Abstract
We evaluated the antibiogram profile of Escherichia coli (n = 300) isolated from selected rivers in Osun State, Nigeria. The identities of the E. coli isolates were confirmed by polymerase chain reaction (PCR) technique. Susceptibility of the isolates to 20 antibiotics conventionally used in clinical cases was assessed in vitro by the standardized agar disc-diffusion method. All the isolates were susceptible to imipenem, meropenem, amikacin and gatilofloxacin. The isolates were variously susceptible to the other antibiotics as follows: ciprofloxacin (96 %), kanamycin (95 %), neomycin (92 %), streptomycin (84 %), chloramphenicol (73 %), nalidixic acid (66 %), nitrofurantoin (64 %), gentamycin (63 %), doxycycline (58 %), cefepime (57 %), tetracycline (49 %) and cephalothin (42 %). The multiple antibiotic resistance indexing ranged from 0.50 to 0.80 for all the sampling locations and exceeded the threshold value of 0.2, suggesting the origin of the isolates to be of high antimicrobial usage. Our findings signify an increase in the incidence of antimicrobial resistance of E. coli towards conventionally used antibiotics necessitating proper surveillance programmes towards the monitoring of antimicrobial resistance determinants in water bodies.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Antimicrobial agents play an indispensable role in reducing morbidity and mortality associated with infectious diseases in animals and humans. However, selective pressure exerted by the exaggerated use of antimicrobials has been the main driving force in the emergence and spread of drug resistance traits among pathogenic and commensal bacteria (Aarestrup et al. 2008). The selection and spread of multi-drug resistance (MDR) organisms can often be traced to complex socioeconomic and behavioural antecedents, and it has contributed to the ever-increasing challenge of antibiotic resistance worldwide (Okeke et al. 1999; Mc Manus and Stockwell 2001; Silbergeld et al. 2008; Ghafur 2010). Surveillance data indicate that resistance in E. coli is consistently higher for antimicrobials that have been in use for a long time in human and veterinary medicine (USFDA and NARMS 2008). Furthermore, antimicrobials are poorly absorbed in the gut of animals and humans and end up being excreted unchanged in faeces and urine, eventually finding their way into the environment through the disposal of sewage, hospital wastewater and animal wastes (Schlusener and Beste 2006). Antibiotic-resistant bacteria have been noticed in various aquatic habitats, including treated and untreated wastewaters (Anderson and Sobrey 2006; Shehabi et al. 2006), rivers (Cernat et al. 2002) and marine water (Boehm et al. 2003).
Surface waters have emerged as reservoirs of faecal coliforms exhibiting multiple antimicrobial resistance owing to the discharge of municipal sewage and wastes from animals, industries and hospitals (Bruneau et al. 2004; Edge and Hill 2005; Qadri et al. 2005; Hamelin et al. 2006). This is because freshwater milieus are readily accessible for the discharge of wastewater, which may contain antimicrobial residues and are therefore, easily contaminated (Hirsch et al. 1999). Microbial indicators have been used worldwide as a tool to indicate the contamination of water by human wastes, and the occurrence of Escherichia coli in drinking water is an indication of faecal contamination and probable incidence of waterborne diseases that are injurious to health (Sivanadham et al. 2012; WHO 2010). Bacterial contamination of surface water, and particularly contamination with faecally derived bacteria, has long been a water quality concern owing to the potential for disease transmission.
The discovery of penicillin in the 1940s and several other antimicrobials in subsequent years led to great improvements in the management of infectious diseases (Norrby et al. 2005). Despite this great achievement, the indiscriminate use of antimicrobials has led to the inevitable development of resistance, as diseases and disease agents are now re-emerging in new forms resistant to antimicrobial therapy (Levy and Marshall 2004), rendering the current drugs used for treatment useless (Hancock 2005).
Antibiotic resistance indexing (ARI) is an excellent tool that enables one to determine the dissemination and prevalence of bacterial resistance in a given population at a specified location (Tandra and Sudha 2014). Isolates from water sources contaminated with antibiotics often give an ARI value >0.2, which is an indication of high-risk source of contamination. However, when antibiotics are seldom or never used, an ARI value <0.2 is observed (Krumperman 1983). A bacterium is termed multiple antibiotic resistant (MAR) if it is found to be resistant to three or more antimicrobials (Manjusha et al. 2005). Antimicrobial resistance increasingly compromises the treatment of many infections that were until recently, controllable, and so remain the most common diseases in Africa. The global challenge of antimicrobial resistance is particularly pressing in developing countries like Nigeria, where the infectious disease burden is high and cost constraints prevent the widespread application of newer and more expensive agents (Okeke et al. 2005).
Globally, about 191 million people rely on surface water as their main source of drinking water with sub-Saharan Africa facing the greatest challenge (WHO 2012). Almost 90 % of child deaths from diarrhoeal diseases are directly linked to contaminated water, inadequate sanitation and hygiene (UNICEF 2013). E. coli remain one of the major causes of morbidity and mortality in infants and young children especially when these diseases fail to be cured due to development of resistance to commonly prescribed antimicrobials (Okeke and Sosa 2003). The present study aimed at determining the high-risk contamination of water by indexing the frequency at which multi-drug resistant E. coli organisms occurred in selected surface waters from Osun State, South-western Nigeria.
