoma and 44 control subjects were examined for serum levels of vitamin A, C, E, B9, and uric acid [23]. Vitamin C levels were lower in the patients than in the control subjects, uric acid levels were higher, and levels of the other substances examined were not significantly different. Oxidative activity in the aqueous humor of the eye is higher in glaucoma patients. Consistent with the notion that the antioxidant levels in the aqueous humor may be associated with glaucoma and hence antioxidant supplementation should be useful is consistent with the findings that some of the treatments used for glaucoma also decrease oxidative stress. For instance, the carbonic anhydrase inhibitor dorzolamide, which is used to lower the intraocular pressure, also decreases the oxidative stress in the eye [24]. Similarly, the β-adrenergic receptor antagonist timolol, which is used to decrease the production of aqueous humor by the ciliary epithelium also exerts a direct antioxidant effect thereby protecting these cells from oxidative stress [25].
A cross-sectional study was conducted on the roles of vitamins A, C, and E on glaucoma in 2,912 participants aged greater than 40 years [26]. The participants were interviewed regarding the use of dietary supplements during the preceding 30-day period. Serum levels of these substances were also determined. Neither the supplementary consumption of vitamin A and E nor its serum levels correlated with the glaucoma prevalence. However, vitamin C consumption correlated with the decrease in the odds of developing glaucoma. It is interesting that the serum levels of vitamin C did not correlate as anticipated. A major pitfall of this study is its being based on the use of antioxidants only during a period of 30 days. Another study on the dietary intake of 3,502 participants aged 55 years and older was based on questionnaires. It also had a much longer follow-up (average 9.7 years) period [27]. It aimed to determine, if the incidence of glaucoma was affected by dietary intake of nutrients that either have antioxidative properties (carotenoids, vitamins, and flavonoids) or influence the blood flow in the eye. Retinol equivalents and vitamin B1 were found to be protective. In another study, the incidence of glaucoma was examined in African-American women who had osteoporosis related fractures. A food frequency questionnaire was used in this study [28]. It was concluded that a higher consumption of fruits and vegetables rich in vitamins A and C and in carotenoids may be associated with a decreased likelihood of glaucoma in the older African-American women. In another study, questionnaires of 76,200 participants were followed up biennially for 6 years to determine if there was any correlation between the dietary supplements and the development of open angle glaucoma [29]. Consumption of alpha-carotene, beta-cryptoxanthin, or vitamin C or vitamin A was not strongly associated with a decrease in the risk of primary open-angle glaucoma.
In a Phase I cross-over study of 11 normal healthy individuals Ginkgo biloba extract increased blood flow to the optic nerve [30]. In another study over 6–59 months, anthocyanins from bilberry and extracts from G. biloba improved best corrected visual acuity [31]. Beneficial effects of the G. biloba extracts have also been reported in other studies [32, 33].
Macular degeneration
Age-related macular degeneration (AMD) is the most common form of macular degeneration although the macula may also be affected in younger individuals [34]. AMD is the most common form of vision loss in people over 50. The back of the eye contains the light sensitive retina, and the central part of the retina which provides the most detailed central vision is termed the macula. Posterior to the retina is the blood vessel containing choroid tissue, which nourishes the retina. AMD may be either dry (more common) or wet type. Dry AMD is due to deposition of drusen (plaque like structures) between the macula and the choroid. Wet AMD is due to an overgrowth of blood vessels in the choroid and may even cause a retinal detachment. In AMD, the loss of vision begins at the macula and may increase to peripheral areas. The prevalence of AMD is age-related. For instance in the US, ~20,000 persons under the age of 50 have AMD, while this figure increases with age to over a million after the age of 80 [2]. The risk factors associated with AMD include genetic, hypertension, high cholesterol, obesity, exposure to sunlight, smoking, and oxidative stress. Early detection of AMD has been facilitated by recent advances in technology and older patients are often recommended to take dietary supplements containing antioxidants and several products have been developed for this purpose (Fig. 2).
