Abstract
The aim of the present study was to investigate the effect of a mandibular advancement device (MAD) for the treatment of sleep apnea (SA) on plasma brain natriuretic peptide (BNP), left ventricular ejection fraction (LVEF), and health-related qualify of life (HRQL) in patients with mild to moderate stable congestive heart failure (CHF). Seventeen male patients aged 68.4±5.5 with an apnea–hypopnea index (AHI) ≥10 were equipped with an individually fitted MAD. SA was evaluated using a portable respiratory multirecording system before and after the initiation of treatment. Eleven patients completed follow-up and were evaluated after 6 months of treatment. The AHI reduced from 25.4±10.3 to 16.5±10.0 (p=0.033) compared to baseline and mean plasma BNP levels decreased from 195.8±180.5 pg/ml to 148.1±139.9pg/ml (p=0.035). SA-related symptoms, e.g., excessive daytime sleepiness, were also reduced (p=0.003). LVEF and HRQL were unchanged. We conclude that SA treatment with a MAD on patients with mild to moderate stable CHF appears to result in the reduction of plasma BNP levels. Further studies to investigate if the observed reduction in BNP concentrations also result in improved prognosis are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congestive heart failure (CHF), especially when due to left ventricular systolic dysfunction, is associated with elevated levels of circulating plasma brain natriuretic peptide (BNP) [1]. The stimulus for BNP secretion is cardiac myocyte stretch and regulation takes place through gene expression [2]. BNP concentrations are closely related to left ventricular pressure and volume indices [3, 4]. In patients with CHF, elevated levels of plasma BNP are associated with an increased risk for sudden death [5] and are also a strong predictor of morbidity and mortality [6]. Sleep apnea (SA) is a common comorbid condition in patients with CHF [7, 8]. Untreated SA is believed to be associated with an increased risk of death in patients with coronary artery disease [9]. Treatment of SA using continues positive airway pressure (CPAP) or upper airway surgery in this group of patients was shown to reduce cardiovascular death, acute coronary syndromes, and hospitalization for cardiac causes [10]. SA has also shown to stimulate secretion of BNP. Nocturnal secretion of BNP increases in association with the elevation of blood pressure during episodes of apnea and fall when SA is treated using CPAP [11]. Decrease in cardiac strain due to reduction of SA-induced hypoxemia, microarousals, and negative intrathoracic pressure were discussed as possible mechanisms explaining the effect of CPAP on plasma BNP levels [11]. Treatment of SA may therefore have a positive impact on cardiac function and reduce symptoms of heart failure [12, 13]. Furthermore, treatment may also improve quality of life [14], that is, of severely impaired patients with CHF irrespective of the degree of left ventricular ejection fraction (LVEF) [15].
A mandibular advancement device (MAD) is a dental appliance designed to eliminate pharyngeal airway obstruction (Fig. 1). MAD was widely recommended for treatment of obstructive sleep apnea (OSA) over the past two decades [16–22]. MAD was shown to reduce SA-induced hypoxemia [16, 18] and arousals [18]. There is also evidence to suggest that it may be useful for the treatment of central sleep apnea (CSA) [22]. We have previously reported that treatment of SA with a MAD reduces the severity of SA and increases oxygen saturation in patients with CHF [23]. By preserving free upper airways, the device is able to reduce repetitive, excessive, and negative intrathoracic pressure. Therefore, treatment of SA with a MAD in patients with CHF may be beneficial and, similar to CPAP, reduces cardiac strain and thereby levels of circulating BNP.
The aim of the present study was to investigate if the treatment of SA with a MAD had an effect on plasma BNP concentrations, left ventricular systolic function, and health-related qualify of life (HRQL) in patients with mild to moderate, stable CHF. The hypothesis was that treatment of SA with a MAD would decrease plasma BNP concentrations, increase LVEF, and improve HRQL.
Materials and methods
Patients
Eligible patients for inclusion in the study were 623 men and women who were previously hospitalized at the department of Cardiology, Malmö University Hospital, Sweden, with diagnosis of stable, mild to moderate CHF, New York Heart Association (NYHA) functional classes II–III, and left ventricular systolic dysfunction.