Materials and methods
Description of study area and sampling sites
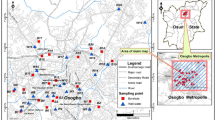
Water samples were collected from ten rivers at different locations in Osun State, South-western Nigeria. Table 1 shows the description of the sampling sites. The sites were selected after consultation with the State Ministries of Environment, Water Resources, Lands and Housing for proper mapping of the state rivers. The ten rivers were purposefully selected to represent the three senatorial districts of Osun State, in addition to being the most popular and major rivers in the state. The sampling locations were coded as follows: R1: Erinle-Ede; R2: Ido-Osun; R3: Osun-Osogbo; R4: Oba-Iwo; R5: Ejigbo; R6: Ilobu-Okinni; R7: Asejire-Ikire; R8: Shasha; R9 and Ila-Oke Ila, R10: Inisha-Okuku.
Sampling and isolation of presumptive E. coli
Water samples were aseptically collected monthly over a period of 1 year from September 2011 to August 2012. All samples were collected in 1.5-l sterile bottles and transported on ice to the laboratory where they were processed within 6 h of collection. The bottles were sterilized by autoclaving and during sampling, were triple rinsed with sample water before being filled. Analysis of water samples was performed according to standard methods (APHA 1998). One hundred milliliter (100 ml) aliquots of the water samples were filtered through a 90-mm diameter, 0.45-μm pore-sized membrane filters (Millipore, Ireland). The filters were incubated overnight at 44.5 °C on eosin methylene blue agar (Oxoid, UK). Characteristic metallic-sheen colonies were selected and purified by streaking on E. coli chromogenic agar (Conda Pronadisa, Spain) plates before storing on glycerol for further use.
PCR confirmation of E. coli isolates
All the presumptive E. coli isolates were subjected to polymerase chain reaction (PCR) technique for identification. DNA extraction was done using the boiling method (Torres et al. 2005; Maugeri et al. 2004). E. coli isolates were grown on nutrient agar plates at 37 °C for 24 h. The colonies were picked and suspended in 200-μl sterile distilled water, vortexed and boiled at 95 °C for 15 min followed by centrifugation at 15,000 rpm for 10 min. The supernatant was removed and stored at −80 °C for PCR confirmation. The PCR conditions, with some modifications, were in accordance with the protocols described elsewhere (Yokoigawa et al. 1999; Daly et al. 2002; Moyo et al. 2007).
Primers specific for a conserved region situated within the E. coli alanine racemase gene were selected [(F: 5´-CTGGAAGAGGCTAGCCTGGACGAG-3´) and (R: 5´-AAAATCGGCACCGGTGGAGCGATC-3´)]. The reaction mixture contained 25 μl of PCR Master Mix (Thermo Scientific, (EU) Lithuania), 0.5 μl each of oligonucleotide primer (Inqaba Biotech, SA), 10 μl of template DNA and 14 μl of nuclease free water to constitute a total reaction volume of 50 μl. PCR amplification was done using the following protocols: initial denaturation at 94 °C for 5 min followed by 35 cycles consisting of 30 s denaturation at 95 °C; primer annealing at 58 °C for 1 min; extension at 72 °C for 1 min and a final extension step for 5 min at 72 °C. The amplicons (5 μl aliquots) were resolved in 1.8 % (w/v) agarose gel (Merck, SA) stained with 5 μl ethidium bromide (Sigma-Aldrich, USA) and visualized under the Gel documentation system (Alliance 4.7, France). A 100-bp DNA ladder (Thermo Scientific) was included on the gel as a molecular size standard. Electrophoresis was carried out at 100 V for 1 h. E. coli ATCC 25922 was used as a reference strain (ATCC, USA).
Antibiotic susceptibility testing
Antimicrobial susceptibility tests were performed on the E. coli isolates by the disc-diffusion method, as previously described (Kirby-Bauer et al. 1966). To prepare the inocula for antibiotic susceptibility testing, 4–5 lone colonies of an 18-h-old culture were picked up with a sterile loop and transferred to a micro-centrifuge tube containing 2 ml of 0.85 % physiological sterile saline and gently vortexed to mix. The turbidity of the resulting solution was adjusted to 0.5 McFarland standard solution (using 0.5 ml of 0.048 M BaCl2 added to 99.5 ml of 0.18 M H2SO4 as a standard for comparison) which is approximately equal to 1 × 108 cells/ml (McFarland 1907). The turbidity of the bacterial suspension was adjusted by either adding inocula or sterile saline solution as required (Panda et al. 2012). One hundred microliter of the suspension was then spread plated onto Mueller Hinton agar plates and left to dry for 10 min prior to placing antibiotic discs on them.
