Abstract
Background
The Berlin Questionnaire (BQ) is a useful tool to identify the high-risk group for obstructive sleep apnea (OSA) in the primary care sites or hospital, but the usefulness of the BQ to identify the high-risk group for OSA in the general population has not been evaluated. The purpose of our study was to develop the Korean version of the BQ (KBQ) and evaluate the usefulness of the BQ in identifying patients with OSA in the general population.
Methods
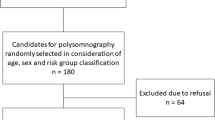
A total of 1,305 subjects were included in a population-based door-to-door cross-sectional study. For validation of the KBQ, an overnight polysomnography (PSG) was performed on 101 subjects who were randomly selected considering their age, sex, and risk group classification at a controlled sleep laboratory.
Results
The KBQ showed a relatively good to excellent internal consistency (Cronbach’s α correlation 0.64–0.78) and test–retest reliability (intraclass correlation 0.92). The apnea–hypopnea index (AHI) was significantly correlated with the scores in each category and the total scores of the KBQ. In addition, high risk grouping based on the KBQ predicted an AHI ≥ 5 with a sensitivity of 0.69 and a specificity of 0.83. According to the risk categorization based on the KBQ, 26.1 % subjects were in the high-risk group for OSA which was similar to the prevalence of OSA in a previous large epidemiological study using PSG in Korea.
Conclusion
This is the first study to confirm the usefulness of the BQ as a screening tool for OSA by prioritizing subjects at high risk for OSA in the general population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sleep-disordered breathing (SDB), especially obstructive sleep apnea (OSA), is known to be a relatively common sleep disorder [1]. OSA is an important medical condition characterized by excessive daytime sleepiness, snoring, and nocturnal hypoxemia during sleep [2] and it has strong association with hypertension, glucose intolerance, cardiovascular disorders, and cerebrovascular disorders [3-6]. In general, the prevalence of SDB in Korea is known to be 27 % in men and 16 % in women [7], and it is similar to that of other countries [8, 9]. However, results from several studies suggested that a considerable number of OSA patients remained undetected and only a few patients with OSA received the benefit of medical services and recent advances in sleep medicine [8, 10]. It has been reported that 93 % of women and 82 % of men with moderate to severe sleep apnea were not clinically diagnosed [10]. Polysomnography (PSG) is generally considered a gold standard diagnostic tool for evaluation of OSA in the sleep clinic but it is an expensive and time-consuming method.
The Berlin Questionnaire (BQ) was first developed in 1996 at the Conference on Sleep in Primary Care in Berlin, Germany. This questionnaire was validated as an authentic tool for identifying patients who are at high risk for OSA in some countries [11, 12], and this questionnaire is composed of three categories: snoring, wake-time sleepiness or tiredness, and the presence of obesity or hypertension [12]. The BQ has been frequently used in the screening for OSA and is well-known as a convenient and inexpensive tool [13]. The usefulness of the BQ to identify the high-risk group for OSA in the general population has not been evaluated.
The purpose of our study was to develop the Korean version of the BQ (KBQ) and evaluate the usefulness of the BQ in identifying patients with OSA in the general population by comparing the prevalence of OSA inferred from the KBQ and that of the previous large epidemiological study. Therefore, if we can prioritize subjects as high risk for OSA and who require PSG preferentially through the screening questionnaire targeting the general population, we can reduce social costs substantially and manage the public health care effectively.
