Abstract
In utero exposure to tobacco smoke is associated with adverse neonatal outcomes; the association with later childhood mental health outcomes remains controversial. We used a strategy involving comparison of maternal and paternal smoking reports in a sample pooling data from six diverse European countries. Data were drawn from mother (N = 4,517) and teacher (N = 4,611) reported attention deficit and hyperactivity disorder (ADHD) symptoms in school children aged 6–11 in Turkey, Romania, Bulgaria, Lithuania, Germany, and the Netherlands, surveyed in 2010. Mothers report on self and husband’s smoking patterns during the pregnancy period. Logistic regression used with control covariates including demographics, maternal distress, live births, region, and post-pregnancy smoking. In unadjusted models, maternal prenatal smoking was associated with probable ADHD based on mother [Odds Ratio (OR) = 1.82, 95 % Confidence Interval (CI) 1.45–2.29], teacher (OR = 1.69, 95 % CI 1.33–2.14) and mother plus teacher (OR = 1.49, 95 % CI 1.03–2.17) report. Paternal prenatal smoking was similarly associated with probable ADHD in unadjusted models. When controlled for relevant confounders, maternal prenatal smoking remained a risk factor for offspring probable ADHD based on mother report (OR = 1.44, 95 % CI 1.06–1.96), whereas the effect of paternal prenatal smoking diminished (e.g., mother report: OR = 1.17, 95 % CI 0.92–1.49). Drawing on data from a diverse set of countries across Europe, we document that the association between maternal smoking and offspring ADHD is stronger than that of paternal smoking during the pregnancy period and offspring ADHD. To the extent that confounding is shared between parents, these results reflect a potential intrauterine influence of smoking on ADHD in children.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adverse maternal and fetal health outcomes associated with smoking in pregnancy are well-established [12, 19, 38, 46, 54]. While smoking in pregnancy is decreasing in many countries, these reductions are not uniform. Smoking in pregnancy remains high in European countries, especially in Eastern Europe [30]. As such, continuing focus on understanding the consequences of exposure to tobacco smoke in utero remains critical to allocate resources, inform prevention efforts, and allocate health care resources to manage potential short and long-term consequences of in utero tobacco exposure.
Most, though not all studies, suggest that exposure to tobacco smoke in utero is associated with offspring hyperactivity symptoms, hyperkinetic disorder, or attention deficit hyperactivity disorder (ADHD) in childhood (reviews include [32, 36] and more recent studies with positive associations include [6, 7, 21, 34, 44, 45]). Among children with clinically diagnosed ADHD, those exposed to prenatal smoking had more severe behavior and attention problems as well as lower cognitive function [49]. Animal studies have found that chronic nicotine exposure during pregnancy produced offspring that were more likely to exhibit spontaneous motor activity and rearing behavior, suggesting a neurobiological mechanism involving alteration of the developing brain [13, 26]. Further, research has demonstrated that this effect is mediated by increases in nicotinic receptors in the developing brain that regulate motor function and anxiety responses [15, 53]. Other hypothesized potential mechanisms underlying an association between prenatal tobacco exposure and offspring ADHD include maternal medical and obstetrical conditions associated with ADHD, and environmental factors, e.g. lead and alcohol exposure [32].
The potential for a causal relation between maternal smoking and offspring ADHD, however, has been called into question [2, 5, 43, 51]. Three different sources of evidence suggest substantial genetic and/or shared familial confounding. First, there are substantially reduced estimates for the association between prenatal smoking exposure and ADHD among siblings discordant for pregnancy exposure to tobacco smoke [9, 35, 40]. Sibling designs are valuable resources for controlling confounding by environmental factors that are shared between siblings [48], though recent evidence suggests that findings from sibling studies should be interpreted with caution as they may underestimate associations [20, 28]. Second, in a small study of children born via assisted reproductive technology, Thapar et al. [50] reported an association between prenatal smoking exposure and hyperactivity among pairs genetically related, but no association among pairs not genetically related. Finally, a recent study that controlled for maternal ADHD suggest that it explains a substantial proportion of the association between maternal smoking and offspring hyperactivity [2], though other studies with measures of maternal hyperactivity symptoms document a robust effect [14]. These studies suggest the possibility of substantial confounding in population-based studies that report associations between maternal smoking and offspring hyperactivity.
To shed further light on the causal relations underlying this association, some recent studies have compared the strength of the association between maternal and paternal prenatal exposures to offspring outcomes [10, 11]. With respect to prenatal smoking, this strategy uses paternal smoking during the pregnancy as a marker of shared familial confounding, as paternal smoking would have little in utero effect on the offspring (while secondhand smoke exposure could have an impact on fetal health, the effect would be weaker than direct exposure through maternal smoking). To the extent that maternal smoking is more strongly related to offspring ADHD than paternal smoking, a causal relationship for an in utero effect of smoking on hyperactivity is supported. Thus far, however, maternal/paternal comparisons have been inconsistent for many outcomes, including hyperactivity [27, 31, 39].