A panel of 20 antibiotic discs (Mast Diagnostics, UK) impregnated with amikacin (30 μg), streptomycin (300 μg), kanamycin (30 μg), neomycin (10 μg), gentamycin (10 μg), cefepime (30 μg), cephalothin (30 μg), cefuroxime (30 μg), meropenem (10 μg), imipenem (10 μg), ciprofloxacin (5 μg), gatilofloxacin (5 μg), nalidixic acid (30 μg), sulphamethoxazole (25 μg); nitrofurantoin (200 μg), chloramphenicol (30 μg), tetracycline (30 μg), doxycycline (30 μg), amoxycillin (25 μg) and ampicillin (25 μg) were placed on the Mueller Hinton agar plates and incubated at 37 °C for 24 h. After incubation, the inhibition zone diameters were measured and classified as resistant (R), intermediate (I) and susceptible (S) to antibiotics according to the zone diameter interpretation standard recommended by the Clinical and Laboratory Standards Institute (CLSI 2010). Multiple antibiotic-resistant phenotypes (MARPs) for each sampling location were then generated for isolates that showed resistance to three or more antimicrobials following the method of Wose et al. (2010). The resistance pattern, number of antimicrobials to which the isolates were resistant, frequencies and percentages were obtained from the result of antimicrobial susceptibility testing.
The ARI for each sampling site was also determined using the formula described by (Tandra and Sudha 2014). It was mathematically expressed as:
A being the total number of resistant determinants recorded, N being the number of isolates and Y being the total number of antibiotics tested.
The multiple antibiotic resistance index (MARI) for each sampled location was equally derived using the mathematical expression of Blasco et al. (2008) which was given as:
where a represented the number of antibiotics to which the isolate was resistant and ‘b’ the total number of antibiotics against which an individual isolate was tested.
Statistical analysis
Statistical analysis was performed using Statistical Package for Social Sciences [(SPSS) IBM version 20 software]. One-way analysis of variance (ANOVA) was done to determine the variation in resistance among the isolates with respect to different locations. Correlations and test of significance were considered statistically significant when P values were >0.05.
Results
Table 2 shows mean annual presumptive and confirmed E. coli counts obtained at each of the sampling sites while Fig. 1 shows the gel electrophoresis picture of E. coli confirmation by PCR amplification of the uidA gene.
The lowest and highest counts were recorded in R7 and R9 with 83 and 41 CFU/ml, respectively. A total of 300 confirmed E. coli isolates, comprising 30 isolates from each study site, was pooled together and subjected to antibiogram analysis.
All the E. coli isolates were susceptible to all members of imipenem, meropenem, amikacin and gatilofloxacin antimicrobials. Similarly, high sensitivities were detected against ciprofloxacin (96 %), kanamycin (95 %), neomycin (92 %), streptomycin (84 %) and chloramphenicol (73 %). Varied susceptibilities were recorded for other antibiotics as follows: nalidixic acid (66 %), nitrofurantoin (64 %), gentamycin (63 %) and cefepime (57 %). Susceptibilities observed against other antibiotics tested were below average as shown in Fig. 2.
Susceptibility pattern of E. coli isolates against selected antimicrobials across different classes. AK Amikacin, S Streptomycin, K Kanamycin, NE Neomycin, G Gentamycin, CPM Cefepime, KF Cephalothin, CXM Cefuroxime, MEM Meropenem, IMI Imipenem, CIP Ciprofloxacin, GAT Gatilofloxacin, NA Nalidixic acid, SMX Sulphamethoxazole, NI Nitrofurantoin, C Chloramphenicol, DXT Doxycycline, T Tetracycline, AP Ampicillin, A Amoxycillin
All the isolates were resistant to sulphamethoxazole. High levels of resistance were equally observed against amoxycillin (59 %) and ampicillin (57 %) while the resistance to cefuroxime at 40 % was slightly below average. The lowest susceptibilities were observed against doxycycline (34 %) and tetracycline (33 %). Others varied as follows: cephalothin (29 %), gentamycin (24 %), nalidixic acid and nitrofurantoin (19 %), amoxycillin (19 %), ampicillin (18 %) and streptomycin (14 %) (Fig. 2).
Compilation of the MAR phenotypes indicated that about 75 % of E. coli isolates in this study exhibited resistance to three or more antimicrobial agents. The frequency of MARPs ranged from 24.8 to 2.2 % for MARPs 5 and 9, respectively. When this was expressed in terms of prevalence, 4, 5, 10, 16, 20, 20 and 25 % of the isolates showed multiple antibiotic resistance to nine, seven, eight, three, four, six and five antimicrobials, respectively (Table 3). The highest prevalence of MARPs across all the sampled sites was recorded in R7 at 70 % and lowest at R9 with 4.4 % (Fig. 3).
The predominant MARPs of the E. coli isolates, indicating the numbers of antimicrobials, resistance patterns and frequencies obtained in all the sampling sites, are presented in Table 3.
Table 4 presents the ARI and MARI values of all the sampling stations. In general, the MAR indices in all the river samples were found to be higher than the 0.2 threshold value, revealing imprudent use and greater exposure to antibiotics in humans, aquaculture, poultry and livestock which may pose high ecological risk to the waters. The MAR index actually ranged from 0.5 to 0.8. The modal MAR index for the tested isolates was 0.8 at R7 which is approximately four times the 0.2 limit while the lowest was at R9 with 0.5. This implies that the burden of antibiotics being discharged into site R7 is greater than others.
