Abstract
The aim of this study was to assess the utility of the Berlin questionnaire (BQ) in adult patients at high risk of obstructive sleep apnea (OSA). The study consisted of 64 patients recruited for the polysomnography diagnostics of sleep respiratory disturbances. The anthropometric assessment included body weight, height, and body mass index (BMI), all related to the risk of OSA. The BQ consisted of the following three categories: 1 – snoring, 2 – daytime somnolence, and 3 – hypertension. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were evaluated. Likelihood ratio was used to assess the diagnostic accuracy. We found that patients were, on average obese; the mean BMI amounted to 31.9 ± 6.0 kg/m2. Polysomnography identified OSA in 73.4% of patients (AHI >5), where the BQ categorized 87.5% of patients at high risk of OSA. Sensitivity of the BQ was 87.2%, specificity 11.8%, PPV 73.2%, and NPV 25.0%. Diagnostic accuracy assessed by the likelihood ratio had a value of 1.00. The BQ had a false discovery rate of 31.2% and misclassification rate of 32.8%. We conclude that the BQ is a sensitive tool that should be used in clinical settings in which the benefit of high sensitivity outweighs the disadvantage of low specificity.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Apnea-hypopnea index
- Diagnostic tool
- Hypertension
- Obesity
- Obstructive sleep apnea
- Polysomnography
- Questionnaire
- Sleep disordered breathing
1 Introduction
Obstructive sleep apnea (OSA) is a condition which typically requires lengthy and complex polysomnographic diagnostics (AASM 1999). The apnea-hypopnea index (AHI) forms the basis for the diagnosis and stratifies patients into mild (5.0–14.9), moderate (15.0–29.9), or severe (≥30.0) apnea-hypopnea events taking longer than 10 s per hour of sleep (Foster et al. 2009). The Berlin questionnaire (BQ) is a screening tool that captures OSA symptoms to identify patients at high risk of OSA (Enciso and Clark 2011) before going through a polysomnographic examination. It consists of 11 items that include such factors as snoring, wake-time sleepiness, fatigue, obesity, and elevated blood pressure (Ahmadi et al. 2008). The BQ is thought of as a suitable substitute for polysomnography that is uncomfortable for patients and pricey for healthcare services. Screening approaches, like rapid tests and questionnaires, are often used to facilitate clinicians’ decisions of whether to subject a patient to more complex or invasive diagnostic procedures.
Clinical utility of the BQ has been recently questioned (Cowan et al. 2014; Iber et al. 2007). Therefore, in the present study we set out to assess the utility of this questionnaire in adult patients at high risk of OSA.
2 Methods
2.1 Study Population
The experimental protocol was approved by the Bioethics Committee of Poznan University of Medical Sciences. The study was performed in accordance with the Helsinki Declaration for Human Research. Written informed consent was obtained from all the subjects who agreed to participate in the study.
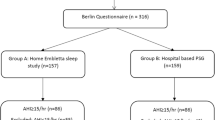
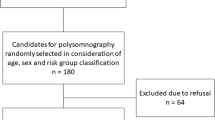
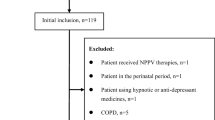
One hundred fifty three patients were screened due to a suspicion of OSA symptoms. Of that group, we qualified 64 individuals for admission to the Department of Pulmonology, Allergology and Respiratory Oncology at the Poznan University of Medical Sciences in Poland for the diagnostics of sleep-related respiratory disturbances. Patients were included in the study if they were over 18 years of age, had symptoms of OSA, were willing to participate in the study, and were on a habitual diet during the period of examination. The exclusion criteria included: pregnancy or lactation, cancer (excluding curatively treated with no evidence of disease for 5 years), severe liver and kidney diseases, and the diagnosed cardiovascular diseases such as myocardial infarct, stroke, or angina pectoris. Any active drug abuse, legal incompetence, and limited legal incompetence were additional exclusion criteria. Medical history, comorbidities, concomitant medications were recorded in the electronic database.
2.2 Assessment of Obstructive Sleep Apnea
Overnight polysomnography was used as a standard method for OSA diagnosis (Embla 4500; Beth Israel Deaconess Medical, Boston, MA). The recommendations of the American Academy of Sleep Medicine (AASM) (Oku and Okada 2008) regarding filters, sample signal rates, and configuration were followed. A respiratory flow trace was provided via a nasal cannula equipped with a thermistor. The thoraco-abdominal motion was recorded with piezoelectric bands. Oxygen saturation was measured with a pulse oximeter. Apnea was defined as a cessation of airflow for at least 10 s and hypopnea as an at least 80% reduction in airflow amplitude for at least 10 s (Sert Kuniyoshi et al. 2011). The AHI was defined as the total apneas plus hypopneas during total time asleep, divided by the number of hours asleep.
