Abstract
Purpose
Although bilevel positive airway pressure (Bilevel PAP) therapy is usually used for overlap syndrome (OS), there is still a portion of OS patients in whom Bilevel PAP therapy could not simultaneously eliminate residual apnea events and hypercapnia. The current study was expected to explore whether auto-trilevel positive airway pressure (auto-trilevel PAP) therapy with auto-adjusting end expiratory positive airway pressure (EEPAP) can serve as a better alternative for these patients.
Methods
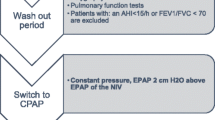
From January of 2014 to June of 2016, 32 hypercapnic OS patients with stable chronic obstructive pulmonary diseases (COPD) and moderate-to-severe obstructive sleep apnea syndrome (OSAS) were recruited. Three variable modes of positive airway pressure (PAP) from the ventilator (Prisma25ST, Weinmann Inc., Germany) were applicated for 8 h per night. We performed the design of each mode at each night with an interval of two nights with no PAP treatment as a washout period among different modes. In Bilevel-1 mode (Bilevel-1), the expiratory positive airway pressure (EPAP) delivered from Bilevel PAP was always set as the lowest PAP for abolishment of snoring. For each patient, the inspiratory positive airway pressure (IPAP) was constantly set the same as the minimal pressure for keeping end-tidal CO2 (ETCO2) ≤45 mmHg for all three modes. However, the EPAP issued by Bilevel PAP in Bilevel-2 mode (Bilevel-2) was kept 3 cmH2O higher than that in Bilevel-1. In auto-trilevel mode (auto-trilevel) with auto-trilevel PAP, the initial part of EPAP was fixed at the same PAP as that in Bilevel-1 while the EEPAP was automatically regulated to rise at a range of ≤4 cmH2O based on nasal airflow wave changes. Comparisons were made for parameters before and during or following treatment as well as among different PAP therapy modes. The following parameters were compared such as nocturnal apnea hypopnea index (AHI), minimal SpO2 (minSpO2), arousal index, sleep structure and efficiency, morning PaCO2, and daytime Epworth Sleepiness Scale (ESS).
Results
Compared with the parameters before PAP therapies, during each mode of PAP treatment, significant reduction was detected in nocturnal AHI, arousal index, morning PaCO2, and daytime ESS while significant elevation was revealed in nocturnal minSpO2 and sleep efficiency (all P < 0.01). Comparison among three PAP modes indicated that under the same IPAP, the auto-trilevel PAP mode could result in the lowest arousal index, daytime ESS, and the highest sleep efficiency. Compared with Bilevel-1, it was detected that (a) AHI was lower but minSpO2 was higher in both Bilevel-2 and auto-trilevel (all P < 0.05) and (b) morning PaCO2 showed no statistical difference from that in auto-trilevel but displayed higher in Bilevel-2 (P < 0.05). Compared with Bilevel-2, in auto-trilevel, both AHI and minSpO2 showed no obvious changes (all P > 0.05) except with a lower morning PaCO2 (P < 0.05).
Conclusion
Auto-trilevel PAP therapy was superior over conventional Bilevel PAP therapy for hypercapnic OS patients with their OSAS moderate to severe, since auto-trilevel PAP was more efficacious in synchronous elimination of residual obstructive apnea events and CO2 retention as well as in obtaining a better sleep quality and milder daytime drowsiness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The “overlap syndrome (OS)” means the coexistence of chronic obstructive pulmonary disease (COPD) and obstructive sleep apnea syndrome (OSAS) in one patient [1,2,3]. OS patients are more liable to have more severe hypoxiemia and hypercapnia during sleep, as well as an earlier occurrence of pulmonary artery hypertension and cor pulmonale [4,5,6]. Therefore, it is of important clinical significance to explore more effective novel therapies for OS patients.
Although there is coexisting OSAS in OS patients, continuous positive airway pressure (CPAP) treatment is used with caution because of CO2 retention which cannot be improved by CPAP. Instead, conventional bilevel positive airway pressure (Bilevel PAP) was often used for OS patients [7]. However, since the expiratory positive airway pressure (EPAP) levels needed for OS patients during sleep are different from that when they are awake, EPAP levels have to be elevated for OS patients during sleep because OSAS selectively occurs during sleep [8, 9]. The contradiction is that on the one hand, if the EPAP level is not high enough, obstructive sleep apnea (OSA) events cannot be well eliminated so that more residual OSA may still exist; on the other hand, hypercapnia may exist if EPAP is too higher to maintain a suitable gap between inspiratory positive airway pressure (IPAP) and EPAP because the narrowed gap between IPAP and EPAP cannot maintain enough ventilation support. Since too high IPAP can cause discomfort and decrease the compliance to positive airway pressure (PAP) treatment in OS patients, better PAP models are desired to be able to solve the contradiction and problems mentioned above.
