Abstract
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder which is caused by the interplay of genetic and environmental risk factors such as second-hand smoke (SHS). The association between postnatal exposure to SHS and ADHD risk in children was still inconclusive. We performed a systematic review and meta-analysis to explore the definite association. We searched for relevant studies from PubMed, Embase, Ovid, and Web of Science databases up to January 2020. We used random effect models to calculate pooled odds ratio (OR) with 95% confidence interval (CI). Subgroup analyses and sensitive analyses were also performed to solve the heterogeneity. According to our inclusion criteria, 9 studies including 6 cross-sectional studies, 2 cohort studies, and 1 case-control study were included in the final analysis. Postnatal exposure to SHS increased the risk of ADHD in children (OR: 1.60; 95% CI: 1.37–1.87). Children who exposed to SHS were found a slight risk for conduct problems (OR: 1.33, 95% CI: 1.00–1.77). Among the studies which used cotinine as a biomarker for SHS exposure, a lower pooled OR (OR = 1.16, 95%CI = 1.01, 1.33) was observed between cotinine and ADHD in children. Our meta-analysis results suggested that SHS exposure may be a risk factor for ADHD. We also found that SHS exposure may be associated with some adverse behavioral outcomes. More prospective studies should be conducted to confirm the relationship between SHS exposure and ADHD in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Attention deficit hyperactivity disorder (ADHD) is one of the most commonly diagnosed neurodevelopmental disorders which are characterized by developmentally inappropriate hyperactivity, inattention and impulsiveness, with an estimated worldwide prevalence of 5% in school-age children (Thapar et al. 2012; Wong et al. 2019). Although the etiology of ADHD is still not fully understood, there is consistent evidence that genetic factors contribute to the etiology of ADHD and that susceptibility genes interact with environmental risk factors in complex ways (Thapar et al. 2007). ADHD often co-occurs with other psychiatric diseases, such as conduct disorder and oppositional defiant disorder, which could be explained by both shared genetic and environmental influences (Tistarelli et al. 2020). In addition, some prospective studies have found that ADHD symptoms can persist into adulthood which may lead to poor quality of life and continuous financial loss (Klein et al. 2012). De Ridder and De Graeve (2006) pointed that ADHD in children had led to a significant increase in the use of healthcare and a negative impact on school performance and parental productivity. Given the social burden of ADHD and its impact on patients’ lives, attention should be paid to the prevention of ADHD.
Second-hand smoke (SHS) has long been a public concern. It refers to tobacco smoke inhaled by both the active first-hand smoker and the people around. Tobacco smoke contains at least 250 toxic chemicals, and some toxic metals ingredients have been shown to cause serious harm to humans (Pagani 2014). In addition, tobacco smoke and its byproducts are among the most common indoor pollutants globally, with about 40% of children, 35% of women, and 33% of men regularly exposed to SHS indoors (Oberg et al. 2011). Among them, infants and children may be more susceptible to SHS because of their immature respiratory, circulatory, and neurological systems (DiFranza et al. 2004). To date, most of studies have focused on the effects of maternal active smoking during pregnancy on children’s behavioral outcomes (Minatoya et al. 2019; Obel et al. 2016; Sourander et al. 2019). A meta-analysis found that prenatal exposure to maternal smoking during pregnancy was significantly associated with childhood ADHD after adjusting for parental psychiatric history and social socioeconomic status (Dong et al. 2018). Although most studies addressing tobacco smoke and behavioral outcome are more abundant with regard to prenatal exposure, there is rationality to think that postnatal SHS exposure evokes comparable adverse outcome. Herrmann et al. (2008) founded that children with either prenatal or postnatal tobacco exposure have more adverse behavioral outcomes such as oppositional defiant disorder, conduct disorder, delinquency, and ADHD. A longitudinal study which included over 2000 children age 4 to 11 years old also found that postnatal SHS exposure was associated with behavior problems in children, even after controlling for multiple potential confounders (Weitzman et al. 1992). Animal studies in adult rats indicated that exposure to SHS during adolescence causes long-term cognitive deficits (Counotte et al. 2009). However, some studies on the relationship between postnatal exposed to SHS and ADHD in children still have inconsistent results. Rückinger et al. (2010) argued that their studies did not show an association between exposure to SHS after birth and ADHD in children. Two recent studies using NHANES data also failed to find an increased risk of ADHD in children who exposed to SHS (Braun et al. 2006; Froehlich et al. 2009).
Therefore, in order to better clarify the relationship between SHS exposure and the risk of ADHD in children, we conducted a systematic review using meta-analysis. Given the adverse effects of ADHD, it makes sense to determine whether SHS exposure is related to ADHD in children. Moreover, the significance of the results will prompt people to quit smoking and create a healthy living environment for children.
