Abstract
In addition to its intracellular roles, the nucleoside guanosine (GUO) also has extracellular effects that identify it as a putative neuromodulator signaling molecule in the central nervous system. Indeed, GUO can modulate glutamatergic neurotransmission, and it can promote neuroprotective effects in animal models involving glutamate neurotoxicity, which is the case in brain ischemia. In the present study, we aimed to investigate a new in vivo GUO administration route (intranasal, IN) to determine putative improvement of GUO neuroprotective effects against an experimental model of permanent focal cerebral ischemia. Initially, we demonstrated that IN [3H] GUO administration reached the brain in a dose-dependent and saturable pattern in as few as 5 min, presenting a higher cerebrospinal GUO level compared with systemic administration. IN GUO treatment started immediately or even 3 h after ischemia onset prevented behavior impairment. The behavior recovery was not correlated to decreased brain infarct volume, but it was correlated to reduced mitochondrial dysfunction in the penumbra area. Therefore, we showed that the IN route is an efficient way to promptly deliver GUO to the CNS and that IN GUO treatment prevented behavioral and brain impairment caused by ischemia in a therapeutically wide time window.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Guanine-based purines (GBPs), specifically the nucleoside guanosine (GUO) and the nucleotides guanosine-5′-mono-, di-, and triphosphate (GMP, GDP, and GTP, respectively), are endogenous molecules and members of the purinergic system, which are known to participate in several intracellular processes. In the central nervous system (CNS), in addition to their intracellular roles, GBPs present extracellular effects that suggest they are putative neuromodulator signaling molecules [1]. Indeed, GBPs can modulate neurotransmitter systems, particularly glutamatergic neurotransmission. Specifically, the nucleoside GUO has been shown to stimulate astrocytic glutamate (GLU) uptake [2, 3] and to inhibit GLU vesicular storage [4], thus modulating glutamatergic synaptic transmission. As GLU is the main excitatory neurotransmitter in the CNS, and excessive GLU signaling (excitotoxicity) is involved with several brain diseases [5, 6], the neuroprotective potential of GUO against excitotoxicity has been investigated. Accordingly, the exogenous administration of GUO has shown neuroprotective effects on CNS injury in several animal models linked to excitotoxicity events, including models of dementia [7], seizures [8, 9], neuropathic pain [10], stroke [11–15], and hepatic encephalopathy [16].
Although modulatory and neuroprotective potentials of GUO were strongly demonstrated, GUO mechanism of action is not fully understood. A putative binding site for GUO was already described in rat brain membranes [17], but in opposite, several evidences point to an adenosine (ADO) receptors contribution for GUO effects. Indeed, some, but not all of the observed neuroprotective effects of GUO, were blocked by ADO receptor antagonists, suggesting multiple mechanisms of action for GUO [18–22]. Certainly, GUO effects seem to be directly mediated by action on the brain, as intracerebroventricular or intracortical GUO infusion in experimental models of excitotoxicity have demonstrated neuroprotection [8, 13]. Nevertheless, most of the neuroprotective effects exerted by GUO were observed after its systemic (intraperitoneal [IP] or oral) administration [7, 9–16]. In this regard, systemic administration routes present important limitations for protocols with endogenous drugs that aim to reach the brain but can be metabolized in the systemic pathway, which is the case for GUO. GUO can be enzymatically degraded to guanine both extra- and intracellularly and subsequently reduced to xanthine (XAN) and uric acid (UA). Moreover, the interconversion among guanine- and adenine-based purines, such as ADO and its derivatives inosine (INO) and hypoxanthine (HYPO), plays an important role in maintaining purine homeostasis [23, 24]. Therefore, a long systemic pathway could decrease the amount of GUO that reaches the brain by metabolization and/or uptake, consequently decreasing the effectiveness of the administered dose [25, 26].
An intranasal (IN) route of administration appears to be a relevant alternative for delivering compounds to the CNS. Several works have demonstrated transport of macromolecules across the nasal epithelia, sometimes faster and higher than the conventional intravascular pathway [27–31]. Currently, it is thought that substances that are able to cross the nasal epithelial barrier can reach the brain through components associated with the olfactory and trigeminal nerves after IN administration. Subsequently, they are rapidly distributed throughout the brain by convective perivascular space flow. Hence, the IN route of administration may be a particularly attractive drug delivery method to manage cerebrovascular diseases, such as stroke [27, 28]. Accordingly, therapeutic proteins and other molecules were delivered to ischemic brains, suggesting that IN administration is clearly a promising route for stroke therapy [29–31]. Thus, IN GUO administration could offer a potential means of improved delivery to the brain.