Auto-trilevel PAP model shows its difference from ordinary bilevel model [10, 11], by setting up two different EPAP levels during expiratory period, i.e., with a relatively lower EPAP level at the early stage of expiratory period but an adjustable higher EPAP level at the end of expiratory period (Fig. 1). The lower early EPAP level is designed to be in favor of CO2 elimination at the beginning of expiration, and the relatively higher end EPAP (EEPAP) levels are aimed to eliminate residual OSA and hypopnea events caused by upper airway collapse since these events are more liable to occur at the end of expiration when there is a tendency of upper airway collapse if EPAP is lower [12,13,14,15]. Based on the characteristics of periodic changes of upper airway patency and collapsibility (Fig. 2), the anti-collapsibility from upper airway is better during the early stage of expiration because of higher intrinsic PAP at this period. However, towards the end of expiration, the anti-collapsibility from upper airway becomes weak possibly because of decreased intrinsic PAP and increased visceral attraction force at the later stage of expiratory period [13, 14]. Therefore, OSA and hypopnea events are more easy to be induced at the end stage of expiration [13, 14].
The three pressure levels of trilevel. IPAP inspiratory positive airway pressure, EPAP expiratory positive airway pressure, EEPAP end expiratory positive airway pressure, PDIFF pressure gap between IPAP and EPAP. Unlike conventional Bilevel PAP support model, EPAP in auto-trilevel is set up by two different parts, i.e., with a relatively lower EPAP level at the early stage of expiratory period but an adjustable higher EPAP level at the end of expiratory period
Besides the precondition that with a relatively lower EPAP at the early stage of expiration CO2 may be effectively expired, the design for auto-trilevel PAP model is aimed to eliminate residual OSA and hypopnea events by adjustably elevating EPAP towards the end of expiration. Theoretically, trilevel PAP therapy is more suitable for OS patients with hypercapnia. Our recruited OS patients with moderate-to-severe OSAS belong to such kind of patients. Through comparison with conventional Bilevel PAP treatment, the efficacy of trilevel PAP therapy for OS existed in this study.
Patients and methods
Patients
Between January 2014 and June of 2016, a total of 32 OS patients with moderate-to-severe OSAS and hypercapnia were recruited by the hospital’s outpatient or inpatient Department of Respirology. The 32 patients (26 males and 6 females) were aged 46–71 years with a mean age of 57.2 ± 8.7 years. Their body mass index (BMI) ranged between 25.7~30.9 (27.6 ± 2.1). All of them had a history of COPD and moderate-to-severe OSAS. During the process of recruitment, all those with a history or evidence of renal dysfunction, stroke, diabetes, and infectious disease were excluded from this investigation.
Polysomnography protocol
Overnight polysomnography (PSG) examination was carried out using the brand of Compumedics E-series Sleep System (Compumedics Sleep, Abbotsford, Australia). The measured PSG parameters included apnea hypopnea index (AHI), pulse oxygen saturation (SpO2), electro-cardiogram, electro-encephalogram, electro-myogram, electro-oculogram, and chest and abdominal respiratory movements. All recorded PSG tracings were manually scored by two technicians from our sleep lab strictly based on international standard criteria. Apnea was decided with an airflow cessation longer than 10 s, while hypopnea was recognized with an airflow amplitute reduction ≥50% accompanied by SpO2 reduction ≥3%. The AHI is defined by the sum of combined apnea and hypopnea events per hour during sleep. The minimal criteria for diagnosis of OSAS were AHI ≥5. Sleep apnea syndrome and its severity were judged by international diagnostic criteria (AHI = 5.0~14.9 as mild, 15.0~29.9 as moderate, and ≥30 as severe sleep apnea syndrome) [15]. Apnea event was defined as obstructive if chest and abdominal respiratory movement was observed during apnea. If a patient’s AHI ≥5 with his apnea events predominantly obstructive, the diagnosis of OSAS was established.