Methods
Subjects
Subjects were recruited between April 2009 and May 2010 in two regions (Daegu and Jinju in South Korea). A representative sample was constituted according to a stratified, multistage random sampling method (sex, age groups, economics, and occupations of the population) based on the 2005 Korean Census, the most current census at that time. Structured door-to-door, personal interviews (paper-and-pencil interview) were conducted in all adults of the household aged between 20 and 69 years (1,484 persons/824 households). This survey was conducted by interviewers who received in-depth training regarding the KBQ as well as interviewing techniques. Demographic information (such as age and sex), living habits (such as smoking, alcohol, and caffeine intake), and history of illness were also investigated. Patients with history of alcoholism, chronic sedative drug use, a recent acute disease that might affect their sleep behaviors adversely (such as respiratory, renal, hepatic, stroke, or cardiovascular disease), or critical illness were excluded. Finally, a total of 1,305 subjects were included in our study. To examine the test–retest reliability of the KBQ, 30 subjects were randomly selected from the 1,305 participants, and they were retested with the questionnaire approximately 2–3 weeks later. Among the 1,305 subjects, 140 participants were randomly selected considering their age, sex, and risk group classification on the basis of the questionnaire, and they were asked to undergo PSG to confirm the diagnosis of SDB objectively. Finally, an overnight PSG was performed on 101 subjects at the controlled sleep laboratory to validate the KBQ. The study was approved by the Institutional Review Board of Kyungpook National University Hospital.
Development of the KBQ
After we acquired permission from the original developer of the BQ, the original English version of the BQ [14] was first translated into Korean by a native Korean professional translator who had majored in English literature. Our panel of sleep apnea experts consisting of neurologists and otolaryngologists reviewed this preliminary KBQ and revised it as close as possible to the original English version. Another bilingual sleep apnea expert back-translated this revised KBQ into English. The correspondence between this back-translated version and the original English version was reviewed again by the entire panel of sleep apnea experts. After considering the original, translated, and back-translated versions together, we developed the final KBQ (Appendix).
To calculate a patient’s risk profile for OSA, we followed all the original instructions except for body mass index (BMI) [12, 14] because the World Health Organization Western Pacific Regional Office proposed a modified BMI cutoff value of 23 kg/m2 to define overweight and 25 kg/m2 to define obesity in Asian populations, and we used this modified cutoff point for BMI in category 3 (≥25 kg/m2) [15].
Polysomnography
A single-night PSG was performed with a computerized PSG machine (Beehive Millennium, Grass-Telefactor) at the controlled sleep laboratory. The parameters, settings, filters, technical specifications, sleep stage scoring, and event scoring were done in accordance with the AASM Manual for the Scoring of Sleep and Associated Events [16]. Various parameters including electroencephalogram, electrooculogram, chin and leg electromyogram, nasal airflow temperature and pressure, thoracic wall, abdominal, and leg movements, transcutaneous oxygen saturation, and body position were monitored. Obstructive apnea was defined as (1) there is a drop in the peak thermal sensor excursion by ≥90 % of baseline, (2) the duration of the event lasts at least 10 s, and (3) at least 90 % of the event’s duration meets the amplitude reduction criteria for apnea. Hypopnea was defined as (1) the nasal pressure signal excursions drop by ≥50 % of baseline, (2) the duarion of this drop occures for a period lasting at least 10 s, (3) there is a ≥3 % desaturation from pre-event baseline or the event is associated with arousal, and (4) at least 90 % of the event’s duration must meet the amplitude reduction of criteria for hyponea [16]. The apnea–hypopnea index (AHI) was calculated by dividing the number of apneas and hypopneas by the number of hours of sleep. One well-trained polysomnographic technologist who had no knowledge of the questionnaire scored all the polysomnographic recordings. His scoring was reconfirmed by a sleep expert who had majored in neurology.
Statistical analysis
All statistical analyses were conducted with SPSS for Windows (version 12, SPSS, 2005). Differences with regard to many variables between the high- and low-risk groups were tested using χ 2 or t tests. The internal validity was examined by means of Cronbach’s α. Also, the test–retest reliability was evaluated by intraclass correlation coefficients. Spearman correlation analyses were used to explore the relationship between the PSG data (AHI) and KBQ variables. We used the overnight PSG data from 101 patients to validate the KBQ. When we assessed the predictive accuracy of risk grouping based on the KBQ, we also classified the degree of OSA based on the AHI (5, 10, and 15, the arbitrary cutoff values). The statistical significance level was set at p < 0.05.
Results
Demographics and prevalence of symptoms
Of 1,484 respondents in the population, 1,305 subjects were finally included in our study. Demographic characteristics of the 1,305 subjects are shown in Table 1.
