Abstract
Twin-block appliance had been advocated as a potential treatment option in paediatric obstructive sleep apnoea (OSA) due to their favourable effect in enhancing upper airway parameters and improving OSA symptoms. The aim of this study was to evaluate the effect of twin-block appliance therapy on upper airway parameters/dimensions and the apnoea-hypopnea indexes (AHIs) in OSA children with class II mandibular retrognathic skeletal malocclusion using cone-beam computed tomography. This prospective longitudinal study comprised 34 polysomnography-proven OSA growing children with class II mandibular retrognathic skeletal malocclusion between the ages of 8 and 12 years who had completed myofunctional twin-block therapy and matched corresponding controls. The upper airway was segmented into the nasopharynx, oropharynx, and hypopharynx, and the effect of twin-bock treatment on upper airway parameters/dimensions was assessed pre- and posttreatment using CBCT analysis, while a second standard overnight PSG was performed to determine changes in the AHI. At the nasopharynx level, minimal (nonsignificant) increases in all variables were observed within the twin-block group and between the groups (P > 0.05). At the level of the oropharynx, all variables increased significantly in the treatment group and between groups (P < 0.001), but these increases were nonsignificant in the control group. At the level of the hypopharynx, only the minimum cross-sectional area (MCA) increased significantly in the treatment group (P = 0.003). The change in MCA was also significant between the groups (P = 0.041). In addition, the upper airway length increased significantly in the twin-block group (P = 0.0154), and the AHI decreased by 74.8% (P < 0.001).
Conclusion: Correction of class II mandibular retrognathic skeletal malocclusion with twin-block appliance resulted in a significant increase in upper airway volume, MCA, anteroposterior and lateral distances of the MCA at the level of the oropharynx, MCA at the level of the hypopharynx and upper airway length, and a significant decrease in AHI, but it had no effect on nasopharynx parameters.
What is Known: • CBCT imaging has been shown to be an effective and precise diagnostic tool for analyzing the upper airways and craniofacial structures. • Twin block appliance may be an effective treatment modality in children with OSA. | |
What is New: • Minimal cross-sectional area of upper ways may be the most relevant potential parameter when explaining how the upper airway anatomy plays role of in the pathogenesis of pediatric OSA. • Twin block appliance induced favorable changes in upper airway morphology (oropharynx area mainly) and respiratory parameters in OSA children with class II malocclusion. |
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Sleep disturbances can burden normal development during childhood. Children who are sleep deprived often demonstrate daytime fatigue, restlessness, hyperactivity, and poor schooling performance [1, 2]. In severe cases, sleep pathology carries devastating health consequences, resulting in hypertension, heart diseases, insulin resistance, and other metabolic disturbances [3, 4]. Sleep breathing disorders (SDBs) have a very large scale of symptoms, from plain, primary snoring, which might be harmless, to obstructive sleep apnoea (OSA), a condition related to snoring with nighttime repetitive airway patency disruptions that can potentially lead to life-threatening complications in the paediatric population. Increased risks of upper airway obstruction have been linked to obesity and fat tissue infiltration, hypertrophy of adenotonsillar tissues, and some craniofacial features that increase the incidence of airway collapsibility [5]. Being unaware of OSA and its potential complications in children may result in delayed diagnosis and unnecessary morbidity. Therefore, early diagnosis and interceptive treatment of children exhibiting signs and symptoms of OSA should be encouraged.
Paediatric OSA is associated with anatomic discrepancies of the upper airway that reduce the cross-sectional area and thus increase upper airway resistance. These discrepancies include adenotonsillar hypertrophy, restricted transverse maxillary dimensions, and retrognathic mandibles [6]. Orthodontic treatment is emerging as a potential modality for paediatric OSA. It has been hypothesized that mandibular advancement via orthodontic functional appliances may increase pharyngeal calibre size and limit the propensity for upper airway collapse [7, 8]. The twin-block appliance is an orthodontic oral appliance that advances the mandible and/or tongue with variable degrees of downwards mandibular rotation. The appliance rapidly and functionally corrects malocclusion by transmitting favourable occlusal forces to occlusal inclined planes that cover the posterior teeth (Fig. 1). This twin-block device was advocated as a potential oral appliance to treat children with OSA through mandibular advancement and improving pharyngeal airway dimensions [7].