Generally, the one-way ANOVA showed that cefepime, cephalothin, cefuroxime, nalidixic acid, nitrofurantoin, chloramphenicol and tetracycline were not significantly different in their effect against the isolates from all locations (P > 0.05), whereas the resistance profile of the isolates against gentamycin, ciprofloxacin, sulphamethoxazole, ampicillin and amoxicillin were significantly different (P < 0.05). Amikacin, kanamycin, streptomycin, meropenem, imipenem and gatilofloxacin were statistically excluded from the analysis since all tested isolates showed total susceptibility to these antimicrobials.
A multiple comparisons analysis was done to determine the resistance patterns of isolates to antimicrobials with respect to isolate sources, i.e. R1–R10. We observed that the differences in resistance patterns of the isolates to ciprofloxacin, cefuroxime, gentamycin, nitrofurantoin, chloramphenicol, doxycycline, tetracycline, ampicillin and amoxicillin were not statistically significant in relation to sampling sites R1, R2, R4, R5, R7 and R8. Similarly, isolates from all locations (R1–R10) did not significantly differ in their resistance profile to sulphamethoxazole as they were all resistant to it. The homogeneous subsets analysis indicated over 60 % resistance to the antimicrobials by isolates from over 70 % of the locations; hence the widespread of antimicrobial resistance in the surface water samples.
Discussion
The presumptive E. coli isolates were confirmed by PCR technique by targeting the uidA gene. The uidA gene has been used in PCR assays for E. coli as a control amplicon due to the shared ability to cleave the colisure indicator 4-methylumbelliferyl-β-D-glucuronide (MUG) among different strains (Bej et al. 1991). Antibiogram results also show that E. coli isolates revealed resistance to more than one antimicrobial, similar to reports by other researchers (Reinthaler et al. 2003; Noble et al. 2003; Lin et al. 2004). The finding on the susceptibility pattern of the bacterial isolates to imipenem and meropenem (cephems), amikacin, kanamycin, neomycin and streptomycin (aminoglycosides) and gatilofloxacin and ciprofloxacin (fluoroquinolones) is consistent with that of other studies which reported high susceptibility to imipenem and low resistance to the quinolones and aminoglycosides, respectively (Osundiya et al. 2013; Olayinka et al. 2009). Results from this study indicate that gatilofloxacin and ciprofloxacin (fluoroquinolones) and amikacin, kanamycin and streptomycin (aminoglycosides) are the drugs of choice for E. coli infections, since none or few of the isolates were resistant to them. This shows the effectiveness of the fluoroquinolones and aminoglycosides, and is in agreement with the finding which suggested the use of these classes of antimicrobial agents against a range of pathogens (Scheld 2003).
The antibiotic sensitivity patterns of the E. coli isolates obtained in this research reveals that a larger percentage of the E. coli was resistant to one or more of the antimicrobial agents tested. The isolates’ resistance to ampicillin and amoxycillin, sulphamethoxazole, and chloramphenicol treatments has been described elsewhere (Manikandan et al. 2011). Although, sampling site R7 is a moderately populated place in the state, the availability of the river has formed the basis for industrial location (e.g. Bottling Company) and a large scale fishing business at sites R4, R7 and R10, as a means of livelihood for the inhabitants of the area. Fishing is common in most of the sampling sites, hence the high possibility of influence of domestic and industrial wastes into the environmental waters and the likelihood of antimicrobials being discharged into the waters is feasible as evidenced by the present findings. Both the presence of human settlements and small-scale industries are among the key factors that may directly or indirectly contribute to the increasing resistance of bacteria in the rivers, a finding that mirrors all the sampling sites except R3, possibly because it is a sacred site. The fact that some of these E. coli isolates showed high levels of resistance to some of the antimicrobials used is an indication that the antibiotics may have been abused or overly used for the treatment of bacterial infections hence, the possibility of building resistance against the antimicrobials (Ramesh et al. 2010). Resistance to antimicrobial agents is most common in areas with high usage of antibiotics such as hospitals (Sternbuerg 1999). Patterns of multi-drug resistance have also been observed in E. coli isolated from patients with urinary tract infections (Sevanan et al. 2011). The detection of multi-drug E. coli resistance in this study was neither shocking nor surprising as some of the rivers act as sinks for hospital wastes in upstream areas. The distribution and occurrence of E. coli having reduced susceptibility to multiple antimicrobial agents in surface water and other environmental media has equally been reported (Boerlin et al. 2005; Sayah et al. 2005).
The development of antimicrobial resistance by the bacteria to these drugs poses a major challenge in both human and animal medicine because these drugs are commonly used in animal and human therapeutic practices. Uncontrolled usage of antibiotics in treatment of animals and their incorporation in animal feeds has been suspected to account significantly to the increase in antimicrobial resistance in pathogenic bacterial isolates (WHO 2000; Galland et al. 2001). High E. coli resistance to tetracyclines and penicillins has been observed by many researchers (Al-Haj et al. 2007; Shitandi and Sternesjö 2001; O’Brien 1987). Animal rearing coupled with slaughtering of animals are a common practice around sampling locations R1, R2 and R8. Since these animals or poultry have often been treated with antibiotics during their breeding, the waste generated contains fairly high levels of antimicrobials. The high level of resistance to tetracyclines obtained in this study may be as a result of it being the most commonly available antimicrobial agent used as a growth promoter and routine chemoprophylaxis among livestock in Nigeria (Olatoye 2010). Penicillin and tetracycline are known to be extensively used in developing countries to treat respiratory infections, diarrhoea, mastitis and other infectious diseases in beef and dairy cattle (Hart and Ariuki 1998; Okeke et al. 1995).