Of the 1,305 subjects included in our study, 586 (44.9 %) reported that they snored and 15 (1.1 %) did not respond to this. Also, among these 586 snoring participants, 417 (71.2 %) subjects complained that their snoring was as loud as talking and 169 (28.8 %) subjects did snore louder than talking or very loudly. Three hundred and twenty-one (54.8) of the 586 snoring respondents complained that they snored at least three to four times per week. Moreover, 202 (32.0 %) of the 586 snoring respondents reported that their snoring bothered other people. Three hundred and eighty-nine (29.8 %) respondents felt tired or fatigued immediately after sleep at least three to four times per week, and 336 (25.7 %) respondents felt tired and fatigued during wake time, too.
In our study, we classified the participants according to the risk categorization based on the KBQ. Three hundred and forty (26.1 %) subjects were in the high-risk group for OSA and 965 (73.9 %) subjects were in the low-risk group for OSA. In addition, we compared the results of the questionnaires between the high- and low-risk groups. These analyses are shown in Table 2. Between the two groups, the results of the responses for all subcategories of the questionnaire were statistically different.
Internal validity and test–retest reliability
The reliability among individual questions within categories was tested by internal validity. The Cronbach’s α value was 0.78 for category 1 and 0.64 for category 2. If the question about sleepiness while driving was excluded, the Cronbach’s α value for category 2 increased to 0.82. In addition, the test–retest intraclass correlation coefficient was 0.92.
Validation of the KBQ
According to the result of risk grouping based on the KBQ, 51 subjects were in the high-risk group for OSA and 50 subjects were in the low-risk group. Between the high- and low-risk groups, demographic information (such as age and sex), living habits (such as smoking, alcohol, and caffeine intake), and history of illness were not statistically different. These results are summarized in Table 3.
We evaluated the relationship between the AHI and KBQ variables (Table 4). In the Spearman’s correlation analyses, the AHIs were significantly correlated with the scores in each category and the total scores of the KBQ.
We also assessed the predictive accuracy of risk grouping based on the KBQ. The distributions of the two risk groups with respect to the AHI and the ability of risk grouping with elevated AHIs are shown in Table 5. Forty-five of the 65 subjects whose AHIs were more than 5 were classified as the high-risk group for OSA based on the KBQ. Thirty of the 36 subjects whose AHIs were under 5 were classified as the low-risk group for OSA. High risk grouping of KBQ predicted an AHI ≥ 5 with a sensitivity of 0.69 and a specificity of 0.83. As the AHI cutoff value increased, the sensitivity of risk grouping based on the KBQ increased and the specificity of risk grouping decreased, as expected.
Discussion
The AHIs derived from the PSG were significantly correlated with the scores in each category of KBQ and the total scores of the KBQ. The AHI ≥ 5 cutoff point has been frequently used as a polysomnographic diagnostic criterion for OSA in many articles especially in several validation studies of the sleep questionnaire [11, 17]. The high risk grouping based on the KBQ predicted an AHI ≥ 5 with a sensitivity of 0.69 and a specificity of 0.83 and as the AHI cutoff value increased, the sensitivity of risk grouping based on the KBQ increased. Our results suggested that the ability of the KBQ to predict the presence of OSA with an elevated AHI was relatively good.
Actually, the predictive accuracy of the BQ for OSA varied greatly in many studies [11-13, 18]. The sensitivity ranged from 62 % to 86 % and the specificity ranged from 43 % to 95 %. These varying results might be due to the different study populations, different PSG methods or cutoff points for OSA diagnosis. At first, Netzer et al. reported that the high-risk group defined by the BQ predicted a respiratory disturbance index (RDI) > 5 with a sensitivity of 86 % and specificity of 77 % [12]. Unlike our study, they evaluated the usefulness of this questionnaire in primary care settings. Furthermore, instead of monitored PSG in a sleep laboratory, they used the home portable sleep monitoring for the validation of the BQ. A recent validation study by Sharma et al. reported that the high-risk category was defined by the modified BQ predicted an AHI > 5 with a sensitivity of 86 % and specificity of 95 % [11]. This higher accuracy of the modified BQ than that of our results might be due to the fact that the subjects in their study were selected only from those patients who visited a tertiary level referral hospital. Since the patients with more severe illnesses are commonly referred to the hospital by their general practitioners and this results in an enriched risk factor profile for sleep apnea, the prevalence of OSA is probably higher among the patients in the tertiary level hospital than those in the general population and its severity is also likely to be higher among the patients in the tertiary level hospital. Only 26 (25.7 %) of 101 subjects who underwent overnight PSG had an AHI ≥ 15 in our study, whereas 50 (48 %) and 38 (37 %) of 104 subjects who underwent PSG in an Indian study had an AHI > 15 and an AHI > 30, respectively [11]. Therefore, to use the KBQ in public health care, it should be validated using overnight PSG at the controlled sleep laboratory targeting the general population.