Methods
Search strategy
We used the search terms related to postnatal, ADHD, and second-hand smoke to seek relevant studies in 4 major databases: PubMed, Embase, Ovid, and Web of Science. We retrieved studies started from database building to January 15, 2020. We not only searched the published literatures but also manually retrieved the references of obtained articles. The details of the search terms in each database were reported in Online Resource 1.
Selection criteria
We included population-based observational studies (cross-sectional studies, case-control studies, or cohort studies, including prospective and retrospective cohort studies) which reported the strength of association, expressed as an odds ratio (OR) or relative ratio (RR) with 95% confidence intervals (CIs), between SHS exposure and ADHD. All the included studies were published in English. The age limit for children is under 18 and there are no area restrictions. If multiple studies use the same population, we included newer studies.
Children with ADHD are identified through (1) the diagnosis of ADHD is by the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the International Classification of Diseases (ICD); (2) any medical records of ADHD; (3) using medication for ADHD, such as stimulants; (4) scores were above the symptom threshold using other valid assessment scales for ADHD; and (5) parent or guardian reported.
The measurements of SHS exposure are based on (1) using questionnaires to ask parents or guardians whether their children are exposed to SHS after birth; (2) information about children exposure to SHS in medical or other records.
Quality assessment
Study and outcome quality of case-control and cohort studies were assessed using the Newcastle–Ottawa Scale (NOS) (Stang 2010) which is a valid assessment tool. The NOS consists of 8 items with a maximum score of 9. If the score of the study is greater than 6, we define it as a high-quality study. The methodological quality of cross-sectional studies was assessed using an 11-item checklist which was recommended by the Agency for Healthcare Research and Quality (AHRQ) (Rostom and Cranney 2004). We classified the quality of the cross-sectional study into 3 categories: high quality (scored 8–11), moderate quality (scored 4–7), and low quality (scored 0–3) (Online Resource 1).
Data extraction
Two reviewers (Huang and Cai) independently extracted information on study characteristics based on the recommendations of the Meta-analysis of Observational Studies in Epidemiology (MOOSE) guidelines (Stroup et al. 2000) and the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISM) statement (Liberati et al. 2009). Characteristics of the selected studies included the first author, publication year, study design, study area, age of children in ADHD, gender, number of case groups and total population, measurement of SHS smoke exposure, different diagnosis methods of ADHD, various adjusted confounders, and risk estimates (OR or RR with 95% CI). We selected the adjusted OR of the model with the most adjustment factors, if there were multiple models in the study. If there was any dispute in the process of data extraction and analysis, the third reviewer (Wu) will discuss with the first two reviewers and re-evaluate the original study, finally reaching a consensus.
Publication Bias
The Begg’s test (Begg and Mazumdar 1994) and Egger’s test (Egger et al. 1997) (p < 0.05) were used to evaluate publication bias in selected studies. We also visualized publication bias using funnel plots. If Begg’s test or Egger’s test indicates that the study has publication bias, we will implement trim-and-fill method (Duval and Tweedie 2000) to adjust publication bias.
Statistical analysis
We calculated the pooled OR which represents the association between SHS exposure and the risk of ADHD in children. In this analysis, we directly considered the RR in the study results as the OR. We also used the Cochrane Q test and calculated the I2 statistic (Higgins et al. 2003) to indicate the degree of heterogeneity. If heterogeneity exists (I2 > 30%) among the selected studies, we will use the random effects model to calculate the pooled OR. Additionally, we used subgroup analysis to explore the heterogeneity sources. Sensitivity analysis was used to estimate the impact of a single study on pooled effect size by excluding one study at a time. All of the statistical analyses were performed using STATA 12.0 (Stata Corp., College Station, TX).
Results
Study selection process
The flow chart of study selection process is shown in Fig. 1. According to our search strategy, we searched from PubMed, Embase, Ovid, and Web of Science databases and found a total of 634 potentially related literatures. After studies which were duplicated being removed, 384 articles were left. Then, based on the title and abstract of the articles, we excluded 361 literatures, including 16 systematic reviews, 8 animal studies, and 6 meta-analyses. We further examined the full-text of remaining 23 literatures according to the previously proposed inclusion criteria, 8 studies were included. Among them, Braun’s study (Braun et al. 2006) which used the same population data as Max’s (Max et al. 2013) was excluded because it was published earlier and included fewer people. Moreover, we included 2 other articles through reference retrieval manually. Finally, we selected 9 studies (Bauer et al. 2015; Cho et al. 2018; Joo et al. 2017; Kabir et al. 2011; Max et al. 2013; Padrón et al. 2016; Rückinger et al. 2010; Tiesler et al. 2011; Twardella et al. 2010) for the systematic review and meta-analysis.
