Abstract
Introduction
Heart failure (HF) is a major public health problem associated with high rates of morbidity and mortality. Patients with HF exhibit a high prevalence of sleep-disordered breathing (SDB). We have investigated the long-term impact of positive airway pressure (PAP) therapy on heart function and clinical outcomes in patients with advanced HF and concomitant SDB.
Materials and methods
We assessed 18 patients with advanced HF (New York Heart Association (NYHA) functional classification III–IV) and concomitant SDB (diagnosed with polysomnography) either of obstructive or central type. Eleven patients who received PAP therapy (auto-titrating PAP or adaptive servo-ventilation) for 12 months were compared with seven patients who refused this therapy. All participants were assessed at both baseline and end of follow-up for NYHA functional status, left and right ventricular function, neurohormonal activation, and exercise tolerance. The rates of hospitalization, deaths, and the combination of both were also recorded.
Results
Patients treated with PAP achieved better functional status, higher left ventricular ejection fraction, improved longitudinal right ventricular contractile function, lower levels of b-type natriuretic peptide, and greater exercise performance compared to those who remained untreated. PAP-treated group had a significantly lower incidence of the prespecified combined end-point (i.e., hospital admissions and death) than the control group (87.5 vs. 18.2%, p = 0.013). Interestingly, the mortality rate was 28% (two out of seven patients) in the control group, while no deaths were recorded in the PAP-treated group.
Discussion
In this preliminary study, we found that treatment of SDB, irrespective of type, in stable patients with advanced HF receiving optimal medical therapy was associated with improvement in cardiac functional status, ventricular contraction, physical performance, and neurohormonal status, leading to better clinical outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Heart failure (HF) is a common clinical entity with increasing prevalence and high rates of morbidity and mortality [1, 2]. Repeated admissions and excessive use of health care resources are major concerns linked to HF since advances in medical therapy have only partially improved the clinical outcomes in HF patients [3].
It has been recognized that sleep-disordered breathing (SDB) presenting either as obstructive sleep apnea (OSA) or central sleep apnea (CSA) with or without Cheyne–Stokes respiration (CSR) is common in patients with HF with the former described in 11–40% and the latter in 25–40% of chronic HF patients [4–7]. Both types of SDB have been related to poor prognosis in HF syndrome and may lead to progression of the disease through several pathophysiological pathways, such as intermittent hypoxia, increased sympathetic activity, endothelial dysfunction, oxidative and inflammatory stress, or coagulopathy [8–10].
Treatment of SDB has recently emerged as a novel treatment modality in patients with end-stage HF [11]. Several studies have shown short-term improvement of heart function after treatment with various forms of positive airway pressure (PAP), such as continuous positive airway pressure (CPAP), bi-level pressure or adaptive servo-ventilation (ASV), in both types of SDB [11, 12]. Especially in the presence of CSR, the use of ASV has been shown to be the most effective mode of treatment of CSA in HF patients [13]. Auto-titrating positive airway pressure (APAP) is a mode of PAP therapy of OSA with similar efficacy to fixed pressure CPAP and associated with better compliance of patients to therapy [14, 15]. However, it has not been extensively investigated in HF patients [16, 17]. Moreover, there is not enough evidence currently available concerning the long-term effects of SDB treatment on cardiac status and the quality of life in HF patients, thus preventing the routine referral of these patients to sleep centers for the evaluation and treatment of SDB [12].
In this study, we investigated the long-term impact of positive airway pressure therapy (APAP or ASV) on heart function and clinical outcomes in patients with advanced HF irrespective of the type of SDB.
Materials and methods
Patients and study design
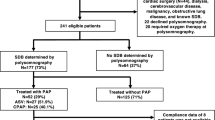
This is a prospective, non-randomized investigation in a tertiary hospital setting. Eligible patients were those with chronic HF aged between 18 and 80 years, with ejection fraction (EF) below 40% and functional class III or IV according to the New York Heart Association (NYHA) criteria. All patients were clinically stable for at least 3 months and were receiving maximal medical therapy according to the current chronic HF guidelines [18]. Exclusion criteria included HF from other cause than ischemic or dilated heart disease, unstable angina, myocardial infarction in the previous 6 months, severe valvular heart disease, neurological disorders, lung diseases requiring supplemental oxygen therapy, hospitalization in the last 3 months for HF decompensation, and known uncontrolled malignancy. All eligible patients were recruited for evaluation of concomitant SDB in the sleep laboratory irrespectively of clinical symptoms related to sleep apnea. Patients who were diagnosed as having SDB (with either predominant obstructive or central respiratory events) were assigned to treatment with APAP in the case of predominant OSA, or with ASV in the case of predominant CSA either with or without CSR. Patients who refused to receive PAP therapy after detailed explanation of the method were shifted into the control group (Fig. 1), whereas subjects who were non-compliant with therapy were excluded from the final analysis.