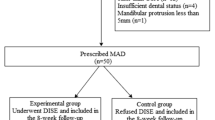
Figure 2 shows the selection of patients is in the study. Patients were excluded if they were previously treated for SA, had dental problems preventing the use of a MAD, or had temporomandibular joint problems. They were also excluded if they were likely to undergo cardiac surgery within 1 year, suffered from any other severe disease likely to interfere with quality of life within the following year or were diagnosed as having any serious mental condition. Alcohol or drug abuse or other conditions making it likely not to comply with the study protocol excluded patients. Also patients were excluded if they were unable to answer the study questionnaire for any reason, participated in any other clinical trial, or if their treating physician deemed participation inappropriate.
Out of 623 patients, 195 patients fulfilled the inclusion criteria. These patients were invited to participate in the study. Sixty-one patients volunteered who underwent new cardiac examinations and polysomnographic registration.
The study included 17 patients with CHF, NYHA functional classes II–III, and LVEF ≤40%, who also had significant SA defined as a nocturnal apnea–hypopnea index (AHI) ≥10. CHF was considered stable if their heart failure medication did not change 4 weeks prior to inclusion or during the study period.
Demographic profile of the study population is shown in Table 1. The study design is illustrated in Fig. 3. All patients gave informed consent to participate in the study, which was approved by the Research Ethics Committee, Lund University, Sweden.
Echocardiography
Echocardiographic examinations were performed using a Hewlett-Packard Sonos 2000 (Andover, MA, USA). Parasternal and apical views were obtained with the patient in a left lateral recumbent position. Measurements were acquired during silent respiration or end-expiratory apnea. Left ventricular systolic function was assessed by determination of the mean left atrioventricular plane displacement, global qualitative assessment, and/or single plane ellipse (modified Simpson’s rule) [24–26].
Polysomnography
An unattended, portable monitor (EdenTrace II Plus Multirecording System, EdenTech Corp, Eden Prairie, MN, USA) was used for nocturnal polysomnography at baseline before and after treatment with the MAD. The second registration was performed when the patients became accustomed to the device. Recordings were made of oronasal airflow, chest effort, oxyhemoglobin saturation (SaO2), body position, and snoring (levels ≥90 dB). A respiratory disturbance (an apnea or hypopnea) was defined as a decrease in airflow that lasted at least 10 s with at least a 50% reduction of airflow compared with baseline amplitude. A respiratory disturbance had to be associated with oxyhemoglobin desaturation defined as a reduction of at least 4% compared with the baseline. The respiratory disturbances are presented as AHI defined as the mean number of respiratory disturbances per hour.
The study population, echocardiographic and polysomnographic procedures were previously described in detail elsewhere [23].
Plasma brain natriuretic peptide assay
Venous blood samples were drawn from a cubital vein with the patient resting in recumbent position for at least 20 min. The time of blood sampling for all patients was around ten o’clock in the morning. The blood samples were collected into 5 ml plastic tubes containing 9 mg of edetic acid as an anticoagulant. The samples were centrifuged at 3,000 rpm for 10 min at 4°C and the plasma was immediately frozen to −70°C until it was assayed. Plasma BNP was measured using a Shionoria BNP immunoassay kit from CIS Bio International (Gif-sur-Yvette Cedex, France) following the instructions of the manufacturer. The detection limit of the assay was 2 pg/ml. The coefficients of variation at the levels 15 and 290 pg/ml were 20 and 10%, respectively. The reference range for adults given by the manufacturer was 0–18 pg/ml.
Health-related quality of life
HRQL was evaluated by using two self-administered questionnaires: Nottingham Health Profile (NHP) and Minnesota Living with Heart Failure Questionnaire (MLHFQ). NHP is a generic instrument divided in two parts containing questions for yes or no answers. NHP was designed to measure the effect of ill health on different dimensions of the quality of life, regardless of the causal disease. The Swedish version of NHP was validated and previously used to assess HRQL in patients with CHF [15]. NHP part one consists of 38 questions reflecting quality of life in the dimensions emotion, sleep, energy, pain, mobility, and social isolation. The score in each dimension could vary from 0 to 100. The higher the NHP score, the poorer the HRQL.
