Abstract
Purpose
Microvesicles (MVs) have been implicated in the pathomechanism of obstructive sleep apnoea (OSA); however, the results are inconsistent, possibly due to an unrevealed temporal variation in circulating MV levels. We aimed to investigate the diurnal changes of MV fractions in OSA.
Methods
Peripheral blood was taken from 18 patients with OSA and 9 healthy subjects at different time points (11:00, 17:00, 21:00, 01:30 and 06:00). Samplings were repeated in nine OSA patients after 2 months of continuous positive airway pressure (CPAP) therapy. CD41+, CD62P+, glycophorin A+ and Annexin V+ MVs were determined with flow cytometry. Areas under the MV concentrations-time curves (AUC) were calculated and correlated with the severity of OSA.
Results
A significant diurnal variability of plasma CD41+ and Annexin V+ MVs was observed only in OSA with a marked peak at 17:00. There was a direct correlation between CD41+ MV AUCs and the severity of OSA. CPAP treatment reduced diurnal variability in both CD41+ and Annexin V+ MV levels.
Conclusions
The relationship between the diurnal variability of CD41+ MVs and disease severity as well as the effect of CPAP treatment on MV levels support the role of MVs in the pathophysiology of OSA. More importantly, considering the significant diurnal variation in circulating MV levels, introduction of strict protocols for blood sampling is required for MV measurements.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnoea (OSA) is a common disorder which is characterised by repetitive overnight hypoxic episodes and subsequent microarousals caused by a complete or partial collapse of the upper airways. It is usually associated with subsequent daily symptoms and long-term cardiovascular and metabolic consequences. Although pathophysiological processes which link OSA with comorbidities are widely investigated, these are not fully understood. Microvesicles (MVs) are small (0.1–1.0 μm), plasma membrane-covered particles which are released by different cell types constitutively and also upon stimulation. As a consequence of their origin, the surface marker as well as the intra-particular protein composition of MVs are characteristic to their parent cells and can be used for identification. It is also well known that they can cargo mRNAs and several regulatory molecules including miRNAs. Target cells can translate extracellular vesicle-associated mRNAs into proteins [1], which exert diverse functions in apoptosis [2], coagulation [3] and vasculogenesis [4], and may also modulate immunologic responses [5] or even participate in antigen presentation [6]. In addition, elevated MV levels correlate with the metabolic syndrome components of diabetes [7] and atherosclerosis [8]. Therefore, it is not surprising that various MV fractions have extensively been studied in OSA and were proposed as potential mediators which may link OSA to comorbidities [9].
However, the results on circulating MVs in OSA are inconsistent. Both higher [3, 10, 11] and similar [4, 12, 13] levels of platelet-derived MVs were reported. Variable results on endothelial MVs were also published [2, 4, 8, 10, 11, 14]. Studies investigating leukocyte-derived MVs are more consistent with higher levels being reported [4, 10, 11, 13]. The former discrepancies among studies may be due to the fact that samples for MV measurements were collected at different time points. This is a relevant issue, considering that many studies report a disturbed diurnal variation in airway [15] and circulating [16, 17] biomarkers in OSA compared to healthy controls. Studies by Geiser et al. and Trzepizur et al. measured circulating MVs at two different time points in OSA [12, 18]. However, the diurnal variation of circulating MVs has not been studied in details so far.
Therefore, our aim was to analyse diurnal changes in the levels of plasma microvesicles in patients with OSA and control subjects. We also investigated the effect of continuous positive airway pressure (CPAP) therapy on MV diurnal variability.
Methods
Study design and subjects
Eighteen patients with OSA (46 ± 7 years) and 9 healthy controls (42 ± 6 years, 6 male) participated in the study. OSA was diagnosed based on an overnight polysomnography (PSG) and all subjects had apnoea-hypopnoea index (AHI) more than ten events per hour. None of the patients had used CPAP device before participating in the study. Control subjects were healthy volunteers without any history of excessive daily sleepiness and an AHI less than five events per hour. Patients with a history of hypertension, cerebrovascular disease, diabetes mellitus and acute coronary syndrome or treated with anticoagulants, platelet aggregation inhibitor or glucocorticoids were excluded from the study. Patients with OSA had similar body mass index (BMI) to control subjects (36.8 ± 4.9 vs. 29.4 ± 9.7 kg/m2, p > 0.05). In nine OSA patients, we repeated the measurements after 2 months of CPAP treatment.