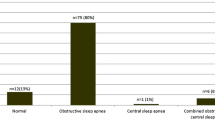
Between February 2006 and December 2008, 29 patients were eligible according to inclusion criteria. Among them, six did not have any kind of SDB while 23 patients were diagnosed as having predominant OSA or predominant CSA/CSR. Seven patients who refused PAP therapy after a 2-week trial of therapy were treated only with optimal medical therapy and classified as the control group. Reasons of refusing therapy were the development of mask claustrophobia, discomfort and no subjective perception of improvement. Among patients who agreed to receive PAP therapy (i.e., 16), two were lost from follow-up and, hence, were excluded from analysis along with three patients who did not have good compliance to therapy. Finally, our study population consisted of 18 patients (13 men, aged 68.9 ± 10.19 years) with 11 of them receiving PAP therapy (six patients on ASV and five on APAP) along with optimal medical therapy, and the remaining seven patients (control group) receiving optimal medical therapy only (Fig. 1).
At baseline all patients enrolled, underwent thorough clinical evaluation and laboratory tests including conventional echocardiography and Doppler tissue imaging (DTI) study, comprehensive full night polysomnography (PSG), 6-min walking test (6-MWT), b-type natriuretic peptide (BNP) measurement, and standard blood tests. Follow-up was repeated every 2 months over a period of 12 months. Bimonthly follow-up included cardiological clinical examination and clinical evaluation of HF symptoms, adjustment of medical therapy as needed and assessment of compliance to PAP treatment by using data downloaded from APAP or ASV devices. Adequate compliance was defined as use of the device more than 4 h per night on at least 70% of nights of the follow-up period. Deaths and hospitalizations due to decompensation of HF during the observation period were also recorded. Patients admitted and discharged alive were categorized as a hospitalization, whereas those that died in the hospital as a death. After 12 months all baseline laboratory tests were repeated.
The study was approved by the ethics committee of our institution and patients signed a written informed consent before inclusion in the study.
PSG and PAP therapy
Full overnight PSG according to standard techniques included monitoring of central and occipital channels of electroencephalogram (C4-A1, C3-A2, O1-A2, and O2-A1), electrooculogram, and submental and anterior electromyograms. Electrocardiogram and heart rate were monitored using the standard limb leads. Airflow was detected by monitoring airflow through a thermistor and a nasal pressure transducer. Respiratory efforts were monitored with piezoelectric transducers placed around the chest and abdomen. Arterial oxygen saturation (SaO2) was measured continuously by pulse oximetry using a finger probe. Body position was assessed with a body position sensor. All variables were recorded on a computerized system (Alice 5; Healthdyne; Marietta, GA).
PSG recordings were manually scored over 30-s periods, according to the current (2007) guidelines of the American Academy of Sleep Medicine [19, 20]. Apnea was defined as the reduction in airflow of ≥ 90% of baseline, lasting for at least 10 s. It was classified as an obstructive apnea when associated with the presence of an inspiratory effort, as central apnea in the absence of an inspiratory effort, or, as mixed apnea if inspiratory effort was absent in the initial part of the event and present at the final part. Hypopnea was defined as the reduction in baseline airflow of ≥ 30% with a ≥ 4% desaturation, lasting for at least 10 s. The apnea/hypopnea index (AHI) was calculated as the number of apnea and hypopnea events per hour of sleep. Clinically significant OSA was defined as an AHI > 10 events per hour. CSA/CSR was diagnosed when the AHI was >10 and central apneas represented more than 70% of the respiratory events with the presence of CSR (characteristic pattern of periodic crescendo–decrescendo in airflow amplitude). PSG scoring was made by the same sleep technician under the supervision of an experienced physician in sleep medicine who was responsible for the interpretation of the sleep studies.
Patients diagnosed with SDB underwent a second night of full PSG for application of PAP therapy using an APAP or ASV device. Patients with predominant OSA were offered an APAP device which automatically adjusts the therapeutic pressure based on a titration algorithm. The monitoring of the efficacy of treatment was supervised by a sleep technician in order to avoid excess pressure delivery, and thus, preventing the appearance of PAP-induced central events which would be undesirable in HF patients. The settings of APAP were between 5 and 8 cmH2O for minimum pressure and 10–14 cmH2O for maximum pressure. Patients with predominant CSA/CSR were offered ASV after manually titration of therapeutic pressures. On ASV, the end- expiratory pressure was set at 4–8 cmH2O in order to eliminate obstructive events, minimum support was set at 4 cm H2O and maximum support at 10 cm H2O using a device that automatically tracks the respiratory rate of patient under monitoring of heart rate and blood pressure. The target was to reduce the AHI < 10 and eliminate CSR.