Recently, we have shown neuroprotective effects of IP treatment with GUO early after permanent focal cerebral ischemia [11, 12], which caused a significant and long-lasting recovery of the impaired behavioral function and decreased the extension of brain infarct volume. These effects were related to modulation of the glutamatergic system, cellular redox environment, and inflammatory cytokine balance in the penumbra area (periphery of lesion), the main presumptive site of endogenous restorative processes and, thus, of the therapeutic target site. Like the conventional drugs to manage stroke, IP GUO was shown to be effective when administered immediately after the induction of experimental brain ischemia [11, 12].
Taken together, in the present work, we aimed to investigate the neuroprotective potential of IN GUO following brain ischemia as an alternative strategy to avoid GUO metabolization and compromised blood circulation as a consequence of ischemia. Thus, we induced a permanent focal cerebral ischemia in rats searching for a therapeutic time window for IN GUO treatment. Preliminarily, we evaluated pharmacokinetic parameters of IN GUO administration and compared them with an IP route using radiolabeled [3H] GUO administration and purine levels determination in brain structures, blood plasma, and cerebrospinal fluid (CSF).
Materials and methods
Chemicals
GUO, acetonitrile (ACN), trifluoroacetic acid (TFA), and methyl triphenyl tetrazolium chloride (TTC) were purchased from Sigma (St. Louis, MO, USA). Methacrylate resin was from Leica®, and methylene blue was obtained from Merck®. [3H] GUO (specific activity 15 Ci/mmol) was obtained from American Radiolabeled Chemicals (St. Louis, MO, USA). The anesthetic ketamine hydrochloride and xylazine were obtained from Syntec Brazil (Cotia, SP, Brazil). All other chemicals were of analytical grade and obtained from standard suppliers.
Animals
One hundred fifty adult male Wistar rats (60–90 days old) were obtained from the animal facility house of the Department of Biochemistry, ICBS, UFRGS. The animals were kept under a 12-h light/dark cycle (light on at 7:00 am) at a temperature of 22 ± 1° C. They were housed in plastic cages (five per cage) with water and commercial food available ad libitum. The animals were anesthetized by IP administration of both ketamine hydrochloride (50 mg/kg) and methyl xylazine (10 mg/kg). The IP injection volume was 1 ml/kg. Animals were sacrificed by decapitation using a guillotine. All experiments were performed following the rules of the Ethics Committee on Animal Use - CEUA-UFRGS. The protocols were approved by the CEUA-UFRGS, Project No.: 22319.
Preparation and administration of IN [3H] GUO solution
A mother solution of unlabeled GUO (120 mg/ml) was prepared on the day of each experiment, and it was used to prepare all the different concentrations of GUO used in the study. Unlabeled GUO at each concentration specified was mixed with a fixed amount of radiolabeled [3H] GUO (0.5 mCi/ml, specific activity 15 Ci/mmol). The mixture of unlabeled GUO with tracer amounts of [3H] GUO was named as [3H] GUO solution.
Six rats per each condition analyzed were anesthetized, and the [3H] GUO solution was administered to both nostrils of each animal at the bottom of the nasal septum with a pipette tip with a long edge. The administered volume of [3H] GUO solution was applied slowly, and the interval between each nostril administration was approximately 2 min. After the time interval specified for each group protocol, blood samples were transcardially collected and the animals were decapitated and the brain structures (i.e., olfactory bulb, parietal cortex, hippocampus, and cerebellum) were dissected and processed.
Rats that received no interference, such as anesthesia, surgery, and/or treatment, were considered control animals that were designated as “naïve” group in each analyses. At the end of the experiments, all naïve animals were grouped into a single population to consider inter-experimental variability (eight rats in total). Thus, the control group was identical for all comparisons in this work.
Evaluation of pharmacokinetic parameters of IN [3H] GUO solution administration
We investigated dose curve and time distribution of IN [3H] GUO into the rat brain and blood plasma. The dose curve of IN [3H] GUO solution was evaluated by applying 0.05 ml per nostril of different concentrations of [3H] GUO solution (2.5, 7.5, 15, 30, and 60 mg/ml) and assessing the radioactivity content and purine levels in brain structures and blood plasma 15 min after administration. Based on the unlabeled GUO concentration and the radioactivity detected for each solution administered, we estimated the dose curve for [3H] GUO exposure of each brain structures and blood plasma. To achieve the IN [3H] GUO time curve, we applied 30 mg/ml IN [3H] GUO solution, 0.05 ml per nostril, and evaluated the radioactivity content and purine levels after 5, 15, 60, 120, and 180 min.
Comparison between IN and IP [3H] GUO administration
The [3H] GUO solution (30 mg/ml) was injected IN (IN GUO, 0.05 ml per nostril) or IP (IP GUO 0.1 ml). After 5 min, the radioactivity and purine levels of the brain structures, CSF, and plasma samples were determined.