Study characteristics
The characteristics of the selected studies are shown in Table 1. We included 6 cross-sectional studies (Bauer et al. 2015; Cho et al. 2018; Kabir et al. 2011; Max et al. 2013; Padrón et al. 2016; Twardella et al. 2010), 2 cohort studies (Rückinger et al. 2010; Tiesler et al. 2011), and 1 case-control study (Joo et al. 2017) for our systematic review and meta-analysis. All of the studies were published between 2010 and 2018 including 6663 ADHD patients and 93,825 controls (Table S1). Among the included studies, 3 were from Germany (Rückinger et al. 2010; Tiesler et al. 2011; Twardella et al. 2010), 2 from Korea (Cho et al. 2018; Joo et al. 2017), 3 from the USA (Bauer et al. 2015; Kabir et al. 2011; Max et al. 2013), and 1 from Spain (Padrón et al. 2016). Most studies (Cho et al. 2018; Kabir et al. 2011; Max et al. 2013; Padrón et al. 2016; Rückinger et al. 2010) collected information about SHS exposure in children based on interviews from parents or guardians. A few studies (Bauer et al. 2015; Joo et al. 2017; Tiesler et al. 2011; Twardella et al. 2010) used questionnaires filled out by parents or guardians to obtain details of children’s SHS exposure. Both cohort studies (Rückinger et al. 2010; Tiesler et al. 2011) as well as two cross-sectional studies (Padrón et al. 2016; Twardella et al. 2010) assessed ADHD symptoms in children at age 10 using the Strengths and Difficulties Questionnaire (SDQ) (Goodman 1997). Some studies (Cho et al. 2018; Kabir et al. 2011; Max et al. 2013) collected information directly from parents or guardians on whether their children were diagnosed with ADHD. In addition, Max et al. (2013) also considers children who used stimulant drugs to be ADHD patients. Only two selected studies (Bauer et al. 2015; Joo et al. 2017) adopted the diagnostic criteria for ADHD from the Diagnostic and Statistical Manual of Mental Disorders, four Edition (DSM-IV) (Association 1994) and the International Classification of Diseases, 9th revision (ICD–9) (Preedy and Watson 2010). In addition, we evaluated the methodological quality of all selected studies. All of the included cohort and case-control studies (Joo et al. 2017; Rückinger et al. 2010; Tiesler et al. 2011) were high quality (score > 6). Two cross-sectional studies (Padrón et al. 2016; Twardella et al. 2010) were rated as high quality and the remaining (Bauer et al. 2015; Cho et al. 2018; Kabir et al. 2011; Max et al. 2013) were rated as medium quality (Table S1).
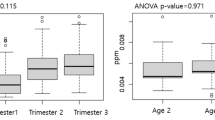
Postnatal SHS exposure and the risk of ADHD in children
We conducted a meta-analysis of all selected studies using random effect model. The pooled adjusted OR was 1.61 (95% CI: 1.37, 1.88). It is indicated that there is a positive association between postnatal SHS exposure and ADHD in children (Fig. 2). Heterogeneity of medium degree among studies was found (I2 = 42.5%, p = 0.084). Of the included studies, four studies used the SDQ scale to assess children behavior problems. We extracted the adjusted OR of two dimensions (conduct problems and peer problems) in the SDQ scale for meta-analysis. No association was found between postnatal SHS exposure and peer-relationship problems in children, the pooled OR was 1.14 (95% CI: 0.96, 1.37; I2 = 0%, p = 0.413) (Fig. S1). However, children who exposed to SHS were found a slight risk for conduct problems (OR = 1.33, 95% CI: 1.00, 1.77; I2 = 61.5%, p = 0.051) (Fig. 3). In the results of these studies, we did not combine the adjusted OR of other dimensions of the SDQ scale (emotional symptoms, prosocial behavior), because data were lacking in some studies.
Publication bias
The funnel plot did not show significant asymmetry (Fig. S2). The results of Begg’s test (Z = 1.77, p = 0.076 > 0.05) and Egger’s test (t = 1.96, p = 0.091 > 0.05) indicated that there was no significant publication bias in the selected studies. We did not use trim-and-fill method here because no significant publication bias was found.
Sensitivity analysis
We excluded one study at a time from the included studies and recalculated the pooled OR with 95% CI. The significant change was not found in the comparison between the new pooled OR and the total pooled OR (Fig. S3).