Diagnosis of stable COPD
COPD is clinically evaluated and defined by the Global Initiative for Chronic Obstructive Lung disease (GOLD) [16]. The stable COPD was clinically recognized when the COPD symptoms such as cough, expectoration, and wheezing were mild and stable [16].
PAP therapy program
With the use of nasal masks and PAP ventilators (Prisma25ST, Weinmann Inc., Germany), three different PAP models issued from the same ventilator were performed and compared. Before PAP treatment, pressure titration for EPAP and IPAP was carried out in advance for patients to be treated. By connecting end-tidal CO2 (ETCO2) monitor to the nasal mask of a ventilator, the IPAP was unanimously set as the minimal pressure for keeping ETCO2 ≤45 cmH2O.
IPAP in three modes was set the same for each patient, while EPAP was various among different modes. In Bilevel-1 mode (Bilevel-1), EPAP was set as the lowest pressure for disappearance of snoring. In Bilevel-2 mode (Bilevel-2), EPAP was 3 cmH2O higher than in Bilevel-1 for each patient. In auto-trilevel mode (auto-trilevel), the EPAP levels were different between the beginning part (first half) and the EEPAP. For each patient, the initial part of EPAP was the same as in Bilevel-1, while the EEPAP levels automatically elevated in response to the changes in ventilation volume. The auto-trilevel is also called the auto-trilevel PAP therapy. For every patient, each PAP model treatment was employed for one full night (8 h) followed by two nights 0without any PAP treatment as previously published studies [17, 18].
Arterial blood gas analysis
Arterial blood was drawn to have blood gas analysis at the night before each mode of PAP treatment (9:00 P.M.) and in the morning following each mode of overnight PAP therapy (6:00 A.M.). In addition, the titration for IPAP ETCO2 was continuously measured via a nasal mask using a sidestream infrared gas analyzer (compact airway module M-COVX, Datex-Ohmeda, Helsinki, Finland).
Evaluation of daytime sleepiness
The degrees of daytime sleepiness before and following PAP therapies were evaluated with the Epworth Sleepiness Scale (ESS) [19].
Statistical analysis
Values were expressed as mean ± SD for continuous variables. ANOVA of repeated measure data was performed to show any significant difference between the three modes (P < 0.05). If Mauchly’s test of sphericity was not satisfied, the Greenhouse -Geisser adjustment result was used. Bonferroni adjustment was used for multiple comparisons. Data were analyzed using statistical software (SPSS 13.0 for Windows; SPSS, Inc., Chicago).
Results
PAP levels
The IPAP levels at three modes were 17.5 ± 2.3 cmH2O. Their EPAP levels were 6.1 ± 1.3 cmH2O at Bilevel-1, 8.1 ± 1.5 cmH2O at Bilevel-2, and 6.1 ± 1.4 cmH2O at auto-trilevel. The EEPAP levels were 8.9 ± 1.8 cmH2O at auto-trilevel.
Since all patients recruited had different degrees of hypercapnia, during PAP treatment, titrated IPAPs were relatively higher. Before each mode of PAP treatment, there were no significant changes in daytime drowsiness (ESS) (Fig. 3) and morning PaCO2 (all P > 0.05) (Table 1). All parameters prior to PAP treatment were expressed as the average from pre-treatment parameters before each mode of treatment.
Changes of Epworth Sleepiness Scale (ESS) before PAP treatment and during different PAP therapies. Number sign: significantly different from the ESS before treatment (P < 0.01); asterisk: significantly different from Bilevel-1 mode (P < 0.05); reference mark: significantly different from Bilevel-2 mode (P < 0.05)
Effects of PAP therapy on sleep respiratory parameters
As shown in Table 1, the AHI before treatment (37.4 ± 12.1) was significantly reduced during each mode of PAP therapy (all P < 0.01), which included an AHI of 6.2 ± 1.4 in Bilevel-1, 3.2 ± 1.0 in Bilevel-2, and 3.5 ± 0.7 in auto-trilevel therapies. Comparison among different modes of PAP therapies demonstrated that there was a statistical difference of AHI between Bilevel-1 and Bilevel-2 therapies (P < 0.05) as well as between Bilevel-1 and auto-trilevel therapies (P < 0.05). However, no remarkable change in AHI was detected between Bilevel-2 and auto-trilevel therapies (P > 0.05).
