Abstract
Unlike traditional, tracer-based methods of molecular imaging, magnetic resonance spectroscopy (MRS) is based on the behavior of specific nuclei within a magnetic field and the general principle that the resonant frequency depends on the nucleus’ immediate chemical environment. Most clinical MRS research has concentrated on the metabolites visible with proton spectroscopy and measured in specified tissue volumes in the brain. This methodology has been applied in various neurodegenerative disorders, most frequently utilizing measures of N-acetylaspartate as a neuronal marker. At short echo times, additional compounds can be quantified, including myo-inositol, a putative marker for neuroglia, the excitatory neurotransmitter glutamate and its metabolic counterpart glutamine, and the inhibitory neurotransmitter gamma-aminobutyric acid. 31P-MRS can be used to study high-energy phosphate metabolites, providing an in vivo assessment of tissue bioenergetic status. This review discusses the application of these techniques to patients with neurodegenerative disorders, including Parkinson’s disease, Alzheimer’s disease, and amyotrophic lateral sclerosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The continuing evolution of new techniques for imaging the central nervous system has produced significant advances in our understanding of the changes in brain structure and function associated with neurodegenerative disease. Magnetic resonance spectroscopy (MRS) has provided insights into some of the underlying metabolic abnormalities, thereby helping to elucidate the underlying pathophysiology of these disorders. Unlike traditional, tracer-based methods of molecular imaging, MRS is based on the behavior of specific nuclei within a magnetic field and the general principle that the resonant frequency of a nucleus depends on its immediate chemical environment. Although the behavior of native nuclei, such as hydrogen (1H) and phosphorous (31P), has formed the basis for the majority of clinical studies done with MRS thus far, other techniques being explored include those involving the administration of exogenous compounds such as 13C labeled lactate or glucose.
1H-Spectroscopy
Most clinical MRS research has concentrated on the metabolites visible with proton (1H) spectroscopy and measured in specified tissue volumes in the brain. With suppression of the MR signal arising from protons in water, it is possible to measure the protons in metabolites that are present at a much lower concentration than water. The metabolites that can be most readily studied with 1H-MRS at long echo times include N-acetyl aspartate (NAA), choline (Cho), creatine (Cr)/phosphocreatine (PCr), and lactate. Although NAA is one of the most abundant molecules in the human brain, accounting for approximately 1% of the brain’s dry weight, there is little hard evidence, but many hypotheses, regarding its role in the brain [1]. NAA is contained almost exclusively within neurons [2] and is therefore considered to act as an in vivo marker of neuronal loss and/or viability. Reduced regional NAA concentrations have been reported in conditions that are characterized by neuronal or axonal loss [3–7]. Because the enzyme responsible for NAA synthesis is present in high concentration in mitochondria, reduced neuronal NAA content may indicate mitochondrial dysfunction [8]. Cho is a precursor to cell membrane phosphatidylcholine, which represents about 40% of the phospholipid contents of cell membranes. The Cho MRS peak measures total levels of mobile Cho, including glycerophosphorylcholine (a byproduct of phosphatidylcholine breakdown) and phosphocholine (a phosphatidylcholine precursor), as well as free Cho, and acetylcholine (present in small concentrations). Altered neuronal membrane synthesis and degradation can therefore produce changes in the Cho peak [9].
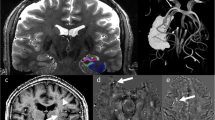
At short echo times, additional compounds are evident with 1H-MRS. These include myo-inositol (mI), a putative marker for neuroglia, the excitatory neurotransmitter glutamate (Glu) and its metabolic counterpart glutamine (Gln), and the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). Although these compounds are of considerable neuroscientific interest, their accurate quantification with MRS can represent a significant challenge due to their low concentration, their strongly coupled and complex spin systems, and their overlapping spectroscopic resonances, as reviewed by Allen et al. [10]. A typical short-echo 1H spectrum is illustrated in Fig. 1.
Typical 1H spectrum from right frontal cortex in a normal volunteer (voxel size 2.5 × 2.5 × 2.5 cm; field strength 1.5 tesla; echo time 20 ms). The lower line corresponds to actual acquired in vivo MR data. Subspectra for each metabolite, with the SUM of these spectra, are shown in the upper set of lines. These subspectra illustrate the decomposition of the acquired spectrum into its components, utilizing LCModel quantitative analysis [74]. Relative metabolite concentrations are determined from the areas under the peaks in these subspectra. Metabolites shown are Creatine + phosphocreatine (Cr + PCr), gamma-aminobutyric acid (GABA), glutamine (Gln), glutamate (Glu), N-acetylaspartyl glutamate (NAAG), N-acetylaspartate (NAA), myo-inositol (myo-Ino), choline (Cho), and aspartate (Asp). Figure courtesy of Chris Hanstock, Ph.D.
Most MRS studies have utilized a single voxel technique in which spectroscopic data are acquired from a single predefined volume of interest, of necessity containing a combination of gray matter, white matter, and cerebrospinal fluid. This is often combined with an MRI segmentation sequence allowing for determination of the relative weighting of these different tissue types. Increasingly, MRS is being performed with a multivoxel spectroscopic imaging technique that utilizes phase-encoding to derive individual spectra from multiple anatomically localized voxels during the same imaging sequence.