MLHFQ is a disease-specific questionnaire consisting of 21 questions focusing on signs and symptoms of heart failure; physical and emotional impairment; and work, social, and sexual activities. Each question in the MLHFQ can be answered according to a 6-point scale from 0 (not a problem at all) to 5 (a very severe problem). The total score could range from 0 (no disability) to 105 (severe disability) [27].
Sleep apnea questionnaire
The purpose of the questionnaire was to study the effect of the MAD intervention on the symptoms associated to nocturnal respiratory disorders and SA syndrome such as snoring, SA, and excessive daytime sleepiness. The questionnaire was composed of 15 questions each with a 5-point scale from 0 (never) to 4 (always) (Appendix). The higher the score, the greater the symptoms of the nocturnal sleep disorder.
Mandibular advancement device
The MAD was made of transparent acrylic (Ortocryl, Dentaurum, Germany) covering the occlusal surfaces of the teeth with the exception of the incisors. The splints were connected by two stainless steel wires, 3.0 mm in diameter, and were retained on the jaws by using active clasps. The degree of the mandibular advancement was individually selected at a level of 50–75% of maximal protrusive movement of the mandible. The exact degree depended on the magnitude of maximal protrusive movement, state of dentition, and degree of comfort for the individual patient (Fig. 1). The patients were instructed to use the device every night. A checkup was performed after 7–10 days at which time, necessary adjustments to the device were made. When the patients were customized with the MAD at earliest 4–6 weeks, a second nocturnal respiratory recording with the device was performed to evaluate the effect of the intervention on the SA.
Statistics
Plasma BNP, LVEF, HRQL, and sleep apnea questionnaire (SAQ) were measured at baseline before treatment and 6 months after the initiation of treatment. Wilcoxon signed rank test was used to determine the statistical significance of changes in continuous variables. P values <0.05 were considered to indicate statistical significance. Values are presented as mean±SD.
Results
Six patients were excluded from the final analysis due to failure to use the MAD regularly, withdrawn consent, or death. Eleven patients completed the 6-month follow-up and were evaluated (Fig. 4). The patients’ clinical characteristics and medication at baseline are shown in Table 1. They remained stable throughout the study. The mean AHI at baseline was 25.4±10.3 and it decreased to 16.5±10.0 after treatment with MAD (p=0.04). The mean plasma BNP levels fell from 195.8±180.5 pg/ml at baseline to 148.1±139.9 pg/ml (p=0.02) (Table 2). The severity of the SA-related symptoms as measured by SAQ decreased (Table 3). There was no change in mean LVEF at 6 months compared to baseline, 31.3±8.0 and 31.1±8.6%, respectively. HRQL, as evaluated using the total mean NHP part one score and the MLHFQ, were unchanged at 6 months compared to baseline (Table 3).
Discussion
In the present study we found that in patients with stable, mild to moderate CHF and SA, the MAD intervention reduced the severity of the SA as expressed by AHI after 6 months of treatment. Furthermore, we observed a reduction in circulating plasma BNP concentration and SA-related symptoms. However, we found no change in LVEF or HRQL.
Williams et al. [28] investigated the correlation between aerobic exercise capacity and plasma N-brain natriuretic peptide (N-BNP), a peptide which is cosecreted with BNP, compared with LVEF, in patients with CHF. The plasma N-BNP was found to significantly correlate with aerobic exercise capacity and duration, whereas LVEF showed very poor correlations. These results may indicate that BNP reflects functional cardiac impairment better than LVEF. It is therefore reasonable to expect that intervention with a MAD may affect functional impairment and not necessarily the left ventricular systolic function. This may explain why reduction in BNP was not accompanied with an improvement in LVEF in the present study. Furthermore, LVEF is an expression of systolic function whereas BNP not only reflects the degree of systolic dysfunction but all also the degree of diastolic dysfunction, which was not evaluated in the study patients [29].
An improvement in functional capacity should ideally result in an improvement in HRQL. The patients in our study, however, appeared to have near normal HRQL, i.e., not very different from what would be expected in an age- and gender-matched normal population [15]. Thus, in this situation it would be unrealistic to expect an improvement of HRQL.