The BQ consists of three categories (category 1 – snoring, category 2 – daytime somnolence, category 3 – hypertension and body mass index (BMI)); all related to the risk of having sleep apnea. The BQ score was assessed based on the responses to ten questions from the three categories. Scores from the first and second category were assessed positively if the patient indicated frequent symptoms (>3–4 times/week). The score from the third category was positively evaluated when a history of hypertension or BMI >30 kg/m2 was reported. If patients had a positive score in two or more categories, they were classified as being at high-risk for OSA. If only one or none category was scored positively, patients were classified being at low-risk (Cole 1990). Polysomnography and BQ were administered at the patient’s first visit in the clinic.
Blood pressure (BP) was measured with a digital electronic tensiometer (Omron, Kyoto, Japan) after a resting period of 10 min. The mean of three consecutive measurements performed in the non-dominant arm at 3-min intervals was taken as the end-result. Regular or large adult cuffs were used, depending on the arm circumference of patients. BP measurements were performed in accordance with the guidelines of the European Society of Hypertension (Mancia et al. 2014).
2.3 Assessment of Covariates
Data on age, sex, smoking, educational status, and anthropometry were collected at the time of enrollment in the study using study-specific data collection tools. Anthropometric assessments included the measurement of weight and height. Weight was measured in light clothes without shoes and recorded to the nearest 100 g. Height was assessed in a similar manner to the nearest 1 cm. BMI was calculated to determine the degree of obesity (Netzer et al. 1999).
2.4 Statistical Analysis
Continuous variables were described as means ±SD, while categorical variables were described as percentages. Sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were evaluated. The likelihood ratio was used to assess the diagnostic accuracy. A p-value of less than 0.05 defined statistically significant changes All analysis were performed using SAS(R) 9.4 (Enterprise guide 6.1).
3 Results
The mean age of study participants was 56.6 ± 10.6 years and the mean BMI of 31.9 ± 6.1 kg/m2 pointed to the prevailing obesity. Over 60% of subjects were smokers, and more than 50% had high school education (Table 1).
Polysomnography identified 73.4% of the patients as having OSA (AHI >5), while the BQ categorized 87.5% of the patients as of high risk for OSA. There was no significant difference in the mean BMI value between OSA and non-OSA subjects identified according to the AHI value. However, BMI of subjects identified by the BQ as OSA was significantly higher than that of non-OSA subjects (Table 2). Moreover, a higher number of patients with OSA were identified by the BQ as hypertensive in comparison to the standard blood pressure measurement (Fig. 1).
Sensitivity of the BQ was 87.2%, specificity was 11.8%, positive predictive value (PPV) was 73.2%, and a negative predictive value (NPV) was 25.0%. Diagnostic accuracy assessed by the likelihood ratio had a value of 1.0. The BQ provided a false discovery rate of 31.2% and a misclassification rate of 32.8% (Table 3).
4 Discussion
This study demonstrates that the BQ has a high sensitivity but low specificity and low positive predictive value. Moreover, BQ has a high misclassification rate and its diagnostic accuracy is no different than a random chance. Our findings corroborate the results of Netzer et al. (1999) concerning the sensitivity of BQ, but not specificity, positive predictive value, and the likelihood ratio, all of which were greater in high risk patients in the study of those authors, amounting to 77%, 87%, and 3.2, respectively.
