Abstract
Prader-Willi Syndrome (PWS) is a rare genetic disorder characterized by a range of physical, psychological, and physiological abnormalities. It is also distinguished by the high prevalence of obstructive sleep apnea syndrome (OSAS), i.e., repetitive upper airway collapse during sleep resulting in hypoxia and sleep fragmentation. In non-PWS populations, OSAS is associated with a range of neurocognitive and psychosocial deficits. Importantly, these deficits are at least partly reversible following treatment. Given the findings in non-PWS populations, it is possible that OSAS may contribute to neurocognitive and psychosocial deficits in PWS. The present review examines this possibility. While acknowledging a primary contribution from the primary genetic abnormality to central neural dysfunction in PWS, we conclude that OSAS may be an important secondary contributing factor to reduced neurocognitive and psychosocial performance. Treatment of OSAS may have potential benefits in improving neurocognitive performance and behavior in PWS, but this awaits confirmatory investigation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Prader-Willi syndrome (PWS) is a complex, multifaceted, and congenital disorder with protean manifestations, including physical (infantile hypotonia, hypogenitalism, facial dysmorphism, scoliosis, obesity, and short stature with small hands and feet), physiological (hypotonia, low metabolic rate, abnormal sleep, and excessive daytime sleepiness) and psychological (hyperphagia, tantrums, irritability, obsessive-compulsive behavior, low frustration threshold, lethargy, and intellectual impairment) abnormalities (Holm et al., 1993). Most of these abnormalities can be attributed to genetic factors (State & Dykens, 2000). However, and importantly, PWS is often accompanied by obstructive sleep apnea syndrome (OSAS) (Nixon & Brouillette, 2002).
Obstructive sleep apnea syndrome is characterized by the presence of repetitive collapse and obstruction of the upper airway. Discrete obstructive events (>10 seconds) cause either a complete pause (apnea) or a partial reduction (hypopnea) in respiration that leads to acute hypoxia and hypercapnia. As a protective mechanism to maintain blood oxygen levels, obstructive apneas and hypopneas often culminate in arousal from sleep. Morbidly obese patients or those with respiratory muscle weakness or abnormalities of central nervous system respiratory control can also suffer another form of sleep disordered breathing known as sleep hypoventilation, characterized by a sustained pattern of “under breathing,” also associated with hypoxia, and especially hypercapnia, but without discrete respiratory events. The American Academy of Sleep Medicine task force guidelines for the diagnosis and treatment of obstructive sleep apnea suggest that five apneas plus hyponeas per hour of sleep in adults is the minimum threshold for determining OSAS (i.e., apnea-hypopnea index [AHI] >5) (ASDATF, 1998) while Marcus et al. (1992) propose that more than one event per hour is diagnostic of OSAS in children less than 12 years of age.
OSAS in both adults and children is associated with a range of neurocognitive and psychosocial deficits (e.g., memory, learning, attention, executive functioning, withdrawal, aggression, etc.) (Beebe & Gozal, 2002; Blunden, Lushington, & Kennedy, 2001; El-Ad & Lavie, 2005; Engleman, Kingshott, Martin, & Douglas, 2000; Naegele et al., 1998). Over and above any genetic contribution, these findings raise the possibility that OSAS may be an additional contributory factor to reduced neurocognitive and psychosocial performance in PWS.
Prader-Willi syndrome and sleep-disordered breathing
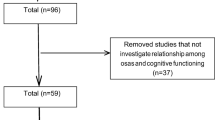
Knowledge about sleep and ventilation in PWS is restricted to a small number of studies and of these only a few have used objective measures of sleep such as PSG. Comparing the frequency of OSAS estimates in the few PSG studies that have been conducted is further complicated by several methodological limitations. These include the reliance on findings from case studies with small subject numbers and evident problems with selection bias, the use in some studies of adult criteria to diagnose OSAS in children and following recent improvements in technology coupled with changes in scoring criteria an increased capacity to now detect OSAS with greater sensitivity. Nevertheless, based on a combined search of PsychInfo and PubMed databases using the term “Prader-Willi” with the words apnea, sleep, or sleepiness and limiting the search to PSG studies (or studies which included a subset of cases with PSG data) which report the frequency of cases with an AHI >5 we identified 17 peer-reviewed publications with a combined total of 103 PWS patients (Clift, Dahlitz, & Parkes, 1994; Doshi & Udwadia, 2001; Harris & Allen, 1996; Hiroe, Inoue, Higami, Suto, & Kawahara, 2000; Kaplan, Fredrickson, & Richardson, 1991; Livingston, Arens, Bailey, Keens, & Ward, 1995; Manni et al., 2001; Nevsimalova et al., 2000; Nixon & Brouillette, 2002; O’Donoghue et al., 2005; Pavone et al., 2006; Richards et al., 1994; Schluter, Buschatz, Trowitzsch, Aksu, & Andler, 1997; Sforza, Krieger, Geisert, & Kurtz, 1991; Vgontzas, Bixler et al., 1996; Vgontzas, Bixler, Kales, & Vela-Bueno, 1995; Vgontzas, Kales et al., 1996). In this literature, sample inspection of cases revealed that 57% (59/103) of PWS patients had OSAS. This estimate is substantially higher than community prevalence estimates based on an AHI >5 of 9% in adult non-PWS women and 24% in men (Duran, Esnaola, Rubio, & Iztueta, 2001). As well, it is higher than prevalence estimates based on PSG evaluation of OSAS in non-PWS children with self-reported habitual snoring of 1–3% (Blunden et al., 2001).
