Abstract
Purpose
Review drug-induced sleep endoscopy (DISE) findings in children with Prader-Willi syndrome (PWS) and correlate the patterns of airway collapse with apnea-hypopnea index (AHI) and body mass index (BMI).
Methods
A total of nine children with PWS underwent DISE. DISE findings were recorded using the VOTE classification system. The relationship between different patterns of airway collapse with AHI and BMI was analyzed.
Results
The majority of children with PWS were found to have multilevel obstruction (six out of nine children, 66.6 %). The velum was the most common site of obstruction (nine out of nine children, 100 %). All of the patients had positional obstructive sleep apnea (OSA). Patients with partial or complete anterior-posterior tongue base collapse were associated with a significantly higher AHI (P = 0.016) compared to patients with no anterior-posterior tongue base collapse. Apart from tongue base collapse, no other patterns of airway collapse showed a consistent association with AHI in our results. No patterns of airway collapse showed a significant association with BMI in our study.
Conclusions
In our study, partial or complete anterior-posterior tongue base collapse was associated with higher AHI values in children with PWS. Therefore, careful attention should be addressed to the management of tongue base collapse. Positional therapy could be a potential treatment for patients with PWS since it may alleviate the severity of tongue base collapse.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prader-Willi syndrome (PWS) is a genetic disorder resulting from the absence of paternally expressed imprinted genes at 15q11.2–q13 through paternal deletion of this region (65–75 % of individuals), maternal uniparental disomy 15 (20–30 %), or an imprinting defect (1–3 %) [1].
Sleep-disordered breathing is well documented in PWS population and includes both central and obstructive apnea. Infants with PWS were more likely to experience central sleep apnea. On the contrary, older children with PWS have obstructive sleep apnea (OSA) [2]. The causes of higher prevalence of OSA in this population include hypotonia leading to airway collapsibility, facial dysmorphism, and mid-facial hypoplasia causing small airways, the hypothalamic abnormalities resulting in central apneas, restriction in lung volume due to obesity and scoliosis, the increase in viscosity of secretions, and the adenoid and/or tonsil hypertrophy [1, 3, 4]. Therefore, the Clinical Advisory Board of the PWS Association recommends a polysomnography (PSG) study in all PWS population during infants and early childhood to screen for any breathing problems.
Growth hormone (GH) replacement therapy is a standard treatment for PWS, which has been shown to normalize height, increase lean body mass by decreasing body fat percentage, and improve motor development and possibly cognition [1, 5]. However, there is some controversy as to whether GH treatment exacerbates or ameliorates OSA. Therefore, children should be monitored carefully for the symptoms of OSA throughout GH treatment, and PSG should be followed [3, 6–8].
Children suffering from OSA have been found to have increased rates of attention problems, hyperactivity, and other psychiatric problems such as depressive mood. Besides, lower cognitive function has been detected in children with OSA compared to controls [9]. Treatment options may include behavioral interventions, weight control, continuous positive airway pressure (CPAP), oral appliance therapy, and surgery [4].
Although adenotonsillectomy is generally effective in most children with PWS, it may not be curative in children with severe OSA [7, 10–13]. An increase in central apneas has been reported in some children postoperatively [11]. Complete resolution of sleep apnea in PWS patients is difficult to obtain with adenotonsillectomy alone. Therefore, residual OSA after adenotonsillectomy confirms the complicated and multifactorial nature of the pathogenesis of upper airway obstruction in children with PWS. The key for surgical success is the accurate identification and management of the sites of upper airway obstruction. Drug-induced sleep endoscopy (DISE) is a well-described modality for identification of obstruction sites. To date, there are no studies regarding DISE in children with PWS. The aim of this study was to further understand the OSA pathophysiology in PWS population by analyzing the patterns of airway collapse from DISE with PSG variables and body mass index (BMI).
Materials and methods
Between January 2013 and August 2014, nine consecutive children with PWS underwent DISE. Of the nine children, one had undergone adenotonsillectomy with relapse of OSA 1 year later. The other eight children did not receive any surgeries. This study was approved by the institutional review board of our institution. Data were collected retrospectively. Patients under the age of 18 years were eligible. The BMI was calculated, and the neck circumference was measured. Daytime sleepiness was assessed by the Epworth Sleepiness Scale.