Most frequently, published NAA measurements have been based on the regional NAA/Cr ratio. The rationale for the use of the Cr resonance as the denominator comes from the concept that Cr and PCr are in chemical equilibrium, and that the total regional concentration of both compounds is expected to be unaffected by neurodegenerative disease processes. Alternate methods are available for the measurement of metabolite concentrations, however, such as those using the unsuppressed regional brain water signal as an internal standard [11] and those involving calibration to an external standard of known concentration [12]. More widespread implementation of these methods in the future should allow for a significant improvement of the quantitative accuracy of 1H-MRS.
Parkinson’s Disease and Related Disorders
Based on the concept that NAA is a marker of functional neuronal integrity, several studies utilizing 1H-MRS in Parkinson’s disease (PD) have been reported, as reviewed by Davie [13] and by Clarke and Lowry [14]. A large multicenter study in 151 patients with PD showed no significant difference in either NAA/Cr or NAA/Cho ratios between controls and patients who were not taking levodopa [15]. Similar results have been reported by others [16–18]. Similarly, in a small study using absolute metabolite quantitation, NAA, Cr, and Cho concentrations in PD did not differ significantly from those measured in controls [19]. In contrast to these studies, although no significant difference was observed in the NAA/Cr ratio in levodopa-treated patients with PD, Ellis and colleagues reported NAA/Cr to be reduced in drug-naïve PD patients [20]. These authors suggested that the reduced ratio in PD may reflect a functional abnormality of neurons in the putamen that can be reversed with levodopa treatment. Clarke and Lowry reported a significant decrease in the NAA/Cho ratio in PD due to an increase in the absolute concentration of Cho unassociated with a change in NAA concentration [21]. The variability in the results of these studies provides some indication of the difficulties associated with the interpretation of metabolite ratios and the importance of employing reliable methodology for absolute quantitation.
O’Neill and colleagues recently reported a small study using quantitative 1H-MRS, in which multiple tissue volumes were assessed [22]. This study applied more rigorous MR methodology than had been used in previous studies, including tissue segmentation to correct for varying gray and white matter content within the volumes of interest and the use of spectroscopic imaging to provide more widespread sampling of multiple brain regions. Observations from this study included decreased Cr concentration in the substantia nigra, but normal NAA and Cho levels. No differences in NAA, Cr, or Cho content were observed between PD patients and controls in other basal ganglia or multiple cortical volumes. These data provide further evidence of the difficulties associated with the interpretation of metabolite ratios that are based on the use of Cr as a denominator and the importance of appropriate quantitative methodology.
The major pathology underlying PD is a loss of dopaminergic neurons in the substantia nigra. This is a challenging structure to study with MRS due to its small size and its high iron content. Oz et al. have recently reported the application of short-echo (five milliseconds), high-field (four tesla) MRS to studies of the unilateral midbrain, acquiring spectroscopic data from 2.2 ml volumes centered on the substantia nigra [23]. They reported a fourfold higher GABA/Glu ratio in substantia nigra than in cerebral cortex, in agreement with established neurochemistry. These preliminary observations, in conjunction with the current proliferation of high-field MR systems, expand the horizons of the type of neurobiological information that can be obtained noninvasively with MRS and can ultimately be applied to studies of neurodegenerative disease.
There is increasing recognition that PD is a multisystem disorder with neuronal dysfunction which is not restricted to dopaminergic pathways or to the basal ganglia. Consistent with this, cortical changes have been reported with a reduced NAA/Cr ratio in motor cortex [24], temporoparietal cortex [25], and posterior cingulate cortex [26]. In PD patients without dementia, the degree of reduction in temporoparietal cortex correlates with measures of global cognitive decline [25].
In contrast to the apparent lack of changes in PD basal ganglia, there does appear to be a significant reduction in basal ganglia NAA concentration in a related neurodegenerative disorder, multiple system atrophy (MSA). Davie et al. reported 1H-MRS studies in the lentiform nucleus in controls and in patients with PD and with clinically probable MSA [16]. In MSA, there was a significant reduction in absolute levels of NAA, particularly in patients with the striatonigral degeneration subtype of MSA, suggesting that the spectroscopic measurement of NAA levels may provide a clinically useful technique to help differentiate MSA from PD. Although Federico et al. showed similar changes in MSA [27], a study using absolute quantitation of metabolite concentrations reported NAA to be unchanged in MSA [21]. Watanabe et al. utilized high-field MRS (three tesla) and observed NAA/Cr to be significantly reduced in the pontine base and putamen in patients with MSA, corresponding to the known widespread neuronal involvement in this disorder, and suggested that these measurements may be of diagnostic value in early disease [28].
Axelson and colleagues have developed an interesting alternate approach to the analysis of spectroscopic data based on pattern recognition with an artificial neural network [29]. These investigators reported that, while conventional data analysis, i.e., estimation of metabolite ratios from peak area measurements, showed no significant abnormalities in PD, trained neural networks could distinguish control from PD spectra with considerable accuracy.