Schematic structure of the human eye. Modified from http://www.onlinenursingprograms.com/assets/Anatomy_and_physiology_of_animals_Structure_of_the_eye-300x167.jpg
In the Age-Related Eye Diseases Study 1 (AREDS1), a multicenter double blind clinical trial was conducted over 6.3 years with 3,640 subjects aged 55–80 years [35]. The subjects received daily oral tablets containing antioxidants (500 mg vitamin C, 268 mg vitamin E, and 15 mg β-carotene), zinc and copper or the three antioxidants plus zinc or a placebo. Advanced AMD was monitored by color fundus photography. As anticipated, in subjects receiving only the placebo the probability of development of advanced AMD increased with age. However, this probability decreased consistently over the years for the subjects that received antioxidants plus zinc (Fig. 3). Subjects receiving only antioxidants or zinc showed a smaller decrease in this probability. Similarly, the probability of visual acuity loss also increased with age and the increase was smaller for the treated groups. Another similar study (AREDS2) has also been conducted. It included lutein plus zeaxanthine, eicosapentaenoic acid, and docosahexaenoic acid in addition to the previous antioxidants and showed that these agents may add to the advantage over those used in AREDS1 [36]. Lutein plus zeaxanthine were of some advantage which was not statistically significant (p < 0.1), and eicosapentaenoic acid and docosahexaenoic acid did not show any benefits. Interestingly, the inclusion of β-carotene increased the risk of lung cancer among the former smokers. β-carotene supplementation has also been contraindicated by others in people who smoke or have been exposed to asbestos [37]. A recent review based on 13 randomized control trials concluded that “people with AMD may experience delay in progression of the disease with antioxidant vitamin and mineral supplementation” [38]. In contrast, a meta-analysis study concluded that there was no benefit of antioxidants in prevention of early AMD [39]. However, several of the studies considered in the meta-analysis were not well controlled or conducted.
Effect of antioxidant supplements in the probability of AMD with number of years in the follow up in AREDS1 study [35]. Subjects in the study were 55–80 years old, and followed up for several years. The probability of AMD development increased with the years in both groups but the increase was smaller in the antioxidant plus zinc group than in the placebo group
In another study, the effect of saffron was examined in 29 early AMD patients and an increase in visual acuity was observed [40]. It is noted that this study was supported by the company that marketed the saffron pills.
Retinopathy
Retinopathy occurs from persistent or acute damage to the retina. As a result, inflammation and vascular remodeling may occur gradually over a prolonged period. Hence, the patient is often not fully aware of the extent of the disease [41, 42]. Diabetes mellitus is the major risk factor associated with retinopathy. The other risk factors are hypertension, sickle cell anemia, radiation, and exposure to ultraviolet rays. The disease is most prevalent in affluent countries—in the USA alone 4 million people over the age of 40 suffer from diabetic retinopathy [2]. Diabetic retinopathy results from damage to the microvasculature of the retina and the light sensitive tissue at the back of the eye. By the time the disease is evident to the patient, significant smooth muscle and endothelial cell damage has occurred leading to an oxygen deprived retina. The problem comes when the tissues attempt to repair the retina and cause the blood vessels to become occluded and ischemic [41]. One of the changes is an increase in the vascular endothelial growth factor pathway and hence a potential treatment is the use of antibodies against this growth factor [42]. Another form of the disease is retinopathy of prematurity which is limited to premature low birth weight babies and results from a birth interrupting normal retinal vascular development. Oxygen therapy exacerbates this condition [43]. In some instances, the disease may also be hereditary.
In one study, the effect of antioxidant supplementation on diabetic retinopathy was evaluated over a 5 year follow-up period [44]. It is not clear if it was a double blind study. However, the supplementation did not change the best corrected visual acuity but it retarded the retinopathy stage when compared to the patients with no antioxidant supplementation. It was concluded that the antioxidant supplementation could be useful only as an adjunct to the long-term therapy of this disease. In another study, over a 6 year period supplementation with Vitamin C and E, a limited protection was observed [45]. Since, antioxidants are effective in animal models as prevention but do not work effectively in human clinical studies, it is suggested that it is because by the time diabetes is detected too much damage has already occurred [41]. Thus, early glycemic control appears to be the best preventive measure in diabetic retinopathy.