Excessive daytime sleepiness and Prader-Willi syndrome
A cardinal symptom of OSAS is excessive daytime sleepiness. The clinical features of excessive daytime sleepiness include the tendency to stay at rest; the propensity to fall asleep unintentionally during the day, especially in passive situations; and difficulty concentrating (Guilleminault & Brooks, 2001). Although the precise etiology has yet to be fully determined, the fragmentation of sleep by respiratory-evoked arousals is thought to underlie excessive daytime sleepiness in OSAS patients (Philip, Stoohs, & Guilleminault, 1994). The clinical assessment of excessive daytime sleepiness is typically based either on self-report measures of sleepiness-related behavior such as the likelihood of falling asleep in inappropriate situations [e.g., “while stopped at traffic light” from Epworth Sleep Scale (Johns, 1994)] or laboratory-based protocols using PSG to measure sleepiness under varying sleep-demand conditions. The latter includes multiple sleep latency testing during which the patient is given four opportunities across the day to attempt to sleep in bed under conditions of low stimulation and the mean time to sleep onset is recorded (Carskadon, 1993). A mean multiple sleep latency testing of less than 5 minutes is considered clinically significant (ASDATF, 1998).
PWS patients commonly report excessive daytime sleepiness. This is reflected by elevated scores on measures of self-reported sleepiness, a high frequency of daytime napping, and the presence of shortened latencies to sleep onset at night or during the daytime on multiple sleep latency testing (Clift et al., 1994; Harris & Allen, 1996; Helbing-Zwanenburg, Kamphuisen, & Mourtazaev, 1993; Hertz, Cataletto, Feinsilver, & Angulo, 1993; Kaplan et al., 1991; O’Donoghue et al., 2005; Richards et al., 1994; Vela-Bueno et al., 1984; Vgontzas, Bixler et al., 1996; Vgontzas, Kales et al., 1996). Survey results also indicate a high prevalence of self-reported excessive daytime sleepiness in PWS (Boer & Clarke, 1999; S.B. Cassidy, McKillop, & Morgan, 1990; Clarke, Waters, & Corbett, 1989; Greenswag, 1987; Laurance, Brito, & Wilkinson, 1981). In a case review study, for example, Greenswag (1987) reports that excessive sleepiness was documented in 231 of 232 PWS patients while Clarke et al. (1989) report excessive daytime sleepiness on parental self-report in 56 of 61 PWS patients.
Neurocognitive performance in Prader-Will syndrome and non-Prader-Willi syndrome patients with Obstructive Sleep Apnea syndrome
Increasing evidence points to the importance of sleep in cognitive functioning and especially learning and memory. Findings from functional neuroimaging and electrophysiology in humans, and investigation of neuronal activity in animal models suggest that sleep plays a role in neuroplasticity (Hobson & Pace-Schott, 2002; Tononi & Cirelli, 2006). Forebrain and cortical regions are coordinated during sleep and there is now emerging evidence that different stages of sleep are responsible for different forms and stages of learning and memory (Hobson & Pace-Schott, 2002). Investigation into the impact of sleep deprivation on cognitive performance further indicates that executive functioning is especially sensitive to sleep debt, pointing to the importance of sleep in prefrontal cortex function (Harrison & Horne, 2000). Neuroimaging data also indicate that the prefontal cortex is additionally sensitive to the chemical and cortical neural injury arising from the sleep fragmentation and hypoxia of OSAS, which may explain the added cognitive deficits beyond those of memory and learning in that patient group (El-Ad & Lavie, 2005).