Blood samples were collected at 11:00, 17:00, 21:00, 01:30 and 06:00. PSG was performed between 21:00 and 06:00 on the same day. Subjects were asked to refrain from strenuous exercise during the day of the measurement.
The study was approved by the Scientific Research Ethics Committee (Semmelweis University TUKEB, 30/2014), and patients gave their informed consent.
Polysomnography
PSG was performed as it was described previously [15] according to the American Academy of Sleep Medicine guidelines [19]. AHI, respiratory disturbance index (RDI), oxygen desaturation index (ODI), percent of total sleep time spent with SpO2 <90% (TB90 (TST%)), minimal saturation (SO2 min) and average saturation (SO2 average) were registered and used as indices for OSA severity.
Sample preparation and microvesicle measurements
The sample preparation was performed as it was described previously [20]. Venous blood samples were collected from the median cubital vein using sodium heparin tubes (Vacutainer, Becton Dickinson, Franklin Lakes, USA) and processed immediately after collection. The samples were centrifuged at 1500×g for 5 min at room temperature to make platelet-rich plasma and then at 13,000×g for 10 min at room temperature to make platelet-free plasma (PFP). The separated PFP was aliquoted and stored at −80 °C.
Samples were analysed using a FACSCalibur flow cytometer (BD Biosciences, San Jose, USA). PFP samples were defrosted, diluted in phosphate-buffered saline (1:500) and stained with fluorochrome-conjugated monoclonal antibodies for the identification of MVs of various cellular origins. The instrument settings and MV gating were adopted from our previous work [20]. Briefly, MVs were first gated on the basis of size and complexity, and then MVs of various cellular origins were detected as positive events in the appropriate fluorescence emission channels corresponding to the labelling antibodies (Fig. 1). The MV gating was established using 1 μm calibration beads as an upper right corner of the gate. The lower border was determined after assessing signal/noise ratios and positive event numbers. For the calculation of absolute MV counts, PKH26 Reference Microbeads (Sigma–Aldrich Co., St. Louis, USA) were used. All antibodies were from BD Biosciences Pharmingen (San Jose, CA, USA). Background fluorescence was compared with that of the isotype-control antibody.
Detection of microvesicle fractions with flow cytometry. Microvesicles (MVs) were identified on the basis of size and complexity. Representative plots and histograms show typical CD41+ (a) and Annexin V+ (b) measurements of samples collected at 6:00 and at 17:00. Numbers indicate percent in parent gate (FSC forward scatter, SSC side scatter)
Statistical analysis
GraphPad Prism 5.0 (GraphPad Software Inc., San Diego, CA, USA) was used for statistical analysis. Within-group changes were analysed with repeated-measures ANOVA followed by Bonferroni post hoc test. Two-way ANOVA test was applied to compare diurnal changes of microvesicles between groups with Bonferroni post hoc test to compare results at each time point. Microvesicle concentrations were expressed along time, and areas under the concentration-time curve (AUC) were calculated for each subject. To assess the relationship between the magnitude of diurnal variability and the severity of OSA, AUC values were correlated with clinical variables registered during PSG.
The sample size was estimated to detect between-group differences in temporal changes of any MV fraction with an effect size of 0.25 and a power of 0.80 [21]. A p value <0.05 was considered significant.
Results
Diurnal changes in circulating microvesicles within groups
There was no change either in CD62P+ MVs or glycophorin A+ particles in any group (p > 0.05, repeated-measures ANOVA). CD41+ MV levels significantly altered in OSA (p < 0.01) but not in controls (p = 0.65, Fig. 2a). Similarly, Annexin V+ MV levels changed significantly only in OSA (p < 0.01), without any alteration in control subjects (p = 0.47, Fig. 2b). In patients with OSA, both CD41+ and Annexin V+ MV levels were significantly higher at 17:00 compared with all other time points (p < 0.05, Fig. 2).
Comparison of diurnal variations of circulating microvesicles between groups
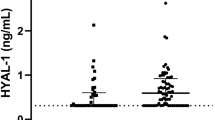
Comparing OSA and control groups using two-way ANOVA, the levels of CD41+ (Fig. 2a) and Annexin V+ (Fig. 2b) MVs were significantly higher in OSA patients compared to healthy controls, without any difference in CD62P+ or glycophorin A+ particles. Using Bonferroni post hoc tests, the differences between OSA patients and healthy controls were significant at 17:00 for CD41+ and also for Annexin V+ MVs.