A meta-analysis of 6 trials evaluated the effects of vitamin E in premature retinopathy [46]. The treatment reduced the risk of retinopathy only in some very low birth weight infants but some negative effects were also observed. It was concluded that the treatment should be limited only to the highest risk very low birth weight infants. Another study also showed small benefits, but recommended that the serum concentrations of vitamin E should be closely monitored to prevent complications of sepsis [47]. Treatment with vitamin E in combination with cryotherapy may also reduce severity of the disease [48]. Lutein and zeaxanthin have also been shown to be ineffective in the treatment of this disease [49]. In another multicenter randomized study for prevention of bronchopulmonary dysplasia, preterm infants received intratracheal recombinant superoxide dismutase or placebo every 48 h for 1 month after the birth and the incidence of retinopathy was examined post hoc [50]. In the whole cohort, there was no effect on retinopathy but when the 24 infants born at less than 25 weeks of gestational age were considered, severe retinopathy was found in 42 % with the placebo treatment and only in 25 % with the superoxide dismutase treatment (p < 0.03). This reinforces the conclusion that antioxidants may be effective only in very low birth weight infants.
Retinitis pigmentosa
Retinitis pigmentosa includes many disorders with degeneration of the photoreceptor containing cells (rods and cones) in the retina. Some authors term it pigmentary retinopathy and include in it all the non-inflammatory inherited diseases in which rods and cones degenerate [51]. The disease is also characterized by specks of the black pigment melanin in the retina. In most cases, the disease is inherited. Genetic loci underlying different forms of this disease have been reported in several chromosomes [52]. Early symptoms of the disease are an impaired adaptation to light/dark environment and night blindness. There are difficulties with mid-peripheral visual fields in adolescence and then there is a slow progressive loss of peripheral vision over many years until only central (tunnel) vision remains. In some patients, it may eventually cause total blindness. The disease has been associated with apoptosis which may be induced by multiple causes including ischemia, toxic substances, neoplastic transformations, radical damage, trophic factor withdrawal, and external factors [51, 52]. The potential treatments are based on the causes of the disease. They include gene therapy, arresting or slowing the progression of degeneration of photoreceptors with antioxidants and other nutritional supplements, neurotrophic factors and other pharmaceutical agents, a regeneration of the lost tissues or photoreceptors, and use of electronic implants [51–56].
In a randomized trial on the effects of vitamins A and E on retinitis pigmentosa, cone electrogram amplitude was measured as the outcome. It was concluded that vitamin A was beneficial in preventing a decline in this amplitude but vitamin E had an adverse effect [57]. This publication, however, was criticized by peers as being inaccurate as based on several letters in the journal where the original findings were published. For patients receiving vitamin A, the addition of docosahexaenoic acid (an omega-3 acid) or lutein further slowed the course of the disease [53, 55, 57]. Another study examined the effect of the formula taurine, diltiazem and vitamin E on the progression of visual field in this disease. A beneficial effect of the treatment was reported [54]. It was concluded that this benefit was “likely through a protective action from free radical reactions in affected photoreceptors”. However, one cannot rely on this study since the results with individual components in the formula were not reported.
Other eye diseases
Eye infections are a major cause of blindness. Trachoma is caused by infection of Chlamydia trachomatis. Globally as many as 40 million people may have an active infection and as many as 8 million may be visually impaired as a result [1]. The disease is most prevalent in African and Middle Eastern countries and in China and Mongolia. Treatment with the oral or topical antibiotic azithromycin is the most effective [58]. Onchocerciasis (also called river blindness or Robles disease) is an African parasitic disease caused by infection by the roundworm Onchocerca volvulus. It is best treated by ivermectin [59].
Inflammation of the uvea (the vascular, pigmented middle layer of the eye wall) may be caused by infection from various agents or by chemical and mechanical injuries. It is also common in people with autoimmune diseases. It is termed uveitis and its treatment depends on the cause of the inflammation. Vitamins C and E have been used in several studies on uveitis but not found to be definitively useful [60–62].