An important limitation of these studies is that they all utilize either mother’s report of offspring ADHD symptoms only [27], or a combined report of mother and teacher [31]. The home and school environments often capture different aspects of ADHD symptoms, and agreement between parents and teachers in offspring behavior is often low to moderate [4, 33, 58]. Teachers are presumably blind to whether the mother smoked during pregnancy or not, and may provide an informative assessment with regard to the child’s ADHD symptoms. Thus, examining the association specifically using teacher reports of ADHD symptoms is an overlooked area of the maternal/paternal comparison research. Further, data pertaining to this issue have primarily been collected in populations in which the prevalence of prenatal smoking is relatively low; examining the association in a diverse array of populations in which prenatal smoking is more common and less socially sanctioned provides an opportunity to examine the association between prenatal smoking and offspring ADHD in populations for which the structure of potential confounding factors such as socio-economic status are less associated with the exposure of interest [10].
The present study uses data from a large sample of European primary school children from six different countries across Europe. We aimed to examine the relation between prenatal tobacco exposure and probable ADHD by comparing the strength of associations between maternal and paternal smoking during pregnancy and offspring probable ADHD at age from 6 to 11 years. We examine this association across both teacher and mother report of offspring probable ADHD.
Method
Sample
The SCHME was a cross-sectional survey conducted in 2010 of schoolchildren aged from 6 to 11 years and one of their parents, most often the mother (86.5 %). Data for the present study were drawn from six countries in which parental smoking during pregnancy was assessed (Germany, Netherlands, Lithuania, Romania, Bulgaria, and Turkey). Primary schools were randomly selected in each participating country. As shown in Online Table 1, approximately, 45–50 schools were approached per country (a greater number of schools were approached in Germany and the Netherlands). Participation rates at the school level varied between 6.5 % (Netherlands) and 95.6 % (Romania). Within participating schools, classes were randomly selected in each school, and 6 children were randomly selected in each class. Approximately, 48 children were then randomly selected in each school, except in the Netherlands, where a lesser number of schools participated and therefore, entire classes were included, about 120 children per class. Parents received an informational letter and a consent form to be returned to the school. If the parents did not mail to the school a consent form stating their refusal to participate, the child was included. Children absent on the day of the survey were excluded. There were no other exclusion criteria. Among participating schools, between 50.5 % (Turkey) and 90.5 % (Netherlands) selected children participated, and between 45.5 % (Netherlands) and 90.9 % (Lithuania) of the child informants (parents and teachers). To reduce heterogeneity, we restricted these analyses to children for whom there was a mother’s report on symptoms (90 % of respondents). The total sample size was 4,611 for teacher reported outcomes and 4,517 for mother reported outcomes. By country: Germany (N = 434), Netherlands (N = 661), Lithuania (N = 1,032), Romania (N = 1,006), Bulgaria (N = 985) and Turkey (N = 491). Additional information about sampling methods was included in the final SCMHE report [41].
Measures
Data were collected from three informants: child, teacher and mother. Mother self-reports included a demographic and social questionnaire concerning household composition (including age, gender and familial link for each member), parental education (highest level completed), marital status, occupational level (professionally active versus inactive), as well as a questionnaire focusing on tobacco use. In the Netherlands, the same questions were completed electronically using a secured website, though paper questionnaires were made available upon request. The present study focuses on mother and teacher reports.
Cigarette smoking
The questionnaire on tobacco use included questions from a periodically administered tobacco use survey known as “Eurobarometer” [18] and from a national Canadian survey [8]. It included questions on the overall smoking history of the respondent and the other parent, such as frequency during pregnancy. Mothers reported on smoking patterns of the father of the child during the pregnancy. Mothers or fathers who were reported to be smoking every day or occasionally were considered current smokers.
Child psychopathology
Child psychopathology was examined using the validated versions of the parent-reported Strengths and Difficulties Questionnaire (SDQ) [23]. The parent and teacher versions of the SDQ include a brief questionnaire divided into five subscales: emotional problems, hyperactivity and inattention, conduct problems, peer relationship difficulties and prosocial behaviours [23]. Probable ADHD was defined using 5 questions rated from 0 to 2 in both the teacher and parent versions; scores were summed and subdivided into 0–5 = “unlikely”, 6 = “possible”, and 7–10 = “probable” cases of ADHD. Probable ADHD cases were defined by both a parent and a teacher score ≥7. Parent and teacher reports were also analysed separately. Using a subsample of more than 600 children recruited from primary care pediatricians, in-patients, and out-patients, parent and teacher reports of probable ADHD from the SDQ were validated in each country against the Development and Well-Being Assessment (DAWBA), a semi-structured instrument to generated DSM-based diagnoses of chid psychopathology [42]. Agreement (Kappa) was 0.48, ranging from 0.22 in Turkey to 0.58 in Romania. Sensitivity and specificity of the SDQ were both high; sensitivity ranged from 100 % in Germany, Netherlands, and Romania to 78.7 % in Lithuania, and specificity ranged from 77.1 % in Lithuania to 59.1 % in Germany.
Maternal psychopathology
Maternal psychological distress was assessed using the MH-5 scale of the Short-Form-36 [1], a five question scale ranging from 1 to 100 (mean = 73.8, SD = 16.6). Women scoring below 57 were classified as distressed as recommended by the authors [56, 57].