The Cronbach’s α value was evaluated in our study to assess internal reliability between responses in each category of the KBQ. The Cronbach’s α value was 0.78 for category 1 and 0.64 for category 2. However, if the question about sleepiness while driving was excluded, the Cronbach’s α value for category 2 increased to 0.82. The same phenomenon had been previously demonstrated in the original validation study of the BQ [12]. The Cronbach’s α value was 0.63 for correlation of questions within category 2 and when the question about drowsy driving was excluded, the Cronbach’s α value in category 2 increased to 0.86 [12]. This question might be associated with the lower internal consistency. The subject who was a nondriver could respond saying that “I haven’t ever nodded off or fallen asleep while driving a vehicle.” The KBQ showed relatively good internal consistency, although the Cronbach’s α value was slightly lower than those of previous studies [11, 12]. Additionally, the reproducibility of the KBQ was excellent in our study.
According to the risk categorization based on the KBQ in our study, as many as 340 (26.1 %) of the 1,305 subjects were in the high-risk group for sleep apnea. Considering the good validity of the KBQ in our study, this result is noteworthy because the prevalence of SDB inferred from the KBQ seems to be relatively similar to that in the well-designed and extensive prevalence study of SDB in Korea [7]. In their study, a random sample of 457 men and women among a total of 5,020 adults aged between 40 and 69 years was studied with use of full overnight PSG to determine the prevalence of SDB, and it was reported that the prevalence of SDB (defined as AHI ≥ 5) was 27 % in men and 16 % in women in Korea [7].
The key strengths of our study include its population-based sample with relatively high participation, minimizing selection bias. It is assumed that the reason for the low dropout rate obtained with our questionnaire is because of our door-to-door survey method. Also, our study is different from all the previous studies associated with the validation of the BQ especially with respect to the study population. However, our study was limited by a relatively large dropout rate and small number of participants having the PSG data because of its inconveniences. Also, we performed a single-night PSG in this study. Several studies suggest that the night-to-night variability might affect the detection of respiratory abnormalities [19, 20]. It is possible that there are the first night effects on sleep and respiratory parameters [21]. However, the first night effects seem to vary in different disease states, for instance, the respiratory parameters showed little variability between the first and second nights in epilepsy patients with OSA [22].
In summary, the KBQ showed relatively good internal consistency and excellent test–retest reliability in our study. Also, the AHI derived from the PSG was significantly correlated with the scores of the KBQ. The high-risk group based on the KBQ predicted an AHI ≥ 5 with a sensitivity of 69 % and specificity of 83 %. The prevalence of OSA inferred from the KBQ seems to be relatively similar to that in the previous large epidemiological study using full overnight PSG. In conclusion, considering the convenience and economic feasibility of the questionnaire, the BQ might be utilized as a useful screening tool for OSA by prioritizing subjects at high risk for OSA in the general population.