Several issues contribute to the variability of the results which have been reported in these spectroscopic studies. As mentioned above, one major potential source of confusion is the methodology used to quantify metabolite concentrations [30]. Perhaps the most widely used approach is to express the data as a ratio between the metabolite of interest and an endogenous metabolite (such as Cr) that is presumed to remain constant. The accuracy of these ratio-based methods is therefore directly related to the accuracy of the assumption that the chosen standard is appropriate. Most studies have reported only a small number of patients, often with fewer than ten individuals in each group. The patient groups themselves have varied somewhat from study to study, with some patients having early, untreated PD, and others having more advanced disease requiring treatment. Variability in the MR technique itself, for example in the choice of echo time, may lead to heterogeneous results. Lastly, it must be considered that the high iron content in the basal ganglia has a significant impact on the ability to obtain reproducible high-resolution spectra from this tissue volume and may impact on the accuracy of quantitative results extracted from the spectra.
Amyotrophic Lateral Sclerosis
The utility of NAA as a neuronal marker has also been exploited in amyotrophic lateral sclerosis (ALS), a disorder characterized primarily by the degeneration of motor neurons from the motor cortex, brain stem, and spinal cord. Not surprisingly, a reduced NAA/Cr ratio corresponds to the anatomy of the corticospinal tracts with changes in the primary motor cortex and with a lesser decrease in primary sensory cortex and premotor areas [31–34]. Reduced NAA/Cr ratio in the motor cortex [35] and the brainstem [36] has been shown to have a high concordance with the presence of upper motor neuron signs.
In a cross-sectional study, Suhy and colleagues [37] showed that the NAA/(Cr + Cho) ratio was reduced in the motor cortex, but suggested that this was due not only to reduced NAA but also to increases in Cr and Cho. The Cr and Cho changes were postulated as being secondary to gliosis and membrane phospholipid breakdown. In longitudinal studies, these investigators found a progressive reduction in each of these metabolites in motor cortex associated with disease progression but no consistent changes in the metabolite ratios. These data again demonstrate the importance of accurate, reproducible, quantitative MRS methodology and the difficulties associated with the interpretation of ratio measures.
A recent study [38] utilized a specially tailored pulse sequence and high-field MRS (three tesla) to evaluate the putative glial marker mI to evaluate the hypothesis that combined measurements of neuronal function and glial function would enhance the ability of MRS to distinguish patients with ALS from control subjects. The resonances of mI are not well resolved at lower field strengths because they originate from a strongly coupled and complex spin system and overlap with resonances from Glu, Gln, glycine, and taurine. These investigators provided evidence that the NAA/mI ratio is a sensitive measure of neuropathology in ALS.
For the most part, ALS is considered to be a relentlessly progressive disorder with no effective treatment, although the antiglutamatergic drug riluzole does have a mild disease-altering effect. Kalra et al. have reported an increase in NAA/Cr ratio in the motor cortex of ALS patients approximately three weeks after starting riluzole [39]. These authors suggest that the increase is due to improved mitochondrial function resulting from a reduction in Glu-mediated excitotoxicity.
Alzheimer’s Disease
Alzheimer’s disease (AD) is characterized by widespread neuronal loss, particularly affecting associative cortical areas, with the medial temporal lobe being the site of the earliest neuronal loss. Reduced NAA ratios have been reported in this region by several groups [40, 41]. The specificity of these changes for AD is supported by the absence of significant changes in metabolite ratios in brain regions that are relatively unaffected in AD, by the observed correlation between NAA/Cr reduction and dementia severity [41], and by the absence of similar changes in patients with cognitive impairment from other (nonneurodegenerative) causes [42]. Kantarci and colleagues, however, have provided evidence that the NAA and mI changes may also occur in other degenerative dementias [43]. In particular, NAA/Cr levels are decreased in posterior cingulate cortex in dementias characterized by neuronal loss, such as AD, frontotemporal lobar degeneration (FTLD), and vascular dementia, whereas mI/Cr levels are elevated in dementias characterized by the presence of gliosis, such as AD and FTLD.
Huang and colleagues utilized 1H-MRS with short echo times and external standards to quantify brain concentrations of mI, NAA, Cr, and Cho in occipital and parietal regions in patients fulfilling clinical criteria for a diagnosis of AD [44]. NAA concentrations were significantly decreased, whereas mI and Cr concentrations were increased in patients compared to age- and sex-matched controls. Interestingly, the mI and Cr changes seemed to differentiate patients with mild disease from the control population. Significant changes in NAA were not evident in early AD but correlated with the severity of cognitive impairment. Because mI [45] and Cr have both been reported to be present in higher concentrations in astrocytes than in neurons, these results imply that glial proliferation may be an early change in AD, preceding significant neuronal loss or mitochondrial dysfunction, at least in the cortical regions surveyed in this study. This study provides further evidence supporting the importance of absolute metabolite quantitation as opposed to the use of metabolic ratios. Changes in these metabolites may also occur as part of the normal aging process, as shown by the demonstration of a significant increase in mI over a period of three years in male subjects in a longitudinal study [46]. Postmortem analysis of AD brains has shown a strong correlation between neurofibrillary tangles and increases in mI [47].
