Abstract
Background
Oral appliances are increasingly advocated as a treatment option for obstructive sleep apnea (OSA). However, it is not clear how the different designs influence treatment efficacy in children. The aim of this study was to investigate the effects of twin block (TB) appliance on children with OSA and mandibular retrognathia.
Methods
A total of 46 children (31 males, 15 females, aged 9.7 ± 1.5 years, BMI: 18.1 ± 1.04 kg/m2) diagnosed with mandibular retrognathia and OSA by polysomnography (PSG) and with no obesity or adenotonsillar hypertrophy were recruited for the study. Patients in the treatment group were instructed to wear the twin block oral appliance full time for an average of 10.8 months. The efficacy of treatment was determined by monitoring the PSG and cephalometric changes before and after appliance removal. Data were analyzed using paired t test.
Results
Results showed an improvement in patient's facial profile after treatment with the TB appliance. The average AHI index decreased from 14.08 ± 4.25 to 3.39 ± 1.86 (p < 0.01), and the lowest SaO2 increased from 77.78 ± 3.38 to 93.63 ± 2.66 (p < 0.01). Cephalometric measurements showed a significant increase in the superior posterior airway space, middle airway space, SNB angle and facial convexity which indicate an enhancement in mandibular growth, and reduction in the soft palate length.
Conclusions
This preliminary study suggests that twin block appliance may improve the patient's facial profile and OSA symptoms in a group of carefully selected children presented with both OSA and mandibular retrognathia symptoms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstructive sleep apnea (OSA) is described as a disordered breathing during sleep with abnormal intermittent complete or partial obstruction which disrupt normal ventilations. It is the most severe form in the continuum of obstructive breathing sleep disorder [1]. Children with this type of disorder usually exhibit daytime symptoms including cognitive, growth, behavioral, cardiac abnormalities [1–3], and sometimes life-threatening problems such as pulmonary hypertension [4]. Different reports suggested that the prevalence of OSA in children is between 1 and 6 % [1, 4, 5]. However, the lack of observer at home might lead to underestimating the prevalence of OSA in children, since most children sleep in their own rooms. In countries like China, the discrepancy is even greater because the birth control policy does not allow families to have more than one child, which eliminates one of the possible source of observers—siblings sleeping in the same room.
There is currently no consensus on the best method of managing OSA in childhood due to the multifactorial nature of OSA. Kaditis proposed an algorithm for the diagnosis and treatment of this disorder [6]. Sleep apnea should be suspected when parents report relevant symptoms or when there are abnormalities that predispose to OSA such as adenotonsillar hypertrophy, obesity, craniofacial anomalies, or neuromuscular disorders. Children with adenotonsillar hypertrophy associated with OSA are usually treated by adenotonsillectomy (ATE). However, patients may not respond satisfactorily with reduction in symptoms due to other underlying factors. A study carried out in 2007 showed that 47 % of the children still suffered from abnormal sleep after ATE [7]. Moreover, ATE carries potential complications such as pain, local bleeding, vomiting, even sometimes velopharyngeal incompetence and nasopharyngeal stenosis. In extreme cases, mortality may result after surgery [5]. The use of continuous positive airway pressure (CPAP) is thought to be the most effective treatment for adult OSA [8], but the application of CPAP in children faces the challenge of low patient compliance and unwanted craniofacial changes after prolonged use of the appliance [9–12].
In adulthood, oral appliance (OA), with its noninvasive nature, is increasingly recognized as an effective and safe choice towards the mild or moderate form of OSA [11–18]. Among the various designs of OA, the soft palate lifters are no longer used; the tongue retainer devices are used only when existing dental reasons hamper other choices; the mandible advancement device (MAD) is by far the most commonly used appliance in treating OSA [12]. Given the consensus that the pharyngeal narrowing or occlusion is conducted by both anatomical factors and physiological factors, the MAD may be able to treat OSA effectively by moving the mandible forward to enlarge the airway and reduce propensity for upper airway collapse [12, 19]. Studies in the adults also indicated that MAD has less or similar effect in treating OSA as CPAP does, but better tolerated by patients [11, 13, 16]. In children, several studies suggested that certain craniofacial abnormities, including retropositioned mandible, was highly linked to children with sleep disorder breathing (SDB) [6, 20–23]. Villa et al. reported on a group of 19 children with symptoms of OSA and malocclusion treated with an oral appliance. The authors found that in 50 % of the subjects, the main respiratory symptom resolved, and the other 50 % had reduced symptom. The authors concluded that treatment of OSA with MAD is effective and well tolerated in children [16].