Two previous studies assessed BNP in patients hospitalized for CHF and showed an association with prognosis including the risk for readmission [30, 31]. The patients in our study were not hospitalized during follow-up suggesting that heart failure were less severe as illustrated by NYHA-class and plasma BNP concentrations. Because CHF is a progressive chronic disease, one would expect a deterioration in parameters and cardiac function. The cohort in the present study tended to improve as shown by BNP analysis, suggesting that the intervention provided may be effective.
In patients with CHF suffering from CSA associated with Cheyne–Stocks respiration (CSR-CSA), treatment with CPAP resulted to reduction of atrium natriuretic peptide (ANP) [32]. ANP is released from the atria of the heart as a result of similar stimuli that promote the secretion of BNP [33]. The BNP is derived from the ventricles and is thought to be more sensitive and specific than ANP as an indicator for ventricular disorders. At inspiration when the thoracic cavity expands, patients with OSA express an exaggerated negative pressure because the airways are still closed. The negative intrathoracic pressure contributes to an increased venous filling, increased preload on the heart, and subsequently increased wall tension. This may be the trigger for increased secretion of natriuretic peptides, both ANP and BNP [11]. A previous study demonstrated strong a correlation between BNP secretion, elevation in systolic blood pressure, and with duration of OSA. It was also shown that treatment of OSA by CPAP was associated with reduction in plasma BNP. The results suggest that both the elimination of SA and direct effects of positive airway pressure are the mechanism behind the effect of CPAP on the BNP [11].
Because a MAD increases and stabilizes the pharyngeal airway dimension [34], there is excellent possibility to prevent OSA, which also means prevention of repetitive, exaggerated, negative intrathoracic pressure and thereby less cardiac wall tension. This means that the MAD-like CPAP may also have a direct beneficial effect on the cardiac load besides its effect to also reduce OSA, SA-induced hypoxemia, and arousals. However, in CHF, CSR-CSA and not OSA were shown to be the most common cause of SA [7]. Previous studies by Nakazawa et al. [22] indicated a positive effect of MAD on CSA and Farrow [35] reported two cases of CSA treated with a tongue-retaining device. The mechanism by which a MAD may decrease CSR-CSA is unclear; however, other treatments primarily introduced for the treatment of OSA have proven effective in CSA. For example CPAP, originally designed for treatment of OSA [36], also reduces CSA. This may not be a direct effect but may be due to a potential interaction between OSA and CSA. It was demonstrated that collapse of the upper airway space may occur during periods of CSA leading to OSA [37] and it was also speculated that OSA may aggravate the instability of the respiratory control system, increase the intensity of periodic breathing, and induce CSA [38].
The present study, which to our knowledge is the first to examine the effect of MAD intervention in patients with CHF and SA, has some limitations. SA was reduced by MAD but the methodology used for polysomnographic registrations could not accurately differentiate between OSA and CSA. However, the distinction between various types of SA may be questionable even with more advanced techniques. Further studies are needed to examine the effect of MAD on CSA. Also, although MAD is a practical and less cumbersome device than CPAP, its usage is limited in elderly patients who have problems with dentition, which may inhibit the use of the treatment [39]. The small sample size and absence of control group does not allow definitive interpretations of the results. The relatively mild degrees of both SA and CHF also reduced the potential to show any changes. However, elaborate protocols and advanced examinations have limited the size of numerous populations in similar studies.
In conclusion, in patients with mild to moderate, stable CHF and SA, Treatment of SA with MAD appeared to reduce plasma BNP and severity of the excessive daytime sleepiness. The results may indicate a beneficial effect of MAD treatment for SA in patients with CHF. Further investigations on the use of a MAD are warranted.