It is bothersome bearing in mind that tetracycline is a first-line drug in Nigeria, and as in most developing countries, people with gastrointestinal infections readily procure it across the counter for self-prescription and medication (Chigor et al. 2010). Resistance was found to be relatively low against streptomycin. This probably may be because of less exposure to the antibiotic due to the discouraged use of the antibiotic and the fact that it is usually administered intravenously thereby restricting indiscriminate use (Cheesbrough 2000). Results of a similar study revealed that more than 90 % of E. coli isolates were multi-drug resistant to three or more commonly used antibiotics (Olowe et al. 2008). All the MDR isolates were resistant to sulphamethoxazole and most to ampicillin, amoxycillin, cephalothin, cefuroxime and cefepime. Findings from water samples of Southwest Nigeria also showed that most of the E. coli isolates were resistant to various antimicrobial agents ranging from two to seven kinds including cotrimoxazole, tetracycline and amoxicillin (Lateef et al. 2003). The study around Jimma, Ethiopia, showed that almost all E. coli isolates from environmental sources were found to be multi-drug resistant to the commonly used antimicrobials including amoxicillin, tetracycline and cotrimoxazole (Wolde-Tenssay 2002). Also, 96.7 % of E. coli isolated from drinking water samples from Hyderabad, India was found to be resistant to two to six antibiotics (Atif et al. 2010). Another similar report also indicated that bacterial isolates from household drinking water demonstrated multiple drug resistance to antibiotics (Obi et al. 2004).
Resistance patterns may demonstrate multiple resistances to many antimicrobial agents phenotypically and genotypically and could present therapeutic consequences. Multiple resistances capable of regional dissemination can emerge as a result of antimicrobial selection pressure in either livestock or humans. This increase in multidrug resistance is quite alarming if coupled with the fact that such isolates harbour plasmids on which these genes may be located, because they are highly transferable (Aarestrup 1995; Levin et al. 1997).
The increased concentration of multi-drug resistant bacteria in the aquatic environment creates selective pressures on natural bacterial strains (Alpay-Karoglu et al. 2007). Basically, the influence of the various anthropogenic and other related activities within the sampling sites might be a strong indication for a high-risk source contamination of water as evidenced by the widespread antimicrobial resistance in the environment since their MARI values were by far greater than the threshold value of 0.2. Based on the comparison of MAR indices for E. coli isolates from a variety of sources, a suggestion was made by (Krumperman 1983) to use a MAR index of 0.2 for differentiating between low- and high-risk contamination, although he acknowledged that this value was arbitrary. Occurrence of antibiotic-resistant bacteria in a given environment may be an indication that an area is contaminated with antimicrobials (Gunaseelan and Ruban 2011). For example, Al-Bahry et al. (2009) suggested that the main reasons causing marine environmental contamination were improper and unnecessary use of antimicrobial drugs by human and animals.
Two major intrinsic mechanisms were reported to confer bacterial resistance to multiple antimicrobial drug classes: mutations in outer membrane porins resulting in reduced permeability to antimicrobials and over expression of multidrug efflux pumps, which tend to pump out antibiotics before they have the opportunity of acting on their target. Multiple antibiotic-resistant bacterial strains may also arise due to dissimilar mechanisms accumulating sequentially in an organism (Navon-Venezia et al. 2005). The observation on high MAR indices indicates that isolates originated from high-risks source(s) of contamination where antibiotics are frequently used and high levels of antibiotics usage and resistance have been found to be associated with animal husbandry (Paul et al. 1997; Bohm et al. 2004).
Conclusion
Confirmation of the presence of E. coli in river water samples in Osun State, South-western Nigeria, indicates faecal contamination and the possible presence of other enteric pathogens. Multiple antibiotic-resistant phenotypes and indices evaluated suggest increased presence of antibiotic-resistant E. coli in the surface waters tested and the prevalence can lead to serious health risk for communities that depend on the waters for sundry purposes. Resistant bacterial strains will continue to emerge unless indiscriminate use of drugs is curtailed by public awareness programmes coupled with enforcement of legislation that limits the prescription and dispensing of antimicrobials to only qualified professionals. Our findings indicate a high incidence of antimicrobial resistance of E. coli towards the conventionally used antibiotics. There is, therefore, a need for good surveillance programmes to monitor antimicrobial resistance patterns in water bodies.