Birth weight
We also examined the relation of prenatal maternal smoking to parent-reported offspring birth weight to test the validity of our approach given the well-documented relation between maternal smoking and offspring birth weight. If comparison of maternal and paternal smoking on offspring health is a valid approach, then there should be a demonstrably larger effect of maternal smoking on offspring birth weight compared to the effect of paternal smoking.
Ethics statement
All participating countries had the support of their governments, including their ministers of education and health and received ethical approval from the corresponding authority
Statistical analysis
First, we examined factors associated with probable ADHD in the sample, by teacher report, mother report, and both teacher and mother report of probable ADHD (i.e., both the mother and the teacher reports were ≥7 on SDQ inattention/hyperactivity items) as three separate outcomes. Chi-square tests used for categorical outcomes and t-tests for continuous outcomes; alpha = 0.05. These factors include sociodemographic (child sex, age, mother’s education, mother’s age, and whether the mother was professionally active versus inactive), maternal psychological distress, number of live births, and maternal smoking behaviour at the time of the interview.
Second, we estimated the association between maternal and paternal smoking during the prenatal period with probable ADHD using the mother, teacher, and both mother and teacher reports of probable ADHD. Logistic regression models were used, and analyses were first conducted unadjusted, and then adjusted for child sex and age as well as mother’s age, educational achievement, maternal psychological distress, employment, marital status, number of live births, and Eastern versus Western European regions. Current smoking at the time of the interview was also controlled, as we were interested in the potential intrauterine effect of prenatal smoking exposure, thus smoking exposures after the prenatal period were not of interest.
Inclusion of covariates is critical in the assessment of prenatal smoking and offspring hyperactivity using these observational data, as families in which women who smoke in pregnancy have lower socio-economic resources and other risk factors for offspring ADHD al [22], thus we would expect a correlation between paternal smoking and offspring ADHD even in the absence of a causal association. We included confounders in multivariable analysis if they were associated with ADHD based on the mother, teacher, or combined mother and teacher report at p < 0.10 based on bivariable Chi-square analyses. Further, we controlled for geographic region in Europe (Eastern regions included East Germany, Bulgaria, Lithuania, Romania, and Turkey; Western regions included West Germany and the Netherlands) in three ways. In the main analysis, we controlled for a dichotomous variable of Eastern region versus Western region. Given regional variation in smoking during pregnancy and in the prevalence of probable ADHD, in sensitivity analysis we also controlled for high prenatal smoking (Lithuania, Netherlands, West Germany) versus low prenatal smoking countries (East Germany, Romania, Bulgaria, and Turkey), and high prevalence of hyperactivity (Lithuania, Turkey, Bulgaria) versus low prevalence (Romania, Netherlands, East and West Germany).
Because we were interested in the specific effect of maternal smoking on offspring ADHD, we examined maternal and paternal smoking patterns on offspring ADHD in two ways. First, mother and father smoking during pregnancy were simultaneously adjusted in controlled models due to the correlation between their smoking statuses. Second, we created dyads of partner smoking—both mother and father smoked, mother only smoked, father only smoked, and neither parent smoked. We then used this four-level variable as the independent variable with probable ADHD as the outcome.
Validation
As a validation of our approach, we examined the effect of maternal and paternal smoking during the prenatal period with offspring birth weight using linear regression. Birth weight was approximately normally distributed. Models were first estimated unadjusted and then adjusted for child sex and age as well as mother’s age, educational achievement, maternal psychological distress, current smoking at the time of the interview, employment, marital status, number of live births, and West versus Eastern European region. Mother and father smoking during pregnancy were simultaneously adjusted.
Treatment of missing data
23.9 % of the sample had missing data on mother’s smoking status during pregnancy, and 17 % of the sample was missing data on father’s smoking status during pregnancy. Missing data on maternal smoking was unrelated to child ADHD (OR = 0.86, 95 % CI 0.60, 1.25). Missing data on paternal smoking was also unrelated to child ADHD (OR = 1.15, 95 % CI 0.74, 1.77). Missing data were related to some covariates, however; specifically, maternal psychological distress, inactivity, number of live births, age, and education. Therefore, we included missing data as a categorical variable in all adjusted regression analyses to control for missing data differences across covariates. Results using this missing data approach did not yield different results than a complete case analysis; we present the analysis with the missing data as a covariate. There was also missing data on some covariates including mother’s employment (N = 339), current smoking status (N = 303), psychological distress (N = 215), marital status (N = 150), age (N = 34), and child’s age (N = 18) and sex (N = 1). Missing data on covariates was handled with list-wise deletion, thus the analytic sample size for the fully-adjusted models was 3,870.
Results
Prevalence of prenatal smoking and probable ADHD across country
Table 1 describes the prevalence of maternal prenatal smoking, paternal smoking during the prenatal period, and probable ADHD across country. Based on both mother and teacher report of probable ADHD, prevalence was 4.3 % in the overall sample. By reporter, 13.5 % of children were probable ADHD cases based on teacher report, and 13.1 % based on mother report (mother and teacher reports were moderately correlated: phi coefficient = 0.25, Chi-square for association between mother and teacher report = 256.2, df = 1, p < 0.001). Maternal prenatal smoking was highest in Turkey (32.9 %) and lowest in Lithuania (7.5 %). Paternal smoking during the prenatal period was highest in Turkey (63.1 %), and lowest in the Netherlands (23.6 %). Probable ADHD was highest in Lithuania, across mother (18.8 %), teacher (17.5 %), and combined mother and teacher report (7.7 %), and lowest in West Germany across mother (6.6 %), teacher (5.6 %), and combined mother and teacher report (0.9 %).