In addition, the minimal SpO2 (minSpO2) before treatment (61.9 ± 10.8%) elevated significantly during each mode of PAP therapy (all P < 0.01), which included a minSpO2 of 81.8 ± 5.6% in Bilevel-1, 90.1 ± 4.1% in Bilevel-2, and 89.9 ± 3.3% in auto-trilevel therapies. Comparison among different modes of PAP therapies revealed that the minSpO2 during Bilevel-1 therapy was significantly lower than that during Bilevel-2 and auto-trilevel therapies (P < 0.01), while no eminent change in minSpO2 was revealed between Bilevel-2 and auto-trilevel therapies (P > 0.05).
The morning PaCO2 levels following each mode of PAP therapy were all significantly lower than those prior to PAP treatment (56.1 ± 4.1 mmHg) (all P < 0.01). Comparison of morning PaCO2 following different modes of PAP therapies demonstrated that there was significant difference between Bilevel-1 and Bilevel-2 PAP therapies (43.2 ± 3.9 vs 47.6 ± 2.8 mmHg, P < 0.05) as well as between Bilevel-2 and auto-trilevel PAP therapies (43.4 ± 3.7 mmHg) (P < 0.05), but no statistical difference between Bilevel-1 and auto-trilevel (P > 0.05).
Effects of different modes of PAP therapies on sleep quality
Compared with the arousal index (AI) before PAP treatment (28.1 ± 5.2), there was a significant decrease in AI at PAP therapies of Bilevel-1 (5.2 ± 1.0), Bilevel-2 (6.9 ± 1.2), and auto-trilevel (4.1 ± 1.6) (all P < 0.01). Comparison of AI at different mode PAP therapies revealed that (a) AI was the highest in Bilevel-2 but the lowest in auto-trilevel and (b) there was a significant difference among three different PAP modes (all P < 0.05) (Fig. 4).
Changes of arousal index (AI) before PAP treatment and during different PAP therapies. Number sign: significantly different from the ESS before treatment (P < 0.01); asterisk: significantly different from Bilevel-1 mode (P < 0.05); reference mark: significantly different from Bilevel-2 mode (P < 0.05)
The N1 + N2/TST% before PAP therapy (73.2 ± 4.4%) was significantly reduced during PAP treatment (all P < 0.01) such as during Bilevel-1 (67.2 ± 4.1%), Bilevel-2 (62.3 ± 3.7%), and auto-trilevel (58.6 ± 3.3%) PAP therapies. Comparison of N1 + N2/TST among different modes of PAP therapies showed that there was no statistical difference in N1 + N2/TST% between Bilevel-1 and Bilevel-2 as well as between Bilevel-2 and auto-trilevel PAP therapies (all P > 0.05) (Table 1).
The N3/TST% before PAP therapy (8.0 ± 1.9%) was significantly increased during PAP therapies (all P < 0.01) such as during Bilevel-1 (11.4 ± 2.1%), Bilevel-2 (15.3 ± 2.3%), and auto-trilevel (19.9 ± 2.8%) PAP therapies. There was statistical difference in N3/TST% among three modes of PAP therapies (all P > 0.05).
Compared with REM/TST% before PAP therapy (18.8 ± 4.7%), there was statistical elevation during Bilevel-2 (22.4 ± 3.6%) and auto-trilevel (21.5 ± 3.3%) PAP therapies (all P < 0.05), but no statistical change during Bilevel-1 (21.4 ± 2.1%) (P > 0.05). No statistical difference in REM/TST% was demonstrated among three different modes of PAP therapies (all P > 0.05).
Sleep efficiency (TST/TRT%) before PAP treatment (60.2 ± 7.1%) was significantly elevated during all three modes of PAP therapies (all P < 0.01) including Bilevel-1 (72.1 ± 5.4%), Bilevel-2 (78.4 ± 4.1%), and auto-trilevel (82.9 ± 4.1%). Comparison among three modes of PAP therapies indicated a statistical change among different modes (all P < 0.05) (Table 1).
Comparison of ESS
Compared with the daytime ESS before PAP therapy (11.6 ± 2.9), ESS was significantly reduced at the days following each mode of PAP therapies (all P < 0.05). Comparison among three different PAP modes showed that the daytime ESS was the lowest at the day following auto-trilevel therapy (5.3 ± 1.7) but the highest at the day following Bilevel-2 therapy (7.5 ± 1.6) with the day following Bilevel-1 therapy in between (7.6 ± 1.9). No statistical difference in daytime ESS was detected between Bilevel-1 and Bilevel-2 therapies. However, there are significant differences in daytime sleepiness between auto-trilevel and Bilevel-1 as well as between auto-trilevel and Bilevel-2 therapies (all P < 0.05) (Fig. 3).