All patients received a standard PSG. Sleep measurements were based on the criteria of the American Academy of Sleep Medicine. The apnea-hypopnea index (AHI) was calculated as the sum of total events (apneas and hypopneas) per hour of sleep. Apnea was defined as a decrease of 90 % or greater from the previous baseline airflow for at least 10 s. Hypopnea was defined as a partial obstructive event with diminution of airflow by more than 30 % from baseline for at least 10 s. It is also associated with oxygen desaturation of 3 % or more or an arousal. The severity of obstructive sleep apnea was classified according to AHI, which defined mild OSA as AHI between 1 and 5, moderate OSA as AHI between 5 and 10, and severe OSA as AHI greater than 10.
DISE was performed by an experienced ENT surgeon in a semi-dark and silent operating room. Patients were placed in a supine position. Both nostrils were topically anesthetized and decongested with lidocaine and phenylephrine 15 min before the procedure. Drug-induced sleep was achieved with intravenous administration of propofol (loading dose of 1 mg/kg, followed by 200–300 μg/kg/min). During the procedure, the anesthesia team helped in monitoring electrocardiography, blood pressure, and oxygen saturation. The target depth of sedation was the absence of a response to verbal stimulation in a normal voice, similar to a Richmond Agitation Sedation Scale of −4. Once the patient has reached a satisfactory level of sedation, a flexible nasal endoscope was used to evaluate the nasal cavity, nasopharynx, velum, oropharynx, tongue base, epiglottis, and larynx.
Intraoperative findings were reported using VOTE classification [14], a method for describing DISE findings. The site, configuration, and degree of obstruction were recorded. The four common obstruction sites are the velum, oropharynx, base of tongue, and epiglottis. The configuration of airway collapse is categorized as antero-posterior, lateral, or concentric. The degree of airway obstruction is sorted as no obstruction (0, <50 %), partial obstruction (1, 50–75 %), and complete obstruction (2, >75 %). The DISE findings were recorded by the author.
Statistical calculations were performed by using SPSS version 17.0 (SPSS, Chicago, Illinois). The associations of AHI and BMI with different patterns of airway obstruction were analyzed using nonparametric Mann-Whitney U test. Descriptive data was presented as mean ± standard deviation. Differences were considered significant if P < 0.05.
Results
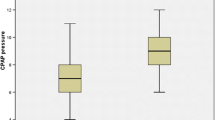
The study population consisted of nine patients, including four males and five females The mean age was 8.72 ± 4.21 years, with a mean BMI of 21.79 ± 5.01 kg/m2. Patient characteristics are listed in Table 1. Although obesity is a major feature of children with PWS, there is only one patient with BMI more than 30. The mean supine AHI was 8.44 ± 6.25. The mean lateral AHI was 2.22 ± 2.05. The mean supine AHI showed at least twice the value of the AHI in lateral position, which defined as positional OSA. All of the patients had positional OSA.
Of all the patients, four out of nine children (44.4 %) had mild OSA, four out of nine children (44.4 %) had moderate OSA, and one out of nine children (11.1 %) had severe OSA as measured by the AHI. The majority of the patients were found to have multilevel obstruction (six out of nine children, 66.6 %). An overview of the distribution of obstruction is shown in Table 2. The velum was the most common site of obstruction (nine out of nine children, 100 %).
Patients with partial or complete anterior-posterior tongue base collapse were associated with a significantly higher AHI (P = 0.016) compared to patients with no anterior-posterior tongue base collapse (Table 3).
No significant association was found between AHI and any other configurations of narrowing at the velum, oropharynx, or epiglottis (Table 3).
No any configurations of airway collapse at the velum, oropharynx, tongue base, or epiglottis showed a significant association with BMI (Table 3).