Association between study covariates and probable ADHD
All assessed study covariates were related to offspring probable ADHD, either through mother report, teacher report, both mother and teacher report of probable ADHD, or all three (Table 2). Males were more likely to exhibit probable ADHD regardless of the reporter, as were those whose mothers had low education, those with more siblings, those whose mothers were living apart from their partner, those whose mother’s had high psychological distress, and those in Eastern European regions. Child age (range was 6–10 years olds) was not significantly related to probable ADHD as designated by either mother or teacher. Younger mothers and professionally inactive mothers were more likely to report high levels of probable ADHD symptoms in children, but neither covariate was related to teacher report.
Association between study covariates, maternal, and paternal smoking during the pregnancy period
Both maternal smoking and paternal smoking in the pregnancy period was more common among those with less education, younger maternal age, those with more children, women living without their partner, women who were professionally inactive, women with psychological distress, those living in Eastern Europe, and women who were currently smoking at the time of the survey (Online Table 2). Age and sex of the child was unrelated to maternal and paternal smoking during the pregnancy period.
Prenatal smoking exposure and offspring probable ADHD
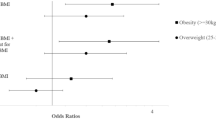
We show the results of regression models for the association between maternal and paternal smoking during the prenatal period with probable ADHD in Table 3. In unadjusted models, maternal prenatal smoking was associated with probable ADHD based on both mother (OR = 1.82, 95 % CI 1.45–2.29), teacher (OR = 1.69, 95 % CI 1.33–2.14) and both mother-teacher (OR = 1.49, 95 % CI 1.03, 2.17) report of probable ADHD. In unadjusted models, paternal smoking was associated with probable ADHD based on both mother (OR = 1.25, 95 % CI 1.25–1.86), teacher (OR = 1.32, 95 % CI 1.09–1.61) and both mother-teacher (OR = 1.48, 95 % CI 1.07, 2.03) report of probable ADHD. We next examined dyads of mother and father smoking; in the unadjusted model, associations were strongest with probable ADHD when both mother and father smoked based on both mother and teacher report of probable ADHD (OR = 2.06, 95 % CI 1.32–3.20).
When controlled for relevant confounders (see Table 3), maternal prenatal smoking remained associated for offspring probable ADHD based on mother report (OR = 1.44, 95 % CI 1.06–1.96), whereas the effect of paternal prenatal smoking diminished (OR for both mother report = 1.17, 95 % CI 0.92–1.49). We also examined each covariate as a single control in a model with maternal and paternal prenatal smoking. The variables with the strongest impact on the observed adjusted odds ratios, i.e. partner’s smoking status, maternal distress, and maternal current smoking, were controlled for in subsequent analyses. Each of these control variables reduced the observed odds ratios by approximately, 15–25 %; remaining covariates reduced the magnitude of the unadjusted estimates by less than 10 %. In adjusted models, the association between both mother and father smoking and offspring ADHD was in the direction of an adverse effect, and statistically significant for the effect of mother and father smoking on offspring ADHD based on mother report (OR = 1.49, 95 % CI 1.02–2.18). We directly tested whether the odds ratio for association between maternal smoking and offspring probable ADHD as reported by both teachers and mothers simultaneously was different than the odds ratio for the association between paternal smoking and ADHD using an additive interaction model; the Chi-square test-statistic and p value for the null hypothesis that there is no difference in these odds ratios was 3.0 and 0.08, respectively.
In Online Table 3, we show the adjusted results when the regional control variable was whether the country had high levels of prenatal smoking high prenatal smoking (Lithuania, Netherlands, West Germany) versus low prenatal smoking countries (East Germany, Romania, Bulgaria, and Turkey), and high prevalence of hyperactivity (Lithuania, Turkey, Bulgaria) versus low prevalence (Romania, Netherlands, East and West Germany). The only difference in the results was that the effect for both mother and father smoking on offspring hyperactivity as reported by both the mother and the teacher became statistically significant when the regional control variable was dichotomized based on the prevalence of hyperactivity (OR = 1.87, 95 % CI 1.01–3.46).
Prenatal smoking exposure and offspring birth weight
If comparisons between maternal smoking and paternal smoking during the prenatal period on offspring health are valid, then we should be able to observe a stronger association between maternal smoking and offspring birth weight compared with the effect of paternal smoking. Smoking in pregnancy is known to restrict fetal growth and has adverse effects on birth weight through an intrauterine pathway [54]. In adjusted models in Online Table 4, we show that the offspring of women who report smoking in pregnancy was about 139 grams lower than offspring of women who report no smoking, in adjusted models (95 % CI −202.2, −77.7). There was a negligible and non-significant effect of father smoking on offspring birth weight, as would be expected (β = −4.1, 95 % CI −48.6, 40.4).