Analysis and summary
An opinion based on key useful observations from various studies is distilled below. In today’s so-called evidence based medical environment there are several problems in conducting studies on the effects of nutrient supplements. First, most humans consume antioxidants in their diet and the antioxidant levels in the body may also be affected by activities. Studies can at best, pretend to monitor them. This is different from animal studies where diet and activities can be controlled. The second problem is the placebo effect which is not easily preventable. These two problems together cloud the use of appropriate controls. The third is patient compliance which is not easy over long-term periods with nutritional supplements. Meta-analysis studies in this area are replete with their own problems. It is not clear if and how such studies can come to any rational conclusions in combining studies which use different antioxidants, different dosages of these, diverse populations, and individual methods of assessment. As a result, there are very few meta-studies in this area that are really meaningful. Finally, even though nutritional supplements are a multibillion dollar industry, it is nothing compared to the allopathic industry in terms of its revenues. Hence, there is a much smaller level of interest in conducting rigorous experiments except, of course, where conflicts of interest may be involved. Considering all these problems, we summarize below the effects of antioxidants on eye diseases.
For cataract, the effects of nutritional supplementation of vitamin C, 500 mg; vitamin A and vitamin E have been examined in several well-conducted studies with follow ups and in well-nourished patients there is no apparent effect on the development and progression in lens opacities or visual acuities related to cataract. N-acetylcarnosine containing lubricant drops may be useful in initial stages of the disease.
For glaucoma, antioxidants were ineffectual in some studies but in one study vitamin C consumption correlated with the decrease in the odds of developing glaucoma and in another retinol equivalents and vitamin B1 were found to be protective. Interestingly, a higher consumption of fruits and vegetables rich in vitamins A and C and carotenoids may be associated with a decreased likelihood of glaucoma in older African-American women. Similarly, the extracts of the herb G. biloba have been found useful in several studies. However, the role of the placebo effect in these studies cannot be ruled out.
For AMD, the multicenter double blind AREDS1, showed that daily oral tablets containing antioxidants (500 mg vitamin C, 400 IU vitamin E, and 15 mg beta-carotene) plus zinc decreased the probability of development of advanced AMD with age compared to the control subjects. Beneficial effects of antioxidants on AMD have also been observed in several other studies but not in all of them. Beta-carotene supplementation is contraindicated in people who smoke or have been exposed to asbestos.
For diabetic retinopathy, an early glycemic control appears to be the best preventive measure but antioxidant supplementation may be useful only as an adjunct. In premature retinopathy, the benefit of antioxidants is limited to very low birth weight infants and excess vitamin E should be avoided as it may lead to sepsis.
For retinitis pigmentosa, vitamin A, DHA and lutein may be beneficial, but vitamin E may have an adverse effect. For eye infections and other causes of uveitis, antioxidants have not been found to be very effective.
Conclusions and recommendations
Humans are living longer lives than before. The oxidative stress levels and vision health both worsen with age. With this association, one can consider the increased oxidative stress as a risk factor in age-related vision health. However, oxidative stress is not the only risk factor. There are also environmental factors, such as prolonged exposure to ultraviolet rays, eye infections, and physical injury factors. Precautions against them should be primary. The use of medical procedures and pharmacological treatments is pivotal to prevention and treatment of vision loss. Having said that, can antioxidant containing food supplements be used for the betterment of vision health? In the case of AMD, glaucoma, and low birth weight retinopathy it is most likely but for other diseases, it is questionable. One can turn this question around and ask if it can be harmful to take antioxidant supplements as a precautionary measure. Except for the use of excessive vitamin E in retinal pigmentosa, no harm has been proven.
The antioxidant containing supplements in the market today are expensive. Also, considering the case of African-American women discussed in this paper, one may ask why not rely on foods for the antioxidants. Table 2 compares the antioxidant contents per 100 g of fruits and vegetables with those of the supplement products listed in Table 1. Carrots, kale, phalsa, and gojiberry are rich in β-carotene while chocolate, nuts, and sea buckthorn berry are rich in vitamin E. Vitamin C is present in many fruits and vegetables with guava being one of the richest sources. Chocolates and nuts are also rich in zinc and copper. Kale, the superfood is also rich in lutein and zeaxanthin, while gojiberries are extremely rich in zeaxanthin. Gojiberries, guava, and tomato also contain large amounts of lycopene that is present in many of the vision health nutrient supplement products (not shown in Tables 1 or 2). Some herbs and spices may also be rich in antioxidants but they are not listed here since they are consumed in much smaller amounts than the fruits and vegetables.