Twin block (TB) is a kind of oral functional appliance used for early treatment of children with mandibular retrognathia. With its effect of the forward position of the mandible, TB may be a suitable oral appliance to treat children with OSA [18]. Until now, there is little research targeting on the use of this appliance to treat children with OSA. The aim of this preliminary study was to make an initial assessment of the efficacy and tolerance of TB in treating pediatric patients with OSAs accompanied by mandibular retrognathia.
Materials and methods
Study population and design
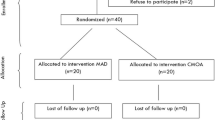
Forty-six patients were recruited from the Department of Orthodontics, School of Stomatology, Wuhan University, China. The inclusion criteria includes: patients who were in category two or three of the cervical vertebrae maturation indices [24], which indicated that patients have not reached the peak pubertal growth spurt; patients who had mandibular retrognathia determined clinically as well as with the aid of cephalometric radiographs (ANB >3°; SNB <80°; incisor overjet >3 mm); patients who had snoring habit reported by their parents and an OSA (apnea/hypopnea index (AHI) >1/h, a criteria which is defined and used by previous articles[16, 25]). The exclusion criteria included patients with acute upper airway infection, adenotonsillar hypertrophy, body mass index above cut off points of overweight which was announced by an international survey [26], or AHI ≤1/h were rejected from the study. The final study group consisted of 46 patients (aged 9.7 ± 1.5 years, BMI: 18.1 ± 1.04 kg/m2), and among them were 31 males and 15 females.
A customized twin block was made for each patient. The degree of mandibular advancement was determined by a wax check bite recording the maximum mandible protrusion within the patient's comfort, according to a previous study [27]. In this study, patients' mandibles were protruded so that the lower incisors reached an edge-to-edge relationship to the upper incisors within comfort. Patients were instructed to wear the appliance full time except for mealtime and return for check up every month. The TB treatment ended 1 month after patient's mandible had reached the designed position, which meant that when the appliance was taken off, the mandible was unable to move backwards and remained with ease in the same position as the appliance was in situ. A second or posttreatment cephalometric radiograph and polysomnography (PSG) were taken immediately after the TB treatment, and the results were compared to the pretreatment data. The treatment protocol was approved by the ethics committee of the School of Stomatology, Wuhan University, and all parents gave written informed consent.
Twin block appliance
Acrylic resin Twin block appliances were fabricated by specially trained laboratory technicians. The removable maxillary appliance was retained with clasps on the upper premolars and molars or in between, while the mandibular removable appliance was retained with clasps on the lower premolars and molars or in between. The inclined planes were interlocked at approximately 70° to the occlusal plane (Fig. 1). The mandible was guided to protrude forward by the inclined planes, and patients were instructed to wear the TB appliance for 24 h every day except for mealtime.
Polysomnography
Attended polysomnography was performed in a sleep laboratory on all patients before and after treatment with the TB appliance using the Sandman Elite (Puritan Bennett, USA). Data including snoring, two-channel electroencephalogram (C3–A2, C4–A1), airflow, electrooculogram, electrocardiogram, and a submental electromyogram were recorded. Arterial oxygen saturation (SaO2) was also recorded by a pulse oximeter. Apnea was defined as a complete interruption of airflow that lasts at least two breath periods, while hypopnea was defined as ≥50 % reduction of airflow with arousal and/or >3 % drop in SaO2, based on previous publication [28]
Cephalometry
The pre and posttreatment cephalometric radiographs were taken in natural head position. Airway-related values including soft palate length (SPL), superior posterior airway space (SPAS), middle airway space (MAS), and inferior airway space (IAS) were measured. A protocol for airway measurements established in 1994 was followed [29]. The sella-nasion-A point (SNA) angle, sella-nasion-B point (SNB) angle, and facial convexity (the angle of a line through soft tissue glabellum–subnasale and a line through subnasale–soft tissue pogonion) were recorded (Fig. 2). All tracings were done by one investigator twice, and the mean value of the two readings was adopted. The method error was measured using the Dahlberg's formula \( \sqrt{{\sum {\frac{{{d^2}}}{2n }} }} \) on ten randomly selected cephalograms. The linear method error was found to be no more than 0.6 mm, and the angular method error was less than 0.9°
Landmarks and measurements: S (sella), N (nasion), G' (soft tissue glabellum), Sn (subnasale), Pg' (soft tissue pogonion), A (A point), B (B point), PNS (posterior nasal spine), P (tip of the soft palate), Go (gonion). 1 SPAS (superior posterior airway space, airway thickness along a line parallel to Go–B plane through the midpoint of PNS–P line), 2 MAS (middle airway space, airway thickness along a line parallel to Go–B plane through P), 3 IAS (inferior airway space, airway thickness along Go–B plane or its extension), 4 SPL (soft palatal length, the linear distance between P and PNS), 5 SNA (angle of a line through sella–nasion and a line through nasion–A point), 6 SNB (angle of a line through sella–nasion and a line through nasion–B point), 7 Facial convexity (angle of a line through G'–Sn and a line through Sn–Pg')
Statistical analysis
Data was computed using the SPSS version 19.0 software program (Chicago, IL, USA). A two-tailed paired student's t test was used to compare the pretreatment and posttreatment data. The significance level was set at p = 0.05.