Discussion
This is the first study to evaluate different patterns of upper airway collapse in children with PWS by DISE. Single-site airway obstruction was observed in three out of nine children with PWS (33.3 %). Multilevel airway obstruction was observed in six out of nine children with PWS (66.6 %). In accordance with previous DISE studies in children and adults with OSA [15–18], our study provided the evidence that the majority of children with PWS had obstruction at multiple sites of the upper airway. The velum was the most common site of obstruction in our study (100 %) as an isolated entity or as part of a multilevel obstruction. In contrast to our study, Seckin et al. [17] reported lateral oropharyngeal collapse as the most common site of obstruction of 82 children with OSA. This difference may be explained by the different disease entity of the two children groups. In our study, only children with PWS were included. In the study of Seckin et al. [17], children with OSA were enrolled, including comorbid conditions such as asthma, seizure disorder, congenital heart disease, autism, sickle cell disease, chronic lung disease, neurofibromatosis, and Down syndrome.
We further analyzed different patterns of airway collapse in children with PWS as seen on DISE with AHI and BMI variables. An analysis of individual collapse patterns revealed that patients with partial or complete anterior-posterior tongue base collapse had significantly higher AHI as compared to patients with no tongue base collapse. Madeline et al. [18] have reported similar findings in their study of adults with OSA, which showed a tongue base collapse associated with higher AHI. Apart from tongue base collapse, no other patterns of airway collapse showed a consistent association with AHI in our results. Children with PWS are generally characterized by weak muscle tone, which may further exacerbate the tongue base collapse. This character could be the reason for the association between tongue base collapse and higher AHI. Therefore, as the disease severity increases, therapies that address tongue base collapse may be considered in children with PWS. No patterns of airway collapse showed a significant association with BMI in our study. However, previous studies reported that complete concentric velum collapse was found to be associated with a higher BMI of adults with OSA [15, 18]. The difference may be explained by the different disease entities of the two studies.
Adenotonsillectomy has traditionally been considered to be effective and improve quality of life in most children with PWS [19]. However, recent studies found that children with PWS who demonstrate severe OSA may not experience complete resolution of sleep apnea after adenotonsillectomy [7, 10–13]. It is also known that results of adenotonsillectomy in certain patient populations, including obese individuals and those with specific comorbidities, such as trisomy 21 (Down) syndrome, cerebral palsy, and craniofacial abnormalities, are suboptimal than in children without these comorbidities [20–22]. Megan et al. [23] used DISE to investigate the possible patterns of airway collapse contributing to residual OSA after adenotonsillectomy in children. They have found that most of the children with suboptimal results after adenotonsillectomy are contributed from tongue base obstruction, primarily due to lingual tonsillar hypertrophy. Their finding emphasized the need of DISE for children with OSA because it may identify the anatomical structures that contribute to obstruction and enable tailored surgical treatment. To date, the complexity of OSA in children with PWS is not fully recognized, with multiple anatomical and systemic contributing factors. DISE may provide a way to tailor better management for OSA in children with PWS.
The potential complications after adenotonsillectomy in children with PWS included hemorrhages, difficult awakening from anesthesia, airway compromised requiring reintubation and/or supplemental oxygen administration, and velopharyngeal dysfunction [10, 13]. Some patients with persisted velopharyngeal dysfunction had structural issues requiring further corrective surgery, such as pharyngeal flap [10]. According to previous studies, the frequency of post-adenotonsillectomy complications in children with PWS ranged from 0 to 80 %, which was higher than general population with OSA [10, 12, 13]. Therefore, careful patient selection for adenotonsillectomy in children with PWS is mandatory to avoid unnecessary morbidity. Victores et al. have reported that nearly all patients with positional OSA (91 %) had at least a partial improvement in the tongue base or epiglottis collapse while in the lateral sleep position [24]. Permut et al. have showed that positional therapy is equivalent to CPAP at normalizing the AHI in patients with positional OSA, with similar effects on sleep quality and nocturnal oxygenation [25]. In our study, all of our patients were positional OSA and a tongue base collapse was associated with higher AHI. Therefore, positional therapy could be a potential therapy for patients with PWS since it may alleviate the severity of tongue base collapse.