Minimal cognitive impairment (MCI) has been considered to be a transitional condition between normal aging and AD, although not all MCI patients will eventually develop dementia. MRS studies in patients with MCI have reported conflicting results, including both increased [48, 49] and normal mI levels [50, 52], unlike AD itself in which nearly all reported studies have indicated increased mI concentrations [51]. In contrast, MCI patients do seem to have changes in medial temporal NAA content [50, 52]. Possible explanations for the variable MRS results include the composition of brain tissue within the volume of interest, as well as volume placement itself.
MRS may have some predictive value in patients with MCI. In a longitudinal study with a three-year clinical follow-up period and with single-voxel MRS in hippocampus, parietal, and occipital volumes, baseline occipital NAA/Cr was significantly lower in patients who developed presumed AD vs. those who did not, with a value below 1.61 predicting the development of dementia with 100% sensitivity and 75% specificity [53]. In contrast, hippocampal and parietal measurements afforded no predictive value. These investigators did not segment the volume of interest into its constituent tissue types, however, so reported values correspond to a variable mix of gray and white tissue and CSF.
An interesting alternate approach to MRS has been reported by Falini et al. [54]. To avoid the limitations related to the vagaries of voxel placement, particularly in longitudinal studies in which repositioning is critical, these investigators utilized a nonlocalized technique to quantify the concentration of NAA in the whole brain. Whole brain NAA was significantly decreased in patients with MCI vs. control subjects; there was no significant difference between these patients, however, and those with a clinical diagnosis of AD.
Proton MRS has been applied to several studies of transgenic mouse models of AD. In a model that coexpresses mutated human presenilin 1 and amyloid-β precursor protein [55], a dramatic increase in mI concentration was reported, as well as a reduction in NAA occurring with increasing age, consistent with observations in human AD. These findings provide further support for the importance glial activation in the pathophysiology of the disease and for the validity of the model itself. Other transgenic mouse models have shown decreased NAA, but did not replicate the mI changes which appear to be a major component of human AD [56, 57].
31P-Spectroscopy and Energy Metabolism
Phosphorous (31P) MRS can be used to study high-energy phosphate metabolites, thereby providing an in vivo assessment of the bioenergetic status of tissues. It is less sensitive than is 1H-MRS, requiring that data be acquired from much larger volumes of interest. The major peaks evident on 31P-MRS include α, β, and γ nucleotide triphosphates (which reflect ATP levels), PCr (an indicator of oxidative metabolism), phosphodiesters and phosphomonoesters (related to cell membranes), and inorganic phosphate (Pi) (from which intracellular pH can be derived). A typical 31P spectrum is illustrated in Fig. 2.
Typical 31P spectrum from temporo-occipital cortex in a normal volunteer (voxel size 3 × 3 × 3 cm; field strength three tesla; surface coil for data acquisition). Metabolites shown are phosphomonoesters (PME); phosphodiesters (PDE); phosphocreatine (PCr); inorganic phosphate (Pi); and the α, β, and γ groups of adenosine trinucleotide phosphate (ATP). Figure courtesy of Chris Hanstock, Ph.D.
Although the etiology of PD is unknown, the possibility of an underlying defect in mitochondrial metabolism has been addressed in several biochemical studies [58]. There is evidence of reduced complex I activity in the substantia nigra in PD, and a mitochondrial DNA abnormality may underlie this complex I defect in at least a subgroup of PD patients [59]. Studies in other tissues, however, have produced conflicting results, perhaps in part because biochemical studies involve the removal of mitochondria from their natural milieu, with consequent mechanical disruption and loss of normal control mechanisms. In contrast, MRS provides the potential to study mitochondrial metabolism in vivo.
The rate of intracellular energy metabolism is reflected by the ratio of Pi to PCr, readily measured with 31P-MRS. The measurement of this ratio in resting muscle has been shown to be a useful diagnostic test for mitochondrial disease [60]. Penn et al. used 31P-MRS to investigate energy metabolism in muscle in patients with PD [61]. The Pi/PCr ratio was significantly increased in PD, suggesting a small, generalized mitochondrial defect. Further studies are needed to determine whether these changes are limited to a clinically definable subset of parkinsonian individuals.
The main function of mitochondria is to maintain an adequate intracellular concentration of high-energy phosphates to support metabolic activities. Evidence of mitochondrial impairment, therefore, may be more readily obtained in situations of increased metabolic workload than at rest. Rango and colleagues [62] have reported 31P-MRS in the visual cortex in patients with PD and normal subjects at rest, during, and after visual activation. In controls, high-energy phosphates were unchanged during activation, but rose during recovery. In PD patients, high-energy phosphates were normal at rest, did not change during activation, and fell significantly during recovery. These data suggest the presence of an energy imbalance in PD with mitochondrial dysfunction evident during periods of increased oxidative demand, such as in the postactivation period. Energy failure is not evident during activation itself, possibly because demands during this time are met primarily by increased anerobic glycolysis, a process that does not rely on mitochondria [63]. The fact that the dysfunction is present in the visual cortex is of interest and provides further support for the presence of widespread mitochondrial impairment in PD.