Given the relation between maternal prenatal smoking and birth weight, we explored the extent to which offspring birth weight might influence associations between prenatal smoking and probable ADHD. In unadjusted and adjusted models, birth weight did not significantly predict probable ADHD (unadjusted: log odds = −0.0002, p = 0.16; adjusted: log odds = −0.0003, p = 0.14), and inclusion of birth weight as a covariate did not alter the magnitude of relations between maternal prenatal smoking and probable ADHD.
Discussion
These data are consistent with an association between maternal smoking during pregnancy and offspring probable ADHD at mean age 8. The data suggest that there is an association between maternal smoking and offspring probable ADHD that is stronger than that of paternal smoking during the pregnancy period and offspring probable ADHD; to the extent that confounding is shared between parents, these results are consistent with a potential intrauterine influence of smoking on inattention and hyperactivity symptoms. Further, we find relative consistency of the magnitude of this effect across reporters of offspring probable ADHD, including teacher, mother, and both mother and teacher reporting probable ADHD. These results are based on data from more than four thousand children across a diverse range of six countries across Eastern and Western Europe with widely varying prevalences of both ADHD and prenatal smoking, using a well-validated multiple informant approach to ADHD assessment [42].
These results add to a growing body of literature that has not yet achieved consensus. The effect of maternal smoking on offspring mental health has been assessed for a range of outcomes, including conduct disorder [22] and behavioral disinhibition [17]. While many studies document an association, the causal relations underlying these associations remain in contest. While we recently documented similar results of stronger associations between maternal smoking and offspring hyperactivity compared with father smoking and hyperactivity within a pregnancy cohort recruited in California [27], other comparisons of maternal smoking with paternal smoking have reported that the associations are similar in magnitude [31], suggesting substantial shared familial confounding [3, 36]. Further, comparisons of siblings discordant for maternal smoking during pregnancy have indicated that the association is substantially confounded [37, 40], although discordant sibling designs may, in some cases, underestimate associations [20, 28]. The results presented here suggest that, while estimates of the effect of maternal smoking on probable ADHD are substantially diminished when controlled for known risk factors, the association remains relatively strong, with odds ratios ranging from 1.5 to 1.9, while the association of paternal smoking with probable ADHD does not. We note that examination of maternal-paternal dyads of smoking indicated a similar relation between maternal smoking and offspring probable ADHD whether the father also smoked (OR = 1.70) or did not (OR = 1.92), although the results were not statistically significant. Further research using novel study designs to assess this complex relation will shed additional light on the impact of the in utero environment on offspring behavioral and mental health.
A central strength of the present data is the consistency of results across both teacher and parent informant, analyzed both separately and together. Teacher reporting on child outcomes is well-recognized as an integral component of assessing attention and hyperactivity problems [4, 33, 58], as symptoms of these disorders are often apparent in a classroom setting where focus and attention are necessary. While mother reporting of child behavior is a critical assessment, teacher reporting of ADHD is also important, as teachers are presumably blind to the prenatal smoking status of the mother. Previous literature has shown substantial differences in mother’s reporting of offspring ADHD compared with teachers, suggesting that each provide unique information on the child behavior. Further, Sherman et al. [47] found that twins were more concordant for ADHD when diagnosis was based on the mother report rather than the teacher report, suggesting that maternal reporting is potentially influenced by subjective comparisons of sibling similarities that do not influence teacher reports when children are in different classrooms. However, mothers may also report on signs and symptoms of behavior problems that occur uniquely in the home and do not manifest in the classroom, thus both reporters are necessary for a full assessment of the child. Interestingly, Fergusson et al. [17] found that, after adjusting for potential confounders, maternal smoking was associated with maternal but not teacher reports of hyperactivity at age 8, whereas maternal smoking was associated with teacher but not maternal reports of hyperactivity at age 10 and 12. Additionally, Langley et al. [31] found that maternal and paternal smoking during the pregnancy period were both similarly associated with hyperactivity symptoms (only mother report used), and that there was a slightly higher effect of maternal smoking on ADHD diagnoses (mother and/or teacher reports considered to be a positive case). We document associations between maternal reports of smoking during pregnancy and teacher reports of offspring probable ADHD.
