Abstract
Purpose
This study aimed to determine the prevalence of positional obstructive sleep apnea (OSA) and its subtypes in Korean adults with newly diagnosed OSA and document the clinical characteristics of positional OSA and its subtypes compared to non-positional OSA
Methods
In this cross-sectional study, we evaluated 1052 OSA adults. Positional OSA was defined as an overall apnea-hypopnea index (AHI) ≥5 and supine AHI to non-supine AHI ratio of ≥2. Positional OSA was subtyped depending on the degree of AHI while in the non-supine position: subtype I (a non-supine AHI <5/h), subtype II (a non-supine AHI ≥5/h and <15/h), and subtype III (a non-supine AHI ≥15/h). To compare clinical characteristics between patient groups depending on the positional tendency of OSA, statistical analyses were performed.
Results
The prevalence of positional OSA was 75.6 % with 39.9 % having AHI normalized <5/h while in non-supine position. Positional OSA patients had milder OSA, older age, and lower BMI than did non-positional OSA patients. However, having positional OSA did not influence daytime sleepiness, depressive symptoms, anxiety, and health-related quality of life. Unlike the subtype I and II positional OSAs, subtype III did not differ in clinical features from non-positional OSA. There were significant differences in supine sleep time depending on the positional tendency of OSA. Subtype III positional OSA had the shortest supine sleep time whereas subtype I positional OSA and non-positional OSA had the longest supine sleep time.
Conclusions
Positional OSA subtypes have different clinical characteristics. Subtyping of positional OSA is helpful for developing specific treatment strategies according to positional tendency
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) syndrome is a common sleep disorder characterized by repetitive obstruction of the upper airway during sleep [1, 2] and has been identified as an independent risk factor for a number of cardiovascular diseases [3]. Positional OSA is a phenotype of OSA in which sleep apneas occur predominantly during sleep in the supine position [4]. The mechanisms underlying positional OSA including its interaction with upper airway collapsibility, or reduced lung volume, are poorly understood [4].
With regard to the criteria for defining positional OSA, Cartwright [5] was the first to describe the arbitrary cutoff point of a difference of 50 % or more in apnea index between supine and non-supine sleep positions. Since then, modified versions of Cartwright’s criteria have been applied in literature [6–9], but there are no universally used criteria for positional OSA. Although prevalence rates vary depending on the criteria defining positional OSA, positional OSA accounts for a significant portion of the OSA population, ranging from 50 to 60 % of OSA patients who present to sleep clinics [10, 11], and occurs more commonly in non-obese patients and patients with mild or moderate OSA rather than severe OSA [6–11].
Management of positional OSA has been significantly improved recently with the introduction of a new generation of positional therapy. A small device attached to either the neck or chest prevents patients with positional OSA from sleep at the supine position through a vibrating stimulus without negatively influencing sleep efficiency [12, 13]. The effectiveness of this simple therapy gave more clinical significance to identifying suitable candidates for positional therapy. However, there are few studies about classification and characterization of subtypes of positional OSA [4, 9]. Recently, two subtypes of positional OSA, i.e., supine-predominant OSA (spOSA) and supine-isolated OSA (siOSA) were proposed and compared [4, 9]. The Amsterdam Positional OSA Classification was recently developed focusing on selecting patients who have a clinically significant improvement with positional therapy, but it needs to be further validated [14]. More understanding is needed to develop specific treatment strategies for different subtypes of positional OSA.
The aims of this study were threefold: (1) to determine the prevalence of positional OSA and its subtypes in Korean adults with newly diagnosed OSA, (2) to document the clinical characteristics of positional OSA and its subtypes compared to non-positional OSA, and (3) to determine the associations between subtypes of positional OSA and sleep in the supine position.