All patients assigned to PAP therapy underwent an initial daytime education on PAP treatment before the second PSG and offered a 2-week trial period before inclusion in the study. They were instructed to use their PAP device at least 6 h per night and support was provided by the sleep laboratory personnel in case of any problems throughout the study period. Compliance with PAP therapy was evaluated by downloading usage data from the PAP devices.
Echocardiographic methods
-
1.
Standard transthoracic examination
Conventional echocardiographic examination was performed early in the morning with a commercially available imaging system (SSA-380A Toshiba Powervision-Japan) using a 2.5-MHz phased array transducer employing second harmonic imaging. All studies were performed and interpreted by the same experienced physician who had Level 3 echocardiographic training as defined by the American College of Cardiology/American Heart Association [21], and was unaware of the patients’ subgroup. Left ventricular ejection fraction (LVEF) was assessed with the biplane Simpson’s method using conventional apical 4- and 2-chamber views. Using conventional pulse wave Doppler, the peak early velocity (E) of the transmitral flow was measured. The two-dimensional echocardiographic study of the RV was performed from the four-chamber view, and the following parameters were measured at end-diastole: Tricuspid annular diameter was measured between the hinge points of the leaflets with the lateral wall and the septum (RVD1). Mid-cavity diameter was also measured at the 4-chamber view (RVD2). Pulmonary artery systolic pressure (PASP) was determined using the modified Bernoulli equation (P = 4 × V2 + right atrial pressure). The use of the inferior vena cava size and dynamics was applied for estimation of the right atrial pressure [22].
-
2.
Pulse wave DTI study
After establishing the resting baseline measurements, a pulse wave DTI study was accomplished, as previously described [23, 24]. From the apical four-chamber view a 5 mm pulsed Doppler sample volume for DTI was positioned just apical to the RV free wall at the level of the tricuspid valve. Every effort was made to obtain a Doppler angle of incidence close to 0-degrees between the interrogating Doppler beam and the longitudinal motion of the RV, to adjust the sample volume size proportionally to annular motion and to obtain recordings at end-expiratory apnea. The peak systolic myocardial velocity at the tricuspid level (SmRV) was measured. Moreover, the average peak early diastolic velocity (E’) from the septal and lateral mitral annulus was recorded. The value assigned to each parameter was the average of five cycles. In addition, the ratio E/E’ was also calculated.
B-type natriuretic peptide
Venous blood for BNP measurement was drawn and was immediately analyzed using Triage® System for BNP (Biosite diagnostics, La Jolla, CA, USA), a test based on fluorescence immunoassay. This test has a range of 5–5,000 pg/mL, with an average 95% analytical sensitivity of 0.2–4.8 pg/mL. Coefficients of variation are 10.1%, 12.4%, and 16.2% for mean values 28.8, 584.4, and 1,080.4 pg/mL. The median value of three consecutive readings of the same test device was used for the final analysis.
Six-minute walking test
The 6-MWT was performed to evaluate clinically the functional status of HF patients according to a standardized test procedure [25]. In brief, patients were asked to walk around a walking track for 6 min and the distance covered was measured. The test was self-paced, and the patient was allowed to rest if needed.
Statistical analysis
Continuous variables are expressed as the mean ± SD or medians (interquartile range) for skewed data and categorical variables as percentages. Comparisons of the continuous variables between groups were made using the t test or Mann–Whitney U statistical test, as appropriate. Associations between two categorical variables were tested by the chi-square test. All tests were two-tailed, and p < 0.05 was considered significant. Statistical analysis was performed with Statistical Package for Social Sciences software (release 15.0, SPSS, Inc., Chicago, Illinois).
Results
Patients’ characteristics-PSG study
The demographic characteristics and PSG findings of the patients enrolled are shown in Table 1. As shown in the latter table no statistically significant differences were detected between treatment and control group regarding age, weight, height, and body mass index. Comparison of PSG findings between the two groups showed that PAP-treated group had a marginally greater number of obstructive respiratory events than the control group (p = 0.056). No significant differences between groups were found for the rest of the variables assessed.
The mean nightly usage of PAP therapy was 4.5 ± 1.3 h per night at the end of follow-up period (i.e., 12 months) without a significant difference between those who used APAP and ASV. Eight out of 11 patients (i.e.73%) were compliant with treatment as defined by use of PAP more than 4 h during more than 70% of nights. Patients with mean usage of less than 2 h or use in less than 50% of nights were excluded from the final analysis.
Evaluation of cardiac status
-
1.
Baseline data
As shown in Table 2 baseline evaluation showed no significant differences between the two groups in the NYHA class (p = 0.59), LVEF (p = 0.26), and echocardiographic findings. Similarly, BNP values as well as the distance covered in the setting of 6-MWT did not differ between groups.
Table 2 Baseline and 12-month values of the parameters assessed in PAP-treated and control patients -
2.