In non-PWS populations, OSAS is associated with reduced neurocognitive performance. In both children and adults the neurocognitive domains affected include executive functioning, verbal and performance IQ, verbal, spatial and visual learning, memory, attention and concentration, and executive functioning (Beebe & Gozal, 2002; El-Ad & Lavie, 2005; Engleman et al., 2000; Friedman et al., 2003; Schechter, 2002).
The relative contributions of daytime sleepiness, hypoxia, and sleep fragmentation to neurocognitive deficits in OSAS remain uncertain. Results from correlational analyses in non-PWS adults with OSAS suggests an association between increased excessive daytime sleepiness and reduced neurocognitive performance and impaired social and occupational functioning (especially an increased risk for motor vehicle and industrial accidents) (Grunstein, Stenlof, Hedner, & Sjostrom, 1995; Marrone, Bonsignore, Insalaco, & Bonsignore, 1998; Melamed & Oksenberg, 2002; Noda et al., 1998; Shiomi et al., 2002; Ulfberg, Carter, Talback, & Edling, 1996). Although not well described, results from correlational analyses in non-PWS children with OSAS suggest that elevated excessive daytime sleepiness is associated with an increased frequency of aggression, delinquency, and paradoxically, hyperactivity (Carroll, McColley, Marcus, Curtis, & Loughlin, 1995; Chervin et al., 2002; Gozal & Pope, 2001). However, the magnitude of the correlations in these studies tends to be small and, notably, reduced neurocognitive performance and impaired social and occupational functioning is also present in OSAS patients who do not report excessive daytime sleepiness. Results from multiple regression analyses suggest in both children and adults with OSAS that AHI and nocturnal hypoxemia are predictive of reduced cognitive and psychomotor performance (Cheshire, Engleman, Deary, Shapiro, & Douglas, 1992; Kennedy et al., 2004) but that explanatory power is not increased with the addition of excessive daytime sleepiness (Kim et al., 1997). Indirect evidence of an association between hypoxia and sleep fragmentation and neurocognitive functioning has come from treatment studies with continuous positive airway pressure in adults and adenotonsillectomy in children. In general, treatment is reported to reduce OSAS severity and improve neurocognitive functioning (Gordon & Sanders, 2005; Mitchell & Kelly, 2006).
PWS is accompanied by a range of neurocognitive deficits. The IQ of PWS patients is generally in the low to moderate range (Cassidy and Schwartz, 1998; Gabel et al., 1986), and while reductions in global neurocognitive abilities are commonly noted, greater verbal than performance IQ deficits are reported (Curfs & Fryns, 1992; Curfs, Wiegers, Sommers, Borghgraef, & Fryns, 1991; Gross-Tsur, Landau, Benarroch, Wertman-Elad, & Shalev, 2001). PWS patients also demonstrate multiple severe learning disabilities with a lower academic performance than that indicated by their mental abilities (Gross-Tsur et al., 2001) The most consistent domains reported to show decrement in PWS patients are short-term memory, attention, concentration, and executive functioning (especially abstract thinking) (S. B. Cassidy & Schwartz, 1998; Dykens & Kasari, 1997; Gabel et al., 1986; Gross-Tsur et al., 2001).
Similarities between the neurocognitive domains affected in patients with OSAS and PWS raise the possibility that at least part of the deficits observed in PWS may be attributable to OSAS. Exploration of the relationship between OSAS and neurocognitive functioning in PWS, however, is limited to preliminary results reported by our group (O’Donoghue et al., 2005). In that study, we found contrary to expectations that PWS patients (n=9) with more severe OSAS, i.e., a higher AHI and a lower nocturnal oxygen nadir, tend to have higher global IQ (r=0.25 and r=−0.62 respectively). While this may be a chance finding, we further found that PWS patients with a higher BMI also tend to have a higher AHI and a lower nocturnal oxygen nadir (r= 0.62 and −0.87, respectively). In addition, and of note, they also had a higher Global IQ (r = 0.75). Obesity is a known risk factor for OSAS (Grunstein & Wilcox, 1994), but is not normally related to IQ. However, the profile of our PWS patients was such that more intelligent patients were also engaged in less supervised activities and, hence, had a greater opportunity to engage in food-foraging behavior. Given these two factors, we propose that obesity may be confounding the relationship between OSAS and neurocognitive performance. This is partly supported by exploratory partial correlation analysis in which after controlling for BMI, as predicted, a higher AHI was associated with a lower global IQ (r=−0.40); conversely, after controlling for BMI, little association was observed between nocturnal oxygen nadir and global IQ (r=−0.02). The proposed post-hoc interpretation requires confirmation in larger subject numbers than those available in our previous study. Nonetheless, based on previous findings in non-PWS populations, we propose that OSAS is likely to contribute to neurocognitive deficits in PWS, but that increased food-seeking behavior, and thus obesity, may be a confounding variable.