Is nourishment based on locally available antioxidant rich foods sufficient for everyone? The daily dose of these antioxidants used in the AREDS2 trial was 15 mg β-carotene, 268 mg vitamin E, 500 mg vitamin C, 80 mg zinc as zinc oxide, 2 mg copper as copper oxide, 10 mg lutein, and 2 mg zeaxanthin [36]. A comparison with these doses may not be a perfect answer since it is not clear whether this amount of each of these components is really needed. The ranges of the daily doses of the antioxidant contents in the various supplementary products listed in Table 1 are: 0–17 mg β-carotene, 7–536 mg vitamin E, 45–3,000 mg vitamin C, 7–150 mg zinc, 1–3 mg copper, 0–100 mg lutein, and 1–6 mg zeaxanthin. Similarly, the various studies have also used different doses and combinations of the antioxidants [63]. In one paper, the following are the recommended daily amounts for a non-smoking male: 15 mg vitamin E, 90 mg vitamin C, 15 mg zinc, and 6 mg lutein [63]. These are quite different from the AREDS1 or 2 studies. Based on the study discussed in this paper on African-American women, the ARED1 and ARED2 studies and the variability in the products used in the market and in the doses used in different studies, we make the following general recommendations. We recommend that a diet high in antioxidant rich foods should be developed as a habit from an early age. However, when initial signs of vision health deterioration are observed, the appropriate nutritional supplement products may be recommended but only to augment the primary medical treatments. The appropriateness of the recommendation should also include considerations of potential adverse effects in segments of the populations.
References
Resnikoff S, Pascolini D, Etya’ale D, Kocur I, Pararajasegaram R, Pokharel GP, Mariotti SP (2004) Global data on visual impairment in the year 2002. Bull World Health Organ 82:844–851
Congdon N, O’Colmain B, Klaver CC, Klein R, Munoz B, Friedman DS, Kempen J, Taylor HR, Mitchell P (2004) Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol 122:477–485
Gunasekera V, Ernst E, Ezra DG (2008) Systematic internet-based review of complementary and alternative medicine for glaucoma. Ophthalmology 115:435–439
Walia M, Kwan CY, Grover AK (2003) Effects of free radicals on coronary artery. Med Princ Pract 12:1–9
Romano AD, Serviddio G, de Matthaeis A, Bellanti F, Vendemiale G (2010) Oxidative stress and aging. J Nephrol 23(Suppl 15):S29–S36
Oliveira BF, Nogueira-Machado JA, Chaves MM (2010) The role of oxidative stress in the aging process. Sci World J 10:1121–1128
Varma SD, Kovtun S, Hegde KR (2011) Role of ultraviolet irradiation and oxidative stress in cataract formation-medical prevention by nutritional antioxidants and metabolic agonists. Eye Contact Lens 37:233–245
Babizhayev MA, Burke L, Micans P, Richer SP (2009) N-Acetylcarnosine sustained drug delivery eye drops to control the signs of ageless vision: glare sensitivity, cataract amelioration and quality of vision currently available treatment for the challenging 50,000-patient population. Clin Interv Aging 4:31–50
Babizhayev MA, Micans P, Guiotto A, Kasus-Jacobi A (2009) N-acetylcarnosine lubricant eyedrops possess all-in-one universal antioxidant protective effects of L-carnosine in aqueous and lipid membrane environments, aldehyde scavenging, and transglycation activities inherent to cataracts: a clinical study of the new vision-saving drug N-acetylcarnosine eyedrop therapy in a database population of over 50,500 patients. Am J Ther 16:517–533
Misner B (2012) What are the effects of topical N-acetylcarnosine [eye drops] on cataract-inhibited vision in an elderly subject?—a case report. Web Med Central http://webmedcentral.com/article_view/3214