Twelve-month data
In contrast to the baseline data at the end of the follow-up period (i.e., at 12 months), a statistically significant difference in NYHA functional class was observed in PAP-treated vs. non-treated patients (p < 0.001, Table 2) along with a better performance in the 6-MWT (<0.001) in comparison to control subjects. In addition, the PAP-treated patients had a significant increase in LVEF when compared with untreated patients (p = 0.033). Interestingly, longitudinal RV contractile function, as detected with DTI and expressed by SmRV was significantly improved (p < 0.001). This is probably attributed to the significant reduction of the RV afterload (as reflected by PASP estimation). No significant differences regarding RV dimensions were observed between the two groups. Moreover, myocardial wall stress and LV filling pressures were both decreased, as assessed by BNP the former (p = 0 < 001) and E/E’ ratio the latter, which was decreased though marginally (p = 0.046).
-
3.
Impact of PAP therapy on cardiac clinical status
When data of PAP-treated patients were separately analysed significant improvements were detected in almost all parameters measured at the end of the study as compared with the baseline measurements. Left ventricular EF increased by approximately 16% (p < 0.001), the distance covered in 6-MWT increased by 10% (p < 0.001) and NYHA class was substantially improved (2.0 ± 0.1 post-PAP vs. 3.4 ± 0.5 pre-PAP, p < 0.001). Myocardial wall stress and LV filling pressures (LVFP) decreased both, as it was estimated by BNP values and E/E’ ratio reductions (p = 0.001 and 0.009, respectively). Regarding the right ventricle (RV), a significant improvement (p = 0.012) was noticed in the longitudinal contractile function as measured by SmRV (p = 0.012), along with a decrease (p = 0.004) in PASP. It is of note that a trend for both RV diameters reduction was seen (p = 0.063 for RVD1 and p = 0.056 for RVD2).
-
4.
Hospitalizations and mortality
Two patients (18.2%) in the PAP-treated group in comparison with four (57.1%) in the control group were hospitalized due to HF decompensation over the study period (p = 0.101, see Table 3). Regarding mortality, two cardiac deaths were recorded in the control group (~28%) and none in the PAP group (p = 0.137). Both deaths were in-hospital 4 and 8 months, respectively, after patients’ inclusion in the study, and were attributed to intractable pump failure. When hospitalizations and deaths were combined as a composite end-point, PAP-treated group showed a significantly lower incidence of unfavorable outcomes (18.2% vs. 85.7%, p = 0.013).
Table 3 Mortality and hospitalization rates in the groups studied
Discussion
In this investigation we showed that PAP therapy for SDB of any type (obstructive, central or both) in stable patients with advanced HF resulted in a significant and sustained improvement of cardiac and functional status, less neurohormonal activation and fewer hospital admissions and deaths over a 12-month period.
SDB in HF might be manifested as either OSA or CSA with or without CSR. The predominant type of SDB in each patient depends on the degree of obesity and the severity of HF. The prevalence of OSA may be higher in obese patients or in those with less severe HF, whereas CSA is more common in those with more severe HF and worse functional status [26, 27]. Our findings confirm the high prevalence of SDB in advanced HF as ~80% (i.e., 23 out of 29) of patients had SDB.
There is evidence supporting that SDB is associated with increased mortality and morbidity in HF patients although this finding has not been confirmed in all relevant studies. Untreated OSA (AHI > 15) in patients with HF has been associated with increased death rates independently of confounding factors and an approximately 2-fold higher risk for death and hospitalizations over 2 years [28, 29]. However, it seems that increased risk is confined in patients with ischemic and not in HF of other etiologies [30]. Regarding the prognostic role of CSA/CSR in HF there is also evidence that central apnea may increase mortality independently of other risk factors although, even in this case, the findings are disparate [31, 32]. CSA/CSR has been associated with increased morbidity, death, and rates of cardiac transplantation whereas CSR, when present, tends to imply a worse prognosis [33–36].
The relative lack of consistency in studies investigating the impact of SDB in clinical outcomes of HF might be due to differences in methodology and duration of follow-up, definitions and severity of SDB, and differences in the etiology, severity or medical treatment of HF. To our knowledge this is the first study to evaluate in patients with advanced HF and concomitant SBD of either type, the long-term impact of PAP therapy on cardiac status and clinical outcome. Despite the small number of participants (as this is a preliminary report) a significantly lower incidence of hospital admissions and mortality (p = 0.013) was detected at the end of the 12-month follow-up period in the group of PAP-treated patients.