Psychosocial functioning in Prader-Willi syndrome and Non-Prader-Willi syndrome obstructive sleep apnea syndrome patients
In non-PWS adults, OSAS severity is associated with increased anxiety, distractibility, confusion, irritability, physical and general complaints, depressed mood, higher emotional reactivity, and reduced energy (D’Ambrosio, Bowman, & Mohsenin, 1999; Day, Gerhardstein, Lumley, Roth, & Rosenthal, 1999; Kales et al., 1985; Sanner et al., 2000). In non-PWS children, OSAS is further associated with reduced academic performance and increased problematic behavior (Spahis, 1994; Urschitz et al., 2003).
Psychosocial deficits similar to those reported in non-PWS OSAS populations are also noticeable in PWS with OSAS. While infants and young children with PWS are not noted for exhibiting problematic behavior, older children and adults with PWS are reported to have difficulty with behavior regulation, usually coinciding with the onset of hyperphagia, (although not all problem behaviors are related to food) (Dykens & Kasari, 1997). Some studies have emphasized the behavioral uniqueness of PWS patients compared to groups with other forms of genetic mental retardation. Compared to patients with either Down syndrome or nonspecific mental retardation, Dykens and Kasari (1997) report that PWS patients have a higher incidence of tantrums, stubbornness and difficulties regulating attention, while Einfeld et al. (1996) report that PWS children and adolescents exhibit more frequent and a wider range of problematic behaviors with a greater percentage in the clinically impaired range. Dykens and Rosner (1999) further report that PWS patients tend to be impatient with a low tolerance to frustration, while Einfeld et al. (1999) report more disturbed behavior compared to controls, especially antisocial behavior.
The literature examining the relationship in PWS between OSAS symptoms and psychosocial functioning is limited. Richdale et al. (1999) report a positive correlation between excessive daytime sleepiness severity and increased problematic behavior, while O’Donoghue et al. (2005) report that OSAS severity was positively correlated with increased daytime inactivity/sleepiness, autistic behavior, and impulsiveness. Indirect support of an association has come from treatment studies. Clift et al. (1994) successfully treated five PWS patients with continuous positive airway pressure, noting significant gains in behavior. Nixon and Brouillette (2002) report a single-case study of a PWS child treated with adenotonsillectomy, with subsequent improvements in AHI (reduction from 100 to 2.8), daytime sleepiness and behavior. These latter two studies raise the possibility that treatment of OSAS in PWS, for example with continuous positive airway pressure in adults and adenotonsillectomy in children, may produce gains not only in sleep quality but also daytime functioning.
Directions and issues for future research
Previous research suggests that sleep problems are common in PWS, as are neurocognitive and behavioral deficits. While it is acknowledged that the genetic disorder, per se, in PWS may explain a substantial portion of these deficits, the additional burden of a sleep disorder should not be dismissed. Clinical approaches that can improve the sleep quality of PWS patients may provide an additional benefit through the reduction of problematic behavior and an increase in neurocognitive functioning.
Future research in this area, however, is not without challenges. The major obstacle to exploring PWS sleep deficits is in filtering through the complex, interactive and overlapping expressions of this disorder. There are obvious difficulties in distinguishing neurocognitive and behavioral abnormalities due to poor sleep, from those related to genetically-determined factors.
Further difficulties lie in the low incidence of this syndrome and the limited number of PWS patients available to participate in research. To date, most studies have employed relatively small numbers of PWS patients and have usually combined both children and adults. Another confounding factor is that few studies disclose the criteria by which they determine if a sleep-related respiratory event is due to upper airway obstruction or has a central neurological origin, making the interpretation of the findings difficult. It is also difficult to test these individuals within a laboratory/hospital environment. The emotional disposition of PWS patients limits their ability to undergo lengthy and complex measurements such as polysomnography.
Notwithstanding the above difficulties it should be feasible to ascertain the contribution of sleep disordered breathing to the neurocognitive and psychosocial abnormalities in PWS using a randomized controlled trial of continuous positive airway pressure treatment among carefully characterized patients with OSAS. To be successful such a study would require prior discussion with PWS families and their self-help organizations, and the recruitment of research staff knowledgeable and experienced in the management of PWS patients. To achieve sufficient statistical power, it is likely that patients would need to be recruited from multiple centers.