The results of the present study should be evaluated in light of the limitations of cross-national survey data. Probable ADHD was based on teacher and parent report of symptoms rather than clinical diagnosis, and previous research indicates that parent and teacher reports may differ from clinical assessment [24]. However, the SDQ is a well-validated and widely used instrument for child psychopathology [23] and we used a combined report across both parents and teachers, suggesting that the probable diagnoses reported are unlikely to be fully attributable to reporting biases. Further, our own work has shown high concordance between mother-teacher reports of probable ADHD based on the SDQ and diagnoses of ADHD based on a semi-structured instrument [42]. Self-report of smoking during pregnancy is retrospective and may be subject to bias, especially women reporting on their husband’s smoking. This self-reported data may be differential by offspring probable ADHD status. Further, women’s misclassification of smoking in pregnancy may be related to misclassification in the husband; those women who misreport their smoking status may be more likely to misreport their husband’s smoking status. However, this misclassification would likely attenuate the results; in fact, our estimates for the effect of maternal smoking on birth weight are less than other large-scale studies [16, 38, 55], suggesting an attenuation of the effect potentially due to misclassification. Next, there was substantial missing data on smoking reports, including more missing data for the mother’s report of smoking than the mother’s report on the father. However, missing data was unrelated to offspring probable ADHD, limiting concerns about the introduction of bias. Further, we controlled for many factors related to missing data, including mother’s mental health status and demographic characteristics. Unmeasured confounders such as childhood nutritional environment, parent–child interactions, and home environment remain potential threats to validity of the present study. However, these factors would likely be shared between mothers and fathers. We find that maternal smoking is more strongly related to offspring hyperactivity than paternal smoking, suggesting that factors shared across parents including nutrition and the home environment are unlikely to explain the results presented here. Some potential confounders that are not shared between mothers and fathers are also important to consider in future studies. In particular, there is evidence that maternal ADHD is related to both smoking and offspring ADHD [2]; we did not have information on maternal ADHD. Finally, participation of eligible children and their parents varied substantially across country. It is possible that those children and mothers who participated in the survey were different than those who did not. We would hypothesize that mothers who participated in the survey may be less likely to be smokers, and may have husbands who were less likely to be smokers, than those who did not, and children may have been less likely to have behavioral problems compared with non-participators. Therefore, our prevalence estimates may be underestimated. However, we conducted a sensitivity analysis by subsetting the data into those countries with higher participation rates (Bulgaria, Romania, Lithuania, and Turkey) and those with lower participation rates (Germany and the Netherlands) and re-running all analyses. The magnitude of results did not change (see Online Tables 5 and 6), though the power to detect effects decreased. If mothers who both smoked in pregnancy, or had husbands who smoked during the pregnancy period, and had children with behavioral problems were less likely to participate than other parents, the associations presented in the analysis may be underestimated compared to what would be observed if all eligible participants had been included. Therefore, our estimates should be considered conservative.
Smoking during pregnancy remains an important modifiable risk factor for positive neonatal outcomes, and increasing evidence indicates that there may be consequences of in utero tobacco smoke exposure later in life [10, 25, 29, 52]. While evaluation of the effects of maternal smoking on offspring health present methodological challenges due to the myriad of potential confounding influences, the research remains a critical part of understanding early determinants of child, adolescent, and adult health. This study presents the most geographically diverse study conducted to date of maternal smoking and offspring probable ADHD. Given differences in risk factors for and distribution of maternal smoking in pregnancy across the six countries represented in the current study, the associations presented here add important additional evidence regarding the potential adverse influence of in utero smoking exposure on emotional and behavioral outcomes in childhood.
Abbreviations
- ADHD:
-
Attention deficit hyperactivity disorder
- SDQ:
-
Strengths and difficulties questionnaire
- CI:
-
Confidence interval
References
Aaronson NK, Acquadro C, Alonso J, Apolone G, Bucquet D, Bullinger M, Bungay K, Fukuhara S, Gandek B, Keller S et al (1992) International quality of life assessment (IQOLA) project. Qual Life Res 1:349–351
Agrawal A, Scherrer JF, Grant JD, Sartor CE, Pergadia ML, Duncan AE, Madden PA, Haber JR, Jacob T, Bucholz KK, Xian H (2010) The effects of maternal smoking during pregnancy on offspring outcomes. Prev Med 50:13–18