Materials and methods
Patients
This was a cross-sectional, single center study including a consecutive series of patients who underwent a polysomnography (PSG) for evaluation of suspected OSA between 2011 and 2013. Criteria for inclusion were as follows: aged over 18 years and newly diagnosed with OSA (apnea-hypopnea index (AHI) ≥5 per hour) by a full-night PSG. Patients were excluded if they had total sleep time less than 100 min; if they had supine or non-supine sleep time less than 30 min; or if they had an active medical, neurological, or psychiatric disorder that would impact their health-related quality of life (HRQoL). Patients with hypertension or type 2 diabetes without overt cardiovascular complications were not excluded. Basic demographic information, medical comorbidities, and medication information were obtained from the self-reported checklist for medical history and electronic medical record. The patient’s body mass index (BMI) was determined on the day of PSG. The study was reviewed and approved by the Institutional Review Board of Asan Medical Center.
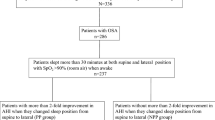
Of the 1440 patients included, 388 were excluded because of supine or non-supine sleep time <30 min (n = 210), total sleep time <100 min (n = 10), and major medical diseases (n = 168). The remaining 1052 subjects (838 men and 214 women) were included in the study (Table 1). The mean age was 51.2 years (SD 11.4 years) and the mean BMI was 26.2 kg/m2 (SD 3.7).
Definitions of positional OSA
We categorized patients as having positional or non-positional OSA according to the criteria suggested by Cartwright [5], which is the most common definition for positional OSA used today. This defined positional OSA (i.e., spOSA) if overall AHI was ≥5/h and a supine AHI was at least two times higher than non-supine AHI [4, 5]. And then, patients with positional OSA were further categorized into the three subtypes depending on the degree of AHI while in the non-supine position: subtype I (i.e., siOSA) which fulfilled a non-supine AHI <5/h, subtype II which fulfilled a non-supine AHI ≥5/h and <15/h, and subtype III which fulfilled a non-supine AHI ≥15/h (Table 2). Respiratory distress in subtype I patients would be normalized by positional therapy alone. Subtype II patients would have a clinically significant improvement with positional therapy, but their AHI was not normalized. Sleep apnea in subtype III patients would improve but remain moderate or severe in severity by positional therapy alone.
Polysomnography
Polysomnography was performed using a digital polygraph system (RemLogic ver. 2.0, Embla Systems Inc., Broomfield, CO, USA). A position sensor is an integrated part of system hardware and is located inside the Patient Unit. A position sensor reacts on physical movement with the output of signals for three directions and differentiates five positions including the supine and the non-supine position (right, left, prone, and upright position). The Patient Unit including a position sensor was attached to the anterior chest wall on the thoracic belt. Sleep and respiratory events were scored according to the 2007 American Academy of Sleep Medicine guidelines [15]. An apnea was defined as a drop in the peak thermal sensor excursion of ≥90 % of the baseline value for at least 10 s. A hypopnea was defined as a nasal pressure signal excursion drop of ≥30 % of the baseline value for at least 10 s, accompanied by a ≥4 % reduction in O2 saturation from the pre-event baseline. AHI was defined as the average number of episodes of apnea and hypopnea per hour. A respiratory effort-related arousal (RERA) was defined as a sequence of breaths lasting at least 10 s characterized by flattening of the nasal pressure waveform and leading to arousal from sleep when the sequence of breaths did not meet criteria for apnea or hypopnea. The respiratory distress index (RDI) was calculated as the average number of episodes of apnea, hypopnea plus RERA per hour. The oxygen desaturation index (ODI) was defined as the number of times that oxygen desaturation was ≥3 % per hour of sleep.
Questionnaires
Daytime sleepiness was evaluated using the Epworth Sleepiness Scale (ESS) [16], which is a self-report, 8-item questionnaire for measuring daytime sleepiness in everyday situations. The total possible score ranges from 0 to 24. Higher scores indicate greater sleepiness during daily activities. Sleep quality was measured using the sleep problems index 2 of the Medical Outcomes Study (MOS)—Sleep Scale [17]. A higher index score indicates poorer sleep quality. Depressive symptoms were assessed using a 21-item BDI [18]. Higher scores represent higher levels of depression. The presence and severity of current symptoms of anxiety (state anxiety level) were assessed using the State Scale of the STAI [19]. The higher the score is, the higher the level of anxiety is. HRQoL was assessed using the Medical Outcomes Study Short-Form Health survey (SF-36) [20], which is non-disease specific and consists of 36 questions measuring 8 domains. All domain scores are transformed, resulting in scale scores from 0 (lowest level of functioning) to 100 (highest level of functioning).