31P-MRS studies of the brain have been reported in comparisons of MSA and PD [64]. In these studies, patients with MSA showed significantly increased Pi content and reduced PCr content, whereas those with PD showed significantly increased Pi but unchanged PCr, suggesting abnormal energy metabolism in both disorders. The combination of 31P-MRS and fluorodeoxyglucose/PET has been used to suggest that temporoparietal cortical glycolytic and oxidative metabolism are both impaired in nondemented PD patients [65]. These observations are consistent with a previous report of temporoparietal cortical reduction in NAA/Cr ratio in nondemented PD patients, which correlated with measures of global cognitive decline independently of motor impairment [25]. In contrast, however, Hoang and colleagues reported normal energy metabolism in the putamen as well as the parietal and occipital lobes in PD, using both 31P- and 1H-MRS [66].
In vivo 31P-MRS studies of phospholipid metabolism have been reported in patients with mild to moderate AD [67]. The phosphate monoester resonance and the phosphate monoester/diester ratio were increased in the prefrontal cortex of AD patients, suggesting either increased synthesis of membrane phospholipids, a reduction in membrane breakdown, or perhaps a combination of these two mechanisms. The degree of abnormality correlated with the degree of cognitive impairment. Future studies of membrane phospholipids with MRS may add to our knowledge of the neuronal changes underlying the development of AD and other neurodegenerative diseases.
An alternate approach to studying energy metabolism is with 1H-MRS. Normal brain energy production is derived from the oxidative metabolism of glucose by way of the Krebs cycle and, ultimately, the electron transport chain. A defect at the level of either of the two latter processes will result in decreased metabolism of pyruvate through these pathways and increased production of lactate. Regional brain lactate concentrations can be readily assessed with 1H-MRS. For example, this methodology has been utilized to demonstrate increased occipital lactate levels, thereby suggesting impaired energy metabolism in Huntington’s disease [68]. We have found similar changes in some but not all patients with PD (unpublished observations), providing further evidence for the presence of a mitochondrial defect in this disorder.
13C-Spectroscopy
It is well established that, under normal conditions, glucose oxidation is the primary mechanism for cerebral energy production. MRS following the administration of 13C-labeled glucose detects the appearance of 13C signal in metabolites of glucose metabolism, assuming their presence in sufficient concentration. Infusion of [1-13C]- glucose results in abundant labeling of [4-13C]-Glu, with the rate of 13C label accumulation providing an estimate of the rate of the tricarboxylic acid cycle. Subsequent labeling of [4-13C]-Gln provides a measure of the rate of the Glu–Gln cycle. Direct 13C-MRS offers a high spectral resolution and a clear discrimination of metabolite resonances, but has relatively low sensitivity. The indirect detection of 13C signal by 1H-[13C]-MRS, which detects the protons attached to 13C nuclei, although more technically demanding, may provide increased sensitivity, allowing for data acquisition from smaller tissue volumes. The interested reader is referred to one of the recent reviews of the principles underlying 13C-MRS [69–71].
More than 90% of cortical neurons utilize either Glu, as the major excitatory neurotransmitter of the central nervous system, or GABA, as its major inhibitory neurotransmitter. Glu is also a precursor of GABA, and therefore, its metabolism plays a central role in both excitatory and inhibitory functions. Knowledge of the compartmentalization of Glu/Gln metabolism in conjunction with 13C-MRS experiments has not only enabled the development of quantitative models of glucose metabolism, but has enhanced our understanding of the links between neuronal energy production and glutamatergic neurotransmission. Quantitative measurements of Glu–Gln cycling and of neuronal glucose oxidation with 13C-MRS have suggested a very close relationship between the rates of Glu neurotransmission and energy metabolism [72].
Excitatory glutamatergic neurotransmission is thought to consume more than 80% of the ATP generated from glucose oxidation. Incorporation of [1-13C]-labeled glucose into cerebral Glu and Gln pools allows for direct in vivo measurement of glutamatergic neurotransmission. Lin and colleagues [73] utilized this technique in three AD patients to measure occipital glutamatergic neurotransmission, glucose oxidation, and the neuronal tricarboxylic acid cycle, and reported significant differences between patients and age-matched controls. These changes correlated with MRS measures of neuronal integrity (NAA/Cr, [NAA], and mI/NAA), consistent with the notion that impaired glutamatergic neurotransmission may contribute to the pathophysiology of AD.
13C-MRS is still in its infancy and has not yet been applied extensively in patient studies. Although technically demanding, in conjunction with recent developments in high-field (seven tesla and greater) MR hardware, it has tremendous potential for helping to unravel the intricacies of brain metabolism and of neurodegenerative disease pathophysiology.
Conclusion
In summary, MRS provides a noninvasive tool to assess the regional concentration of certain metabolites in patients with neurodegenerative disorders. Its ability to quantify compounds such as N-acetylaspartate, a neuronal marker, and Cho, the basis for a number of cell membrane constituents, has provided useful information regarding the neuronal populations affected in these disorders. This type of information, however, represents only a small part of the promise of MRS. 1H-MRS also affords the potential to study compounds such as Glu and GABA, whereas 13C-MRS offers significant benefits in terms of studies of bioenergetics and glutamatergic neurotransmission. The future application of these tools is expected to yield important insights to the pathophysiology of neurodegenerative disease.