References
Aarestrup F, Wegener HC, Collignon P (2008) Resistance in bacteria of the food chain: epidemiology and control strategies. Expert Rev Anti Infect Ther 6:733–750
Aarestrup FM (1995) Occurrence of glycopeptides resistance among Enterococcus faecium isolates from conventional and ecological poultry farms. J Microbial Drug Resist 1:255–257
Al-Bahry S, Mahmoud I, Elshfie A, Al-Harthy A, Al-Ghafri S, Al-Amri I et al (2009) Bacterial flora and antibiotic resistance from eggs of green turtles Chelonia myans: an indication of polluted effluents. Mar Pollut Bull 58:720–725
Al-Haj N, Mariana NS, Raha AR, Ishak Z (2007) Prevalence of antibiotic resistance among Escherichia coli from different sources. Malaysia Res J Pharmacol 1(2):44–49
Alpay-Karoglu S, Ozgumus OB, Sevim E (2007) Investigation of antibiotic resistance profile and TEM-type β-lactamase gene carriage of ampicillin resistant Escherichia coli strains isolates from drinking water. Ann Microbiol 57:281–288
Anderson ME, Sobrey MD (2006) Detection and occurrence of antimicrobially resistant Escherichia coli in groundwater on or near swine farms in eastern North Carolina. Water Sci Technol 54:211–218
APHA (1998) Standard methods for the examination of water and wastewater, 19th ed, Washington DC
Atif AP, Bushra BP, Vikram M (2010) High prevalence of multi-drug resistant Escherichia coli in drinking water samples from Hyderabad. Gomal J Med Sci 8(1):23–26
Bej AK, DiCesare JL, Haff L, Atlas RM (1991) Detection of Escherichia coli and Shigella spp. in water by using the polymerase chain reaction and gene probes for uid. Appl Environ Microbiol 57:1013–1017
Blasco MD, Esteve C, Alcaide E (2008) Multiresistant waterborne pathogens isolated from water reservoirs and cooling systems. J Appl Microbiol 105:469–475
Boehm AB, Fuhrman JA, Mrse RD, Grant SB (2003) Tiered approach for identification of a human fecal pollution source at a recreational beach: case study at Avalon Bay, Catalina Island, California. Environ Sci Technol 37:673–680
Boerlin P, Travis R, Gyles C, Reid-Smith R, Janecko N, Lim H et al (2005) Antimicrobial resistance and virulence genes of Escherichia coli from swine in Ontario. Appl Environ Microbiol 71:6753–6761
Bohm R, Gozalan F, Philipp W (2004) Comparative study on antibiotic resistance in selected bacterial species isolated from wastewater originating from slaughterhouses and of municipal sources. In Proceedings of International Society for Animal Hygiene. Saint-Malo 277
Bruneau A, Rodrigu H, Ismael J, Dion R, Allard R (2004) Outbreak of E. coli O157:H7 associated with bathing at a public beach in the Montreal-Centre region. Can Commun Dis Rep 30:133–136
Cernat R, Lazar V, Balotescu C, Cotar A, Coipan E, Cojocaru C (2002) Distribution and diversity of conjugative plasmids among some multiple antibiotic-resistant Escherichia coli strains isolated from river waters. Bacteriol Virusol Parazitol Epidemiol 47:147–153
Cheesbrough M (2000) District laboratory practice in tropical countries, 2nd edn. Cambridge University Press, United Kingdom, pp 151–220
Chigor VN, Umoh JV, Smith IS, Igbinosa OE, Okoh IA (2010) Multidrug resistance and plasmid patterns of Escherichia coli O157 and other E. coli isolated from diarrhoeal stools and surface waters from some selected sources in Zaria, Nigeria. Int J Environ Res Public Health 7:3831–3841
Clinical and Laboratory Standards Institute (CLSI) (2010) M100-S20. Performance Standards for Antimicrobial Disk Susceptibility Tests, Informational Supplement, Wayne, PA
Daly P, Collier T, Doyle S (2002) PCR-ELISA detection of Escherichia coli in milk. Lett Appl Microbiol 34:222–226
Edge TA, Hill S (2005) Occurrence of antibiotic resistance in Escherichia coli from surface waters and fecal pollution sources near Hamilton, Ontario. Can J Microbiol 51:501–505
Galland J, Hyatt RD, Crupper SS, Acheson WD (2001) Prevalence, antibiotic susceptibility, and diversity of E. coli O157:H7 isolates from a longitudinal study of beef cattle feedlots. Appl Environ Microbiol 67:4
Ghafur AK (2010) An obituary-on the death of antibiotics. J Assoc Physicians 1:58
Gunaseelan C, Ruban P (2011) Antibiotic resistance of bacteria from Krishna Godavari Basin, Bay of Bengal, India. Environ Exp Biol 9:133–136
Hamelin K, Bruant G, El-Shaarawi A, Hill S, Edge TA, Bekal S, Fairbrother JM, Harel J et al (2006) A virulence and antimicrobial resistance DNA microarray detects a high frequency of virulence genes in Escherichia coli isolates from great lakes recreational waters. Appl Environ Microbiol 72:4200–4206
Hancock EW (2005) Mechanisms of action of newer antibiotics for Gram positive pathogens. Lancet Inf Dis 5(4):209–218
Hart A, Ariuki KS (1998) Antimicrobial resistance in developing countries. Br Med J 317:647–650