Results
All recruited patients completed the clinical trial. After an average of 10.8 months of treatment with the TB appliance, all patients exhibited an edge-to-edge incisor relationship.
Polysomnography readings
Table 1 compares the pre and posttreatment AHI, the lowest SaO2, and the mean oxygen saturation readings for the studied patients.
The average AHI value dropped 75.9 % after the TB treatment. The paired t test indicated that the differences were statistically significant (p < .01).
The lowest SaO2 level increased 20.4 % after treatment with TB appliance. The difference was found to be statistically significant (p < .01), while no statistical influence was found in mean SaO2.
Cephalometric measurements
Table 2 shows the cephalometric measurements related to the airway and the profile. Significant increase in the SPAS and MAS were found. No significant change was found in the IAS. Reduction in SPL was noted after treatment with the TB appliance.
A forward movement of the mandible was achieved after treatment. The SNB angle increased (p < .01) together with an improvement in the facial convexity, indicating a favorable forward growth pattern.
Discussion
The effect of oral appliance in adult patients with OSA has been reported by several investigators [11, 27, 30]. However, few studies have focused on the effects of oral appliance in children with OSA and mandibular retrognathia [16]. The present study suggests that twin block appliance may be an alternative choice for treatment of children with OSA and retrognathia. Patients in this clinical trial had lower AHI score and an increase in the lowest SaO2 after treatment. The fact that none of the patients abandoned the therapy indicates that the TB appliance was well tolerated by children, which is in agreement of other studies [16, 27].
In adult patients, the MAD including the TB appliance has become a preferred choice for treatment of OSA. However, unfavorable dentoalveolar changes and soft tissue discomfort have discouraged adult patients from using MAD [15]. The situation in children is quite different. The side effect of dentoalveolar changes is beneficial to children with retrognathia because protrusion of the mandible helps in reducing the overjet and overbite as well as improving the facial profile [16]. The soft tissue is also better tolerated by children than adults. In addition, unlike adults, children may not need to wear the MAD for lifetime to prevent OSA as in adults, since mandibular growth stimulated by MAD may remove the possible etiology of OSA. In this study, all patients were found to have an improved facial profile change and dental relationship after treatment with the TB appliance. Moreover, a recent review suggested that SDB could induce craniofacial abnormalities which in turn worsen the OSA symptoms [21, 22]. This is another advantage of treating pediatric OSA with retrognathia by orthodontic treatment.
The result of this study showed a significant change in AHI and SaO2 after treatment. The reduction in AHI (75.9 %) and the improvement of lowest SaO2 (20.4 %) were higher than those reported by previous OSA studies [11–14, 16, 27, 30]. This difference may be related to the criteria of patient selection. Previous studies collected OSA patients without considering the different etiology of OSA. Given the multifactorial nature of OSA, OSA is more like a symptom of airway difficulty rather than an individual disease [6]. The narrowing of the airway may be induced by obesity, adenotonsillar hypertrophy, retrognathia, vocal cord paralysis, or other factors which obstruct the airway. An effective treatment towards OSA must be aiming at one or more risk factors to help in curing the obstruction. On the other hand, the treatment may not be effective when the aimed factors do not exist in the particular individuals. It is neither likely for adenotonsillectomy to function on OSA patients with a normal tonsil and a paralyzed vocal cord, nor for oral appliances to function when the exact obstruction is caused by enlarged adenoid tissues. Hence, an accurate diagnosis of the etiology of OSA is crucial to successful treatment. A recent research focusing on stepwise diagnosis and treatment of pediatric OSA also addressed that since the abnormalities which contribute to OSA varied, the treatment should also be multifaceted towards every existing factors in patient [6]. The higher success rate in the current study might be due to the fact that the subjects were selected from otherwise healthy OSA children with retrognathia only. Other factors such as adenotonsillar hypertrophy or obesity causing OSA were excluded, and patients with those factors who are unlikely to respond to OAs are also excluded. That might be one explanation of this satisfactory result. However, it should be pointed out that the changes in polysomnography readings did not return to the normal range, suggesting that there are possible factors other than retrognathia existing in the study group. For patients with residue pathological AHI, follow-up attention and intervention should be given. Another full examination and consultation with sleep specialists is needed to identify factors that may still narrow the airway while sleeping, and etiological intervention should be carried out to further relieve airway difficulty.