References
Clark JF, Doepke A, Filosa JA, et al. (2006) N-acetylaspartate as a reservoir for glutamate. Med Hypotheses 67:506–512
Urenjak J, Williams SR, Gadian DG, Noble M (1993) Proton nuclear magnetic resonance spectroscopy unambiguously identifies different neural cell types. J Neurosci 13:981–989
Matthews PM, Francis G, Antel J, Arnold DL (1991) Proton magnetic resonance spectroscopy for metabolic characterisation of plaques in multiple sclerosis. Neurology 41:1251–1256
Chong WK, Sweeney B, Wilkinson ID, et al. (1993) Proton spectroscopy of the brain in HIV infection: correlation with clinical, immunologic and MR imaging findings. Radiology 188:119–124
Shino A, Matsuda M, Morikawa S, Inubushi T, Akiguchi I, Handa J (1993) Proton magnetic resonance spectroscopy with dementia. Surg Neurol 39:143–147
Gideon P, Henriksen O, Sperling B, et al. (1992) Early time course of N-acetylaspartate, creatine and phosphocreatine, and compounds containing choline in the brain after acute stroke. A proton magnetic resonance spectroscopy study. Stroke 23:1566–1572
Cwik V, Hanstock C, Allen PS, Martin WRW (1998) Estimation of brainstem neuronal loss in amyotrophic lateral sclerosis with in vivo proton magnetic resonance spectroscopy. Neurology 50:72–77
Clark JB (1998) N-acetyl aspartate: a marker for neuronal loss or mitochondrial dysfunction. Dev Neurosci 20:271–276
Vion-Dury J, Meyerhoff DJ, Cozzone PJ, Weiner MW (1994) What might be the impact on neurology of the analysis of brain metabolism by in vivo magnetic resonance spectroscopy? J Neurol 241:354–371
Allen PS, Thompson RB, Wilman AH (1997) Metabolite-specific NMR spectroscopy in vivo. NMR Biomed 10:435–444
Christiansen P, Henriksen O, Stubgaard M, Gideon P, Larsson HBW (1993) In vivo quantification of brain metabolites by 1H MRS using water as an internal standard. Magn Reson Imaging 11:107–108
Michaelis T, Merboldt KD, Bruhn H, Hanicke W, Frahm J (1993) Absolute concentrations of metabolites in the adult human brain in vivo: quantification of localized proton MR spectra. Radiology 187:219–227
Davie C (1998) The role of spectroscopy in parkinsonism. Mov Disord 13:2–4
Clarke CE, Lowry M (2001) Systematic review of proton magnetic resonance spectroscopy of the striatum in parkinsonian syndromes. Eur J Neurol 8:573–577
Holshauser BA, Komu M, Moller HE, et al. (1995) Localised proton NMR spectroscopy in the striatum of patients with idiopathic Parkinson’s disease: a multicenter pilot study. Magn Reson Med 33:589–594
Davie CA, Wenning GK, Barker GJ, et al. (1995) Differentiation of multiple system atrophy from idiopathic Parkinson’s disease using proton magnetic resonance spectroscopy. Ann Neurol 37:204–210
Cruz CJ, Aminoff MJ, Meyerhoff DJ, Graham SH, Weiner MW (1997) Proton MR spectroscopic imaging of the striatum in Parkinson’s disease. Magn Reson Imaging 15:619–624
Tedeschi G, Litvan I, Bonavita S, et al. (1997) Proton magnetic resonance spectroscopic imaging in progressive supranuclear palsy, Parkinson’s disease and corticobasal degeneration. Brain 120:1541–1552
Clarke CE, Lowry M, Horsman A (1997) Unchanged basal ganglia N-acetylaspartate and glutamate in idiopathic Parkinson’s disease measured by proton magnetic resonance spectroscopy. Mov Disord 12:297–301
Ellis CM, Lemmens G, Williams SCR, et al. (1997) Changes in putamen N-acetylaspartate and choline ratios in untreated and levodopa treated Parkinson’s disease: a proton magnetic resonance spectroscopy study. Neurology 49:438–444
Clarke CE, Lowry M (2000) Basal ganglia metabolite concentrations in idiopathic Parkinson’s disease and multiple system atrophy measured by proton magnetic resonance spectroscopy. Eur J Neurol 7:661–665
O’Neill J, Schuff N, Marks WJ, Feiwell R, Aminoff MJ, Weiner MW (2002) Quantitative 1H magnetic resonance spectroscopy and MRI of Parkinson’s disease. Mov Disord 17:917–927
Oz G, Terpstra M, Tkac I, et al. (2006) Proton MRS of the unilateral substantia nigra in the human brain at 4 tesla: detection of high GABA concentrations. Magn Reson Med 55:296–301
Lucetti C, del Dotto P, Gambaccini G, et al. (2001) Proton magnetic resonance spectroscopy (1H-MRS) of motor cortex and basal ganglia in de novo Parkinson’s disease patients. Neurol Sci 22:69–70
Hu MTM, Taylor-Robinson SD, Chaudhuri KR, et al. (1999) Evidence for cortical dysfunction in clinically non-demented patients with Parkinson’s disease: a proton MR spectroscopy study. J Neurol Neurosurg Psychiatry 67:20–26