Relationship between diurnal variability of MVs and severity of OSA
Significant direct correlations were shown between the AUC of CD41+ MVs and AHI (p < 0.01, r = 0.60, Fig. 3), RDI (p = 0.02, r = 0.55), ODI (p < 0.01, r = 0.65), TB90 (TST%) (p = 0.02, r = 0.55), SO2min (p = 0.03, r = −0.53) and SO2average (p = 0.03, r = −0.52). In contrast, none of the other measured MVs’ AUCs correlated with the severity of OSA. There was no correlation between BMI and any of the MVs’ AUCs (all p > 0.05).
The effect of CPAP treatment on circulating MVs
Apnoea-hypopnoea index decreased in nine patients with OSA after 2 months of CPAP treatment (from 40.4 ± 19.5 to 1.9 ± 1.7/h, p < 0.01), without any change in BMI (p > 0.05). The diurnal variation for CD41+ and Annexin V+ MVs were blunted following 2 months of CPAP treatment. The MV peak observed in untreated OSA at 17:00 was significantly diminished by 2 months of CPAP therapy (both p < 0.05, for CD41+ and Annexin V+ MVs, Fig. 4).
The effect of CPAP treatment on diurnal variability of CD41+ and Annexin V+ microvesicles in patients with OSA. CPAP treatment significantly reduced diurnal variability of CD41+ (a) as well as Annexin V+ (b) levels in patients with OSA (*p < 0.05 Pre-CPAP vs. Post-CPAP, data are expressed as mean ± SEM)
Discussion
In this study, we investigated diurnal changes of circulating microvesicles for the first time. We found a marked rise in CD41+ and Annexin V+ microvesicles in OSA at 17:00. These changes were more pronounced in patients with greater severity, and CPAP treatment reduced the diurnal variability significantly.
Obstructive sleep apnoea is characterised by a significant failure in oxygenation exclusively during sleep, leading to desynchronization of the diurnal rhythm. It is not surprising therefore that the levels of various biomolecules may vary depending on the time of sampling in OSA patients [15–17]. On one hand, these changes may contribute to the complex pathophysiology of this disorder by destabilising the physiological homeostasis of the human body. On the other hand, these alterations may also mislead the researchers providing inconsistent results in clinical studies.
Although diurnal variation of circulating microvesicles has not been investigated before, MV levels at two different time points were compared in two studies. Trzepizur et al. investigated overnight changes in leukocyte-derived (CD62L+) MVs in OSA and control subjects. In the morning, they found a significant decrease in healthy subjects and a significant increase in moderate-to-severe OSA patients compared to the evening measurements [18]. However, analysing platelet-derived MVs, Geiser et al. observed no change between 04:00 and 07:00 in patients with OSA [12].
Erythrocyte-derived glycophorin A+ microvesicles have not been measured in OSA before. We did not observe any difference between OSA and control subjects or in diurnal change in this MV fraction. This may suggest that these MVs do not play a significant role in the pathophysiology of OSA.
Platelet-derived microvesicles have been investigated in numerous studies in OSA [3, 4, 10–13]. CD41 and CD62P are characteristic surface markers of platelets and megakaryocytes, thus expression of these glycoproteins indicate platelet origin. In addition, CD62P (P-selectin) indicates platelet activation [22], which can be investigated in details when analysing changes in CD41/CD62P balance. CD41+ MVs were found to be higher in OSA when measured between 09:00 and 10:00 [10]. Contrarily, when blood was sampled between 07:00 and 08:00, no difference was reported [4]. Interestingly, when the exact time was not mentioned either higher [11] or similar [13], CD41+ MV levels were observed in the morning. These results suggest that CD41 levels tend to fluctuate in OSA which is supported by the current study. Morning CD62P+ microvesicles were investigated only in one study showing no difference between OSA and control subjects [13]. Similarly, we did not find significant difference in CD62P+ MVs between OSA and health. Although nocturnal platelet activation was reported by various studies [23], in line with the findings of Geiser et al. [12], our current study has also pointed out that platelet activation does not necessarily correspond to the release of MVs [12]. Some [3, 11], but not all [10], of the previous studies have found a significant correlation between circulating platelet-derived MVs and severity of OSA. However, the latter study enrolled only patients with mild disease [10]. Supporting the positive findings, we also report a significant association between the severity of OSA and the diurnal production of CD41+ MVs. Moreover, initiation of CPAP treatment significantly reduced platelet-derived MVs [3]; however, CPAP withdrawal did not affect CD41+ MVs levels [24]. In the current study, CPAP therapy significantly decreased CD41+ MV levels. Considering that platelet-derived microvesicles may serve as a potential link to cardiovascular complications [25], our results may add some evidence why CPAP might be effective in the reduction of cardiovascular events in OSA.