In the past, lateral cephalograms were the most commonly used two-dimensional (2D) imaging modalities for evaluating airways. However, a 2D representation of three-dimensional (3D) craniofacial structures has serious diagnostic limitations due to image distortion, various magnifications, and superimposition of bilateral structures [9, 10]. Furthermore, lateral cephalograms cannot reveal upper airway changes in the transverse dimension [11]. Recent advances in cone-beam computed tomography (CBCT) of the craniofacial complex coupled with the greatly reduced radiation dose and high-resolution images have yielded more accurate diagnostic assessments of volumetric regions and cross-sectional areas. Axial sections of 3D CBCT scanning volumes enhance the visibility of soft tissue points that are derived from the projection of shaded areas when compared with 2D radiographs, thereby improving airway assessment. However, CBCT images have certain limitations regarding OSA diagnosis; they provide no information on neuromuscular tone, collapsing tendency, or actual function of the airway. CBCT scans are taken at a fixed point in time with the patient in the upright position during wakefulness. Therefore, patterns of obstruction or decreased cross-sectional area detected on these images may not actually reflect the dynamic upper airway anatomy during the sleep state. In contrast, 3D imaging of the upper airways may be used for monitoring or treatment considerations [12]. The aim of this study was to evaluate the effect of twin-block appliance therapy on upper airway parameters/dimensions in OSA children with class II mandibular retrognathic skeletal malocclusion using cone-beam computed tomography.
Materials and methods
This prospective longitudinal study was approved by the Research and Ethics Committee of the Health Campus at Universiti Sains Malaysia (approval number: Malaysia SM/JEPeM/20060315). The study was conducted in accordance with the Declaration of Helsinki, and all the procedures being performed were part of routine care. Informed consent was obtained from the participants and/or their parents prior to the assessment, and explanatory letters explaining the study were provided. Using PS software, a minimum sample size of 34 subjects in each group was required to detect airway differences between both groups at a level of significance of 0.05 and power of 80%. For this purpose, a standard deviation of lower-pharyngeal airway volume of 1104.04 mm3 from a previous publication was used [13]. Subjects enrolled in this study were growing children in the age range of 8 to 12 years prior to their peak pubertal growth spurt with cervical vertebrae maturation of stage 2 or 3. The study group comprised polysomnography-proven OSA children (apnoea-hypopnea index (AHI) > 1.0/h), while controls had negative PSG tests (AHI < 1.0/h). Both groups had similar selection criteria: class II skeletal malocclusion associated with normal maxilla (SNA, 79° to 84°) and mandibular retrusion (SNB ≤ 76°). The Frankfort mandibular plane angle (FMA) was in the range of 20° to 28°, and overjet was 6 to 10 mm with minimal crowding or spacing in either arch. The study group was treated with a twin-block myofunctional appliance, while the control group received a phase of prefunctional therapy (sectional, fixed orthodontic appliance) to correct occlusal interferences. The control group (class II skeletal malocclusion with retrognathic mandible) was matched with the study group in terms of age, sex, and body mass index (Table 1). In addition, smoking, alcohol, and other medication intake, as possible confounders, were considered during matching. Patients with a previous history of adenotonsillectomy or orthodontic treatment, genetic craniofacial syndromes, and lower respiratory airway diseases were excluded from the study.
An individual customized twin block was fabricated for each patient. One-step mandibular advancement was performed during wax check-bite recording with an edge-to-edge incisor relationship and a 3-mm opening between the maxillary and mandibular incisors. Single-phase advancement was proposed to maximize the orthopaedic effect of the twin-block appliance despite its reduced patient compliance and comfort relative to the incremental advancement method [14]. A midline expansion screw was incorporated in the upper part of the appliance if any crossbite or cusp-to-cusp relation of the posterior teeth was noted during bite registration. Maxillary expansion was performed when needed. The patients were instructed to wear the appliance full time even during mealtimes when possible to reduce the overjet and achieve a class I molar relationship. The bite blocks were trimmed to encourage normal vertical development of the mandibular buccal segments. To ensure patient adherence to treatment, parents were asked to fill out a daily wear time assessment booklet. All patients were reviewed monthly for 9 months. CBCT scanning was performed before appliance placement and at the end of treatment for all subjects in both groups to determine whether optimal clinical results were achieved. In addition, a second standard overnight polysomnography was performed for the study group 30 days after the end of treatment as a wash-out period to minimize the effects of muscle tension.