Camicioli RM, Korzan JR, Foster SL, et al. (2004) Posterior cingulate metabolic changes occur in Parkinson’s disease patients without dementia. Neurosci Lett 354:177–180
Federico F, Simone IL, Lucivero V, et al. (1999) Usefulness of proton magnetic resonance spectroscopy in differentiating parkinsonian syndromes. Ital J Neurol Sci 20:223–229
Watanabe H, Fukatsu H, Katsun M, et al. (2004) Multiple regional 1H-MR spectroscopy in multiple system atrophy: NAA/Cr reduction in pontine base as a valuable diagnostic marker. J Neurol Neurosurg Psychiatry 75:103–109
Axelson D, Bakken IJ, Gribbestad IS, Ehrnholm B, Nilsen G, Aasly J (2002) Applications of neural network analyses to in vivo 1H magnetic resonance spectroscopy of Parkinson disease patients. J Magn Reson Imaging 16:13–20
Tofts PS, Wray S (1988) A critical assessment of methods of measuring metabolite concentrations by NMR spectroscopy. NMR Biomed 1:1–10
Pioro EP, Antel JP, Cashman NR, Arnold DL (1994) Detection of cortical neuron loss in motor neuron disease by proton magnetic resonance spectroscopic imaging in vivo. Neurology 44:1933–1938
Kalra S, Cashman NR, Caramanos Z, Genge A, Arnold DL (2003) Gabapentin therapy for amyotrophic lateral sclerosis: lack of improvement in neuronal integrity shown by MR spectroscopy. AJNR Am J Neuroradiol 24:476–480
Kalra S, Genge A, Arnold D (2003) A prospective, randomized, placebo controlled evaluation of corticoneuronal response to intrathecal BDNF therapy in ALS using magnetic resonance spectroscopy: feasibility and results. Amyotroph Lateral Scler Other Motor Neuron Disord 4:22–26
Abe K, Takanashi M, Watanabe Y (2001) Decrease in N-acetylaspartate/creatine ratio in the motor area and the frontal lobe in amyotrophic lateral sclerosis. Neuroradiology 43:537–541
Kaufmann P, Pullman SL, Shungu DC, et al. (2004) Objective tests for upper motor neuron involvement in amyotrophic lateral sclerosis (ALS). Neurology 62:1753–1757
Cwik VA, Hanstock CC, Allen PS, Martin WRW (1998) Estimation of brainstem neuronal loss in amyotrophic lateral sclerosis with in vivo proton magnetic resonance spectroscopy. Neurology 50:72–77
Suhy J, Miller RG, Rule R, et al. (2002) Early detection and longitudinal changes in amyotrophic lateral sclerosis by 1H-MRSI. Neurology 58:773–779
Kalra S, Hanstock CC, Martin WRW, et al. (2006) Detection of cerebral degeneration in amyotrophic lateral sclerosis using high-field magnetic resonance spectroscopy. Arch Neurol 63:1144–1148
Kalra S, Cashman NR, Genge A, Arnold DL (1998) Recovery of N-acetylaspartate in corticomotor neurons of patients with ALS after riluzole therapy. Neuroreport 9:1757–1761
Schuff N, Capizzano AA, Du AT, et al. (2002) Selective reduction of N-acetyl aspartate in medial temporal and parietal lobes in AD. Neurology 58:928–935
Jessen F, Block W, Traber F, et al. (2000) Proton MR spectroscopy detects a relative decrease of N-acetylaspartate in the medial temporal lobe of patients with AD. Neurology 55:684–688
Frederick BD, Lyoo IK, Satlin A, et al. (2004) In vivo proton magnetic resonance spectroscopy of the temporal lobe in Alzheimer’s disease. Prog Neuropsychopharm Biol Psychiatry 28:1313–1322
Kantarci K, Petersen RC, Boeve BF, et al. (2004) 1H MR spectroscopy in common dementias. Neurology 63:1393–1398
Huang W, Alexander GE, Chang L, et al. (2001) Brain metabolite concentration and dementia severity in Alzheimer’s disease: a 1H MRS study. Neurology 57:626–632
Glanville NT, Byers DM, Cook HW, Spence MW, Palmer FB (1989) Differences in the metabolism of inositol and phosphoinositides by cultured cells of neuronal and glial origin. Biochim Biophys Acta 1004:169–179
Ross AJ, Sachdev PS, Wen W, Brodaty H (2006) Longitudinal changes during aging using proton magnetic resonance spectroscopy. J Gerontol A Biol Sci Med Sci 61A:291–298
Klunk WE, Xu C, Panchalingham K, McClure RJ, Pettegrew JW (1996) Quantitative 1H and 31P MRS of PCA extracts of postmortem Alzheimer’s disease brain. Neurobiol Aging 17:349–357
Catani M, Cherubini R, Howard R, et al. (2001) 1H-MR spectroscopy differentiates mild cognitive impairment from normal brain aging. Neuroreport 12:2315–2317
Kantarci K, Jack CR Jr, Xu YC, et al. (2000) Regional metabolic patterns in mild cognitive impairment and Alzheimer’s disease. Neurology 55:210–217