During the TB treatment, some of the patients reported salivation and initial discomfort which were gradually alleviated in the next few days, and no one abandoned the treatment. The better compliance, compared to previous study [16], might come from the different appliance design. One-piece appliance “fixed” the lower jaw to the upper, and the patient was unable to move the mandible, while two-piece appliance, like TB, allowed lateral and vertical jaw movement and thus enhanced compliance.
Currently, there is a lack of research on the cephalometric comparison of the effect of OAs on pediatric OSA. Results from the cephalometric measurements suggested that treatment with the TB appliance could increase SPAS, MAS, SNB, and reduced SPL (p < 0.01), while IAS remains basically the same. An increase in the SNB angle and facial convexity indicated a preferred forward growth of the mandible and a better profile, which was the classic effect of twin block in orthodontic treatment. It is interesting to find that the main changes were found in the soft palate-related measurements (SPAS, MAS, SPL), while twin block mainly affected the mandible. Maybe the change was due to the complex interaction between the tissues of upper and lower jaws. More research is needed to investigate the effect of OAs' on airway alteration.
There are certain limitations in the design of this study. The most important one is that there is no control group to compare and to eliminate other factors such as growth that might affect the results. However, due to ethical consideration, all children were recruited in the treatment group because the use of functional appliance before puberty might be the only possibility for patients with obvious retrognathia to gain a relatively normal profile and avoid orthognathic surgery in the future. Hence, the effect of growth on PSG or cephalometry measurement was not excluded. More well-designed studies might be carried out to investigate to what extent does TB or other OAs alone improves children OSA symptoms. Patients' compliance is also a possible factor associate with responses to the appliance. The change in airway is both anatomical and physiological. Since the mandible moved forward, the interplay between different muscle groups controlling the airway might be altered [12]. Although all patients reached designed anatomical mandible position, the ones wearing MAD more might end up with a more stable and favorable muscle function against airway collapsibility, while noncompliant patients did not. However, the present study did not record the actual time of MAD wearing. Moreover, the short follow-up prevented us from evaluating the long-term efficiency of TB in treating children OSA. Studies of long time follow-up about sleep condition after MAD removal and fixed orthodontic treatment is called for, to further explore the treatment efficacy and stability of MAD.
Conclusions
From the present preliminary study, twin block might be an efficient appliance for treatment of children with OSA and mandibular retrognathia, as long as the patients were carefully diagnosed and selected, while its long-term stability is yet to be determined.