Hirsch R, Ternes T, Haberer K, Kratz KL (1999) Occurrence of antibiotics in the aquatic environment. Sci Total Environ 225(1–2):109–118
Kirby-Bauer WM, Sherris JC, Turck M (1966) Antibiotic susceptibility testing by single disc method. Am J Clin Pathol 45:4
Krumperman PH (1983) Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of fecal contamination of foods. Appl Environ Microbiol 46:165–170
Lateef AJ, Oloke K, Gueguimkana EB (2003) The prevalence of bacterial resistance in clinical, food, water and some environmental samples in Southwest Nigeria. J Environ Monit Assess 100:59–69
Levin B, Lipsitch M, Pettot V, Schrags S, Anita R, Simonsen L (1997) Popul Genet Antibiot Resist J Clin Infect Dis 24:9–16
Levy SB, Marshall B (2004) Antibacterial resistance worldwide: causes, challenges and responses. Nat Rev 10(12):122–129
Lin J, Biyela PT, Puckree T (2004) Antibiotic resistance profiles of environmental isolates from Mhlathuze River, KwaZulu- Natal (RSA). Water SA 30(11):23–28
Manikandan S, Ganesapandian S, Singh M, Kumaraguru AK (2011) Emerging of multidrug resistance human pathogens from urinary tract infections. Curr Res Bacteriol 4:9–15
Manjusha S, Sarita GB, Elyas KK, Chandrasekaran M (2005) Multiple antibiotic resistances of Vibrio isolates from coastal and brackish water areas. Am J Biochem Biotechnol 1(4):201–206
Maugeri TL, Carbone M, Fera MT, Irrera GP, Gugliandolo C (2004) Distribution of potentially pathogenic bacteria as free living and plankton associated in a marine coastal zone. J Appl Microbiol 97:354–361
Mc Manus PS, Stockwell VO (2001) Antibiotic use for plant disease management in the United States. Plant Health Prog. doi:10.1094/PHP-2001-0327-01-RV
McFarland J (1907) The nephelometer: an instrument for estimating the number of bacteria in suspensions used for calculating the opsonic index and for vaccines. Am J Med Assoc 49(14):1176–1178
Moyo SJ, Maselle SY, Matee MI, Langeland N, Mylvaganam H (2007) Identification of diarrhoeagenic Escherichia coli isolated from infants and children in Dares salaam, Tanzania. BMC Infect Dis 7:92
Navon-Venezia S, Ben-Am R, Carmeli Y (2005) Update on Pseudomonas aeruginosa and Acinetobacter baumannii infections in the healthcare setting. Curr Opin Infect Dis 18:306–313
Noble RT, Moore DF, Leecaster MK, McGee CD, Weisberg SB (2003) Comparison of total coliform, faecal coliform, and Enterococcus bacterial indicator response for ocean recreational quality testing. Water Res 37:1637–1643
Norrby RS, Nord CE, Finch R (2005) Lack of development of new antimicrobial drugs: a potential serious threat to public health. Lancet Inf Dis 5(2):115–119
O’Brien TF (1987) Resistance of bacteria to antibacterial agents: report of task force. Rev Infect Dis 9:244–260
Obi CL, Bessong PO, Momba MNB, Potgieter N, Samie A, Igumbor EO (2004) Profiles of antibiotic susceptibilities of bacterial isolates and physico-chemical quality of water supply in rural Venda communities. South Africa Water SA 30:515–519
Okeke IN, Lamikanra A, Edelman R (1999) Socioeconomic and behavioural factors leading to acquired bacterial resistance to antibiotics in developing countries. Emerg Infect Dis 5:18–27
Okeke IN, Laxminarayan R, Bhutta ZA, Duse AG, Jenkins P, O'Brien TF et al (2005) Antimicrobial resistance in developing countries. Part 1: recent trends and current status. Lancet Inf Dis 5(8):481–493
Okeke IN, Sosa A (2003) Antibiotic resistance in Africa—discerning the enemy and plotting a defence. Africa Health 25:10–15
Okeke N, Lamikana A, Edelman R (1995) Socioeconomic and behavioural factors leading to acquired bacterial resistance in developing countries. Emerg Infect Dis 5:18–27
Olatoye IO (2010) The incidence and antibiotics susceptibility of Escherichia coli O157:H7 from beef in Ibadan Municipal, Nigeria. Afr J Biotechnol 9(8):1196–1199
Olayinka AT, Onile BA, Olayinka BO (2009) Antibiotic susceptibility and plasmid pattern of Pseudomonas aeruginosa from the surgical unit of a university teaching hospital in north central Nigeria. Int J Med Med Sci 1(3):079–083
Olowe OA, Okanlawo BM, Olowe RA, Olayemi AB (2008) Antimicrobial resistant pattern of Escherichia coli from human clinical samples in Osogbo, south western Nigeria. Afr J Microbiol Res 1(2):8–11
Osundiya OO, Oladele RO, Oduyebo OO (2013) Multiple antibiotic resistance (MAR) indices of Pseudomonas and Klebsiella species isolates in Lagos University Teaching Hospital. Afr J Clin Exp Microbiol 14(3):164–168
Panda SK, Patra AK, Kar RN (2012) Monitoring of multiple drug-resistant pathogens in a selected stretch of Bay of Bengal. J Environ Monit Assess 184:193–200
Paul SL, Bezbarua RL, Roy MK, Ghosh AC (1997) Multiple antibiotic resistance index and its reversion in Pseudomonas aeruginosa. Lett Appl Microbiol 24:169–171