CBCT imaging
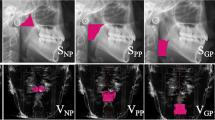
CBCT scans were performed using a Kavo 3DeXam (Kavo, Biberach, Germany). The scan covered the area from the basis cranii to the fourth cervical vertebra level with the following parameters: 120 kV and 5 mA, a voxel size of 0.4 mm, and a scanning time of 8.9 s. All CBCT scans were performed by the same operator following the manufacturer’s instructions. Patients were seated comfortably in an upright posture while maintaining a natural head with teeth at maximum intercuspation. The lips and tongue were in the resting position without swallowing during scanning. All CBCT datasets were exported and viewed in Digital Imaging and Communications in Medicine (DICOM) format and examined using Dolphin imaging and Management Solution, version 11.0 (Chatsworth, CA) software, which allows 3D virtual model reconstruction of the upper airways. Anatomical landmarks were identified (Fig. 2), and the upper airway was segmented into three regions—the nasopharynx, oropharynx, and hypopharynx—according to the corresponding cross-sectional slices (Fig. 3). Table 2 shows the limits and boundaries of each region. The volumes of airway subregions were measured based on variations in the density of different tissues using a patient-specific threshold range.
Anatomical landmarks of upper airway on the cone beam computed tomography (CBCT). 1: PNS, posterior nasal spine; 2: ANS, anterior nasal spine; 3: AICV, anterior-inferior aspect of the vertebral body of 2nd cervical vertebra (AICV); 4: TUV, tip of the uvula; 5: TEP, tip of the epiglottis; 6: BEP, base of epiglottis
Based on these landmarks and data, the following parameters were identified:
-
1.
Airway volume of each region (nasopharynx, oropharynx, hypopharynx)
-
2.
Minimum cross-sectional area (MCA) of each region (nasopharynx, oropharynx, hypopharynx) in the axial view
-
3.
Anteroposterior and lateral distances of the smallest axial cross-sectional slice of each region
-
4.
Length of the upper airway (vertical distance from the tip of the PNS to the inferior border of C2)
Reliability
Two trained observers (the principal investigator and a radiologist) independently performed anatomical landmark localization and measurements of the upper airways. One week later, being blinded to previous patient information and results, both observers reassessed the same variables to determine intra- and interobserver reliability using intraclass correlation coefficients (ICCs).
Statistical analysis
The data in both the twin-block and control groups were tested with the Shapiro‒Wilk test, which showed that they were normally distributed. Differences pre- and posttreatment within the same group were tested with paired t tests, while significant changes in each group were assessed by unpaired t tests. Multiple comparisons between the twin-block and the control groups were performed using Bonferroni correction. To measure the size of mean differences between the twin-block and control groups, effect size was tested using Cohen’s d formula (the difference of the means of two groups divided by the weighted pooled standard deviations of these groups).
Results
The ICCs of intra- and interobserver reliability for upper airway measurements are shown in Table 3. Both intraobserver and interobserver reliability were excellent (ICC = 0.946–0.992), except for the interobserver reliability of the MCA of the nasopharynx and hypopharynx (ICC = 0.840 and 0.862, respectively).
The mean daily wear time was 13.43 ± 3.79 h. Treatment with the twin-block appliance caused mandibular protrusion, as SNB increased by 3.28° (P < 0.001) and ANB (anteroposterior relationship of the mandible to the maxilla) decreased by 2.98° (P < 0.001). The FMA increased by 2.40° (P = 0.021), and the mandibular length increased by 2.76 mm (P < 0.001). Table 4 shows the mean upper airway parameters, standard deviations, and differences within the treatment group (pre- and posttreatment) and between both groups (treatment/controls). At the level of the nasopharynx, the change (minimal increase) in all variables was insignificant within the treatment group and between both groups (P > 0.05). At the level of the oropharynx, all variables increased significantly in the twin-block group and between both groups (P < 0.05). After treatment, the volume increased by 3137 mm3 (P < 0.001), the MCA increased by 40.47 mm2 (P < 0.001), and the anterior–posterior and lateral distances of the MCA increased by 3.53 mm (P = 0.027) and 4.26 mm (P = 0.016), respectively. However, the increase pre- and post-follow-up was nonsignificant for all variables in the control group. At the level of the hypopharynx, the MCA increased significantly in the treatment group by 19.91 mm2 (P = 0.003). The change in the MCA was also significant between both groups (P = 0.041). After Bonferroni correction for repeated measures, all parameters at the level of the oropharynx, the MCA at the level of the hypopharynx, and upper airway length were significantly greater in the twin-block group than in the control group (Table 4). Effect sizes for the differences between the groups were small or medium (0.2–0.5). Only the MCA of the oropharynx and hypopharynx demonstrated a large effect size (1.9 and 1.1, respectively). At the end of treatment, the AHIs had dropped significantly by 11.2 events/hour (P < 0.001).