Subgroup analysis
We also conducted subgroup analysis based on different study design, regions, ADHD diagnosis methods, and adjustment factors. The studies which observed a lower pooled OR were conducted in Korea (OR = 1.55, 95% CI: 1.11, 2.17; I2 = 0.2%, p = 0.317) and the USA (OR = 1.49, 95% CI: 1.29, 1.72; I2 = 0%, p = 0.561). A higher pooled OR (OR = 1.81, 95% CI: 1.23, 2.65) was observed in the studies from Europe, but there was a high heterogeneity (I2 = 73.2%, p = 0.011) among these studies (Fig. S4). The pooled OR of cross-sectional studies was 1.71 (95% CI: 1.38, 2.12) and a moderated heterogeneity was found (I2 = 50.9%, p = 0.07). The pooled OR of cohort studies was 1.35 (95% CI: 1.03, 1.78; I2 = 50.9%, p = 0.07) (Fig. S5). A strong association was found in the studies using SDQ to assess the ADHD in children (OR = 1.81, 95% CI: 1.23, 2.65; I2 = 73.2%, p = 0.011). The studies which adjusted parental mental health have a higher pooled OR (OR = 1.82, 95% CI: 1.36, 2.45) than the studies not adjusted (OR = 1.53, 95% CI: 1.27, 1.84). A lower pooled OR was observed in the studies after adjusted maternal prenatal smoke (OR = 1.53, 95% CI: 1.30, 1.80). Since the number of included studies was less than 10, meta-regression was not performed. The results of subgroup analyses are summarized in Table 2.
Discussion
We used adjusted ORs for meta-analysis of included studies to uncover the association between SHS exposure and ADHD in children. SHS exposure after birth may be associated with ADHD in children. Children who exposed to SHS have a 1.6 times higher risk of developing ADHD than children not exposed. In addition, we also selected studies that used the SDQ scale to evaluate children’s behavioral problems under SHS exposure and combined some of the results of these studies. We found that children exposed to postnatal SHS had a greater risk of conduct problems, consistent with the findings of (Wang et al. 2019). However, we did not find a significant association between SHS and peer relationship problems in children.
Due to the moderate heterogeneity among the selected studies, we conducted a subgroup analysis based on some common characteristics to explore the sources of heterogeneity. When performing subgroup analyses based on different study designs, we found that there was still moderate heterogeneity in cross-sectional and cohort studies. A higher pooled OR was observed in Europe than in the USA and Korea. However, studies in Europe are highly heterogeneous due to the large differences in study populations. We also found that all of the selected Europe studies used the SDQ scale to assess ADHD symptoms. Therefore, we continued to perform another subgroup analysis based on the diagnosis method of ADHD. Except for the European study, the rest of the studies ascertained ADHD in children by parent-reported clinical diagnosis records. Heterogeneity was not found in these studies, whereas the lower pooled OR was observed. So, it is reasonable to believe that the heterogeneity of the included studies is due to the different methods and criteria of diagnosing ADHD.
Notably, many studies focused on maternal smoking during pregnancy and concluded that prenatal maternal smoking is a risk factor for ADHD in offspring (Langley et al. 2005; Schmitz et al. 2006). Some meta-analyses also reported the similar results (Dong et al. 2018; Huang et al. 2018). We combined the ORs of included studies that adjusted for maternal prenatal smoking and still found a strong association between postnatal SHS exposure and ADHD in children. Heath and Picciotto (2009) suggest that this may be caused by nicotine-mediated neurobiological disorders. Nicotine exposure in the environment may cause a variety of changes at the molecular and cellular levels of neurons. Fergusson et al. (1993) also found that after controlling for maternal prenatal smoking and other confounding factors, children exposed to SHS after birth showed a significant increase in ADHD symptoms compared with children not exposed to SHS.
The heritability of ADHD has been confirmed by many studies. Twin studies show that identical twins are more likely to develop ADHD than fraternal twins (Thapar et al. 1999). Moreover, ADHD also seems to share a genetic predisposition to other psychiatric problems (Cole et al. 2009; Lichtenstein et al. 2010; Thapar et al. 2001). However, the inherited factor is not the only explanation of ADHD. Environmental risk factors also play an important role (Thapar et al. 2012). We found a significant association between SHS exposure and ADHD in children from the studies that adjusted for parental psychiatric history. It further suggested that exposed to SHS may be a risk factor for ADHD in children. In addition, ADHD may be associated with indicators of social and economic disadvantage, including shorter parental education, lower family income, and younger parents (Cho et al. 2018). Animal studies also revealed a link between postnatal SHS exposure and ADHD. Slotkin et al. (2006) observed that changes in brain cell development in rhesus monkeys exposed to environmental SHS during perinatal or early life were similar to those seen in rodents exposed to nicotine before birth. However, studies on SHS exposure and ADHD in children are still controversial. A small number of studies found no association between SHS exposure and ADHD (Braun et al. 2006; Froehlich et al. 2009; Rückinger et al. 2010). Bandiera et al. (2011) pointed that SHS after birth was positively correlated with ADHD symptoms but could not be directly diagnosed as ADHD.