Ball SW, Gilman SE, Mick E, Fitzmaurice G, Ganz ML, Seidman LJ, Buka SL (2010) Revisiting the association between maternal smoking during pregnancy and ADHD. J Psychiatr Res 44:1058–1062
Biederman J, Faraone SV, Monuteaux MC, Grossbard JR (2004) How informative are parent reports of attention-deficit/hyperactivity disorder symptoms for assessing outcome in clinical trials of long-acting treatments? A pooled analysis of parents’ and teachers’ reports. Pediatrics 113:1667–1671
Biederman J, Petty CR, Bhide PG, Woodworth KY, Faraone S (2012) Does exposure to maternal smoking during pregnancy affect the clinical features of ADHD? Results from a controlled study. World J Biol Psychiatry 13:60–64
Brion MJ, Victora C, Matijasevich A, Horta B, Anselmi L, Steer C, Menezes AM, Lawlor DA, Davey Smith G (2010) Maternal smoking and child psychological problems: disentangling causal and noncausal effects. Pediatrics 126:e57–65
Button TM, Thapar A, McGuffin P (2005) Relationship between antisocial behaviour, attention-deficit hyperactivity disorder and maternal prenatal smoking. Br J Psychiatry 187:155–160
CCHS (2007) Canadian community health survey, cycle 4.1. Statistics Canada, Canada
D’Onofrio BM, Van Hulle CA, Waldman ID, Rodgers JL, Harden KP, Rathouz PJ, Lahey BB (2008) Smoking during pregnancy and offspring externalizing problems: an exploration of genetic and environmental confounds. Dev Psychopathol 20:139–164
Davey Smith G (2008) Assessing intrauterine influences on offspring health outcomes: can epidemiological studies yield robust findings? Basic Clin Pharmacol Toxicol 102:245–256
Smith GD (2012) Negative control exposures in epidemiologic studies. Epidemiology 23:350–351
DiFranza JR, Aligne CA, Weitzman M (2004) Prenatal and postnatal environmental tobacco smoke exposure and children’s health. Pediatrics 113:1007–1015
DiPietro JA, Hodgson DM, Costigan KA, Hilton SC, Johnson TR (1996) Fetal neurobehavioral development. Child Dev 67:2553–2567
Ellis LC, Berg-Nielsen TS, Lydersen S, Wichstrom L (2012) Smoking during pregnancy and psychiatric disorders in preschoolers. Eur Child Adolesc Psychiatry 21:635–644
Eriksson P, Ankarberg E, Fredriksson A (2000) Exposure to nicotine during a defined period in neonatal life induces permanent changes in brain nicotinic receptors and in behaviour of adult mice. Brain Res 853:41–48
Eskenazi B, Prehn AW, Christianson RE (1995) Passive and active maternal smoking as measured by serum cotinine: the effect on birthweight. Am J Public Health 85:395–398
Fergusson DM, Horwood LJ, Lynskey MT (1993) Maternal smoking before and after pregnancy: effects on behavioral outcomes in middle childhood. Pediatrics 92:815–822
European Communities (2008) Flash Eurobarometer, Survey on Tobacco. European Union, The Office for publications of the European Communities
Fogelman KR, Manor O (1988) Smoking in pregnancy and development into early adulthood. BMJ 297:1233–1236
Frisell T, Oberg S, Kuja-Halkola R, Sjolander A (2012) Sibling comparison designs: bias from non-shared confounders and measurement error. Epidemiology 23:713–720
Froehlich TE, Lanphear BP, Auinger P, Hornung R, Epstein JN, Braun J, Kahn RS (2009) Association of tobacco and lead exposures with attention-deficit/hyperactivity disorder. Pediatrics 124:e1054–1063
Gilman SE, Gardener H, Buka SL (2008) Maternal smoking during pregnancy and children’s cognitive and physical development: a causal risk factor? Am J Epidemiol 168:522–531
Goodman R (1997) The strengths and difficulties questionnaire: a research note. J Child Psychol Psychiatry 38:581–586
Gualtieri CT, Johnson LG (2005) ADHD: is objective diagnosis possible? Psychiatry (Edgmont) 2:44–53
Ino T (2010) Maternal smoking during pregnancy and offspring obesity: meta-analysis. Pediatr Int 52:94–99
Johns JM, Louis TM, Becker RF, Means LW (1982) Behavioral effects of prenatal exposure to nicotine in guinea pigs. Neurobehav Toxicol Teratol 4:365–369
Keyes KM, Davey Smith G, Susser E (2014) Associations of prenatal maternal smoking with offspring hyperactivity: causal or confunded? Psychol Med 44:857–867
Keyes KM, Davey Smith G, Susser E (2014) Commentary: smoking in pregnancy and offspring health: early insights into family-based and ‘negative control’ studies? Int J Epidemiol 43:1381–1388
Knopik VS (2009) Maternal smoking during pregnancy and child outcomes: real or spurious effect? Dev Neuropsychol 34:1–36
Kovess V, Pilowsky DJ, Boyd A, Pez O, Bitfoi A, Carta M, Eke C, Golitz D, Kuijpers R, Lesinskiene S, Mihova Z, Otten R, Susser E (2013) Parental smoking in the vicinity of children and tobacco control policies in the European region. PLoS One 8:e56783
Langley K, Heron J, Smith GD, Thapar A (2012) Maternal and paternal smoking during pregnancy and risk of ADHD symptoms in offspring: testing for intrauterine effects. Am J Epidemiol 176:261–268
Langley K, Rice F, van den Bree MB, Thapar A (2005) Maternal smoking during pregnancy as an environmental risk factor for attention deficit hyperactivity disorder behaviour. A review. Minerva Pediatr 57:359–371
Lavigne JV, Dulcan MK, LeBailly SA, Binns HJ (2012) Can parent reports serve as a proxy for teacher ratings in medication management of attention-deficit hyperactivity disorder? J Dev Behav Pediatr 33:336–342
Li J, Olsen J, Vestergaard M, Obel C (2010) Attention-deficit/hyperactivity disorder in the offspring following prenatal maternal bereavement: a nationwide follow-up study in Denmark. Eur Child Adolesc Psychiatry 19:747–753