Discussion
Several reports have advocated the twin-block device as an efficient oral appliance for the treatment of children with class II skeletal malocclusion with retrognathic mandible given its noninvasiveness and good tolerability by the patients [15, 16]. Clinically, twin-block appliance therapy can significantly reduce AHI and snoring time, increase the overall oxygen saturation, and improve symptoms related to OSA, such as quality of life, behaviour, and school performance [17,18,19]. Anatomically, results have shown an improvement in upper airway dimensions following functional appliance therapy [20, 21]. However, those reports contained several methodological flaws, such as heterogeneous samples with a lack of sound control conditions. In addition, the analysis of upper airway dimensions was based on lateral cephalometric analysis, which is not ideal for diagnosing the complex 3-dimensional configuration of upper airways. This study utilized 3D-based CBCT evaluation of the effects of twin-block appliance therapy on different upper airway subregions and AHIs in paediatric OSA.
One limitation in this study is that the CBCT scans were taken in the upright position, while OSA usually occurs during sleep (supine position). Camacho and colleagues found that the minimum cross-sectional area decreased significantly when patients were scanned in the supine relative to the upright position due to retrodisplacement of the base of the tongue and epiglottis in the supine position [22]. However, there was evidence of an insignificant association between head posture and airway volume [23].
Another dilemma is that breathing was not controlled during acquisition of CBCT scans (alterations in respiration phases), which could bias assessment. In addition, there is no standardized approach for upper airway assessment with CBCT due to many uncontrolled variables, such as alterations in tongue position during acquisition, the influence of neighbouring structures, and systematic errors in identifying anatomical landmarks and boundaries. Additional evidence of underestimation of the actual upper airway dimensions arises when various software programs are utilized, with measuring errors ranging from 1.1 to 10.8% [24, 25]. However, such inaccuracy would be neglected when all samples are analysed in the same manner. The implications of these confounding variables are already widely recognized by mainstream sleep research.
At the level of the nasopharynx, no significant differences were found within the treatment group (pre- and posttreatment) or between the treatment group and controls in all parameters (volume, MCA, AP, and lateral dimensions of MCA). The nasopharynx is the superior part of the upper airway formed by muscle and fascia and bounded by relatively rigid components (choanae anteriorly; vertebral bodies of C1, C2 posteriorly, sphenoid sinus and the basisphenoid superiorly, and roof of the soft palate inferiorly). This relationship between the nasopharynx and its bony enclosure may explain why the upper parts of the upper airway demonstrate less airway collapsibility during sleep than the lower parts as well as the fewer dimensional changes during mandibular advancement therapy. In normal circumstances, assessment of nasal airflow dynamics shows that nasopharynx geometry contributes minimally to upper airway resistance [26]. In this regard, rapid maxillary expansion (RME) was found to significantly impact the volume and dimensions of the nasal cavity and nasopharynx but not the oropharynx due to the remote nature of the anatomical features of the nasopharynx and their relationship with the maxillary complex [27]. The minimal increase in all variables among both groups might be attributed to two factors: normal growth development and reduced thickness of the posterior pharyngeal wall as a compensatory mechanism to maintain upper airway patency.