Most of the studies used parent-reported tobacco use to determine SHS exposure of children. It often causes the misclassification from recall bias and response bias. To reduce such bias, some studies used cotinine as an objective indicator of tobacco exposure to assess the association between SHS exposure and ADHD in children (Max et al. 2013). As the main plasma metabolite of nicotine, cotinine is currently considered to be the best biomarker for tobacco smoke exposure (Seccareccia et al. 2003). However, some studies shown that cotinine has a short half-life (less than 24 h). Therefore cotinine cannot be used as an appropriate biomarker for the long-term effects of SHS (Jarvis et al. 1988). In order to explore the relationship between cotinine level in children and ADHD, we selected related studies from the same database and conducted a meta-analysis (Braun et al. 2006; Joo et al. 2017; Kim et al. 2018; Max et al. 2013). We observed a lower pooled OR (OR = 1.16, 95%CI = 1.01, 1.33) which indicated that there was a low association between cotinine and ADHD. High heterogeneity was observed across selected studies (I2 = 89.6%, p < 0.01) (Fig. S6). This may be due to the lack of original studies and the difference in measurement accuracy among different periods (Max et al. 2013). Moreover, there are differences in the concentration of cotinine in blood, urine, and saliva (Torres et al. 2018). Inconsistencies in cotinine sources can lead to reduced comparability among various studies. Nevertheless, other studies (Gehring et al. 2006) suggested that the agreement between cotinine concentrations and questionnaire reports of smoking was good. Despite some misclassification, the questionnaire report remains a valid measure for estimating SHS exposure in preschool and school children.
Our study has several advantages. To our knowledge, this is the first meta-analysis assessing the relationship between postnatal SHS exposure and ADHD in children. Although there was moderate heterogeneity among our included studies, we found a positive association between postnatal exposure to SHS and ADHD in children in our subgroup analysis. It is indicated that our findings are highly reliable. Moreover, we also found that there may be a link between SHS exposure and some adverse behavioral problems in children. Tistarelli et al. (2020) reported that some behavioral problems often co-occur with ADHD. Therefore, the results of our study can provide a clue and basis for the mechanism research of ADHD in the future.
The limitations of our study should also be considered. First of all, most of the studies included were cross-sectional studies, with relatively low levels of evidence quality. Second, the language of included studies was limited to English and probably could not reflect all the results. Third, the diagnosis of ADHD is a comprehensive process that requires a detailed assessment of current and previous symptoms. It is insufficient to diagnose ADHD using a single assessment scale. Different assessment methods for ADHD are also prone to bias. Fourth, measurements of SHS exposure are largely based on subjective reports, which may lead to a misclassification of SHS exposure. Due to the large differences in the classification of SHS exposure in selected studies, we were unable to combine these studies to explore the dose-response relationship between SHS exposure and ADHD in children.
Conclusions
The results of our meta-analysis suggest that postnatal exposure to SHS may be associated with ADHD in children. Exposure to SHS can also lead to a variety of adverse behavioral outcomes in children. Therefore, parents should stop smoking to create a good growing environment for their children. Further prospective studies should fully adjust for potential confounding factors to determine whether there is a causal relationship between SHS and ADHD. In addition, the mechanisms by which passive smoking increases the risk of ADHD in children also need to be elucidated by more high-quality researches.