In patients with HF and OSA, CPAP has been regarded as an effective therapy not only for OSA but also for the underlying HF in short-term investigations that showed improvement of LVEF, NYHA class, and quality of life [37–40]. APAP which is an alternative mode of PAP application in OSA patients, has been found to be equally effective to CPAP and has been linked with enhanced compliance to treatment [15]. However, the effects of APAP in HF patients have not been thoroughly investigated. A recent study, in patients with HF and OSA, found that APAP improved subjective sleepiness after 6 weeks but had no effect on cardiac functional status during this short-term period [16]. Thus, there is lack of studies evaluating the long-term effects of CPAP or APAP therapy on heart function. Concerning treatment of CSA (with or without CSR) in HF patients, several forms of PAP therapy including CPAP, bi-level pressure support and the novel ASV have been used [13, 41, 42]. In short-term randomized studies it has been shown that CPAP improves LVEF in patients with CSA especially in the presence of CSR but, according to other trials, this is true for only a minority of patients [35, 43–46]. Thus, the use of CPAP is not widely recommended since there is no evidence of improving long-term mortality and there are cautions for possible adverse effects in non-responders [41, 45, 47]. Concerning ASV, it has been found to be superior to CPAP in eliminating CSA/CSR in HF patients, improving LEVF, functional status, quality of life, exercise tolerance, and enhancing compliance [13, 44, 48–50]. ASV treatment had a favorable impact on cardiac function, functional status, exercise tolerance and quality of life after 6 months [49, 51]. However, long-term benefit on mortality has not yet been proven.
In the present study, the choice of the most appropriate mode of ventilation for each patient was based on the prominent type of SDB. Thus, we offered APAP for patients with OSA, and ASV for those with CSA/CSR. In this specific population of stable patients with advanced HF and SDB of any type, we found that PAP therapy improved cardiac and functional status. We wish to emphasize that improvement of heart function was sustained for 12 months. Good compliance to PAP therapy seems to be the most important key of effective therapy and sustained benefit from PAP in HF. We adopted a close follow-up schedule (bimonthly) with aim to evaluate and enhance compliance in all patients providing adequate education and support by authorized and trained personnel.
In this investigation, we also sought to assess the impact of PAP therapy in less investigated parameters, such as E/E’ ratio, a simple non invasive measurement that predicts LVFP [52, 53]. Previous studies have shown that E/E’ < 8 accurately predicts normal LVFP, whereas E/E’ > 15 identifies increased LVFP [53]. We found that E/E’ ratio was significantly decreased over 12 months (p = 0.009) to a value suggestive of low LVFP (7.0 ± 0.9), demonstrating an important mechanism of beneficial effect of PAP on LV function. In line with this finding and with previously published data, treatment with PAP was associated with significantly lower BNP values at the end of the study [54]. BNP reflects neurohormonal activation which constitutes an important pathophysiologic mechanism leading to HF syndrome and has been introduced as a tool for the diagnosis and management of HF, in terms of effectiveness of therapy [24]. The modification of neurochemical profile in HF patients by PAP may explain improvement of clinical outcomes. We wish to stress that neither E/E’ ratio nor BNP changed throughout the study in the control group. Another remarkable finding of this study is related to RV systolic function which has not been evaluated in detail in HF patients receiving PAP therapy. Although successful treatment of OSA has been shown in a study to improve RV function no data are available for HF patients with SDB [55]. Hence, our finding of longitudinal RV contractile function improvement (as detected with DTI and expressed by SmRV) earns particular importance. Furthermore, along with RV systolic function improvement a significant decrease of the PASP with PAP therapy was found. This may be due to a better LV performance as reflected by LVEF improvement, decreased LVFP and less neurhormonal activation. PAP application has been also shown to reduce pulmonary arterial systolic pressure levels by restoring the normal levels of vasoactive mediators, thus aborting vasoconstriction and endothelial cell proliferation [56]. Nevertheless, further investigations of RV function in patients with HF and SDB are certainly needed.
Finally, in our study population, a statistically significant improvement in the 6-MWT covered distance (by ~40 m) was noticed in the PAP-treated group. As it has been shown in previous studies, 6-MWT is an integral element of the functional capacity assessment and prognosis in patients with chronic cardiopulmonary disease [57].
The effect of PAP therapy on functional capacity along with its favorable effects on several other parameters above reported contributed in a dissociation of the subgroups assessed regarding clinical status, cardiac function and, most importantly, clinical outcomes. Indeed, no deaths and fewer hospital admissions were recorded in the PAP-treated patients as compared to the control group. The difference was significant (p = 0.013) when deaths and hospitalization rates were examined in combination.
Study limitations
Some study limitations should be considered in the interpretation of our results. The most important is related to the small number of participants. However, the limited sample size did not prevent us from reaching statistically significant results. Certainly, randomized multicenter studies are needed to confirm our findings.
Secondly, this is a non-randomized study with the control group including patients who refused PAP therapy. Although someone could consider that the latter patients were less compliant to medical advice, we made every possible effort to control their adherence to medical treatment through a close follow-up.