Qadri F, Svennerholm AM, Faruque ASG, Sack RB (2005) Enterotoxigenic Escherichia coli in developing countries: epidemiology, microbiology, clinical features, treatment and prevention. Clin Microbiol Rev 18:465–483
Ramesh S, Manivasagan P, Ashokkumar S, Rajaram G, Mayavu P (2010) Plasmid profiling and multiple antibiotic resistance of heterotrophic bacteria isolated from Muthupettai Mangrove Environment, Southeast Coast of India. Cur Res Bacteriol 3:227–237
Reinthaler FF, Posch J, Feierl G, Wust G, Haas D, Ruckenbauer G et al (2003) Antibiotic resistance of E. coli in sewage and sludge. Wat Res 37:1685–1690
Sayah RS, Kaneene JB, Johnson Y, Miller R (2005) Patterns of antimicrobial resistance observed in Escherichia coli isolates obtained from domestic- and wild-animal fecal samples, human septage, and surface water. Appl Environ Microbiol 71:1394–1404
Scheld MW (2003) Maintaining fluoroquinolone class efficiency: review of influencing factors. Emerg Infect Dis J 9(1):1–9
Schlusener MP, Beste K (2006) Persistence of antibiotics such as macrolides, tiamulin and salinomycin in soil. Environ Pollut 143:565–571
Sevanan M, Pongiya UD, Peedikayil NJ (2011) Antimicrobial susceptibility pattern of biofilm producing Escherichia coli of urinary tract infections. Curr Res Bacteriol 4:73–80
Shehabi AA, Odeh JF, Fayyad M (2006) Characterization of antimicrobial resistance and class 1 integrons found in Escherichia coli isolates from human stools and drinking water sources in Jordan. J Chemother 18:468–472
Shitandi A, Sternesjö A (2001) Detection of antimicrobial residues in Kenyan milk. J Food Saf 21:205–215
Silbergeld EK, Graham J, Price LB (2008) Industrial food animal production, antimicrobial resistance, and human health. Annu Rev Publ Health 29:151–169
Sivanadham V, Muthukumar K, James RA (2012) Antibiotic resistant pathogens versus human impacts: a study from three eco-regions of the Chennai coast, southern India. Mar Pollut Bull 64:790–800
Sternbuerg S (1999) Antimicrobial resistance in bacteria in pets and horses. Acta Vet Scand Suppl 92:37–50
Tandra M, Sudha G (2014) Prevalence of antibiotic-resistant bacteria in three different aquatic environments over three seasons. Environ Monit Assess 186:5089–5100
Torres AG, Zhou X, Kaper JB (2005) Adherence of diarrheagenic Escherichia coli strains to epithelial cells. Infect Imm 73:18–29
UNICEF (2013) http://www.unicef.org. Accessed 27th June, 2014
USFDA, NARMS (2008) Food and Drug Administration, National Antimicrobial Resistance Monitoring System (USFDA and NARMS) Enteric Bacteria (NARMS): 2008 executive report. Rockville (MD) http://www.fda.gov/AnimalVeterinary/SafetyHealth/ Antimicrobial Resistance /National Antimicrobial Resistance Monitoring System/default.htm
WHO (2000) Global principles for the containment of antimicrobial resistance in animals intended for food; report of WHO consultation with the participation of Food and Agriculture Organization of The United Nation and the Office International Des Epizooties, Department of Communicable Disease Surveillance and Response. Geneva Switzerland 5–9 June, 2000
WHO (2010) Global alert response (GAR): hepatitis A. http://www.who.int/csr/disease/hepatitis/whocdscsredc2007/en/index3.htmL Accessed: 05/06/2014
WHO (2012) Progress on sanitation and drinking-water: 2012 update. WHO Press, Geneva, Switzerland, pp 1–66
Wolde-Tenssay Z (2002) Multiple antimicrobial resistances in bacterial isolates from clinical and environmental sources of Jimma Hospital, Southwest Ethiopia. Ethiop J Sci 25(2):295–302
Wose KCN, Ateba N, Kawadza TD (2010) Antibiotic resistance profiles of Escherichia coli isolated from different water sources in the Mmabatho locality, North-West Province, South Africa. Res Lett 106(1–2):44–49
Yokoigawa K, Inoue K, Okubo Y, Kawai H (1999) Primers for amplifying an alanine racemase gene fragment to detect E. coli strains in foods. J Food Sci 64:571–575
Acknowledgments
The authors express their gratitude to the Water Research Commission of South Africa for the grant K5/2145 which enabled access to facilities to complete this study. Yinka Titilawo is grateful to the University of Fort Hare for provision of doctoral bursary.
Conflicts of interest
The authors declare no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible editor: Philippe Garrigues
Rights and permissions
About this article
Cite this article
Titilawo, Y., Sibanda, T., Obi, L. et al. Multiple antibiotic resistance indexing of Escherichia coli to identify high-risk sources of faecal contamination of water. Environ Sci Pollut Res 22, 10969–10980 (2015). https://doi.org/10.1007/s11356-014-3887-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-014-3887-3