References
Association AP (1994) Diagnostic and statistical manual of mental disorders, fourth edition(DSM-IV) vol 42. Am Psych Ass
Bandiera FC, Richardson AK, Lee DJ, He J-P, Merikangas KR (2011) Secondhand smoke exposure and mental health among children and adolescents. Arch Pediatr Adolesc Med 165:332–338. https://doi.org/10.1001/archpediatrics.2011.30
Bauer NS, Anand V, Carroll AE, Downs SM (2015) Secondhand smoke exposure, parental depressive symptoms and preschool behavioral outcomes. J Pediatr Nurs 30:227–235. https://doi.org/10.1016/j.pedn.2014.06.004
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Braun JM, Kahn RS, Froehlich T, Auinger P, Lanphear BP (2006) Exposures to environmental toxicants and attention deficit hyperactivity disorder in U.S. children. Environ Health Perspect 114:1904–1909. https://doi.org/10.1289/ehp.9478
Cho YJ, Choi R, Park S, J-w K (2018) Parental smoking and depression, and attention-deficit hyperactivity disorder in children and adolescents: Korean national health and nutrition examination survey 2005-2014. Asia Pac Psychiatry 10:e12327. https://doi.org/10.1111/appy.12327
Cole J, Ball HA, Martin NC, Scourfield J, McGuffin P (2009) Genetic overlap between measures of hyperactivity/inattention and mood in children and adolescents. J Am Acad Child Adolesc Psychiatry 48:1094–1101. https://doi.org/10.1097/CHI.0b013e3181b7666e
Counotte DS, Spijker S, van de Burgwal LH, Hogenboom F, Schoffelmeer ANM, de Vries TJ, Smit AB, Pattij T (2009) Long-lasting cognitive deficits resulting from adolescent nicotine exposure in rats. Neuropsychopharmacology 34:299–306. https://doi.org/10.1038/npp.2008.96
De Ridder A, De Graeve D (2006) Healthcare use, social burden and costs of children with and without ADHD in Flanders, Belgium. Clin Drug Investig 26:75–90. https://doi.org/10.2165/00044011-200626020-00003
DiFranza JR, Aligne CA, Weitzman M (2004) Prenatal and postnatal environmental tobacco smoke exposure and children's health. Pediatrics 113:1007–1015. https://doi.org/10.1542/peds.113.4.S1.1007
Dong T et al (2018) Prenatal exposure to maternal smoking during pregnancy and attention-deficit/hyperactivity disorder in offspring: a meta-analysis. Reprod Toxicol 76:63–70. https://doi.org/10.1016/j.reprotox.2017.12.010
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot–based method of testing and adjusting for publication Bias in Meta-analysis. Biometrics 56:455–463. https://doi.org/10.1111/j.0006-341X.2000.00455.x
Egger M, Smith GD, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315:629–634. https://doi.org/10.1136/bmj.315.7109.629
Fergusson DM, Horwood LJ, Lynskey MT (1993) Maternal smoking before and after pregnancy: effects on behavioral outcomes in middle childhood. Pediatrics 92:815–840. https://doi.org/10.1203/00006450-199312000-00028
Froehlich TE, Lanphear BP, Auinger P, Hornung R, Epstein JN, Braun J, Kahn RS (2009) Association of tobacco and lead exposures with attention-deficit/hyperactivity disorder. Pediatrics 124:e1054–e1063. https://doi.org/10.1542/peds.2009-0738
Gehring U, Leaderer BP, Heinrich J, Oldenwening M, Giovannangelo MECA, Nordling E, Merkel G, Hoek G, Bellander T, Brunekreef B (2006) Comparison of parental reports of smoking and residential air nicotine concentrations in children. Occup Environ Med 63:766–772. https://doi.org/10.1136/oem.2006.027151
Goodman R (1997) The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 38:581–586. https://doi.org/10.1111/j.1469-7610.1997.tb01545.x
Heath CJ, Picciotto MR (2009) Nicotine-induced plasticity during development: modulation of the cholinergic system and long-term consequences for circuits involved in attention and sensory processing. Neuropharmacology 56(Suppl 1):254–262. https://doi.org/10.1016/j.neuropharm.2008.07.020
Herrmann M, King K, Weitzman M (2008) Prenatal tobacco smoke and postnatal secondhand smoke exposure and child neurodevelopment. Curr Opin Pediatr 20:184–190. https://doi.org/10.1097/MOP.0b013e3282f56165
Higgins JPT, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327:557–560. https://doi.org/10.1136/bmj.327.7414.557
Huang L, Wang Y, Zhang L, Zheng Z, Zhu T, Qu Y, Mu D (2018) Maternal smoking and attention-deficit/hyperactivity disorder in offspring: a meta-analysis. Pediatrics 141:e20172465. https://doi.org/10.1542/peds.2017-2465