Ha JW, Schwahn AB, Downard KM (2010) Ability of N-acetylcarnosine to protect lens crystallins from oxidation and oxidative damage by radical probe mass spectrometry (RP-MS). Rapid Commun Mass Spectrom 24:2900–2908
Gritz DC, Srinivasan M, Smith SD, Kim U, Lietman TM, Wilkins JH, Priyadharshini B, Aravind S, Prajna NV, Smolin G, Thulasiraj RD, Selvaraj S, Whitcher JP (2006) Antioxidants in prevention of cataracts in South India: methodology and baseline data. Ophthalmic Epidemiol 13:97–107
Gritz DC, Srinivasan M, Smith SD, Kim U, Lietman TM, Wilkins JH, Priyadharshini B, John RK, Aravind S, Prajna NV, Duraisami TR, Whitcher JP (2006) The Antioxidants in Prevention of Cataracts Study: effects of antioxidant supplements on cataract progression in South India. Br J Ophthalmol 90:847–851
Toh T, Morton J, Coxon J, Elder MJ (2007) Medical treatment of cataract. Clin Experiment Ophthalmol 35:664–671
Fernandez MM, Afshari NA (2008) Nutrition and the prevention of cataracts. Curr Opin Ophthalmol 19:66–70
Mathew MC, Ervin AM, Tao J, Davis RM (2012) Antioxidant vitamin supplementation for preventing and slowing the progression of age-related cataract. Cochrane Database Syst Rev 6:CD004567
Agte V, Tarwadi K (2010) The importance of nutrition in the prevention of ocular disease with special reference to cataract. Ophthalmic Res 44:166–172
Casson RJ, Chidlow G, Wood JP, Crowston JG, Goldberg I (2012) Definition of glaucoma: clinical and experimental concepts. Clin Experiment Ophthalmol 40:341–349
Grant J, Tran V, Bhattacharya SK, Bianchi L (2013) Ionic currents of human trabecular meshwork cells from control and glaucoma subjects. J Membr Biol 246:167–175
Shoshani YZ, Harris A, Shoja MM, Rusia D, Siesky B, Arieli Y, Wirostko B (2012) Endothelin and its suspected role in the pathogenesis and possible treatment of glaucoma. Curr Eye Res 37:1–11
Anwar Z, Wellik SR, Galor A (2013) Glaucoma therapy and ocular surface disease: current literature and recommendations. Curr Opin Ophthalmol 24:136–143
Zanon-Moreno V, Ciancotti-Olivares L, Asencio J, Sanz P, Ortega-Azorin C, Pinazo-Duran MD, Corella D (2011) Association between a SLC23A2 gene variation, plasma vitamin C levels, and risk of glaucoma in a Mediterranean population. Mol Vis 17:2997–3004
Yuki K, Murat D, Kimura I, Ohtake Y, Tsubota K (2010) Reduced-serum vitamin C and increased uric acid levels in normal-tension glaucoma. Graefes Arch Clin Exp Ophthalmol 248:243–248
Zanon-Moreno V, Garcia-Medina JJ, Gallego-Pinazo R, Vinuesa-Silva I, Moreno-Nadal MA, Pinazo-Duran MD (2009) Antioxidant status modifications by topical administration of dorzolamide in primary open-angle glaucoma. Eur J Ophthalmol 19:565–571
Izzotti A, Sacca SC, Di Marco B, Penco S, Bassi AM (2008) Antioxidant activity of timolol on endothelial cells and its relevance for glaucoma course. Eye (Lond) 22:445–453
Wang SY, Singh K, Lin SC (2013) Glaucoma and vitamins A, C, and E supplement intake and serum levels in a population-based sample of the United States. Eye (Lond) 27:487–494
Ramdas WD, Wolfs RC, Kiefte-de Jong JC, Hofman A, de Jong PT, Vingerling JR, Jansonius NM (2012) Nutrient intake and risk of open-angle glaucoma: the Rotterdam Study. Eur J Epidemiol 27:385–393
Giaconi JA, Yu F, Stone KL, Pedula KL, Ensrud KE, Cauley JA, Hochberg MC, Coleman AL (2012) The association of consumption of fruits/vegetables with decreased risk of glaucoma among older African-American women in the study of osteoporotic fractures. Am J Ophthalmol 154:635–644
Kang JH, Pasquale LR, Willett W, Rosner B, Egan KM, Faberowski N, Hankinson SE (2003) Antioxidant intake and primary open-angle glaucoma: a prospective study. Am J Epidemiol 158:337–346