The promise of further research in this area is that it may ultimately lead to improvements in sleep quality, behavior and neurocognitive performance in a group of people already subjected to a wide array of detrimental health and quality of life issues. Any alleviation of these problems would be of considerable benefit, not only to patients but, in addition, caregivers and family members whose present role in the support of PWS patients can only be described as extensive.
References
ASDATF. (1998). The Chicago criteria for measurements, definitions, and severity of sleep related breathing disorders in adults. New Orleans, LA: Association of Professional Sleep Societies Conference.
Beebe, D. W., & Gozal, D. (2002). Obstructive sleep apnea and the prefrontal cortex: towards a comprehensive model linking nocturnal upper airway obstruction to daytime cognitive and behavioral deficits. Journal of Sleep Research, 11(1), 1–16.
Blunden, S., Lushington, K., & Kennedy, D. (2001). Cognitive and behavioural performance in children with sleep-related obstructive breathing disorders. Sleep Medicine Reviews, 5(6), 447–461.
Boer, H., & Clarke, D. (1999). Development and behaviour in genetic syndromes: Prader-Willi syndrome. Journal of Applied Research in Intellectual Disabilities, 12(4), 294–301.
Carroll, J. L., McColley, S. A., Marcus, C. L., Curtis, S., & Loughlin, G. M. (1995). Inability of clinical history to distinguish primary snoring from obstructive sleep apnea syndrome in children. Chest, 108(3), 610–618.
Carskadon, M. A. (1993). Evaluation of excessive daytime sleepiness. Neurophysiologie Clinique, 23(1), 91–100.
Cassidy, S. B., McKillop, J. A., & Morgan, W. J. (1990). Sleep disorders in Prader-Willi syndrome. Dysmorphology and Clinical Genetics, 4(1), 13–17.
Cassidy, S. B., & Schwartz, S. (1998). Prader-Willi and Angelman syndromes. Disorders of genomic imprinting. Medicine (Baltimore), 77(2), 140–151.
Chervin, R. D., Archbold, K. H., Dillon, J. E., Panahi, P., Pituch, K. J., Dahl, R. E., et al. (2002). Inattention, hyperactivity, and symptoms of sleep-disordered breathing. Pediatrics, 109(3), 449–456.
Cheshire, K., Engleman, H., Deary, I., Shapiro, C., & Douglas, N. J. (1992). Factors impairing daytime performance in patients with sleep apnea/hypopnea syndrome. Archives of Internal Medicine, 152(3), 538–541.
Clarke, D. J., Waters, J., & Corbett, J. A. (1989). Adults with Prader-Willi syndrome: Abnormalities of sleep and behaviour. Journal of the Royal Society of Medicine, 82, 21–24.
Clift, S., Dahlitz, M., & Parkes, J. D. (1994). Sleep apnoea in the Prader-Willi syndrome. Journal of Sleep Research, 3(2), 121–126.
Curfs, L. M., & Fryns, J. P. (1992). Prader-Willi syndrome: a review with special attention to the cognitive and behavioral profile. Birth Defects Original Article Series, 28(1), 99–104.
Curfs, L. M., Wiegers, A. M., Sommers, J. R., Borghgraef, M., & Fryns, J. P. (1991). Strengths and weaknesses in the cognitive profile of youngsters with Prader-Willi syndrome. Clinical Genetics, 40(6), 430–434.
D’Ambrosio, C., Bowman, T., & Mohsenin, V. (1999). Quality of life in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure—a prospective study. Chest, 115(1), 123–129.
Day, R., Gerhardstein, R., Lumley, A., Roth, T., & Rosenthal, L. (1999). The behavioral morbidity of obstructive sleep apnea. Progress in Cardiovascular Diseases, 41(5), 341–354.
Doshi, A., & Udwadia, Z. (2001). Prader-Willi syndrome with sleep disordered breathing: effect of two years nocturnal CPAP. Indian Journal of Chest Diseases and Allied Sciences, 43(1), 51–53.
Duran, J., Esnaola, S., Rubio, R., & Iztueta, A. (2001). Obstructive sleep apnea-hypopnea and related clinical features in a population-based sample of subjects aged 30 to 70 yr. American Journal of Respiratory and Critical Care Medicine, 163(3 Pt 1), 685–689.
Dykens, E. M., & Kasari, C. (1997). Maladaptive behavior in children with Prader-Willi syndrome, Down syndrome, and nonspecific mental retardation. American Journal of Mental Retardation, 102(3), 228–237.