This study has some limitations. First, DISE is a subjective assessment, and the results may be biased. However, there are several studies reporting the acceptable consistency of DISE [26–28]. Although, to our knowledge, this is the first study to analyze the patterns of airway collapse from DISE with AHI in children with PWS, the statistical analysis of this study is limited in terms of power owing to the small number of subjects. However, we still found the significant association between tongue base collapse and higher AHI. Larger and more detailed investigations are needed to fully assess the patterns of airway collapse from DISE in children with PWS. Another limitation is the effect of propofol in sleep patterns and in muscle relaxation. Rabelo et al. have observed that propofol significantly increased N3 sleep and totally extinguished REM. However, the main respiratory parameters, AHI and mean SaO2, remained unchanged [29]. Capasso et al. have reported that DISE with propofol group had a significantly increased likelihood of demonstrating complete tongue base obstruction compared to DISE with dexmedetomidine group [30]. In addition, Lin et al. also stated that the use of propofol may cause excessive hypotonia and muscle relaxation resulting in inaccurate airway evaluation [31]. However, Yoon et al. have found that the upper airway collapse during DISE sedated with propofol and dexmedetomidine were in excellent agreement [32]. Although there were diverse results regarding the effect of propofol in airway evaluation, careful use of propofol to prevent oversedation is important.
In conclusion, our results indicate that the majority of children with PWS were found to have multilevel obstruction. The velum was the most common site of obstruction. Partial or complete anterior-posterior tongue base collapse was associated with higher AHI values, which may be explained by the poor muscle tone exacerbating the tongue base collapse. Therapies that address tongue base collapse may be considered. Therefore, positional therapy could be a potential treatment for patients with PWS since it may alleviate the severity of tongue base collapse.
References
Cassidy SB, Schwartz S, Miller JL, Driscoll DJ (2012) Prader-Willi syndrome. Genet Med 14:10–26
Cohen M, Hamilton J, Narang I (2014) Clinically important age-related differences in sleep related disordered breathing in infants and children with Prader-Willi syndrome. PLoS One 9:e101012
Miller J, Wagner M (2013) Prader-Willi syndrome and sleep-disordered breathing. Pediatr Ann 42:200–204
Nixon GM, Brouillette RT (2002) Sleep and breathing in Prader-Willi syndrome. Pediatr Pulmonol 34:209–217
Sedky K, Bennett DS, Pumariega A (2014) Prader Willi syndrome and obstructive sleep apnea: co-occurrence in the pediatric population. J Clin Sleep Med 10:403–409
Nixon GM, Rodda CP, Davey MJ (2011) Longitudinal association between growth hormone therapy and obstructive sleep apnea in a child with Prader-Willi syndrome. J Clin Endocrinol Metab 96:29–33
DeMarcantonio MA, Darrow DH, Gyuricsko E, Derkay CS (2010) Obstructive sleep disorders in Prader-Willi syndrome: the role of surgery and growth hormone. Int J Pediatr Otorhinolaryngol 74:1270–1272
Bizzarri C, Rigamonti AE, Luce A, et al. (2010) Children with Prader-Willi syndrome exhibit more evident meal-induced responses in plasma ghrelin and peptide YY levels than obese and lean children. Eur J Endocrinol 162:499–505
Camfferman D, Lushington K, O’Donoghue F, Doug McEvoy R (2006) Obstructive sleep apnea syndrome in Prader-Willi syndrome: an unrecognized and untreated cause of cognitive and behavioral deficits? Neuropsychol Rev 16:123–129
Crockett DJ, Ahmed SR, Sowder DR, Wootten CT, Chinnadurai S, Goudy SL (2014) Velopharyngeal dysfunction in children with Prader-Willi syndrome after adenotonsillectomy. Int J Pediatr Otorhinolaryngol 78:1731–1734
Meyer SL, Splaingard M, Repaske DR, Zipf W, Atkins J, Jatana K (2012) Outcomes of adenotonsillectomy in patients with Prader-Willi syndrome. Arch Otolaryngol Head Neck Surg 138:1047–1051