References
Maisel AS, Krishnaswamy P, Nowak RM et al (2002) For the breathing not properly multinational study investigators. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 347:161–167
Onuoha GN, Nicholls DP, Patterson A, Beringer T (1998) Neuropeptide secretion in exercise. Neuropeptides 32:319–325
Shapiro BP, Chen HH, Burnett JC, Redfield MM (2003) Use of plasma brain natriuretic peptide concentration to aid in the diagnosis of heart failure. Mayo Clin Proc 78:481–486
Doggrell SA (2001) Brain natriuretic peptide: disease marker or more in cardiovascular medicine? Drugs Today (Barc) 37:463–476
Berger R, Huelsman M, Strecker K et al (2002) B-type natriuretic peptide predicts sudden death in patients with chronic heart failure. Circulation 105:2392–2397
Latini R, Masson S, Anand I et al (2004) For the Val-HeFT investigators. The comparative prognostic value of plasma neurohormones at baseline in patients with heart failure enrolled in Val-HeFT. Eur Heart J 25:292–299
Javaheri S, Parker TJ, Liming JD et al (1998) Sleep apnea in 81 ambulatory male patients with stable heart failure. Types and their prevalences, consequences and presentations. Circulation 97:2154–2159
Naughton MT, Bradley TD (1998) Sleep apnea in congestive heart failure. Clin Chest Med 19:99–113
Peker Y, Hedner J, Kraiczi H, Loth S (2000) Respiratory disturbance index: an independent predictor of mortality in coronary artery disease. Am J Respir Crit Care Med 162:81–86
Milleron O, Pilliere R, Foucher A et al (2004) Benefits of obstructive sleep apnoea treatment in coronary artery disease: a long-term follow-up study. Eur Heart J 25:728–734
Kita H, Ohi M, Chin K et al (1998) The nocturnal secretion of cardiac natriuretic peptides during obstructive sleep apnoea and its response to therapy with nasal continuous positive airway pressure. J Sleep Res 7:199–207
Yan AT, Bradley TD, Liu PP (2001) The role of continuous positive airway pressure in the treatment of congestive heart failure. Chest 120:1675–1685
Bradley TD, Floras JS (1996) Pathophysiologic and therapeutic implications of sleep apnea in congestive heart failure. J Card Fail 2:223–240
Silverberg DS, Iaina A, Oksenberg A (2002) Treating obstructive sleep apnea improves essential hypertension and quality of life. Am Fam Physician 65:229–236
Cline CM, Willenheimer RB, Erhardt LR, Wiklund I, Israelsson BY (1999) Health-related quality of life in elderly patients with heart failure. Scand Cardiovasc J 33:278–285
Fransson AM, Isacsson G, Leissner LC, Nasman AB, Alton MK (2001) Treatment of snoring and obstructive sleep apnea with a mandibular protruding device: an open-label study. Sleep Breath 5:23–33
Marklund M, Sahlin C, Stenlund H, Persson M, Franklin KA (2001) Mandibular advancement device in patients with obstructive sleep apnea: long-term effects on apnea and sleep. Chest 120:162–169
Yoshida K (2000) Effects of a mandibular advancement device for the treatment of sleep apnea syndrome and snoring on respiratory function and sleep quality. Cranio 18:98–105
Wilhelmsson B, Tegelberg A, Walker-Engstrom ML et al (1999) A prospective randomized study of a dental appliance compared with uvulopalatopharyngoplasty in treatment of obstructive sleep apnea. Acta Otolaryngol 119:503–509
O’Sullivan RA, Hillman DR, Mateljan R, Pantin C, Finucane KE (1995) Mandibular advancement splint: an appliance to treat snoring and obstructive sleep apnea. Am J Respir Crit Care Med 151:194–198
Eveloff SE, Rosenberg CL, Carlisle CC, Millman RP (1994) Efficacy of a Herbst mandibular advancement device in obstructive sleep apnea. Am J Respir Crit Care Med 149:905–909
Nakazawa Y, Sakamoto T, Yasutake R et al (1992) Treatment of sleep apnea with prosthetic mandibular advancement (PMA). Sleep 15:499–504
Eskafi M, Cline C, Israelsson B, Nilner M (2004) A mandibular advancement device reduces sleep disordered breathing in patients with congestive heart failure. Swed Dent J 28:155–163
Willenheimer R, Cline C, Erhardt L, Israelsson B (1997) Left ventricular atrioventricular plane displacement: an echocardiographic technique for rapid assessment of prognosis in heart failure. Heart 78:230–236