At the level of the oropharynx, all upper airway parameters (volume, MCA, AP and lateral dimensions of the MCA) were significantly improved within the treatment group (pre- and posttreatment) and a significant difference was also detected between the treatment group and controls (P < 0.05). However, the increase in upper airway parameters within the control group was minimal (P > 0.05). This increase in oropharyngeal volume (3137 mm3) after twin-block therapy might reflect an improvement in airway flow. Similar results were reported by Wang et al. [28] and Shete and Bhad [21], who focused on the velopharynx and oropharynx, while Haskell et al. found that the change in volume was insignificant [29]. The MCA is the most critical site that causes maximum resistance to airflow. In OSA subjects, a smaller MCA and related anterior-posterior and lateral dimensions at the oropharynx level are a consistent finding in the literature regardless of BMI matching between OSA patients and the corresponding and of the method of assessment (MRI or CBCT) [30, 31]. The increase in the MCA following mandibular advancement therapy (40.47 mm2 in this study) is considered a definite clinical indicator for the improvement of airflow and upper airway volume [28]. The AP and lateral dimensions of the MCA represent the severity of the obstruction of the upper airway in the sagittal and transverse planes, respectively. At the level of the oropharynx, we found a greater increase in the lateral dimensions of the MCA (4.26 mm) than in the AP dimensions (3.53 mm). Similar findings of greater transverse dimensional changes in the upper airway were reported by Zhao et al. [32] and Shete and Bhad [21]. Furthermore, evidence from paediatric anaesthesia concurs with our findings; propofol-based sedation is associated with greater transverse collapsibility of upper airways than anterior-posterior collapsibility [33]. The exact mechanism of these morphological changes remains unclear. However, there is agreement that upper-way patency is controlled by the pharyngeal muscles that comprise the nonbony portions of the pharyngeal wall. In fact, the anatomic alterations of the upper airways induced by twin-block therapy seem to be quite sophisticated due to the complex configuration of upper airway structures.
The influence of tongue volume on the patency of upper airways should be highlighted, as the posterior one-third of the tongue is located in the oropharynx. Jena et al. suggested that the backward position of the tongue in subjects with a retrognathic mandible pushes the soft palate posteriorly and encroaches on the upper airway dimensions [34]. Thus, the forward posture of the tongue and mandible by twin-block therapy might improve the sagittal jaw relationship and upper airway patency at this level.
At the level of the hypopharynx, only the MCA increased significantly (19.91 mm2) with twin-block therapy (P = 0.003). This difference was also significant between the groups (P = 0.041), whereas other variables showed no differences. Interestingly, we demonstrated a large effect size for differences in MCA of the oropharynx and hypopharynx (1.9 and 1.1, respectively) between the groups. Evaluation of effect size allows a more general interpretation and quantitative description of the size of an observed effect rather than overvaluing its statistical significance. These findings demonstrate that the MCA is the most relevant potential parameter when explaining how the upper airway anatomy plays a role in the pathogenesis of paediatric OSA. At this level, Chen et al. proposed the MCA at the base of epiglottis as a primary outcome and detected a reduced MCA in OSA patients [35].
In this study, the supraglottic portion (PNS-C2 distance) was identified as the upper airway length because the pharyngeal musculature and soft tissues are more susceptible to tube collapsibility than the more rigid cartilaginous subglottic portion. Increased upper airway length is directly related to increased airway resistance and is considered a predictor of OSA. This study showed that twin-block therapy increases the vertical dimensions of the upper airways, and this increase may be attributed to the fact that during TB treatment, the mandible is advanced in the vertical direction, and the hyoid bone is in a more forwards and inferior position. In this regard, Li et al. found similar vertical growth patterns among OSA subjects and corresponding controls with mixed dentition and of young adult age [36].
The significant increase in SNB and FMA and overjet reduction in the study group demonstrated the clinical effectiveness of the twin-block appliance in the anteroposterior skeletal correction of class II malocclusion. In addition, a significant reduction was observed in the AHI (74.8% drop), which mirrors data reported by Zhang et al., who reported an average AHI decrease of 75.9% [16]. However, others have reported lower values of AHI reduction, including 63.4% by Villa et al. [37] and 28.6% by Umemoto et al. [17]. Patient compliance might partially explain these conflicting findings, wherein subjects wearing the twin-block appliance more often might end up with more stable and favourable muscle function against upper airway collapsibility, while noncompliant patients did not. In addition, inconsistencies in patient selection criteria and different underlying aetiologies of OSA might play a role. It is clear that twin-block therapy is advantageous in treating paediatric OSA and reducing the overall AHIs, although they did not return to normal paediatric reference values. However, it should be noted that some AHI changes may have been attributed to growth of the upper airway or regression of lymphoid tissues. Rongo et al. found that airway dimensions increased for both control subjects and class II patients treated with a Sander bite-jumping appliance due to physiological growth [38]. Their study highlighted the importance of growth in the assessment of the effect of orthodontic functional therapy on pharyngeal dimensions.