Elevated levels of Annexin V+ MVs are associated with procoagulant [26] and proapoptotic [27] capacity in peripheral blood. Practically any cell type can produce Annexin V+ MVs, including endothelial cells [8], leukocytes [11], red blood cells [28] and platelets [11]. Annexin V+ MVs were found to be higher in OSA in some [8, 10, 11], but not all [13, 14], studies. In studies where blood sampling was performed between 06:00 and 09:30 [8] and between 09:00 and 10:00 [10], higher Annnexin V+ MV levels were reported. However, inconsistent results were reported by other studies ignoring specification for the time of blood withdrawal [11, 13, 14], which might be due to the considerable diurnal variation of Annexin V+ MVs in OSA as shown by our study. We found that Annexin V+ MVs tend to peak in the afternoon, which is blunted by CPAP treatment. This may explain why Annexin V+ MV levels measured in the morning did not change after CPAP treatment in a previous work [8].
Although this study was powered to investigate the diurnal variation of MVs in OSA, our findings may also provide valuable new insight into the research on diurnal rhythm of coagulation and cardiovascular events. It is known that the daily incidence of myocardial infarction and stroke has a morning and afternoon peak [29]. In addition, in the afternoon, the activity of tissue plasminogene activator [29] and the potential of platelets for aggregation [30] are on their rise. Our findings are in line with these observations, showing peaks in platelet-derived (CD41+) and procoagulant Annexin V+ MV levels in the afternoon.
The causative or consequential role for the diurnal variability of circulating MVs in OSA has not been explained by the current study. Diurnal monitoring of the platelet function, however, would provide explanation for the significant peak in MV levels at 17:00. The involvement of the MVs in complex machinery of the haemostasis, and their exact contribution to the pathophysiology and complications of OSA are yet to be defined.
In summary, a significant diurnal variation in circulating platelet-derived and Annexin V positive microvesicles has been observed in OSA with a significant peak at 17:00. This variation was related to the severity of OSA and was blunted by CPAP treatment suggesting that the diurnal rhythm of MV formation may play a role in the complex pathophysiology of OSA. Our results may at least partly explain discrepancies between previous studies via revealing the fact that blood collection timing has a significant impact on MV measurements and therefore suggest important methodological considerations for future studies.
References
Gyorgy B, Szabo TG, Pasztoi M, Pal Z, Misjak P, Aradi B, Laszlo V, Pallinger E, Pap E, Kittel A, Nagy G, Falus A, Buzas EI (2011) Membrane vesicles, current state-of-the-art: emerging role of extracellular vesicles. Cellular and molecular life sciences : CMLS 68(16):2667–2688. doi:10.1007/s00018-011-0689-3
Jelic S, Lederer DJ, Adams T, Padeletti M, Colombo PC, Factor P, Le Jemtel TH (2009) Endothelial repair capacity and apoptosis are inversely related in obstructive sleep apnea. Vasc Health Risk Manag 5:909–920
Maruyama K, Morishita E, Sekiya A, Omote M, Kadono T, Asakura H, Hashimoto M, Kobayashi M, Nakatsumi Y, Takada S, Ohtake S (2012) Plasma levels of platelet-derived microparticles in patients with obstructive sleep apnea syndrome. J Atheroscler Thromb 19(1):98–104
Tual-Chalot S, Gagnadoux F, Trzepizur W, Priou P, Andriantsitohaina R, Martinez MC (2014) Circulating microparticles from obstructive sleep apnea syndrome patients induce endothelin-mediated angiogenesis. Biochim Biophys Acta 1842(2):202–207. doi:10.1016/j.bbadis.2013.11.017