Conclusion
This prospective study demonstrated that treatment of SDB with PAP therapy in patients with advanced HF, irrespective of SDB type, leads to a sustained (12 months) improvement in cardiac function, physical performance, neurohormonal activation, and decreased morbidity and mortality. Physicians should closely evaluate patients’ compliance which might be a crucial factor for the accomplishment of the best possible results. Our preliminary data firmly support the routine investigation and treatment of SDB in patients with advanced HF.
References
Braunwald E, Bristow M (2000) Congestive heart failure: 50 years of progress. Circulation 102:(20 Suppl 4):IV14–23
Sans S, Kesteloot H, Kromhout D (1997) The burden of cardiovascular diseases mortality in Europe. Task force of the European society of cardiology on cardiovascular mortality and morbidity statistics in Europe. Eur Heart J 18:1231–1248
The SOLVD Investigators (1991) Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Eng J Med 325:293–302
Shahar E, Whitney CW, Redline S, Lee ET, Newman AB, Javier Nieto F, O’Connor GT, Boland LL, Schwartz JE, Samet JM (2001) Sleep disordered breathing and cardiovascular disease: cross-sectional results of the sleep heart health study. Am J Respir Crit Care Med 163:19–25
Sin D, Fitzgerald F, Parker JD, Newton G, Floras JS, Bradley TD (1999) Risk factors for central and obstructive apnoea in 450 men and women with congestive heart failure. Am J Respir Crit Care Med 160:1101–1106
Javaheri S, Parker TJ, Liming JD, Corbett WS, Nishiyama H, Wexler L, Roselle GA (1998) Sleep apnea in 81 ambulatory male patients with stable heart failure. Circulation 97:2154–2159
Javaheri S, Parker TJ, Wexler L, Michaels SE, Stanberry E, Nishyama H, Roselle GA (1995) Occult sleep disordered breathing in stable congestive heart failure. Ann Intern Med 122:487–492
Bradley TD, Floras JS (2003) Sleep apnea and heart failure: Part I: obstructive sleep apnea. Circulation 107:1671–1678
Bradley TD, Floras JS (2003) Sleep apnea and heart failure: Part II: central sleep apnea. Circulation 107:1822–1826
Butt M, Dwivedi G, Khair O, Lip GY (2010) Obstructive sleep apnea and cardiovascular disease. Int J Cardiol 139:7–16
Arzt M, Bradley TD (2006) Treatment of sleep apnea in heart failure. Am J Respir Crit Care Med 173:1300–1308
De Backer W, Javaheri S (2007) Treatment of sleep apnea in heart failure. Sleep Med Clin 2:631–638
Teschler H, Dohring J, Wang YM, Berthon-Jones M (2001) Adaptive pressure support servo-ventilation. A novel treatment for Cheyne–Stokes respiration in heart failure. Am J Respir Crit Care Med 164:614–619
Masa JF, Jimenez A, Duran J, Capote F, Monasterio C, Mayos M, Teran J, Hermandez L, Barbe F, Maimo A, Rubio M, Montserrat JM (2004) Alternative methods of titrtating continous positive airway pressure: a large multicenter study. Am J Respir Crit Care Med 170:1218–1224
Massie CA, McArdle N, Hart RW, Schmidt-Nowara WW, Lankford A, Hudgel DW, Gordon N, Douglas NJ (2003) Comparison between automatic and fixed positive airway pressure therapy at home. Am J Respir Crit Care Med 167:20–23
Smith LA, Vennelle M, Gardner RS, McDonagh TA, Denvir MA, Douglas NJ, Newby DE (2007) Auto-titrating continuous positive pressure therapy in continuous positive airway pressure in patients with chronic heart failure and obstructive sleep apnea: a randomized placebo-controlled trial. Eur Heart J 28:1221–1227
Caples SM, Somers V (2007) CPAP treatment for obstructive sleep apnea in heart failure: expectations unmet. Eur Heart J 28:1184–1186
Heart Failure Society of America (2006) Executive summary: HFSA 2006 comprehensive heart failure practice guideline. J Card Fail 12:10–38
Iber C, Ancoli-Israel S, Chesson A, Quan SF, editors. 1st ed. Westchester, IL: American Academy of Sleep Medicine; 2007. The AASM manual for the scoring of sleep and associated events: rules, terminology, and technical specification
Kushida CA, Littner MR, Morgenthaler T, Alessi CA, Bailey D, Coleman J Jr, Friedman L, Hirshkowitz M, Kapen S, Kramer M, Lee-Chiong T, Loube DL, Owens J, Pancer JP, Wise M (2005) Practice parameters for the indications for polysomnography and related procedures: an update for 2005. Sleep 28:499–521