The literature shows that twin-block appliances are superior to other myofunctional treatment modalities in terms of improving upper airway parameters among class II malocclusion subjects with retrognathic mandibles. Kinzinger et al. found that the Herbst appliance was ineffective in preventing breathing problems in OSA patients despite its forwards advancement of the mandible and anterior traction of the tongue [39]. Jena et al. found that twin-block appliances were more efficient in improving PAP dimensions among class II malocclusion subjects with retrognathic mandibles than the mandibular protraction appliance-IV [40]. They concluded that the orthopaedic action (outgrowth and advancement of the mandible) was significantly greater with the twin-block therapy device than with other myofunctional appliances.
Interestingly, the current study showed very good daily wear time (13.43 h), which is clearly above the 8-h threshold required to achieve good patient compliance as reported by Sarul et al. [41]. However, patient compliance and adherence to the treatment protocol seem to be lower in younger children, an age group for which compliance and adherence are largely related to parental cooperation [42]. Overall, correction of anteroposterior dental arch discrepancies induced favourable changes in upper airway morphology. The long-term stability of functional therapy on improving upper airways and the resilience of these benefits against later growth should be addressed in future studies.
Conclusion
The current study shows that the correction of class II mandibular retrognathic skeletal malocclusion with a twin-block appliance resulted in a significant increase in the upper airway volume, MCA, and anteroposterior and lateral distances of the MCA at the level of the oropharynx, MCA at the level of the hypopharynx, increased upper airway length, and a significant reduction in the AHI, but it had no effect on nasopharynx parameters.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Kaneita Y, Yokoyama E, Harano S, Tamaki T, Suzuki H, Munezawa T, Nakajima H, Asai T, Ohida T (2009) Associations between sleep disturbance and mental health status: a longitudinal study of Japanese junior high school students. Sleep Med 10:780–786
Akinci B, Aslan GK, Kiyan E (2018) Sleep quality and quality of life in patients with moderate to very severe chronic obstructive pulmonary disease. Clin Respir J 12:1739–1746
Jensen ME, Gibson PG, Collins CE, Wood LG (2013) Airway and systemic inflammation in obese children with asthma. Eur Respir J 42:1012–1019
Pretl M, Lattová Z, Polák AP, Westlake K (2019) Metabolic disorders and sleep. Cas Lek Cesk Fall 5:185–192
Gulotta G, Iannella G, Vicini C, Polimeni A, Greco A, de Vincentiis M, Visconti IC, Meccariello G, Cammaroto G, De Vito A, Gobbi R, Bellini C, Firinu E, Pace A, Colizza A, Pelucchi S, Magliulo G (2019) Risk factors for obstructive sleep apnea syndrome in children: state of the art. Int J Environ Res Public Health 16(18):3235
Liu Y, Zhao T, Ngan P, Qin D, Hua F, He H (2023) The dental and craniofacial characteristics among children with obstructive sleep apnoea: a systematic review and meta-analysis. Eur J Orthod 45(3):346–355
Ghodke S, Utreja AK, Singh SP, Jena AK (2014) Effects of twin-block appliance on the anatomy of pharyngeal airway passage (PAP) in class II malocclusion subjects. Prog Orthod 15(1):68
Xiang M, Hu B, Liu Y, Sun J, Song J (2017) Int J Pediatr Otorhinolaryngol 97:170–180
de Oliveira AE, Cevidanes LH, Phillips C, Motta A, Burke B, Tyndall D (2009) Observer reliability of three-dimensional cephalometric landmark identification on cone-beam computerized tomography. Oral Surg Oral Med Oral Pathol Oral Radiol 107:256–265
Katkar RA, Kummet C, Dawson D, Uribe L, Allareddy V, Finkelstein M, Ruprecht A (2013) Comparison of observer reliability of three-dimensional cephalometric landmark identification on subject images from Galileos and i-CAT cone beam CT. Dentomaxillofac Radiol 42:20130059