Chung HS, Harris A, Kristinsson JK, Ciulla TA, Kagemann C, Ritch R (1999) Ginkgo biloba extract increases ocular blood flow velocity. J Ocul Pharmacol Ther 15:233–240
Shim SH, Kim JM, Choi CY, Kim CY, Park KH (2012) Ginkgo biloba extract and bilberry anthocyanins improve visual function in patients with normal tension glaucoma. J Med Food 15:818–823
Park JW, Kwon HJ, Chung WS, Kim CY, Seong GJ (2011) Short-term effects of Ginkgo biloba extract on peripapillary retinal blood flow in normal tension glaucoma. Korean J Ophthalmol 25:323–328
Quaranta L, Bettelli S, Uva MG, Semeraro F, Turano R, Gandolfo E (2003) Effect of Ginkgo biloba extract on preexisting visual field damage in normal tension glaucoma. Ophthalmology 110:359–362
de Jong PT (2006) Age-related macular degeneration. N Engl J Med 355:1474–1485
The Age-Related Eye Disease Study 1(AREDS1) Research Group (2001) A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol 119:1417–1436
The Age-Related Eye Disease Study 2(AREDS2) Research Group (2013) Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration: the Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. JAMA 309:2005–2015
Evans JR, Lawrenson JG (2012) Antioxidant vitamin and mineral supplements for preventing age-related macular degeneration. Cochrane Database Syst Rev 6:CD000253
Evans JR, Lawrenson JG (2012) Antioxidant vitamin and mineral supplements for slowing the progression of age-related macular degeneration. Cochrane Database Syst Rev 11:CD000254
Chong EW, Wong TY, Kreis AJ, Simpson JA, Guymer RH (2007) Dietary antioxidants and primary prevention of age related macular degeneration: systematic review and meta-analysis. BMJ 335:755
Piccardi M, Marangoni D, Minnella AM, Savastano MC, Valentini P, Ambrosio L, Capoluongo E, Maccarone R, Bisti S, Falsini B (2012) A longitudinal follow-up study of saffron supplementation in early age-related macular degeneration: sustained benefits to central retinal function. Evid Based Complement Alternat Med 2012:429124
Madsen-Bouterse SA, Kowluru RA (2008) Oxidative stress and diabetic retinopathy: pathophysiological mechanisms and treatment perspectives. Rev Endocr Metab Disord 9:315–327
Williams M, Hogg RE, Chakravarthy U (2013) Antioxidants and diabetic retinopathy. Curr Diab Rep 13:481–487
Saugstad OD (2006) Oxygen and retinopathy of prematurity. J Perinatol 26(Suppl 1):S46–S50
Garcia-Medina JJ, Pinazo-Duran MD, Garcia-Medina M, Zanon-Moreno V, Pons-Vazquez S (2011) A 5-year follow-up of antioxidant supplementation in type 2 diabetic retinopathy. Eur J Ophthalmol 21:637–643
Millen AE, Klein R, Folsom AR, Stevens J, Palta M, Mares JA (2004) Relation between intake of vitamins C and E and risk of diabetic retinopathy in the Atherosclerosis Risk in Communities Study. Am J Clin Nutr 79:865–873
Raju TN, Langenberg P, Bhutani V, Quinn GE (1997) Vitamin E prophylaxis to reduce retinopathy of prematurity: a reappraisal of published trials. J Pediatr 131:844–850
Brion LP, Bell EF, Raghuveer TS (2003) Vitamin E supplementation for prevention of morbidity and mortality in preterm infants. Cochrane Database Syst Rev 4:CD003665
Johnson L, Schaffer D, Quinn G, Goldstein D, Mathis MJ, Otis C, Boggs TR Jr (1982) Vitamin E supplementation and the retinopathy of prematurity. Ann N Y Acad Sci 393:473–495
Dani C, Lori I, Favelli F, Frosini S, Messner H, Wanker P, De Marini S, Oretti C, Boldrini A, Massimiliano C, Bragetti P, Germini C (2012) Lutein and zeaxanthin supplementation in preterm infants to prevent retinopathy of prematurity: a randomized controlled study. J Matern Fetal Neonatal Med 25:523–527
Parad RB, Allred EN, Rosenfeld WN, Davis JM (2012) Reduction of retinopathy of prematurity in extremely low gestational age newborns treated with recombinant human Cu/Zn superoxide dismutase. Neonatology 102:139–144