Jarvis MJ, Russell MAH, Benowitz NL, Feyerabend C (1988) Elimination of cotinine from body fluids: implications for noninvasive measurement of tobacco smoke exposure. Am J Public Health 78:696–698. https://doi.org/10.2105/ajph.78.6.696
Joo H, Lim M-H, Ha M, Kwon H-J, Yoo SJ, Choi K-H, Paik K-C (2017) Secondhand smoke exposure and low blood lead levels in association with attention-deficit hyperactivity disorder and its symptom domain in children: a community-based case-control study. Nicotine Tob Res 19:19–101. https://doi.org/10.1093/ntr/ntw152
Kabir Z, Connolly GN, Alpert HR (2011) Secondhand smoke exposure and neurobehavioral disorders among children in the United States. Pediatrics 128:263–270. https://doi.org/10.1542/peds.2011-0023
Kim KM, Lim MH, Kwon H-J, Yoo S, Kim JW, Ha M, Paik K (2018) Associations between urinary cotinine and symptoms of attention deficit/hyperactivity disorder and autism spectrum disorder. Environ Res 166:481–486. https://doi.org/10.1016/j.envres.2018.06.018
Klein RG, Mannuzza S, Olazagasti MAR, Roizen E, Hutchison JA, Lashua EC, Castellanos FX (2012) Clinical and functional outcome of childhood attention-deficit/hyperactivity disorder 33 years later. Arch Gen Psychiatry 69:1295–1303. https://doi.org/10.1001/archgenpsychiatry.2012.271
Langley K, Rice F, van den Bree MBM, Thapar A (2005) Maternal smoking during pregnancy as an environmental risk factor for attention deficit hyperactivity disorder behaviour. A review. Minerva Pediatr 57:359–371
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ 339:b2700. https://doi.org/10.1136/bmj.b2700
Lichtenstein P, Carlström E, Råstam M, Gillberg C, Anckarsäter H (2010) The genetics of autism spectrum disorders and related neuropsychiatric disorders in childhood. Am J Psychiatry 167:1357–1363. https://doi.org/10.1176/appi.ajp.2010.10020223
Max W, Sung H-Y, Shi Y (2013) Attention deficit hyperactivity disorder among children exposed to secondhand smoke: a logistic regression analysis of secondary data. Int J Nurs Stud 50:797–806. https://doi.org/10.1016/j.ijnurstu.2012.10.002
Minatoya M, Araki A, Itoh S, Yamazaki K, Kobayashi S, Miyashita C, Sasaki S, Kishi R (2019) Prenatal tobacco exposure and ADHD symptoms at pre-school age: the Hokkaido Study on Environment and Children’s Health. Environ Health Prev Med 24:74. https://doi.org/10.1186/s12199-019-0834-4
Obel C, Zhu JL, Olsen J, Breining S, Li J, Grønborg TK, Gissler M, Rutter M (2016) The risk of attention deficit hyperactivity disorder in children exposed to maternal smoking during pregnancy - a re-examination using a sibling design. J Child Psychol Psychiatry 57:532–537. https://doi.org/10.1111/jcpp.12478
Oberg M, Jaakkola MS, Woodward A, Peruga A, Prüss-Ustün A (2011) Worldwide burden of disease from exposure to second-hand smoke: a retrospective analysis of data from 192 countries. Lancet 377:139–146. https://doi.org/10.1016/S0140-6736(10)61388-8
Padrón A, Galán I, García-Esquinas E, Fernández E, Ballbè M, Rodríguez-Artalejo F (2016) Exposure to secondhand smoke in the home and mental health in children: a population-based study. Tob Control 25:307–312. https://doi.org/10.1136/tobaccocontrol-2014-052077
Pagani LS (2014) Environmental tobacco smoke exposure and brain development: the case of attention deficit/hyperactivity disorder. Neurosci Biobehav Rev 44:195–205. https://doi.org/10.1016/j.neubiorev.2013.03.008
Preedy VR, Watson RR (2010) ICD-9. In: Handbook of disease burdens and quality of life measures. Springer, New York, pp 4232–4232
Rostom A DC, Cranney A (2004) Celiac disease: summary. In: Rockville (MD): Agency for Healthcare Research and Quality (US)
Rückinger S, Rzehak P, Chen CM, Sausenthaler S, Koletzko S, Bauer CP, Hoffmann U, Kramer U, Berdel D, von Berg A, Bayer O, Wichmann HE, von Kries R, Heinrich J, GINI-plus Study Group (2010) Prenatal and postnatal tobacco exposure and behavioral problems in 10-year-old children: results from the GINI-plus prospective birth cohort study. Environ Health Perspect 118:150–154. https://doi.org/10.1289/ehp.0901209
Schmitz M, Denardin D, Laufer Silva T, Pianca T, Hutz MH, Faraone S, Rohde LA (2006) Smoking during pregnancy and attention-deficit/hyperactivity disorder, predominantly inattentive type: a case-control study. J Am Acad Child Adolesc Psychiatry 45:1338–1345. https://doi.org/10.1097/S0890-8567(09)61916-X