References
Carroll JL (2003) Obstructive sleep-disordered breathing in children: new controversies, new directions. Clin Chest Med 24:261–282
Alexopoulos EI, Gletsou E, Kostadima E, Kaditis D, Zakynthinos E, Gourgoulianis K, Kaditis A (2011) Effects of obstructive sleep apnea severity on serum lipid levels in Greek children with snoring. Sleep Breath 15:625–631
Owens J, Spirito A, Marcotte A, McGuinn M, Berkelhammer L (2000) Neuropsychological and behavioral correlates of obstructive sleep apnea syndrome in children: a preliminary study. Sleep Breath 4:67–78
Xu Z, Jiaqing A, Yuchuan L, Shen K (2008) A case–control study of obstructive sleep apnea-hypopnea syndrome in obese and nonobese chinese children. Chest 133:684–689
Praud JP, Dorion D (2008) Obstructive sleep disordered breathing in children: beyond adenotonsillectomy. Pediatr Pulmonol 43:837–843
Kaditis A, Kheirandish-Gozal L, Gozal D (2012) Algorithm for the diagnosis and treatment of pediatric OSA: a proposal of two pediatric sleep centers. Sleep Med 13:217–227
Guilleminault C, Huang YS, Glamann C, Li K, Chan A (2007) Adenotonsillectomy and obstructive sleep apnea in children: a prospective survey. Otolaryngol Head Neck Surg 136:169–175
Giles TL, Lasserson TJ, Smith BH, White J, Wright J, Cates CJ (2006) Continuous positive airways pressure for obstructive sleep apnoea in adults. Cochrane Database Syst Rev 3:CD001106
Tsuda H, Almeida FR, Tsuda T, Moritsuchi Y, Lowe AA (2010) Craniofacial changes after 2 years of nasal continuous positive airway pressure use in patients with obstructive sleep apnea. Chest 138:870–874
Villa MP, Pagani J, Ambrosio R, Ronchetti R, Bernkopf E (2002) Mid-face hypoplasia after long-term nasal ventilation. Am J Respir Crit Care Med 166:1142–1143
Ghazal A, Sorichter S, Jonas I, Rose EC (2009) A randomized prospective long-term study of two oral appliances for sleep apnoea treatment. J Sleep Res 18:321–328
Hoffstein V (2007) Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath 11:1–22
Ahrens A, McGrath C, Hagg U (2011) A systematic review of the efficacy of oral appliance design in the management of obstructive sleep apnoea. Eur J Orthod 33:318–324
Ahrens A, McGrath C, Hagg U (2010) Subjective efficacy of oral appliance design features in the management of obstructive sleep apnea: a systematic review. Am J Orthod Dentofac Orthop 138:559–576
Almeida FR, Lowe AA (2009) Principles of oral appliance therapy for the management of snoring and sleep disordered breathing. Oral Maxillofac Surg Clin North Am 21:413–420
Villa MP, Bernkopf E, Pagani J, Broia V, Montesano M, Ronchetti R (2002) Randomized controlled study of an oral jaw-positioning appliance for the treatment of obstructive sleep apnea in children with malocclusion. Am J Respir Crit Care Med 165:123–127
Villa MP, Miano S, Rizzoli A (2012) Mandibular advancement devices are an alternative and valid treatment for pediatric obstructive sleep apnea syndrome. Sleep Breath 16:971–976
Chen H, Lowe A A (2012) Updates in oral appliance therapy for snoring and obstructive sleep apnea. Sleep Breath
Almeida FR, Tsuiki S, Hattori Y, Takei Y, Inoue Y, Lowe AA (2011) Dose-dependent effects of mandibular protrusion on genioglossus activity in sleep apnoea. Eur Respir J 37:209–212
Guilleminault C, Pelayo R, Leger D, Clerk A, Bocian RC (1996) Recognition of sleep-disordered breathing in children. Pediatrics 98:871–882
Zucconi M, Caprioglio A, Calori G, Ferini-Strambi L, Oldani A, Castronovo C, Smirne S (1999) Craniofacial modifications in children with habitual snoring and obstructive sleep apnoea: a case–control study. Eur Respir J 13:411–417
Tsuda H, Fastlicht S, Almeida FR, Lowe AA (2011) The correlation between craniofacial morphology and sleep-disordered breathing in children in an undergraduate orthodontic clinic. Sleep Breath 15:163–171
Deng J, Gao X (2012) A case–control study of craniofacial features of children with obstructed sleep apnea. Sleep Breath 16:1219–1227
Hassel B, Farman AG (1995) Skeletal maturation evaluation using cervical vertebrae. Am J Orthod Dentofac Orthop 107:58–66
Uliel S, Tauman R, Greenfeld M, Sivan Y (2004) Normal polysomnographic respiratory values in children and adolescents. Chest 125:872–878
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320:1240–1243
Lawton HM, Battagel JM, Kotecha B (2005) A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: a prospective study. Eur J Orthod 27:82–90
Chang SJ, Chae KY (2010) Obstructive sleep apnea syndrome in children: epidemiology, pathophysiology, diagnosis, and sequelae. Korean J Pediatr 53:863–871
Pae EK, Lowe AA, Sasaki K, Price C, Tsuchiya M, Fleetham JA (1994) A cephalometric and electromyographic study of upper airway structures in the upright and supine positions. Am J Orthod Dentofac Orthop 106:52–59
Blanco J, Zamarron C, Abeleira PM, Lamela C, Suarez QD (2005) Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome. Sleep Breath 9:20–25
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, C., He, H. & Ngan, P. Effects of twin block appliance on obstructive sleep apnea in children: a preliminary study. Sleep Breath 17, 1309–1314 (2013). https://doi.org/10.1007/s11325-013-0840-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-013-0840-5