Szabo GT, Tarr B, Paloczi K, Eder K, Lajko E, Kittel A, Toth S, Gyorgy B, Pasztoi M, Nemeth A, Osteikoetxea X, Pallinger E, Falus A, Szabo-Taylor K, Buzas EI (2014) Critical role of extracellular vesicles in modulating the cellular effects of cytokines. Cellular and molecular life sciences : CMLS. doi:10.1007/s00018-014-1618-z
Raposo G, Nijman HW, Stoorvogel W, Liejendekker R, Harding CV, Melief CJ, Geuze HJ (1996) B lymphocytes secrete antigen-presenting vesicles. J Exp Med 183(3):1161–1172
Diamant M, Nieuwland R, Pablo RF, Sturk A, Smit JW, Radder JK (2002) Elevated numbers of tissue-factor exposing microparticles correlate with components of the metabolic syndrome in uncomplicated type 2 diabetes mellitus. Circulation 106(19):2442–2447
Yun CH, Jung KH, Chu K, Kim SH, Ji KH, Park HK, Kim HC, Lee ST, Lee SK, Roh JK (2010) Increased circulating endothelial microparticles and carotid atherosclerosis in obstructive sleep apnea. Journal of clinical neurology (Seoul, Korea) 6(2):89–98. doi:10.3988/jcn.2010.6.2.89
Trzepizur W, Martinez MC, Priou P, Andriantsitohaina R, Gagnadoux F (2014) Microparticles and vascular dysfunction in obstructive sleep apnoea. The European respiratory journal. doi:10.1183/09031936.00197413
Ayers L, Ferry B, Craig S, Nicoll D, Stradling JR, Kohler M (2009) Circulating cell-derived microparticles in patients with minimally symptomatic obstructive sleep apnoea. The European respiratory journal 33(3):574–580. doi:10.1183/09031936.00107408
Kim J, Bhattacharjee R, Kheirandish-Gozal L, Spruyt K, Gozal D (2011) Circulating microparticles in children with sleep disordered breathing. Chest 140(2):408–417. doi:10.1378/chest.10-2161
Geiser T, Buck F, Meyer BJ, Bassetti C, Haeberli A, Gugger M (2002) In vivo platelet activation is increased during sleep in patients with obstructive sleep apnea syndrome. Respiration; international review of thoracic diseases 69(3):229–234 doi:63625
Priou P, Gagnadoux F, Tesse A, Mastronardi ML, Agouni A, Meslier N, Racineux JL, Martinez MC, Trzepizur W, Andriantsitohaina R (2010) Endothelial dysfunction and circulating microparticles from patients with obstructive sleep apnea. Am J Pathol 177(2):974–983. doi:10.2353/ajpath.2010.091252
Akinnusi ME, El Solh AA (2009) Circulating endothelial microparticle levels and hemodynamic severity of pulmonary hypertension: is there a role for sleep apnea? Am J Respir Crit Care Med 179(4):328 . doi:10.1164/ajrccm.179.4.328aauthor reply 328-329
Kunos L, Bikov A, Lazar Z, Korosi BZ, Benedek P, Losonczy G, Horvath I (2014) Evening and morning exhaled volatile compound patterns are different in obstructive sleep apnoea assessed with electronic nose. Sleep & breathing = Schlaf & Atmung. doi:10.1007/s11325-014-1003-z
Vgontzas AN, Bixler EO, Lin HM, Prolo P, Trakada G, Chrousos GP (2005) IL-6 and its circadian secretion in humans. Neuroimmunomodulation 12(3):131–140. doi:10.1159/000084844
Jordan W, Reinbacher A, Cohrs S, Grunewald RW, Mayer G, Ruther E, Rodenbeck A (2005) Obstructive sleep apnea: plasma endothelin-1 precursor but not endothelin-1 levels are elevated and decline with nasal continuous positive airway pressure. Peptides 26(9):1654–1660. doi:10.1016/j.peptides.2005.02.012
Trzepizur W, Priou P, Paris A, Nardi J, Tual-Chalot S, Meslier N, Urban T, Andriantsitohaina R, Martinez MC, Gagnadoux F (2011) Nocturnal release of leukocyte-derived microparticles in males with obstructive sleep apnoea. The European respiratory journal 37(5):1293–1295. doi:10.1183/09031936.00150010
Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Loube DL, Owens J, Pancer JP, Wise M (2005) Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28(4):499–521
Pap E, Pallinger E, Falus A, Kiss AA, Kittel A, Kovacs P, Buzas EI (2008) T lymphocytes are targets for platelet- and trophoblast-derived microvesicles during pregnancy. Placenta 29(9):826–832. doi:10.1016/j.placenta.2008.06.006