Statistical analysis
Normally distributed data are expressed as a mean and standard deviation, and non-normally distributed data are expressed as a median and interquartile range. To compare patient characteristics between positional and non-positional OSA, statistical analyses were performed using Student’s t test for normally distributed data, the Mann–Whitney U test for non-normally distributed data, or the Chi-square test for categorical variables. To compare patient characteristics between the three positional OSA subgroups and non-positional OSA, statistical analyses were performed using one-way analysis of variance (ANOVA) with Scheffé post hoc test, the Kruskal–Wallis test, or the Chi-square test. The post hoc testing of the Kruskal–Wallis test was performed using the Mann–Whitney U test with the Bonferroni correction. In order to examine the independent factors associated with positional OSA and its subtype I (siOSA) with AHI normalized in the non-supine position, logistic regression analyses were performed on variables with p < 0.1 in univariate analysis. The independent variables included were age, sex, BMI, hypertension, type 2 diabetes, and AHI. Log transformation was applied to the AHI with right-skewed distribution to satisfy the normality assumption. Correlations between supine sleep time and apnea severity were performed using Spearman’s rank correlation test. The significance level was set to p < 0.05. Data were analyzed using SPSS version 21.0 (SPSS Inc., Chicago, IL).
Results
The prevalence of positional OSA
Of the 1052 subjects analyzed in this study, 75.6 % (n = 795) fulfilled the Cartwright’s criteria for positional OSA. Subtype I, subtype II, and subtype III were 39.9, 21.0, and 14.6 % (Table 2), respectively.
Comparison between positional and non-positional OSA
Patients with positional OSA had less severe sleep apnea (p < 0.001) measured by AHI, RDI, ODI, and minimum O2 saturation (MinO2Sat); the older age (p < 0.001); the lower BMI (p < 0.001); the lower proportion of type 2 diabetes (p < 0.01); the better sleep architecture (p < 0.05) including N1, N2, N3, rapid eye movement (REM) sleep, TST, and sleep latency; and the lower SPI-2 scores (p < 0.05) than those with non-positional OSA (Table 3). There were no differences in sex, ESS, BDI, STAI-S, and SF-36 between positional and non-positional OSA. In the subtype analyses, differences of subtype I and II positional OSA from non-positional OSA were similar to overall positional OSA. However, clinical features of subgroup III except the percentage of N2 sleep did not differ from those of non-positional OSA (Table 4).
Based on logistic regression analyses, positional OSA and its subtype I were independently associated with the older age (p < 0.05), the lower BMI (p < 0.001), and the lower AHI (p < 0.001) (Table 5). In addition, a subtype I positional OSA was also independently associated with the absence of type 2 diabetes (p < 0.05).
Relations between positional OSA subtypes and sleep position
There were significant differences in supine sleep time and proportion depending on the positional tendency of OSA. Subtype III positional OSA had the smallest amount and proportion of sleep in a supine position among the patient groups depending on positional tendency (p < 0.001) (Fig. 1 and Table 4). However, there were no differences between subtype I positional OSA and non-positional OSA.
Percentage of supine sleep time in patients with obstructive sleep apnea (OSA) according to positional tendency. Subtype III positional OSA had the smallest proportion of sleep in a supine position among the patient groups depending on positional tendency (p < 0.001). However, there was no difference between subtype I positional OSA and non-positional OSA. Error bar 95 % confidence interval
In patients with both positional and non-positional OSA, supine sleep time and proportion were negatively related to supine AHI (p < 0.001), the AHI differences between supine and non-supine position (p < 0.001), and age (p < 0.01) (Table 6). The overall AHI was positively and negatively related to the amount of supine sleep in patients with positional and non-positional OSA, respectively. Body mass index was negatively related to the amount of supine sleep only in patients with positional OSA. The time spent in supine did not differ depending on gender.