In general, BQ has expectedly high sensitivity, as this tool has been developed for identifying high risk patients at the primary care level. However, low specificity and high misclassification rate suggest that BQ has a low discriminatory power and its utility is no different than the judgement of clinicians (Cowan et al. 2014; Sert Kuniyoshi et al. 2011). The present findings also support earlier studies showing that the BQ is of limited utility in specialized clinics (Ahmadi et al. 2008). Currently, clinicians look for a simple questionnaire that may be used as a tool to determine the risk of OSA syndrome and to predict the possible perioperative respiratory complications. The latter may improve clinical outcome when anesthesia and surgery are required (Gokay et al. 2016). The data from recently published systematic review suggest that the BQ is a questionnaire that enables to risk stratify patients for peri- and postoperative complications. However, testing of BQ is still required with a focus on specific surgery types, adjusted for potentially confounding factors (Dimitrov and Macavei 2016). A higher score of BQ in specific groups of patients after stroke or transient ischemic attack indicates that this tool is but moderately predictive for OSA exclusion (Boulos et al. 2016). It patients suffering from type 2 diabetes, BQ fails to identify 31% of patients with moderate-to-severe OSA, preventing such patients from receiving correct diagnosis and treatment. However, BQ may be suboptimal when OSA screening is done with home sleep monitoring devices (Westlake et al. 2016). An evaluation of BQ in Iranian patients with AHI >5 shows its sensitivity and specificity for OSA diagnosis as 77.3% and 23.1%, respectively, PPV of 68.0%, and NPV of 22.0% (Khaledi-Paveh et al. 2016), which is akin to present findings in the Polish population. The BQ has also been tested in Portuguese patients in whom it shows an acceptable reliability, but after excluding the following two questions: ‘Has anyone noticed that you stop breathing during your sleep?’ and ‘Have you ever dozed off or fallen asleep while driving?’ (Silva et al. 2016). Arunsurat et al. (2016) have assumed that the BQ may be useful as an OSA screening tool for the Thai or Asian populations after some adjustments. In addition, there is an apparent paucity of BQ testing in population samples comprising women and individuals of a low educational level (Silva et al. 2016). Interestingly, Gupta et al. (2016), in view of the unavailability of any screening tool for OSA in Hindi, have undertaken an attempt to explore the validity of a Hindi version of BQ, irrespective of the literacy status of subjects. The results have demonstrated sensitivity of 89%, specificity of 58%, PPV of 87%, and NPV of 63%, which supports the role of BQ as a valid tool for OSA screening OSA in that population. There is also a need to use simple tools for OSA screening in Africa, where the awareness of OSA is poor and its incidence is underreported, despite a high prevalence of symptoms (Desalu et al. 2016).
The current practice model of screening and assessment for OSA in primary care seems fragmented and ineffective (Miller and Berger 2016). Primary care providers encounter patients with OSA symptoms but do not routinely screen, assess, or refer to a sleep specialist. The present study contributes to the existing evidence that the BQ is not a reliable instrument to discriminate between high and low risk patients. Therefore, professionals should be exercised in the knowledge of using the BQ for mass screening since this tool is neither a perfect substitute to polysomnography in diagnosing OSA and predicting its course nor is it of perfect research utility as its application should be addressed to specific populations. In addition, since one-third of the score is assigned to hypertension or obesity, the misclassification of OSA cases among hypertensive and obese patients might be high. A low accuracy of BQ in identifying OSA patients has been confirmed by Margallo et al. (2014) in a large cohort of resistant hypertensive patients. Thurtell et al. (2011) have validated the BQ as a screening tool for OSA in idiopathic intracranial hypertension patients and found that only a low-risk BQ score identifies such hypertensive patients who are unlikely to have OSA. Therefore, other protocols need to be developed to improve diagnostic accuracy in such patients.
In conclusion, the BQ is a sensitive tool that should be used in the setting in which the benefits of high sensitivity outweigh the disadvantage of low specificity. Further research is needed to improve specificity and accuracy of screening tools for OSA.
References
AASM (1999) American Academy of Sleep Medicine European Respiratory Society Australasian Sleep Association American Thoracic Society Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research: the report of an American Academy of Sleep Medicine Task Force. Sleep 22:667–689
Ahmadi N, Chung SA, Gibbs A, Shapiro CM (2008) The Berlin questionnaire for sleep apnea in a sleep clinic population: relationship to polysomnographic measurement of respiratory disturbance. Sleep Breath 12(1):39–45