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*power 3.1: tests for correlation and regression analyses. Behav Res Methods 41(4):1149–1160. doi:10.3758/brm.41.4.1149
van der Zee PM, Biro E, Ko Y, de Winter RJ, Hack CE, Sturk A, Nieuwland R (2006) P-selectin- and CD63-exposing platelet microparticles reflect platelet activation in peripheral arterial disease and myocardial infarction. Clin Chem 52(4):657–664. doi:10.1373/clinchem.2005.057414
Barcelo A, Pierola J, de la Pena M, Frontera G, Yanez A, Alonso-Fernandez A, Ayllon O, Agusti AG (2012) Impaired circadian variation of platelet activity in patients with sleep apnea. Sleep & breathing = Schlaf & Atmung 16(2):355–360. doi:10.1007/s11325-011-0501-5
Ayers L, Stoewhas AC, Ferry B, Stradling J, Kohler M (2013) Elevated levels of endothelial cell-derived microparticles following short-term withdrawal of continuous positive airway pressure in patients with obstructive sleep apnea: data from a randomized controlled trial. Respiration; international review of thoracic diseases 85(6):478–485. doi:10.1159/000342877
Kafian S, Mobarrez F, Wallen H, Samad B (2015) Association between platelet reactivity and circulating platelet-derived microvesicles in patients with acute coronary syndrome. Platelets 26(5):467–473. doi:10.3109/09537104.2014.940304
Mallat Z, Benamer H, Hugel B, Benessiano J, Steg PG, Freyssinet JM, Tedgui A (2000) Elevated levels of shed membrane microparticles with procoagulant potential in the peripheral circulating blood of patients with acute coronary syndromes. Circulation 101(8):841–843
Werner N, Wassmann S, Ahlers P, Kosiol S, Nickenig G (2006) Circulating CD31+/annexin V+ apoptotic microparticles correlate with coronary endothelial function in patients with coronary artery disease. Arterioscler Thromb Vasc Biol 26(1):112–116. doi:10.1161/01.atv.0000191634.13057.15
Livaja Koshiar R, Somajo S, Norstrom E, Dahlback B (2014) Erythrocyte-derived microparticles supporting activated protein C-mediated regulation of blood coagulation. PLoS One 9(8):e104200. doi:10.1371/journal.pone.0104200
Manfredini R, Boari B, Smolensky MH, Salmi R, la Cecilia O, Maria Malagoni A, Haus E, Manfredini F (2005) Circadian variation in stroke onset: identical temporal pattern in ischemic and hemorrhagic events. Chronobiol Int 22(3):417–453. doi:10.1081/cbi-200062927
Haus E, Cusulos M, Sackett-Lundeen L, Swoyer J (1990) Circadian variations in blood coagulation parameters, alpha-antitrypsin antigen and platelet aggregation and retention in clinically healthy subjects. Chronobiol Int 7(3):203–216
Acknowledgements
The study was supported by Hungarian Respiratory Society (grants to Andras Bikov and Zsolt I. Komlosi) as well as Hungarian Scientific Research Fund (OTKA 68758, 109008). The authors are also grateful to Elektro-Oxigén Inc. for providing the polysomnographic devices. This publication was supported by the Janos Bolyai Research Scholarship of the Hungarian Academy of Sciences to Andras Bikov. The authors are extremely grateful to Mrs. Monika Banlaky for her technical assistance with PSG.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Hungarian Respiratory Society (grants to Andras Bikov and Zsolt I. Komlosi) as well as Hungarian Scientific Research Fund (OTKA 68758, 109008) provided financial support in the form of funding to buy materials and reagents for experiments. The sponsor had no role in the design or conduct of this research.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Bikov, A., Kunos, L., Pállinger, É. et al. Diurnal variation of circulating microvesicles is associated with the severity of obstructive sleep apnoea. Sleep Breath 21, 595–600 (2017). https://doi.org/10.1007/s11325-017-1464-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-017-1464-y