Discussion
Both OSAS and COPD are two common respiratory diseases often concurrent within one individual. In recent years, more and more attention has been paid to the deleterious effects of comorbid COPD and OSAS [20]. The O2 desaturation at sleep in OS patients was more serious than that in COPD patients with the same extent of bronchial obstruction. Moreover, OS patients have a higher risk of type 2 respiratory failure and pulmonary artery hypertension than the patients suffering from only one of the diseases [4,5,6]. Since both COPD and OSAS have been recognized as independent risk factors of cardiovascular disorders and their coexistence as OS possibly enhances such a risk, patients with OS have a substantially higher morbidity and mortality than the patients suffering from either COPD or OSA [6]. This usual concurrency of OSAS and COPD may exhibit important implications for diagnosis, treatment, and consequences [6]. Even though noninvasive ventilators have proved their efficacy in OS patients, the association of different ventilation modes with their variety in efficacy has not yet been well investigated.
Although CPAP has been applied to solve the problems of upper airway collapse and obstruction in OSAS patients, there are still some adverse effects of CPAP on pulmonary mechanics and CO2 retention’s elimination in patients with obstructive upper airway [21]. Instead of CPAP, conventional BiPAP treatment with a difference between IPAP and EPAP (Pdifference) has been successfully used for OS patients and shown its efficacy to a certain degree for OS patients with hypercapnia [22, 23]. Since in OS patients, their obstructive sleep apnea (OSA) events selectively occur only at sleep, the EPAP demands are changing from awake to sleep and vice versa. In addition, to eliminate hypercapnia, enough ventilation volume is needed. Bilevel PAP can assist COPD patients to increase their ventilation by providing a Pdifference. Usually the higher the Pdifference is, the more effective it is to increase ventilation volume and remove hypercapnia. Because in clinical practice, COPD patients under Bilevel PAP treatment are often complained of discomfort when IPAP was set too high and so comes a lower compliance to Bilevel PAP therapy. However, if the EPAP was set too lower in order to keep enough Pdifference, the upper airway may suffer from collapse at expiration during sleep. Such a collapse is especially prone to take place at the end stage of expiration [14]. To solve these problems and improve efficacy, auto-trilevel PAP mode, a new auto-adjusting bilevel mode with additional EEPAP, is designed for clinical use. In this study, the efficacy of auto-trilevel PAP mode was tested for its efficacy in OS patients by comparison with conventional Bilevel PAP treatment modes.
To compare with auto-trilevel PAP treatment, two modes of Bilevel PAP were used. In Bilevel-1, enough Pdifference could effectively eliminate the previously existing hypercapnia, but a relatively higher residual OSA event was noticed. While in Bilevel-2, a higher EPAP could eminently reduce the residual OSA events, but the problem of hypercapnia could not be efficiently avoided. Auto-trilevel PAP is a combination of three PAP levels, IPAP, EPAP, and EEPAP. A relatively lower EPAP is beneficial for CO2 discharge while a higher EEPAP is in favor of eliminating residual OSA events. Our results revealed that by comparison with conventional Bilevel PAP therapy in OS patients, the auto-trilevel PAP treatment was superior in simultaneous removal of hypercapnia and residual OSA events; moreover, a better sleep quality and milder daytime drowsiness were achieved during application of auto-trilevel mode for OS patients with hypercapnia.
The limitation of this study is that the recruited sample is still small; further investigation is commendatory to enlarge the sample at multiple centers and find out what type of OS patients benefit most from this treatment algorithm.