Dykens, E. M., & Rosner, B. A. (1999). Refining behavioral phenotypes: personality-motivation in Williams and Prader-Willi syndromes. American Journal of Mental Retardation, 104(2), 158–169.
Einfeld, S., Tonge, B., Turner, G., Parmenter, T., & Smith, A. (1996). Longitudinal course of behavioural and emotional problems of young persons with Prader-Willi, Fragile X, Williams and Down syndromes. Journal of Intellectual & Developmental Disability, 24(4), 349–354.
Einfeld, S. L., Smith, A., Durvasula, S., Florio, T., & Tonge, B. J. (1999). Behavior and emotional disturbance in Prader-Willi syndrome. American Journal of Medical Genetics, 82(2), 123–127.
El-Ad, B., & Lavie, P. (2005). Effect of sleep apnea on cognition and mood. International Review of Psychiatry, 17(4), 277–282.
Engleman, H. M., Kingshott, R. N., Martin, S. E., & Douglas, N. J. (2000). Cognitive function in the sleep apnea/hypopnea syndrome (SAHS). Sleep, 23(Suppl 4), S102–108.
Friedman, B. C., Hendeles-Amitai, A., Kozminsky, E., Leiberman, A., Friger, M., Tarasiuk, A., et al. (2003). Adenotonsillectomy improves neurocognitive function in children with obstructive sleep apnea syndrome. Sleep, 26(8), 999–1005.
Gabel, S., Tarter, R. E., Gavaler, J., Golden, W. L., Hegedus, A. M., & Maier, B. (1986). Neuropsychological capacity of Prader-Willi children: general and specific aspects of impairment. Applied Research in Mental Retardation, 7(4), 459–466.
Gordon, P., & Sanders, M. H. (2005). Sleep.7: positive airway pressure therapy for obstructive sleep apnoea/hypopnoea syndrome. Thorax, 60(1), 68–75.
Gozal, D., & Pope, D. W., Jr. (2001). Snoring during early childhood and academic performance at ages thirteen to fourteen years. Pediatrics, 107(6), 1394–1399.
Greenswag, L. R. (1987). Adults with Prader-Willi syndrome: a survey of 232 cases. Developmental Medicine and Child Neurology, 29(2), 145–152.
Gross-Tsur, V., Landau, Y. E., Benarroch, F., Wertman-Elad, R., & Shalev, R. S. (2001). Cognition, attention, and behavior in Prader-Willi syndrome. Journal of Child Neurology, 16(4), 288–290.
Grunstein, R. R., Stenlof, K., Hedner, J. A., & Sjostrom, L. (1995). Impact of self-reported sleep-breathing disturbances on psychosocial performance in the Swedish Obese Subjects (SOS) Study. Sleep, 18(8), 635–643.
Grunstein, R. R., & Wilcox, I. (1994). Sleep-disordered breathing and obesity. Baillieres Clinical Endocrinology and Metabolism, 8(3), 601–628.
Guilleminault, C., & Brooks, S. N. (2001). Excessive daytime sleepiness: a challenge for the practising neurologist. Brain, 124(Pt 8), 1482–1491.
Harris, J. C., & Allen, R. P. (1996). Is excessive daytime sleepiness characteristic of Prader-Willi syndrome? The effects of weight change. Archives of Pediatrics and Adolescent Medicine, 150(12), 1288–1293.
Harrison, Y., & Horne, J. A. (2000). The impact of sleep deprivation on decision making: A review. Journal of Experimental Psychology. Applied, 6(3), 236–249.
Helbing-Zwanenburg, B., Kamphuisen, H. A., & Mourtazaev, M. S. (1993). The origin of excessive daytime sleepiness in the Prader-Willi syndrome. Journal of Intellectual Disability Research, 37(Pt 6), 533–541.
Hertz, G., Cataletto, M., Feinsilver, S. H., & Angulo, M. (1993). Sleep and breathing patterns in patients with Prader Willi syndrome (PWS): effects of age and gender. Sleep, 16(4), 366–371.
Hiroe, Y., Inoue, Y., Higami, S., Suto, Y., & Kawahara, R. (2000). Relationship between hypersomnia and respiratory disorder during sleep in Prader-Willi syndrome. Journal of Neuropsychiatry and Clinical Neurosciences, 54(3), 323–325.
Hobson, J. A., & Pace-Schott, E. F. (2002). The cognitive neuroscience of sleep: neuronal systems, consciousness and learning. Natural Review of Neuroscience, 3(9), 679–693.