Baumgartner WA (2000) Etiology, pathogenesis, and experimental treatment of retinitis pigmentosa. Med Hypotheses 54:814–824
Hartong DT, Berson EL, Dryja TP (2006) Retinitis pigmentosa. Lancet 368:1795–1809
Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Moser A, Brockhurst RJ, Hayes KC, Johnson CA, Anderson EJ, Gaudio AR, Willett WC, Schaefer EJ (2004) Further evaluation of docosahexaenoic acid in patients with retinitis pigmentosa receiving vitamin A treatment: subgroup analyses. Arch Ophthalmol 122:1306–1314
Pasantes-Morales H, Quiroz H, Quesada O (2002) Treatment with taurine, diltiazem, and vitamin E retards the progressive visual field reduction in retinitis pigmentosa: a 3-year follow-up study. Metab Brain Dis 17:183–197
Berson EL, Rosner B, Sandberg MA, Weigel-DiFranco C, Willett WC (2012) Omega-3 intake and visual acuity in patients with retinitis pigmentosa receiving vitamin A. Arch Ophthalmol 130:707–711
Jacobson SG, Cideciyan AV (2010) Treatment possibilities for retinitis pigmentosa. N Engl J Med 363:1669–1671
Berson EL, Rosner B, Sandberg MA, Hayes KC, Nicholson BW, Weigel-DiFranco C, Willett W (1993) A randomized trial of vitamin A and vitamin E supplementation for retinitis pigmentosa. Arch Ophthalmol 111:761–772
Amza A, Goldschmidt P, Einterz E, Huguet P, Olmiere C, Bensaid P, Bella-Assumpta L (2010) Elimination of active trachoma after two topical mass treatments with azithromycin 1.5 % eye drops. PLoS Negl Trop Dis 4:e895
Katabarwa MN, Eyamba A, Nwane P, Enyong P, Kamgno J, Kuete T, Yaya S, Aboutou R, Mukenge L, Kafando C, Siaka C, Mkpouwoueiko S, Ngangue D, Biholong BD, Andze GO (2013) Fifteen years of annual mass treatment of onchocerciasis with ivermectin have not interrupted transmission in the west region of cameroon. J Parasitol Res 2013:420928
van Rooij J, Schwartzenberg SG, Mulder PG, Baarsma SG (1999) Oral vitamins C and E as additional treatment in patients with acute anterior uveitis: a randomised double masked study in 145 patients. Br J Ophthalmol 83:1277–1282
Read RW (2006) Uveitis: advances in understanding of pathogenesis and treatment. Curr Rheumatol Rep 8:260–266
Nussenblatt RB, Kim J, Thompson DJ, Davis MD, Chew E, Ferris FL, Buggage R (2006) Vitamin E in the treatment of uveitis-associated macular edema. Am J Ophthalmol 141:193–194
Bartlett H, Eperjesi F (2003) Age-related macular degeneration and nutritional supplementation: a review of randomised controlled trials. Ophthalmic Physiol Opt 23:383–399
Rathore M (2009) Nutrient content of important fruit trees from arid zone of Rajasthan. J Hortic For 1:103–108
Weller P, Breithaupt DE (2003) Identification and quantification of zeaxanthin esters in plants using liquid chromatography-mass spectrometry. J Agric Food Chem 51:7044–7049
Acknowledgments
The authors thank Drs. Kalpna Varshney and M.D. Coughlin for pre-reviewing the manuscript. The following websites are thankfully acknowledged for the images showing the effects of different eye diseases on vision: http://www.nei.nih.gov/health/cataract/cataract_facts.asp, http://www.edinaeyeclinic.com/wp-content/uploads/glaucoma_simulation.jpg, http://oshawaoptometrist.pinkclassic.com/wp-content/uploads/2012/04/amd-vision-loss-5.jpg, http://upload.wikimedia.org/wikipedia/commons/thumb/9/9c/Eye_disease_simulation,_diabetic_retinopathy.jpg/220px-Eye_disease_simulation,_diabetic_retinopathy.jpg.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Grover, A.K., Samson, S.E. Antioxidants and vision health: facts and fiction. Mol Cell Biochem 388, 173–183 (2014). https://doi.org/10.1007/s11010-013-1908-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11010-013-1908-z