References
Borukhov I, Rizzolo D (2016) Overlap syndrome: obstructive sleep apnea and chronic obstructive pulmonary disease. JAAPA 29:18–22
Tsai SC (2016) Chronic obstructive pulmonary disease and sleep related disorders. Curr Opin Pulm Med
McNicholas WT (2016) Chronic obstructive pulmonary disease and obstructive sleep apnoea-the overlap syndrome. J Thorac Dis 8:236–242
Lacedonia D, Carpagnano GE, Aliani M, Sabato R, Foschino Barbaro MP et al (2013) Daytime PaO2 in OSAS, COPD and the combination of the two (overlap syndrome). Respir Med 107:310–316
Shiina K, Tomiyama H, Takata Y, Yoshida M, Kato K, Nishihata Y et al (2012) Overlap syndrome: additive effects of COPD on the cardiovascular damages in patients with OSA. Respir Med 106:1335–1341
Marin JM, Soriano JB, Carrizo SJ, Boldova A, Celli BR (2010) Outcomes in patients with chronic obstructive pulmonary disease and obstructive sleep apnea: the overlap syndrome. Am J Respir Crit Care Med 182:325–331
Mansukhani MP, Kolla BP, Olson EJ, Ramar K, Morgenthaler TI (2014) Bilevel positive airway pressure for obstructive sleep apnea. Expert Rev Med Devices 11:283–294
Murphy PB, Arbane G, Ramsay M, Suh ES, Mandal S et al (2015) Safety and efficacy of auto-titrating noninvasive ventilation in COPD and obstructive sleep apnoea overlap syndrome. Eur Respir J 46:548–551
Zhang XW, Cai W, Jin F, Zhang YQ, Zhang XL (2011) Effect of bi-level positive airway pressure ventilator on the heart function and vascular endothelial function of patients with the overlap syndrome. Zhonghua Jie He He Hu Xi Za Zhi 34:17–20
Verbraecken J (2014) From CPAP to trilevel adaptive servo ventilation in chronic heart failure—have we got the magic bullet? Sleep Med 15:846–848
Oldenburg O, Bitter T, Wellmann B, Fischbach T, Efken C, Schmidt A et al (2012) Trilevel adaptive servoventilation for the treatment of central and mixed sleep apnea in chronic heart failure patients. Sleep Med 14:422–427
Heinzer R, White DP, Malhotra A, Lo YL, Dover L, Stevenson KE et al (2008) Effect of expiratory positive airway pressure on sleep disordered breathing. Sleep 31:429–432
Braga CW, Chen Q, Burschtin OE, Rapoport DM, Ayappa I (2011) Changes in lung volume and upper airway using MRI during application of nasal expiratory positive airway pressure in patients with sleep-disordered breathing. J Appl Physiol 111:1400–1409
Morrell MJ, Arabi Y, Zahn B, Badr MS (1998) Progressive retropalatal narrowing preceding obstructive apnea. Am J Respir Crit Care Med 158:1974–1981
American Academy of Sleep Medicine Task Force (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep 22:667–689
Celli BR, MacNee W, ATS/ERS task force (2004) Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 23:932–946
Teschler H, Döhring J, Wang YM, Berthon-Jones M (2001) Adaptive pressure support servo-ventilation: a novel treatment for Cheyne-Stokes respiration in heart failure. Am J Respir Crit Care Med 164:614–619
Zhang XL, Yin KS, Li XL, Jia EZ, Su M (2006) Efficacy of adaptive servoventilation in patients with congestive heart failure and Cheyne-Stokes respiration. Chin Med J 119:622–627
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Sanders MH, Newman AB, Haggerty CL, Redline S, Lebowitz M, Samet J et al (2003) Sleep and sleep-disordered breathing in adults with predominantly mild obstructive airway disease. Am J Respir Crit Care Med 167:7–14
Murphy PB, Arbane G, Ramsay M, Suh ES, Mandal S, Jayaram D et al (2015) Safety and efficacy of auto-titrating noninvasive ventilation in COPD and obstructive sleep apnoea overlap syndrome. Eur Respir J 46:548–551
Kouns A, Phillips B (2011) New developments in the management of chronic obstructive pulmonary disease and the overlap syndrome. Curr Treat Options Neurol 13:488–495
De Backer L, Vos W, Dieriks B, Daems D, Verhulst S, Vinchurkar S et al (2011) The effects of long-term noninvasive ventilation in hypercapnic COPD patients: a randomized controlled pilot study. Int J Chron Obstruct Pulmon Dis 6:615–624
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in this study involving human participants were in accordance with the ethical standards of Patient Ethics and Research Committee of the First Affiliated Hospital of Nanjing Medical University and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare that they have no conflict of interest.
Funding
The 333 high level personnel training program in Jiangsu Province (BRA-2014131) provided financial support in the form of ventilator application training, and the key research and development program of Huai’an (social development HAS201611) provided financial support in the form of necessary equipment for this study. The sponsors had no role in the design or conduct of this research.
Rights and permissions
About this article
Cite this article
Su, M., Huai, D., Cao, J. et al. Auto-trilevel versus bilevel positive airway pressure ventilation for hypercapnic overlap syndrome patients. Sleep Breath 22, 65–70 (2018). https://doi.org/10.1007/s11325-017-1529-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1529-y