Holm, V. A., Cassidy, S. B., Butler, M. G., Hanchett, J. M., Greenswag, L. R., Whitman, B. Y., et al. (1993). Prader-Willi syndrome: consensus diagnostic criteria. Pediatrics, 91(2), 398–402.
Johns, M. W. (1994). Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep, 17(8), 703–710.
Kales, A., Caldwell, A. B., Cadieux, R. J., Vela-Bueno, A., Ruch, L. G., & Mayes, S. D. (1985). Severe obstructive sleep apnea–II: Associated psychopathology and psychosocial consequences. Journal of Chronic Diseases, 38(5), 427–434.
Kaplan, J., Fredrickson, P. A., & Richardson, J. W. (1991). Sleep and breathing in patients with the Prader-Willi syndrome. Mayo Clinic Proceedings, 66(11), 1124–1126.
Kennedy, J. D., Blunden, S., Hirte, C., Parsons, D. W., Martin, A. J., Crowe, E., et al. (2004). Reduced neurocognition in children who snore. Pediatric Pulmonology, 37(4), 330–337.
Kim, H. C., Young, T., Matthews, C. G., Weber, S. M., Woodward, A. R., & Palta, M. (1997). Sleep-disordered breathing and neuropsychological deficits. A population-based study. American Journal of Respiratory and Critical Care Medicine, 156(6), 1813–1819.
Laurance, B. M., Brito, A., & Wilkinson, J. (1981). Prader-Willi Syndrome after age 15 years. Archives of Disease in Childhood, 56(3), 181–186.
Livingston, F. R., Arens, R., Bailey, S. L., Keens, T. G., & Ward, S. L. (1995). Hypercapnic arousal responses in Prader-Willi syndrome. Chest, 108(6), 1627–1631.
Manni, R., Politini, L., Nobili, L., Ferrillo, F., Livieri, C., Veneselli, E., et al. (2001). Hypersomnia in the Prader Willi syndrome: clinical-electrophysiological features and underlying factors. Clinical Neurophysiology, 112(5), 800–805.
Marcus, C. L., Omlin, K. J., Basinki, D. J., Bailey, S. L., Rachal, A. B., Von Pechmann, W. S., et al. (1992). Normal polysomnographic values for children and adolescents. American Review of Respiratory Disease, 146(5 Pt 1), 1235–1239.
Marrone, O., Bonsignore, M. R., Insalaco, G., & Bonsignore, G. (1998). What is the evidence that obstructive sleep apnoea is an important illness? Monaldi Archives for Chest Disease, 53(6), 630–639.
Melamed, S., & Oksenberg, A. (2002). Excessive daytime sleepiness and risk of occupational injuries in non-shift daytime workers. Sleep, 25(3), 315–322.
Mitchell, R. B., & Kelly, J. (2006). Long-term changes in behavior after adenotonsillectomy for obstructive sleep apnea syndrome in children. Otolaryngology—Head and Neck Surgery, 134(3), 374–378.
Naegele, B., Pepin, J. L., Levy, P., Bonnet, C., Pellat, J., & Feuerstein, C. (1998). Cognitive executive dysfunction in patients with obstructive sleep apnea syndrome (OSAS) after CPAP treatment. Sleep, 21(4), 392–397.
Nevsimalova, S., Vankova, J., Sonka, K., Faraco, J., Rogers, W., Overeem, S., et al. (2000). [Hypocretin (orexin) deficiency in narcolepsy-cataplexy]. Sbornik Lekarsky, 101(4), 381–386.
Nixon, G. M., & Brouillette, R. T. (2002). Sleep and breathing in Prader-Willi syndrome. Pediatric Pulmonology, 34(3), 209–217.
Noda, A., Yagi, T., Yokota, M., Kayukawa, Y., Ohta, T., & Okada, T. (1998). Daytime sleepiness and automobile accidents in patients with obstructive sleep apnea syndrome. Journal of Neuropsychiatry and Clinical Neurosciences, 52(2), 221–222.
O’Donoghue, F. J., Camfferman, D., Kennedy, J. D., Martin, A. J., Couper, T., Lack, L. D., et al. (2005). Sleep-disordered breathing in Prader-Willi syndrome and its association with neurobehavioral abnormalities. Journal of Perinatology, 147(6), 823–829.
Pavone, M., Paglietti, M. G., Petrone, A., Crino, A., De Vincentiis, G. C., & Cutrera, R. (2006). Adenotonsillectomy for obstructive sleep apnea in children with Prader-Willi syndrome. Pediatric Pulmonology, 41(1), 74–79.