Tikku T, Khanna R, Sachan K, Agarwal A, Srivastava K, Lal A (2016) Dimensional and volumetric analysis of the oropharyngeal region in obstructive sleep apnea patients: a cone beam computed tomography study. Dent Res J (Isfahan) 13:396–404
Behrents RG, Shelgikar AV, Conley RS, Flores-Mir C, Hans M, Levine M, McNamara JA, Palomo JM, Pliska B, Stockstill JW, Wise J, Murphy S, Nagel NJ, Hittner J (2019) Obstructive sleep apnea and orthodontics: an American Association of Orthodontists White Paper. Am J Orthod Dentofacial Orthop 156(1):13–28
OnemOzbilen E, Yilmaz HN, Kucukkeles N (2019) Comparison of the effects of rapid maxillary expansion and alternate rapid maxillary expansion and constriction protocols followed by facemask therapy. Korean J Orthod 49(1):49–58
Banks P, Wright J, O’Brien K (2004) Incremental versus maximum bite advancement during twin-block therapy: a randomized controlled clinical trial. Am J Orthod Dentofacial Orthop 126:583–588
Nazarali N, Altalibi M, Nazarali S, Major MP, Flores-Mir C, Major PW (2015) Mandibular advancement appliances for the treatment of paediatric obstructive sleep apnea: a systematic review. Eur J Orthod 37:618–626
Zhang C, He H, Ngan P (2013) Effects of twin block appliance on obstructive sleep apnea in children: a preliminary study. Sleep Breath 17:1309–1314
Umemoto G, Toyoshima H, Yamaguchi Y, Aoyagi N, Yoshimura C, Funakoshi K (2019) Therapeutic efficacy of twin-block and fixed oral appliances in patients with obstructive sleep apnea syndrome. J Prosthodont 28:830–836
Lawton HM, Battagel JM, Kotecha B (2005) A comparison of the Twin Block and Herbst mandibular advancement splints in the treatment of patients with obstructive sleep apnoea: a prospective study. Eur J Orthod 27:82–90
Zreaqat M, Hassan R, Samsudin R, Alforaidi S (2023) Effects of twin-block appliance therapy on urinary leukotriene E4 and serum C-reactive protein levels in obstructive sleep apnea children with class II malocclusion and mandibular retrognathia: a prospective longitudinal study. Indian J Pediatr 90(7):729
Geoghegan F, Ahrens A, McGrath C, Hägg U (2015) An evaluation of two different mandibular advancement devices on craniofacial characteristics and upper airway dimensions of Chinese adult obstructive sleep apnea patients. Angle Orthod 85:962–968
Shete CS, Bhad WA (2017) Three-dimensional upper airway changes with mandibular advancement device in patients with obstructive sleep apnea. Am J Orthod Dentofacial Orthop 151:941–948
Camacho M, Capasso R, Schendel S (2014) Airway changes in obstructive sleep apnoea patients associated with a supine versus an upright position examined using cone beam computed tomography. J Laryngol Otol 128:824–830
Gurani SF, Di Carlo G, Cattaneo PM, Thorn JJ, Pinholt EM (2016) Effect of head and tongue posture on the pharyngeal airway dimensions and morphology in three-dimensional imaging: a systematic review. J Oral Maxillofac Res 31:1–12
Wong AK, Beattie KA, Min KK et al (2015) A trimodality comparison of volumetric bone imaging technologies. Part I: short-term precision and validity. J Clin Densitom 18:124–135
Rodriguez A, Ranallo FN, Judy PF, Gierada DS, Fain SB (2014) CT reconstruction techniques for improved accuracy of lung CT airway measurement. Med Phys 41:111911
Borojeni A, Frank-Ito DO, Kimbell JS, Rhee JS, Garcia GJM (2017) Creation of an idealized nasopharynx geometry for accurate computational fluid dynamics simulations of nasal airflow in patient-specific models lacking the nasopharynx anatomy. Int J Numer Method Biomed Eng 33:10–18
Izuka EN, Feres MF, Pignatari SS (2015) Immediate impact of rapid maxillary expansion on upper airway dimensions and on the quality of life of mouth breathers. Dental Press J Orthod 20:43–49
Wang W, Mo SC, Wang L (2018) Changes of airway before and after twin-block treatment in patients with mandibular retrusion. Shanghai Kou Qiang Yi Xue 27:607–611