References
Weinreich G, Plein K, Teschler T, Resler J, Teschler H (2006) Is the Berlin questionnaire an appropriate diagnostic tool for sleep medicine in pneumological rehabilitation? Pneumologie 60:737–742
American Academy of Sleep Medicine (2005) International classification of sleep disorders: diagnostic and coding manual, 2nd edn. American Academy of Sleep Medicine, Westchester
Nieto FJ, Young TB, Lind BK, Shahar E, Samet JM, Redline S, D’Agostino RB, Newman AB, Lebowitz MD, Pickering TG (2006) Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 283:1829–1836
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342:1378–1384
Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V (2005) Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 353:2034–2041
Babu AR, Herdegen J, Fogelfeld L, Shott S, Mazzone T (2005) Type 2 diabetes, glycemic control, and continuous positive airway pressure in obstructive sleep apnea. Arch Intern Med 165:447–452
Kim J, In K, Kim J, You S, Kang K, Shim J, Lee S, Lee J, Lee S, Park C, Shin C (2004) Prevalence of sleep-disordered breathing in middle-aged Korean men and women. Am J Respir Crit Care Med 170:1108–1113
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Ohayon MM, Guilleminault C, Priest RG, Caulet M (1997) Snoring and breathing pauses during sleep: telephone interview survey of a United Kingdom population sample. BMJ 314:860–863
Young T, Evans L, Finn L, Palta M (1997) Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep 20:705–706
Sharma SK, Vasudev C, Sinha S, Banga A, Pandey RM, Handa KK (2006) Validation of the modified Berlin questionnaire to identify patients at risk for the obstructive sleep apnoea syndrome. Indian J Med Res 124:281–290
Netzer NC, Stoohs RA, Netzer CM, Clark K, Strohl KP (1999) Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131:485–491
Ahmadi N, Chung SA, Gibbs A, Shapiro CM (2008) The Berlin questionnaire for sleep apnea in a sleep clinic population: relationship to polysomnographic measurement of respiratory disturbance. Sleep Breath 12:39–45
Dement WC, Netzer NC (2000) Primary care: is it the setting to address sleep disorders? [published erratum appears in Sleep Breath 2000;4:187-92]. Sleep Breath 4:1–9
World Health Organization (WHO) Regional Office for the Western Pacific/International Association for the Study of Obesity/International Obesity Task Force (2000) The Asia-Pacific perspective: redefining obesity and its treatment. Health Communications Australia, Sydney, Australia
Iber C, Ancoli-Israel S, Chesson A, Quan S (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. American Academy of Sleep Medicine, Westchester
Mok WY, Lam CL, Lam B, Cheung MT, Yam L, Ip MS (2004) A Chinese version of the Sleep Apnea Quality of Life Index was evaluated for reliability, validity, and responsiveness. J Clin Epidemiol 57:470–478
Wiegand L, Zwillich CW (1994) Obstructive sleep apnea. Dis Mon 40:197–252
Redline S, Tosteson T, Boucher MA, Millma RP (1991) Measurement of sleep-related breathing disturbances in epidemiologic studies. Assessment of the validity and reproducibility of a portable monitoring device. Chest 100:1281–1286
Bliwise DL, Benkert RE, Ingham RH (1991) Factors associated with nightly variability in sleep-disordered breathing in the elderly. Chest 100:973–976
Agnew HW Jr, Webb WB, Williams RL (1966) The first night effect: an EEG study of sleep. Psychophysiology 2:263–266
Selwa LM, Marzec ML, Chervin RD, Weatherwax KJ, Vaughn BV, Foldvary-Schaefer N, Wang L, Song Y, Malow BA (2008) Sleep staging and respiratory events in refractory epilepsy patients: is there a first night effect? Epilepsia 49:2063–2068
Acknowledgments
This research was supported by a grant of Korea Centers for Disease Control and Prevention, Republic of Korea (2009-E33029-00) and by Kyungpook National University Research Fund, 2012.
Conflict of interest
This was not an industry-supported study. The authors have indicated no financial conflicts of interest. There is no off-label or investigational use in this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Kyunghun Kang and Ki-Soo Park contributed equally to this work.
Appendix. The Korean version of Berlin Questionnaire
Appendix. The Korean version of Berlin Questionnaire

Rights and permissions
About this article
Cite this article
Kang, K., Park, KS., Kim, JE. et al. Usefulness of the Berlin Questionnaire to identify patients at high risk for obstructive sleep apnea: a population-based door-to-door study. Sleep Breath 17, 803–810 (2013). https://doi.org/10.1007/s11325-012-0767-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-012-0767-2