Quiñones MA, Douglas PS, Foster E, Gorcsan J 3rd, Lewis JF, Pearlman AS, Rychik J, Salcedo EE, Seward JB, Stevenson JG, Thys DM, Weitz HH, Zoghbi WA (2003) ACC/AHA clinical competence statement on echocardiography: a report of the American College of Cardiology/American Heart Association/American College of Physicians-American Society of Internal Medicine Task Force on Clinical Competence. J Am Coll Cardiol 41:687–708
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise J, Solomon S, Spencer KT, St John Sutton M, Stewart W (2006) American Society of Echocardiography’s Nomenclature and Standards Committee; Task force on chamber quantification; American College of Cardiology Echocardiography Committee; American Heart Association; European Association of Echocardiography, European Society of Cardiology. Recommendations for chamber quantification. Eur J Echocardiogr 7:79–108
Donovan CL, Armstrong WF, Bach DS (1995) Quantitative Doppler tissue imaging of the left ventricular myocardium: validation in normal subjects. Am Heart J 130:100–104
Karavidas A, Lazaros G, Matsakas E, Farmakis D, Parissis J, Paraskevaidis IA, Michailidis C, Avramidis D, Zacharoulis A, Arapi S, Kaoukis A, Zacharoulis A (2008) Clinical value of B-type natriuretic peptide for the assessment of left ventricular filling pressures in patients with systolic heart failure and inconclusive tissue Doppler indexes. Heart Vessels 23:181–186
Opasich C, Pinna GD, Mazza A, Febo O, Riccardi R, Riccardi PG, Capomolla S, Forni G, Cobelli F, Tavazzi L (2001) Six-minute walking performance in patients with moderate to severe heart failure; is it a useful indicator in clinical practice? Eur Heart J 22:488–496
Javaheri S (2006) Sleep disorders in systolic heart function: a prospective study in 100 male patients. The final report. Int J Cardiol 106:21–28
Ferrier K, Campell A, Yee B, Richards M, O’Meeghan T, Weatherall M, Neill A (2005) Sleep-disordered breathing occurs frequently in stable outpatients with congestive heart failure. Chest 128:2116–2122
Wang H, Parker JD, Newton GE, Floras JS, Mak S, Chiu KL, Ruttanaumpawan P, Tomlinson G, Bradley TD (2007) Influence of obstructive sleep apnea on mortality in patients with heart failure. J Am Coll Cardiol 49:1625–1631
Kasai T, Narui K, Dohi T, Yanagisawa N, Ishiwata S, Ohno M, Yamaguchi T, Momomura S (2008) Prognosis of patients with heart failure and obstructive sleep apnea treated with continuous positive airway pressure. Chest 133:690–696
Yumino D, Wang H, Floras JS, Newton GE, Mak S, Ruttanaumpawan P, Parker JD, Bradley TD (2009) Relationship between sleep apnoea and mortality in patients with ischemic heart failure. Heart 95:819–824
Roebuck T, Solin P, Kaye DM, Bergin P, Bailey M, Naughton MT (2004) Increased long-term mortality in heart failure due to sleep apnea is not yet proven. Eur Respir J 23:735–740
Andreas S, Hagenah G, Moller C, Werner GS, Kreuzer H (1996) Cheyne-Stokes respiration and prognosis in congestive heart failure. Am J Cardiol 78:1260–1264
Finley LJ, Zwillich CW, Ancoli-Israel S, Kripke D, Tisi G, Moser KM (1985) Cheyne-Stokes breathing during sleep in patients with left ventricular heart failure. S Med J 78:11–15
Lanfranchi PA, Braghiroli A, Bosimini E, Mazzuero G, Colombo R, Donner CF, Giannuzzi P (1999) Prognostic value of nocturnal Cheyne stokes respiration in chronic heart failure. Circulation 99:1435–1440
Sin DD, Logan AG, Fitzerald FS, Liu PP, Bradley TD (2000) Effects of continuous positive airway pressure on cardiovascular outcomes in heart failure in patients with and without Cheyne-Stokes respiration. Circulation 102:61–66
Hanly PJ, Zuberi-Khokhar NS (1996) Increased mortality associated with Cheyne-Stokes respiration in patients with congestive heart failure. Am J Respir Crit Care Med 153:272–276
Johnson CB, Beanlands RS, Yoshinaga K, Haddad H, Leech J, de Kemp R, Burwash IG (2008) Acute and chronic effects of continuous positive airway pressure therapy on left ventricular systolic and diastolic function in patients with obstructive sleep apnea and congestive heart failure. Can J Cardiol 24:697–704
Malone S, Liu PP, Holloway R, Rutherford R, Xie A, Bradley TD (1991) Obstructive sleep apnea in patient with dilated cardiomyopathy; effects of continuous positive airway pressure. Lancet 338:1480–1484
Kaneko Y, Floras JS, Usui K, Plante J, Tkacova R, Kubo T, Ando S, Bradley TD (2003) Cardiovascular effects of continuous positive airway pressure in patients with heart failure and obstructive sleep apnea. N Eng J Med 348:1233–1241