Haskell JA, McCrillis J, Haskell BS, Scheetz JP (2009) Effects of mandibular advancement device (MAD) on airway dimensions assessed with cone-beam computed tomography. Semin Orthod 9:132–158
Schwab RJ, Gupta KB, Gefter WB, Metzger LJ, Hoffman EA, Pack AI (1995) Upper airway and soft tissue anatomy in normal subjects and patients with sleep-disordered breathing. Significance of the lateral pharyngeal walls. Am J Respir Crit Care Med 152:1673–1689
Ciscar MA, Juan G, Martínez V, Ramón M, Lloret T, Mínguez J, Armengot M, Marín J, Basterra J (2001) Magnetic resonance imaging of the pharynx in OSA patients and healthy subjects. Eur Respir J 17:79–86
Zhao X, Liu Y, Gao Y (2008) Three-dimensional upper-airway changes associated with various amounts of mandibular advancement in awake apnea patients. Am J Orthod Dentofacial Orthop 133:661–668
Litman RS, Weissend EE, Shrier DA, Ward DS (2002) Morphologic changes in the upper airway of children during awakening from propofol administration. Anesthesiology 96:607–611
Jena AK, Singh SP, Utreja AK (2010) Sagittal mandibular development effects on the dimensions of the awake pharyngeal airway passage. Angle Orthod 80:1061–1067
Chen H, Aarab G, de Ruiter MH, de Lange J, Lobbezoo F, van der Stelt PF (2016) Three-dimensional imaging of the upper airway anatomy in obstructive sleep apnea: a systematic review. Sleep Med 21:19–27
Li L, Liu H, Cheng H, Han Y, Wang C, Chen Y, Song J, Liu D (2014) CBCT evaluation of the upper airway morphological changes in growing patients of class II division 1 malocclusion with mandibular retrusion using twin block appliance: a comparative research. PLoS ONE 9:94378
Villa MP, Bernkopf E, Pagani J, Broia V, Montesano M, Ronchetti R (2002) Randomized controlled study of an oral jaw-positioning appliance for the treatment of obstructive sleep apnea in children with malocclusion. Am J Respir Crit Care Med 165:123–127
Rongo R, Martina S, Bucci R, Festa P, Galeotti A, AlessandriBonetti G, Michelotti A, D’Antò V (2020) Short-term effects of the Sander bite-jumping appliance on the pharyngeal airways in subjects with skeletal class II malocclusion: a retrospective case-control study. J Oral Rehabil 47(11):1337–1345
Kinzinger G, Czapka K, Ludwig B, Glasl B, Gross U, Lisson J (2011) Effects of fixed appliances in correcting angle Class II on the depth of the posterior airway space: FMA vs. Herbst appliance–a retrospective cephalometric study. J Orofac Orthop 72(4):301–320
Jena AK, Singh SP, Utreja AK (2013) Effectiveness of twin-block and mandibular protraction appliance-IV in the improvement of pharyngeal airway passage dimensions in class II malocclusion subjects with a retrognathic mandible. Angle Orthod 83(4):728–734
Sarul M, Nahajowski M, Gawin G, Antoszewska-Smith J (2022) Does daily wear time of twin block reliably predict its efficiency of class II treatment? J Orofac Orthop 83(3):195–204
Chuang LC, Lian YC, Hervy-Auboiron M, Guilleminault C, Huang YS (2017) Passive myofunctional therapy applied on children with obstructive sleep apnea: a 6- month follow-up. J Formos Med Assoc 116:536–541
Funding
This work was supported by the Health Campus in Universiti Sains Malaysia (grant code: USM/JEPeM/20060315).
Author information
Authors and Affiliations
Contributions
The main conception was proposed by Rani Samsudin and Rozita Hassan. Material preparation, data collection were performed by Maen Zreaqat and Rozita Hassan. Data analysis were performed by Maen Zreaqat and Sahal Alforaidi. The first draft of the manuscript was written by Maen Zreaqat and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zreaqat, M., Hassan, R., Samsudin, A. et al. Effects of twin-block appliance on upper airway parameters in OSA children with class II malocclusion and mandibular retrognathia: a CBCT study. Eur J Pediatr 182, 5501–5510 (2023). https://doi.org/10.1007/s00431-023-05226-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-05226-3