Seccareccia F, Zuccaro P, Pacifici R, Meli P, Pannozzo F, Freeman KM, Santaquilani A, Giampaoli S (2003) Serum cotinine as a marker of environmental tobacco smoke exposure in epidemiological studies: the experience of the MATISS project. Eur J Epidemiol 18:487–492. https://doi.org/10.1023/A:1024672522802
Slotkin TA, Pinkerton KE, Seidler FJ (2006) Perinatal environmental tobacco smoke exposure in rhesus monkeys: critical periods and regional selectivity for effects on brain cell development and lipid peroxidation. Environ Health Perspect 114:34–39. https://doi.org/10.1289/ehp.8286
Sourander A, Sucksdorff M, Chudal R, Surcel HM, Hinkka-Yli-Salomäki S, Gyllenberg D, Cheslack-Postava K, Brown AS (2019) Prenatal cotinine levels and ADHD among offspring. Pediatrics 143:e20183144. https://doi.org/10.1542/peds.2018-3144
Stang A (2010) Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25:603–605. https://doi.org/10.1007/s10654-010-9491-z
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB (2000) Meta-analysis of observational studies in epidemiologyA proposal for reporting. JAMA 283:2008–2012. https://doi.org/10.1001/jama.283.15.2008
Thapar A, Holmes J, Poulton K, Harrington R (1999) Genetic basis of attention deficit and hyperactivity. Br J Psychiatry 174:105–111. https://doi.org/10.1192/bjp.174.2.105
Thapar A, Harrington R, McGuffin P (2001) Examining the comorbidity of ADHD-related behaviours and conduct problems using a twin study design. Br J Psychiatry 179:224–229. https://doi.org/10.1192/bjp.179.3.224
Thapar A, Langley K, Asherson P, Gill M (2007) Gene-environment interplay in attention-deficit hyperactivity disorder and the importance of a developmental perspective. Br J Psychiatry 190:1–3. https://doi.org/10.1192/bjp.bp.106.027003
Thapar A, Cooper M, Jefferies R, Stergiakouli E (2012) What causes attention deficit hyperactivity disorder? Arch Dis Child 97:260–265. https://doi.org/10.1136/archdischild-2011-300482
Tiesler CMT, Chen CM, Sausenthaler S, Herbarth O, Lehmann I, Schaaf B, Krämer U, von Berg A, von Kries R, Wichmann HE, Heinrich J, LISA Study Group (2011) Passive smoking and behavioural problems in children: results from the LISAplus prospective birth cohort study. Environ Res 111:1173–1179. https://doi.org/10.1016/j.envres.2011.06.011
Tistarelli N, Fagnani C, Troianiello M, Stazi MA, Adriani W (2020) The nature and nurture of ADHD and its comorbidities: a narrative review on twin studies. Neurosci Biobehav Rev 109:63–77. https://doi.org/10.1016/j.neubiorev.2019.12.017
Torres S, Merino C, Paton B, Correig X, Ramírez N (2018) Biomarkers of exposure to secondhand and thirdhand tobacco smoke: recent advances and future perspectives. Int J Environ Res Public Health 15. https://doi.org/10.3390/ijerph15122693
Twardella D, Bolte G, Fromme H, Wildner M, von Kries R (2010) Exposure to secondhand tobacco smoke and child behaviour - results from a cross-sectional study among preschool children in Bavaria. Acta Paediatr 99:106–111. https://doi.org/10.1111/j.1651-2227.2009.01522.x
Wang H, Li F, Zhang Y, Jiang F, Zhang J (2019) The association between exposure to secondhand smoke and psychological symptoms among Chinese children. BMC Public Health 19:923. https://doi.org/10.1186/s12889-019-7006-8
Weitzman M, Gortmaker S, Sobol A (1992) Maternal smoking and behavior problems of children. Pediatrics 90:342–349
Wong ICK, Banaschewski T, Buitelaar J, Cortese S, Döpfner M, Simonoff E, Coghill D (2019) Emerging challenges in pharmacotherapy research on attention-deficit hyperactivity disorder-outcome measures beyond symptom control and clinical trials. Lancet Psychiatry 6:528–537. https://doi.org/10.1016/S2215-0366(19)30096-3
Funding
This study was funded by Shantou Science and Technology Project (No. 190827075265313, 190823105264087, 2019ST005).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 711 kb).
Rights and permissions
About this article
Cite this article
Huang, A., Wu, K., Cai, Z. et al. Association between postnatal second-hand smoke exposure and ADHD in children: a systematic review and meta-analysis. Environ Sci Pollut Res 28, 1370–1380 (2021). https://doi.org/10.1007/s11356-020-11269-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-020-11269-y