Discussion
There has been a wide range of prevalence of positional OSA in the literature depending on various definitions for positional OSA. The most common definition for positional OSA was that the overall AHI was ≥5/h, and a supine AHI was at least two times higher than non-supine AHI [4, 5]. Using these criteria (i.e., spOSA), the prevalence of positional OSA, 75.6 %, in this study was consistent with 67∼75 % of the Asian population [9, 21, 22] but was higher than 50∼60 % in the Western countries [10, 11, 23]. Using the more strict criteria (i.e., siOSA), the prevalence of subtype I positional OSA having AHI normalized <5/h in the non-supine position was also higher, 39.9 %, in this study comparing to 25∼30 % in the Western countries [7, 11]. The higher prevalence of positional OSA in the Asian population could be partly explained by the lower BMI in the Asian population because obesity is one of the important determining factors for positional OSA.
Most studies consistently show that positional OSA is a milder form of the OSA syndrome [7, 10, 11, 22]. PSG data in this study also showed that positional OSA had milder degree of sleep apnea, more preserved sleep architecture, more total sleep time, and shorter sleep latency than did non-positional OSA. These objective data indicating a milder degree of sleep apnea were accompanied by the better subjective sleep quality measured by the MOS Sleep Scale in this study. The subtype analyses of positional OSA showed that subtypes I and II positional OSA shared clinical characteristics of overall positional OSA compared to non-positional OSA, but subtype III did not differ in clinical features from those of non-positional OSA.
In spite of milder sleep apnea found in positional OSA, having positional OSA did not influence daytime sleepiness, depressive symptoms, anxiety, and HRQoL. Consistent with our data, Mador et al. [7] and Teerapraipruk et al. [21] found no difference in ESS between positional and non-positional OSA groups. Although multiple sleep latency test data from Oksenberg et al. [10] demonstrated a trend toward reduced sleepiness in positional OSA patients compared to non-positional OSA patients, these data were confounded by the fact that the non-positional patients had more severe OSA. In contrast, Joosten et al. [11] reported using the ESS that patients with positional OSA were subjectively rather sleepier than were the other OSA patients. Kim et al. [9] unexpectedly found that the siOSA group, a milder form of positional OSA, had higher Pittsburgh Sleep Quality Index, BDI-2, and Hospital Anxiety Depression Scale scores, indicative of poorer sleep quality and higher levels of depression and anxiety than spOSA. In our study, however, there were no differences in depressive symptoms, anxiety, and HRQoL between positional OSA subtypes. Consistent with our study, some studies [7, 9, 24] showed that there were no significant differences in daytime sleepiness measured by ESS between positional OSA subtypes.
Patients with positional OSA were significantly less obese in the present study, even when controlling for the lower AHI found in the positional OSA. The more strict criteria we used for subtyping positional OSA, the lower BMI the patients with positional OSA had. Consistent with our study, the lower BMI or the smaller neck circumferences has been usually reported to be associated with positional OSA [9–11, 21, 23, 24], although some studies found no difference in BMI between positional and non-positional OSA [21, 25]. However, the relationship between age and positional OSA was inconsistent. Positional OSA was significantly associated with older age in this study but oppositely with younger age in most Western studies [10, 11, 23, 24]. Moreover, some Asian studies found no difference in age between positional and non-positional OSA [9, 21, 25]. It is unclear what made this discrepancy. It could be partially explained by racial differences in the susceptibility to age which may differentiate the features of positional OSA between Asian and Western OSA populations.