Chantal S, Braun CMJ, Bouchard RW, Labelle M, Boulanger Y (2004) Similar 1H magnetic resonance spectroscopic metabolic pattern in the medial temporal lobes of patients with mild cognitive impairment and Alzheimer disease. Brain Res 1003:26–35
Valenzuela MJ, Sachdev P (2001) Magnetic resonance spectroscopy in Alzheimer’s disease. Neurology 56:592–598
Ackl N, Ising M, Schreiber YA, Atiya M, Sonntag A, Auer DP (2005) Hippocampal metabolic abnormalities in mild cognitive impairment and Alzheimer’s disease. Neurosci Lett 384:23–28
Modrego PJ, Fayed N, Pina MA (2005) Conversion from mild cognitive impairment to probably Alzheimer’s disease predicted by brain magnetic resonance spectroscopy. Am J Psychiatry 162:667–675
Falini A, Bozzali M, Magnani G, et al. (2005) A whole brain MR spectroscopy study from patients with Alzheimer’s disease and mild cognitive impairment. Neuroimage 26:1159–1163
Marjanska M, Curran GL, Wengenack TM, et al. (2005) Monitoring disease progression in transgenic mouse models of Alzheimer’s disease with proton magnetic resonance spectroscopy. Proc Natl Acad Sci U S A 102:11906–11910
Dedeoglu A, Choi J-K, Cormier K, Kowall NW, Jenkins BG (2004) Magnetic resonance spectroscopic analysis of Alzheimer’s disease mouse brain that express mutant human APP shows altered neurochemical profile. Brain Res 1012:60–65
von Kienlin M, Kunnecke B, Metzger F, et al. (2004) Altered metabolic profile in the frontal cortex of PS2APP transgenic mice, monitored throughout their life span. Neurobiol Dis 18:32–39
DiMauro S (1993) Mitochondrial involvement in Parkinson’s disease: the controversy continues. Neurology 43:2170–2171
Gu M, Cooper JM, Taanman JW, Schapira AHV (1998) Mitochondrial DNA transmission of the mitochondrial defect in Parkinson’s disease. Ann Neurol 44:177–186
Matthews PM, Allaire C, Shoubridge EA, Karpati G, Carpenter S, Arnold DL (1991) In vivo muscle magnetic resonance spectroscopy in the clinical investigation of mitochondrial disease. Neurology 41:114–120
Penn AMW, Roberts T, Hodder J, Allen PS, Zhu G, Martin WRW (1995) Generalized mitochondrial dysfunction in Parkinson’s disease detected by magnetic resonance spectroscopy of muscle. Neurology 45:2097–2099
Rango M, Bonifati C, Bresolin N (2006) Parkinson’s disease and brain mitochondrial dysfunction: a functional phosphorus magnetic resonance spectroscopy study. J Cereb Blood Flow Metab 26:283–290
Fox PT, Raichle ME, Mintun MA, Dence C (1988) Nonoxidative glucose consumption during focal physiologic neural activity. Science 241:462–464
Barbiroli B, Martinelli P, Patuelli A, et al. (1999) Phosphorus magnetic resonance spectroscopy in multiple system atrophy and Parkinson’s disease. Mov Disord 14:430–435
Hu MTM, Taylor-Robinson SD, Chaudhuri KR, et al. (2000) Cortical dysfunction in non-demented Parkinson’s disease patients. A combined 31P-MRS and 18FDG-PET study. Brain 123:340–352
Hoang TQ, Bluml S, Dubowitz DJ, et al. (1998) Quantitative proton-decoupled 31P MRS and 1H MRS in the evaluation of Huntington’s and Parkinson’s diseases. Neurology 50:1033–1040
Forlenza OV, Wacker P, Nunes PV, et al. (2005) Reduced phospholipid breakdown in Alzheimer’s brains: a 31P spectroscopy study. Psychopharmacology (Berl) 180:359–365
Jenkins BG, Koroshetz WJ, Beal MF, Rosen BR (1993) Evidence for impairment of energy metabolism in vivo in Huntington’s disease using localized 1H NMR spectroscopy. Neurology 43:2689–2695
Morris P, Bachelard H (2003) Reflections on the application of 13C-MRS to research on brain metabolism. NMR Biomed 16:303–312
de Graaf RA, Mason GF, Patel AB, Behar KL, Rothman DL (2003) In vivo 1H-[13C]-NMR spectroscopy of cerebral metabolism. NMR Biomed 16:339–357
Gruetter R, Adriany G, Choi I-Y, Henry P-G, Lei H, Oz G (2003) Localized in vivo 13C NMR spectroscopy of the brain. NMR Biomed 16:313–338
Hyder F, Patel AB, Gjedde A, Rothman DL, Behar KL, Shulman RG (2006) Neuronal-glial glucose oxidation and glutamatergic-GABAergic function. J Cereb Blood Flow Metab 26:865–877
Lin AP, Shic F, Enriquez C, Ross BD (2003) Reduced glutamate neurotransmission in patients with Alzheimer’s disease—an in vivo 13C magnetic resonance spectroscopy study. MAGMA 16:29–42
Provencher SW (2001) Automatic quantitation of localized in vivo 1H spectra with LCModel. NMR Biomed 14:260–264
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Martin, W.R.W. MR Spectroscopy in Neurodegenerative Disease. Mol Imaging Biol 9, 196–203 (2007). https://doi.org/10.1007/s11307-007-0087-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11307-007-0087-2