Mansfield DR, Gollogly NC, Kaye DM, Richardson M, Bergin P, Naughton MT (2004) Controlled trial of continuous positive airway pressure therapy in obstructive sleep apnea and heart failure. Am J Respir Crit Care Med 169:361–366
Bradley TD, Logan AG, Kimoff RJ, Sériès F, Morrison D, Ferguson K, Belenkie I, Pfeifer M, Fleetham J, Hanly P, Smilovitch M, Tomlinson G, Floras JS (2005) CANPAP Investigators. Continuous positive airway pressure for central sleep apnea and heart failure. N Eng J Med 353:2025–2033
Arzt M, Wensel R, Montalvan S, Schichtl T, Schroll S, Budweiser S, Blumberg FC, Riegger GA, Pfeifer M (2008) Effects of dynamic bi-level airway pressure support on central sleep apnea in men with heart failure. Chest 134:61–66
Naughton MT, Liu PP, Bernard DC, Goldstein RS, Bradley TD (1995) Treatment of congestive heart failure and Cheyne stokes during sleep by continuous positive airway pressure. Am J Respir Crit Care Med 151:92–97
Naughton MT, Benard DC, Liu PP, Rutherford R, Rankin F, Bradley TD (1995) Effects of nasal CPAP on sympathetic activity in patients with heart failure and central sleep apnea. Am J Respir Crit Care Med 152:473–479
Javaheri S (2000) Effects of continuous positive airway pressure on sleep apnea and ventricular irritability in patients with HF. Circulation 101:392–397
Buckle P, Millar T, Kryger M (1992) The effects of short term nasal CPAP on Cheyne-Stokes respiration in congestive heart failure. Chest 102:31–35
Javaheri S (2006) CPAP should not be used for central sleep apnea in congestive sleep apnea. J Clin Sleep Med 2:399–402
Philippe C, Stoïca-Herman M, Drouot X, Raffestin B, Escourrou P, Hittinger L, Michel PL, Rouault S, d’Ortho MP (2005) Compliance with and efficacy of adaptive servo-ventilation (ASV) versus continuous positive airway pressure (CPAP) in the treatment of Cheyne-Stokes respiration in heart failure over a 6 month period. Heart 92:337–342
Oldenburg O, Schmidt A, Lamp B, Bitter T, Muntean BG, Langer C (2008) Adaptive servo ventilation improves cardiac function in patients with chronic heart failure and Cheyne-Stokes respiration. Eur J Heart Fail 10:581–586
Kasai T, Usui Y, Yoshioka T, Yanagisawa N, Takata Y, Narui K, Yamaguchi T, Yamashina A, Momomura SI (2010) JASV Investigators. Effect of flow-triggered adaptive servo-ventilation compared with continuous positive airway pressure in patients with chronic heart failure with coexisting obstructive sleep apnea and Cheyne-Stokes respiration. Circ Heart Fail 3:140–148
Hastings PC, Vazir A, Meadows GE, Dayer M, Poole-Wilson PA, McIntyre HF, Morrell MJ, Cowie MR, Simonds AK (2010) Adaptive servo-ventilation in heart failure patients with sleep apnea: a real world study. Int J Cardiol 139:17–24
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA (1997) Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527–1533
Ommen SR, Nishimura RA, Appleton CP, Miller FA, Oh JK, Redfield MM, Tajik AJ (2000) Clinical utility of Doppler echocardiography and tissue Doppler imaging in the estimation of left ventricular filling pressures: a comparative simultaneous Doppler-catheterization study. Circulation 102:1788–1794
Eskafi M, Cline C, Nilner M, Israelsson B (2006) Treatment of sleep apnea in congestive heart failure with a dental device: the effect on brain natriuretic peptide and quality of life. Sleep Breath 10:90–97
Nahmias J, Lao R, Karetzky M (1996) Right ventricular dysfunction in obstructive sleep apnoea: reversal with nasal continuous positive airway pressure. Eur Respir J 9:945–951
Arias MA, García-Río F, Alonso-Fernández A, Martínez I, Villamor J (2006) Pulmonary hypertension in obstructive sleep apnoea: effects of continuous positive airway pressure: a randomized, controlled cross-over study. Eur Heart J 27:1106–1113
Olsson LG, Swedberg K, Clark AL, Witte KK, Cleland JG (2005) Six minute corridor test as an outcome measure for the assessment of treatment in randomized, blinded, intervention trials of chronic heart failure: a systematic review. Eur Heart J 26:778–793
Conflicts of interest
The authors declare they have no conflicts of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karavidas, A., Kapsimalis, F., Lazaros, G. et al. The impact of positive airway pressure on cardiac status and clinical outcomes in patients with advanced heart failure and sleep-disordered breathing: a preliminary report. Sleep Breath 15, 701–709 (2011). https://doi.org/10.1007/s11325-010-0425-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-010-0425-5