The more severe degree of sleep apnea OSA patients has, the lower positional dependency they have. The supine sleep time is an important determining factor of the overall AHI in positional OSA patients regardless of its subtypes. Recently, a Swedish study [24] did not find any difference in time spent in the supine position between positional OSA groups or any correlation between positional dependency and time spent in the supine position. Joosten et al. [4] also described that having spOSA or siOSA does not influence the amount of time spent supine as these patients appear to spend as much time in the supine position as do unselected patients with OSA. In our study, supine sleep time did not differ between positional and non-positional OSA. However, the amount of time spent supine was significantly decreased according to the lower positional dependency among positional OSA subtypes. Therefore, the amount and proportion of sleep in a supine position was the smallest in subtype III positional OSA. However, when the positional dependency disappeared in non-positional OSA, the amount of sleep spent supine was increased up to the level of subtype I positional OSA. These findings imply that positional OSA patients with more severe sleep apnea (subtype III) compared to other positional OSA subtypes spontaneously have developed a strategy of sleeping in the non-supine positions. Similarly, Pevernagie and Shepard [26] reported that positional OSA patients spent significantly less supine sleep time (in relation to the supine AHI severity) than non-positional OSA patients (32 versus 45 % of total sleep).
Certain limitations should be noted when interpreting the results of our present study. First, our study population was recruited from a single university sleep laboratory and was therefore susceptible to referral bias. Second, the deleterious effect of REM sleep on positional OSA was not considered in this study. REM sleep-related OSA has been found in about 34 % of the OSA population and has been much more common in mild and moderate OSA than severe OSA [27]. Third, it is possible that sleeping with a PSG equipment attached predisposes to supine sleep, thus overestimating the apnea severity in positional OSA patients. A prospective study reported that subjects had more supine sleep during a PSG night than during a night when pulse oximetry only was recorded [28]. Finally, it is well recognized that there is a night-to-night variability of the AHI in patients with OSA [29]. Given that the data was collected from a single-night PSG, there is a possibility that PSG phenotypes of positional OSA are not stable and therefore may change over subsequent nights.
In summary, the prevalence of positional OSA was 75.6 % with 39.9 % having AHI normalized <5/h while in non-supine position. Positional OSA patients had milder OSA, older age, and lower BMI than did non-positional OSA patients. The more strict criteria we used for subtyping positional OSA, the lower AHI and BMI positional OSA patients had. However, having positional OSA did not influence daytime sleepiness, depressive symptoms, anxiety, and HRQoL. Unlike the subtype I and II positional OSAs, subtype III did not differ in clinical features from non-positional OSA. There were significant differences in supine sleep time depending on the positional tendency of OSA. Subtype III positional OSA had the shortest supine sleep time, whereas subtype I positional OSA and non-positional OSA had had the longest supine sleep time.
References
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Kang K, Seo JG, Seo SH, Park KS, Lee HW (2014) Prevalence and related factors for high-risk of obstructive sleep apnea in a large Korean population: results of a questionnaire-based study. J Clin Neurol 10:42–49
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342:1378–1384
Joosten SA, O’Driscoll DM, Berger PJ, Hamilton GS (2014) Supine position related obstructive sleep apnea in adults: pathogenesis and treatment. Sleep Med Rev 18:7–17
Cartwright RD (1984) Effect of sleep position on sleep apnea severity. Sleep 7:110–114
Bignold JJ, Mercer JD, Antic NA, McEvoy RD, Catcheside PG (2011) Accurate position monitoring and improved supine dependent obstructive sleep apnea with a new position recording and supine avoidance device. J Clin Sleep Med 7:376–383