Lindblad F, Hjern A (2010) ADHD after fetal exposure to maternal smoking. Nicotine Tob Res 12:408–415
Linnet KM, Dalsgaard S, Obel C, Wisborg K, Henriksen TB, Rodriguez A, Kotimaa A, Moilanen I, Thomsen PH, Olsen J, Jarvelin MR (2003) Maternal lifestyle factors in pregnancy risk of attention deficit hyperactivity disorder and associated behaviors: review of the current evidence. Am J Psychiatry 160:1028–1040
Linnet KM, Wisborg K, Obel C, Secher NJ, Thomsen PH, Agerbo E, Henriksen TB (2005) Smoking during pregnancy and the risk for hyperkinetic disorder in offspring. Pediatrics 116:462–467
Nigg JT, Breslau N (2007) Prenatal smoking exposure, low birth weight, and disruptive behavior disorders. J Am Acad Child Adolesc Psychiatry 46:362–369
Nomura Y, Marks DJ, Halperin JM (2010) Prenatal exposure to maternal and paternal smoking on attention deficit hyperactivity disorders symptoms and diagnosis in offspring. J Nerv Ment Dis 198:672–678
Obel C, Olsen J, Henriksen TB, Rodriguez A, Jarvelin MR, Moilanen I, Parner E, Linnet KM, Taanila A, Ebeling H, Heiervang E, Gissler M (2011) Is maternal smoking during pregnancy a risk factor for hyperkinetic disorder? Findings from a sibling design. Int J Epidemiol 40:338–345
Pez O, Boyd A, Fermanian C, Kovess V (2013) The school children mental health project. School Children Mental Health Europe. Available at: http://www.scmheproject.com/admin/includes/archivos//EUROPEAN_REPORT-_School_survey_FINAL.pdf
Pez O, Boyd A, Fermanian C, Kovess-Masfety V (2011) European report: the school children mental health evaluation phase 1: validation of the SCMHE instruments. http://www.scmheproject.com/resources.php
Rodriguez A, Bohlin G (2005) Are maternal smoking and stress during pregnancy related to ADHD symptoms in children? J Child Psychol Psychiatry 46:246–254
Roza SJ, Verhulst FC, Jaddoe VW, Steegers EA, Mackenbach JP, Hofman A, Tiemeier H (2009) Maternal smoking during pregnancy and child behaviour problems: the Generation R Study. Int J Epidemiol 38:680–689
Schmitz M, Denardin D, Laufer Silva T, Pianca T, Hutz MH, Faraone S, Rohde LA (2006) Smoking during pregnancy and attention-deficit/hyperactivity disorder, predominantly inattentive type: a case-control study. J Am Acad Child Adolesc Psychiatry 45:1338–1345
Sexton M, Hebel JR (1984) A clinical trial of change in maternal smoking and its effect on birth weight. JAMA 251:911–915
Sherman DK, McGue MK, Iacono WG (1997) Twin concordance for attention deficit hyperactivity disorder: a comparison of teachers’ and mothers reports. Am J Psychiatry 154:532–535
Susser E, Eide MG, Begg M (2010) Invited commentary: the use of sibship studies to detect familial confounding. Am J Epidemiol 172:537–539
Thakur GA, Sengupta SM, Grizenko N, Schmitz N, Page V, Joober R (2013) Maternal smoking during pregnancy and ADHD: a comprehensive clinical and neurocognitive characterization. Nicotine Tob Res 15:149–157
Thapar A, Rice F, Hay D, Boivin J, Langley K, van den Bree M, Rutter M, Harold G (2009) Prenatal smoking might not cause attention-deficit/hyperactivity disorder: evidence from a novel design. Biol Psychiatry 66:722–727
Thapar A, Rutter M (2009) Do prenatal risk factors cause psychiatric disorder? Be wary of causal claims. Br J Psychiatry 195:100–101
Tyrrell J, Huikari V, Christie JT, Cavadino A, Bakker R, Brion MJ, Geller F, Paternoster L, Myhre R, Potter C, Johnson PC, Ebrahim S, Feenstra B, Hartikainen AL, Hattersley AT, Hofman A, Kaakinen M, Lowe LP, Magnus P, McConnachie A, Melbye M, Ng JW, Nohr EA, Power C, Ring SM, Sebert SP, Sengpiel V, Taal HR, Watt GC, Sattar N, Relton CL, Jacobsson B, Frayling TM, Sorensen TI, Murray JC, Lawlor DA, Pennell CE, Jaddoe VW, Hypponen E, Lowe WL Jr, Jarvelin MR, Davey Smith G, Freathy RM (2012) Genetic variation in the 15q25 nicotinic acetylcholine receptor gene cluster (CHRNA5-CHRNA3-CHRNB4) interacts with maternal self-reported smoking status during pregnancy to influence birth weight. Hum Mol Genet 21:5344–5358
van de Kamp JL, Collins AC (1994) Prenatal nicotine alters nicotinic receptor development in the mouse brain. Pharmacol Biochem Behav 47:889–900
Vik T, Jacobsen G, Vatten L, Bakketeig LS (1996) Pre- and post-natal growth in children of women who smoked in pregnancy. Early Hum Dev 45:245–255
Villalbi JR, Salvador J, Cano-Serral G, Rodriguez-Sanz MC, Borrell C (2007) Maternal smoking, social class and outcomes of pregnancy. Paediatr Perinat Epidemiol 21:441–447
Ware JE, Kosinski M, Keller SD (1994) SF-36 Physical and mental component summary measures: a user’s manual. The Health Institute, New England Medical Center, Boston
Ware JE, Snow KK, Kosinski M, Gandek B (1993) SF-36 Health Survey: Manual and Interpretation Guide. The Health Institute, New England Medical Center, Boston
Wolraich ML, Lambert EW, Bickman L, Simmons T, Doffing MA, Worley KA (2004) Assessing the impact of parent and teacher agreement on diagnosing attention-deficit hyperactivity disorder. J Dev Behav Pediatr 25:41–47
Acknowledgments
This project had been financed by the European Union, grant number 2006336.
Conflict of interest
The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kovess, V., Keyes, K.M., Hamilton, A. et al. Maternal smoking and offspring inattention and hyperactivity: results from a cross-national European survey. Eur Child Adolesc Psychiatry 24, 919–929 (2015). https://doi.org/10.1007/s00787-014-0641-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00787-014-0641-9