Tanna N, Choi SS (2009) Efficacy and safety of adenotonsillectomy for pediatric obstructive sleep apnea in Prader-Willi syndrome. Ann Otol Rhinol Laryngol 118:267–269
Pavone M, Paglietti MG, Petrone A, Crino A, De Vincentiis GC, Cutrera R (2006) Adenotonsillectomy for obstructive sleep apnea in children with Prader-Willi syndrome. Pediatr Pulmonol 41:74–79
Kezirian EJ, Hohenhorst W, de Vries N (2011) Drug-induced sleep endoscopy: the VOTE classification. Eur Arch Otorhinolaryngol 268:1233–1236
Vroegop AV, Vanderveken OM, Boudewyns AN, et al. (2014) Drug-induced sleep endoscopy in sleep-disordered breathing: report on 1,249 cases. Laryngoscope 124:797–802
Koo SK, Choi JW, Myung NS, Lee HJ, Kim YJ, Kim YJ (2013) Analysis of obstruction site in obstructive sleep apnea syndrome patients by drug induced sleep endoscopy. Am J Otolaryngol 34:626–630
Ulualp SO, Szmuk P (2013) Drug-induced sleep endoscopy for upper airway evaluation in children with obstructive sleep apnea. Laryngoscope 123:292–297
Ravesloot MJ, de Vries N (2011) One hundred consecutive patients undergoing drug-induced sleep endoscopy: results and evaluation. Laryngoscope 121:2710–2716
Wong CP, Ng DK, Ma TM, Chau C, Chow PY, Kwok KL (2010) Improvement in quality of life after adenotonsillectomy in a child with Prader Willi syndrome. Sleep Breath 14:167–170
Donnelly LF, Shott SR, LaRose CR, Chini BA, Amin RS (2004) Causes of persistent obstructive sleep apnea despite previous tonsillectomy and adenoidectomy in children with down syndrome as depicted on static and dynamic cine MRI. AJR Am J Roentgenol 183:175–181
Donaldson JD, Redmond WM (1988) Surgical management of obstructive sleep apnea in children with down syndrome. J Otolaryngol 17:398–403
Kotagal S, Gibbons VP, Stith JA (1994) Sleep abnormalities in patients with severe cerebral palsy. Dev Med Child Neurol 36:304–311
Durr ML, Meyer AK, Kezirian EJ, Rosbe KW (2012) Drug-induced sleep endoscopy in persistent pediatric sleep-disordered breathing after adenotonsillectomy. Arch Otolaryngol Head Neck Surg 138:638–643
Victores AJ, Hamblin J, Gilbert J, Switzer C, Takashima M (2014) Usefulness of sleep endoscopy in predicting positional obstructive sleep apnea. Otolaryngol Head Neck Surg 150:487–493
Permut I, Diaz-Abad M, Chatila W, et al. (2010) Comparison of positional therapy to CPAP in patients with positional obstructive sleep apnea. J Clin Sleep Med 6:238–243
Vroegop AV, Vanderveken OM, Wouters K, et al. (2013) Observer variation in drug-induced sleep endoscopy: experienced versus nonexperienced ear, nose, and throat surgeons. Sleep 36:947–953
Kezirian EJ, White DP, Malhotra A, Ma W, McCulloch CE, Goldberg AN (2010) Interrater reliability of drug-induced sleep endoscopy. Arch Otolaryngol Head Neck Surg 136:393–397
Rodriguez-Bruno K, Goldberg AN, McCulloch CE, Kezirian EJ (2009) Test-retest reliability of drug-induced sleep endoscopy. Otolaryngol Head Neck Surg 140:646–651
Rabelo FA, Kupper DS, Sander HH, Fernandes RM, Valera FC (2013) Polysomnographic evaluation of propofol-induced sleep in patients with respiratory sleep disorders and controls. Laryngoscope 123:2300–2305
Capasso R, Rosa T, Tsou, DY et al. (2016) Variable findings for drug-induced sleep endoscopy in obstructive sleep apnea with propofol versus dexmedetomidine. Otolaryngol Head Neck Surg 154(4):765–770
Lin AC, Koltai PJ (2012) Sleep endoscopy in the evaluation of pediatric obstructive sleep apnea. Int J Pediatr 2012:576719
Yoon BW, Hong JM, Hong SL, Koo SK, Roh HJ, Cho KS (2016) A comparison of dexmedetomidine versus propofol during drug-induced sleep endoscopy in sleep apnea patients. Laryngoscope 126:763–767
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or nonfinancial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Funding
No funding was received for this research.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Lan, MC., Hsu, YB., Lan, MY. et al. Drug-induced sleep endoscopy in children with Prader-Willi syndrome. Sleep Breath 20, 1029–1034 (2016). https://doi.org/10.1007/s11325-016-1338-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1338-8