Mador MJ, Kufel TJ, Magalang UJ, Rajesh SK, Watwe VGBJB (2005) Prevalence of positional sleep apnea in patients undergoing polysomnography. Chest 128:2130–2137
Permut I, Diaz-Abad M, Chatila W, Crocetti J, Gaughan JP, D’Alonzo GE, Krachman SL (2010) Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. J Clin Sleep Med 6:238–243
Kim KT, Cho YW, Kim DE, Hwang SH, Song ML, Motamedi GK (2016) Two subtypes of positional obstructive sleep apnea: supine-predominant and supine-isolated. Clin Neurophysiol 127:565–570
Oksenberg A, Silverberg DS, Arons E, Radwan H (1997) Positional vs nonpositional obstructive sleep apnea patients: anthropomorphic, nocturnal polysomnographic, and multiple sleep latency test data. Chest 112:629–639
Joosten SA, Hamza K, Sands S, Turton A, Berger P, Hamilton G (2012) Phenotypes of patients with mild to moderate obstructive sleep apnoea as confirmed by cluster analysis. Respirology 17:99–107
vanMaanen JP, Meester KA, Dun LN, Koutsourelakis I, Witte BI, Laman DM, Hilgevoord AA, de Vries N (2013) The sleep position trainer: a new treatment for positional obstructive sleep apnoea. Sleep Breath 17:771–779
Ravesloot MJ, van Maanen JP, Dun L, de Vries N (2013) The undervalued potential of positional therapy in position-dependent snoring and obstructive sleep apnea—a review of the literature. Sleep Breath 17:39–49
Frank MH, Ravesloot MJ, van Maanen JP, Verhagen E, de Lange J, de Vries N (2015) Positional OSA part 1: towards a clinical classification system for position dependent obstructive sleep apnoea. Sleep Breath 19:473–480
American Academy of Sleep Medicine (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester, IL
Cho YW, Lee JH, Son HK, Lee SH, Shin C, Johns MW (2011) The reliability and validity of the Korean version of the Epworth sleepiness scale. Sleep Breath 15:377–384
Kim MK, You JA, Lee JH, Lee SA (2011) The reliability and validity of the Korean version of the medical outcomes study—sleep scale in patients with obstructive sleep apnea. Sleep Med Res 2:89–95
Lee YH, Song JY (1991) A study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. J Korean Neuropsychiatr Assoc 10:93–113
Kim JT, Shin DK (1978) A study based on the standardization of the STAI for Korea. Recent Med 2:69–75
Han CW, Lee EJ, Iwaya T, Kataoka H, Kohzuki M (2004) Development of the Korean version of short-form 36-item health survey: health related QOL of healthy elderly people and elderly patients in Korea. Tohoku J Exp Med 203:189–194
Teerapraipruk B, Chirakalwasan N, Simon R, Hirunwiwatkul P, Jaimchariyatam N, Desudchit T, Charakorn N, Wanlapakorn C (2012) Clinical and polysomnographic data of positional sleep apnea and its predictors. Sleep Breath 16:1167–1172
Mo JH, Lee CH, Rhee CS, Yoon IY, Kim JW (2011) Positional dependency in Asian patients with obstructive sleep apnea and its implication for hypertension. Arch Otolaryngol Head Neck Surg 137:786–790
Richard W, Kox D, den Herder C, Laman M, van Tinteren H, de Vries N (2006) The role of sleeping position in obstructive sleep apnea. Eur Arch Otorhinolaryngol 263:946–950
Sunnergren O, Brostrom A, Svanborg E (2013) Positional sensitivity as a confounder in diagnosis of severity of obstructive sleep apnea. Sleep Breath 17:173–179
Chang ET, Shiao GM (2008) Craniofacial abnormalities in Chinese patients with obstructive and positional sleep apnea. Sleep Med 9:403–410
Pevernagie DA, JW S Jr (1992) Relations between sleep stage, posture and effective nasal CPAP levels in OSA. Sleep 15:162–167
Conwell W, Patel B, Doeing D, Pamidi S, Knutson KL, Ghods F, Mokhlesi B (2012) Prevalence, clinical features, and CPAP adherence in REM-related sleep-disordered breathing: a cross-sectional analysis of a large clinical population. Sleep Breath 16:519–526
Metersky ML, Castriotta RJ (1996) The effect of polysomnography on sleep position: possible implications on the diagnosis of positional obstructive sleep apnea. Respiration 63:283–287
Levendowski DJ, Zack N, Rao S, Wong K, Gendreau M, Kranzler J, Zavora T, Westbrook PR (2009) Assessment of the test-retest reliability of laboratory polysomnography. Sleep Breath 13:163–167
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lee, SA., Paek, JH., Chung, YS. et al. Clinical features in patients with positional obstructive sleep apnea according to its subtypes. Sleep Breath 21, 109–117 (2017). https://doi.org/10.1007/s11325-016-1379-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1379-z