Arunsurat I, Luengyosluechakul S, Prateephoungrat K, Siripaupradist P, Khemtong S, Jamcharoensup K, Thanapatkaiporn N, Limpawattana P, Laohasiriwong S, Pinitsoontorn S, Boonjaraspinyo S, Sawanyawisuth K (2016) Simplified Berlin questionnaire for screening of high risk for obstructive sleep apnea among Thai male healthcare workers. J UOEH 38(3):199–206
Boulos MI, Wan A, Im J, Elias S, Frankul F, Atalla M, Black SE, Basile VS, Sundaram A, Hopyan JJ, Boyle K, Gladstone DJ, Murray BJ, Swartz RH (2016) Identifying obstructive sleep apnea after stroke/TIA: evaluating four simple screening tools. Sleep Med 21:133–139
Cole TJ (1990) The LMS method for constructing normalized growth standards. Eur J Clin Nutr 44:45–60
Cowan DC, Allardice G, Macfarlane D, Ramsay D, Ambler H, Banham S, Livingston E, Carlin C (2014) Predicting sleep disordered breathing in outpatients with suspected OSA. BMJ 4(4):e004519
Desalu O, Onyedum C, Sanya E, Fadare J, Adeoti A, Salawu F, Oluyombo R, Olamoyegun M, Fawale M, Gbadegesin B, Bello H (2016) Prevalence, awareness and reporting of symptoms of obstructive sleep apnoea among hospitalized adult patients in Nigeria: a multicenter study. Ethiop J Health Sci 26(4):321–330
Dimitrov L, Macavei V (2016) Can screening tools for obstructive sleep apnea predict postoperative complications? A systematic review of the literature. J Clin Sleep Med 12(9):1293–1300
Enciso R, Clark GT (2011) Comparing the Berlin and the ARES questionnaire to identify patients with obstructive sleep apnea in a dental setting. Sleep Breath 15(1):83–89
Foster GD, Borradaile KE, Sanders MH, Millman R, Zammit G, Newman AB, Wadden TA, Kelley D, Wing RR, Pi-Sunyer FX, Reboussin D, Kuna ST, Sleep AHEAD Research Group of Look AHEAD Research Group (2009) A randomized study on the effect of weight loss on obstructive sleep apnea among obese patients with type 2 diabetes: the Sleep AHEAD study. Arch Intern Med 169(17):1619–1626
Gupta R, Ali R, Dhyani M, Das S, Pundir A (2016) Hindi translation of Berlin questionnaire and its validation as a screening instrument for obstructive sleep apnea. J Neurosci Rural Pract 7(2):244–249
Gokay P, Tastan S, Orhan ME (2016) Is there a difference between the STOP-BANG and the Berlin obstructive sleep apnoea syndrome questionnaires for determining respiratory complications during the perioperative period? J Clin Nurs 25(9–10):1238–1252
Iber C, Ancoli-Israel S, Chesson A, Quan SF (2007) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, 1st edn. American Academy of Sleep Medicine, Westchester
Khaledi-Paveh B, Khazaie H, Nasouri M, Ghadami MR, Tahmasian M (2016) Evaluation of Berlin questionnaire validity for sleep apnea risk in sleep clinic populations. Basic Clin Neurosci 7(1):43–48
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M et al (2014) Task Force for the Management of Arterial Hypertension of the European Society of Hypertension and the European Society of Cardiology. 2013 ESH/ESC Practice Guidelines for the Management of Arterial Hypertension. Blood Press 23(1):3–16
Margallo VS, Muxfeldt ES, Guimarães GM, Salles GF (2014) Diagnostic accuracy of the Berlin questionnaire in detecting obstructive sleep apnea in patients with resistant hypertension. J Hypertens 32(10):2030–2036
Miller JN, Berger AM (2016) Screening and assessment for obstructive sleep apnea in primary care. Sleep Med Rev 29:41–51
Netzer NC, Stoohs SA, Netzer CM, Clark K, Strohl KP (1999) Using the Berlin questionnaire to identify patients at risk for the sleep apnea syndrome. Ann Intern Med 131(7):485–491
Oku Y, Okada M (2008) Periodic breathing and dysphagia associated with a localized lateral medullary infarction. Respirology 13(4):608–610
Sert Kuniyoshi FH, Zellmer MR, Calvin AD, Lopez-Jimenez F, Albuquerque FN, van der Walt C, Trombetta IC, Caples SM, Shamsuzzaman AS, Bukartyk J, Konecny T, Gami AS, Kara T, Somers VK (2011) Diagnostic accuracy of the Berlin questionnaire in detecting sleep-disordered breathing in patients with a recent myocardial infarction. Chest 140(5):1192–1197
Silva KV, Rosa ML, Jorge AJ, Leite AR, Correia DM, Silva Dde S, Cetto DB, Brum Ada P, Silveira Netto P, Rodrigues GD (2016) Prevalence of risk for obstructive sleep apnea syndrome and association with risk factors in primary care. Arq Bras Cardiol 106(6):474–480
Thurtell MJ, Bruce BB, Rye DB, Newman NJ, Biousse V (2011) The Berlin questionnaire screens for obstructive sleep apnea in idiopathic intracranial hypertension. J Neuroophthalmol 31(4):316–319
Westlake K, Plihalova A, Pretl M, Lattova Z, Polak J (2016) Screening for obstructive sleep apnea syndrome in patients with type 2 diabetes mellitus: a prospective study on sensitivity of Berlin and STOP-Bang questionnaires. Sleep Med. doi:10.1016/j.sleep.2016.07.009
Acknowledgements
The authors are grateful to Dr. Robert Tower for proofreading of the manuscript.
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Stelmach-Mardas, M., Iqbal, K., Mardas, M., Kostrzewska, M., Piorunek, T. (2017). Clinical Utility of Berlin Questionnaire in Comparison to Polysomnography in Patients with Obstructive Sleep Apnea. In: Pokorski, M. (eds) Respiratory System Diseases. Advances in Experimental Medicine and Biology(), vol 980. Springer, Cham. https://doi.org/10.1007/5584_2017_7
Download citation
DOI: https://doi.org/10.1007/5584_2017_7
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-59497-2
Online ISBN: 978-3-319-59498-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)