Philip, P., Stoohs, R., & Guilleminault, C. (1994). Sleep fragmentation in normals: a model for sleepiness associated with upper airway resistance syndrome. Sleep, 17(3), 242–247.
Richards, A., Quaghebeur, G., Clift, S., Holland, A., Dahlitz, M., & Parkes, D. (1994). The upper airway and sleep apnoea in the Prader-Willi syndrome. Clinical Otolaryngology, 19(3), 193–197.
Richdale, A. L., Cotton, S., & Hibbit, K. (1999). Sleep and behaviour disturbance in Prader-Willi syndrome: a questionnaire study. Journal of Intellectual Disability Research, 43(Pt 5), 380–392.
Sanner, B. M., Klewer, J., Trumm, A., Randerath, W., Kreuzer, I., & Zidek, W. (2000). Long-term treatment with continuous positive airway pressure improves quality of life in obstructive sleep apnoea syndrome. European Respiratory Journal, 16(1), 118–122.
Schechter, M. S. (2002). Technical report: diagnosis and management of childhood obstructive sleep apnea syndrome. Pediatrics, 109(4), e69.
Schluter, B., Buschatz, D., Trowitzsch, E., Aksu, F., & Andler, W. (1997). Respiratory control in children with Prader-Willi syndrome. European Journal of Pediatric Surgery, 156(1), 65–68.
Sforza, E., Krieger, J., Geisert, J., & Kurtz, D. (1991). Sleep and breathing abnormalities in a case of Prader-Willi syndrome. The effects of acute continuous positive airway pressure treatment. Acta Paediatrica Scandinavica, 80(1), 80–85.
Shiomi, T., Arita, A. T., Sasanabe, R., Banno, K., Yamakawa, H., Hasegawa, R., et al. (2002). Falling asleep while driving and automobile accidents among patients with obstructive sleep apnea-hypopnea syndrome. Journal of Neuropsychiatry and Clinical Neurosciences, 56(3), 333–334.
Spahis, J. (1994). Sleepless nights: obstructive sleep apnea in the pediatric patient. Pediatric Nursing, 20(5), 469–472.
State, M. W., & Dykens, E. M. (2000). Genetics of childhood disorders: XV. Prader-Willi syndrome: genes, brain, and behavior. Journal of the American Academy of Child and Adolescent Psychiatry, 39(6), 797–800.
Tononi, G., & Cirelli, C. (2006). Sleep function and synaptic homeostasis. Sleep Medicine Review, 10(1), 49–62.
Ulfberg, J., Carter, N., Talback, M., & Edling, C. (1996). Excessive daytime sleepiness at work and subjective work performance in the general population and among heavy snorers and patients with obstructive sleep apnea. Chest, 110(3), 659–663.
Urschitz, M. S., Guenther, A., Eggebrecht, E., Wolff, J., Urschitz-Duprat, P. M., Schlaud, M., et al. (2003). Snoring, intermittent hypoxia and academic performance in primary school children. American Journal of Respiratory and Critical Care Medicine, 168(4), 464–468.
Vela-Bueno, A., Kales, A., Soldatos, C. R., Dobladez-Blanco, B., Campos-Castello, J., Espino-Hurtado, P., et al. (1984). Sleep in the Prader-Willi syndrome. Clinical and polygraphic findings. Archives of Neurology, 41(3), 294–296.
Vgontzas, A. N., Bixler, E. O., Kales, A., Centurione, A., Rogan, P. K., Mascari, M., et al. (1996). Daytime sleepiness and REM abnormalities in Prader-Willi syndrome: evidence of generalized hypoarousal. International Journal of Neuroscience, 87(3–4), 127–139.
Vgontzas, A. N., Bixler, E. O., Kales, A., & Vela-Bueno, A. (1995). Prader-Willi syndrome: effects of weight loss on sleep-disordered breathing, daytime sleepiness and REM sleep disturbance. Acta Paediatrica, 84(7), 813–814.
Vgontzas, A. N., Kales, A., Seip, J., Mascari, M. J., Bixler, E. O., Myers, D. C., et al. (1996). Relationship of sleep abnormalities to patient genotypes in Prader- Willi syndrome. American Journal of Medical Genetics, 67(5), 478–482.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Camfferman, D., Lushington, K., O’Donoghue, F. et al. Obstructive Sleep Apnea Syndrome in Prader-Willi Syndrome: An Unrecognized and Untreated Cause of Cognitive and Behavioral Deficits?. Neuropsychol Rev 16, 123–129 (2006). https://doi.org/10.1007/s11065-006-9010-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-006-9010-x