Remme WJ, Swedberg K (2001) Task force for the diagnosis and treatment of chronic heart failure, European Society of Cardiology. Guidelines for the diagnosis and treatment of chronic heart failure. Eur Heart J 22:1527–1560
Folland ED, Parisi AF, Moynihan PF, Jones DR, Feldman C, Tow DE (1979) Assessment of left ventricular ejection fraction and volumes by real-time, two-dimensional echocardiography. A comparison of cineangiographic and radionuclide techniques. Circulation 60:760–766
Rector TS, Kubo SH, Cohn JN (1987) Patients’ self-assessment of their congestive heart failure. Part 2: content, reliability and validity of a new measure, the Minnesota Living with Heart Failure Questionnaire. Heart Fail 1:198–209
Williams SG, Ng LL, O’Brien RJ, Taylor S, Li YF, Tan LB (2004) Comparison of plasma N-brain natriuretic peptide, peak oxygen consumption, and left ventricular ejection fraction for severity of chronic heart failure. Am J Cardiol 93:1560–1561
Troughton RW, Prior DL, Pereira JJ et al (2004) Plasma B-type natriuretic peptide levels in systolic heart failure: importance of left ventricular diastolic function and right ventricular systolic function. J Am Coll Cardiol 43:416–422
Cheng V, Kazanagra R, Garcia A et al (2001) A rapid bedside test for B-type peptide predicts treatment outcomes in patients admitted for decompensated heart failure: a pilot study. J Am Coll Cardiol 37:386–391
Bettencourt P, Ferreira S, Azevedo A, Ferreira A (2002) Preliminary data on the usefulness of B-type natriuretic peptide levels in predicting outcomes after hospital discharge in patients with heart failure. Am J Med 113:215–219
Tkacova R, Liu PP, Naughton MT, Bradley TD (1997) Effect of continuous positive airway pressure on mitral regurgitant fraction and atrial natriuretic peptide in patients with heart failure. J Am Coll Cardiol 30:739–745
Chen HH, Burnett JC (1999) The natriuretic peptides in heart failure: diagnostic and therapeutic potentials. Proc Assoc Am Physicians 111:406–416
Eskafi M, Cline C, Petersson A, Israelsson B, Nilner M (2004) The effect of mandibular advancement device on pharyngeal airway dimension in patients with congestive heart failure treated for sleep apnoea. Swed Dent J 28:1–9
Farrow SJ (1991) Successful treatment of central sleep apnea with an oral prosthesis. Chest 100:1461–1462
Issa F, Sullivan C (1986) Reversals of central sleep apnea using nasal CPAP. Chest 90:165–171
Hillarp B, Nylander G, Rosén I, Wickström O (1996) Videoradiography of patients with habitual snoring and/or sleep apnea. Acta Radiol 37:307–314
De Backer WA (1995) Central sleep apnoea, pathogenesis and treatment: an overview and perspective. Eur Respir J 8:1372–1383
Eskafi M, Ekberg E, Cline C, Israelsson B, Nilner M (2004) Use of a mandibular advancement device in patients with congestive heart failure and sleep apnoea. Gerodontology 21:100–107
Acknowledgements
Financial support of this project was given by the Faculty of Odontology, Malmö University; the Research Unit, Department of Cardiology, Malmö University Hospital; and the Swedish Heart and Lung Foundation.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
The self-administered Sleep Apnea Questionnaire (SAQ) used in the study
-
1.
Is your snoring loud and disturbing?
-
2.
Do you sometimes stop breathing when you sleep?
-
3.
Does your snoring disturb other persons?
-
4.
Do you have difficulties falling asleep?
-
5.
Are you sleepy during the day?
-
6.
Do you fall asleep during meetings, when you read, or when you are doing needlework?
-
7.
Do you fall asleep in front of the TV?
-
8.
Do you fall asleep when you are driving?
-
9.
Do you have difficulties concentrating during the day?
-
10.
Do you wake up at night and have difficulties breathing?
-
11.
Do you wake up with a dry mouth?
-
12.
Do you need to get up and go to the bathroom at night?
-
13.
Do you wake up rested?
-
14.
Do you wake up with a headache?
-
15.
Do you have irresistible attacks of sleep in the daytime?
Rights and permissions
About this article
Cite this article
Eskafi, M., Cline, C., Nilner, M. et al. Treatment of sleep apnea in congestive heart failure with a dental device. Sleep Breath 10, 90–97 (2006). https://doi.org/10.1007/s11325-006-0053-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-006-0053-2