Brain structure processing
The olfactory bulb, parietal cortex, hippocampus, and cerebellum were dissected from the brain, weighed, and the right hemisphere structures were used for quantification of radioactivity (by liquid scintillation counter Hidex 300 SL), and the left hemisphere structures were used for determination of purines by high performance liquid chromatography (HPLC) measurements. The following procedure was performed for both hemispheres according to [25] with minor modifications; the structures were homogenized in 0.6 ml of 7 % TFA, except the bulb, which was homogenized in 0.3 ml of 7 % TFA for deproteinization. Next, the homogenates were centrifuged at 10,000×g at 4 °C for 10 min, and the supernatants were collected. Aliquots of 0.2 and 0.4 ml from the olfactory bulb and other structures, respectively, were used to measure the radioactivity content. To analyze purines by the HPLC method, an aliquot of 0.1 ml was neutralized with 0.075 ml of 1.5 M potassium bicarbonate (KHCO3). After, the samples were filtered through cellulose 0.22 μm pore size membrane and finally stored at −70 °C.
CSF and plasma sampling
CSF samples (approximately 0.1 ml) were removed by direct puncture of the cisterna magna with an insulin needle in a stereotactic apparatus. Each sample was centrifuged at 10,000×g at 4 °C for 10 min to obtain a cell-free supernatant. This supernatant was filtered through a cellulose 0.22 μm pore size membrane, and the samples were individually stored at −70 °C.
Blood was withdrawn (approximately 2 ml) by cardiac puncture and added to collection tubes containing sodium citrate as an anticoagulant. The samples were centrifuged at 5000×g for 10 min and the supernatant (plasma) was collected. An aliquot of 0.4 ml was added to 0.6 ml of 7 % TFA to deproteinization. After, the samples were centrifuged at 10,000×g at 4 °C for 10 min and the supernatant was collected. A supernatant aliquot (0.4 ml) was collected for radioactivity analysis. Another aliquot (0.1 ml) was submitted to the same process of neutralization and storage as brain structures and it was used for purines analysis.
HPLC
Determination of the purines concentration in CSF, blood plasma, and brain structures was performed using the methodology of HPLC described previously [7]. The injected sample volume was 0.02 ml. The following purines were analyzed: ADO, INO, HYP, GUO, XAN, and UA.
Evaluation of the neuroprotective potential of IN GUO treatment in the cerebral ischemia model
To investigate the neuroprotective potential of IN GUO treatment, we used a permanent focal cerebral ischemia model in rats and evaluated parameters of behavioral functionality (cylinder test), histological damage (infarct volume by TTC stained), and mitochondrial dysfunction at the penumbra area (MitoTrackerTM analyses).
Before any surgical manipulation, we performed cylinder test (described below) in all animals to exclude potential asymmetric rats. Following this preliminary test, the animals were randomly separated into two main groups: ischemia saline (IS; craniotomy with induced ischemia followed by saline solution administration) and GUO ischemia (IG; craniotomy with induction of ischemia followed by GUO treatment). Of note, we previously showed that animals submitted only to surgical procedures (craniotomy) without thermocoagulation of pial vessels (SHAM) showed no behavioral impairment or brain histological damage [11, 12]. The IG group was subdivided according to the administration schedule: IG 0 h (immediately, 1, 3, and 6 h after surgery), IG 1 h (1, 3, and 6 h after surgery), or IG 3 h (3, 5, and 8 h after surgery). Saline or 30 mg/ml GUO solutions were IN administered (0.05 ml per nostril). The saline group received four administrations of saline solution (NaCl 0.9 %) immediately, 1, 3, and 6 h after surgery. For saline and/or GUO administration 3 to 8 h after the surgery, animals were anesthetized again with half of the initial anesthetic dose. The concentration of GUO solution for neuroprotective experiments was chosen based on the pharmacokinetics profile of IN administration. The administration schedule was initially chosen based on previous studies by our research group [11, 12]. After induction of ischemia, further analyses were performed by investigators blind to the treatments.
Induction of permanent focal ischemia
Ischemic injury was induced by thermocoagulation of pial blood vessels in the motor and sensorimotor cortices by approaching a hot probe to the meninges [11, 12]. This procedure resulted in the degeneration of the six cortical layers just below the affected blood vessels [32]. Briefly, the animals were anesthetized and placed in a stereotaxic apparatus. The skull was surgically exposed and a craniotomy was performed, exposing the left fronto-parietal cortex (+3–6 mm and AP + LL 2–0 mm bregma). After the procedure, the skin was sutured and the body temperature was maintained at 37 °C using a heating pad until recovery from anesthesia.
Measurement of sensorimotor activity
This procedure was based on the spontaneous exploratory behavior of rodents. It consisted of placing the animal into a glass cylinder (20 cm in diameter and 30 cm high) and counting the first 20 forelimb contacts with the cylinder walls. Occurrences of contact with exclusive use of the ipsilateral limb (to the injury) or contralateral limb or the use of both limbs were recorded separately. The animals were submitted to a pre-test prior to surgery and a post-test 48 h after surgery. The score of symmetry for each animal was calculated each day by the formula previously described [11, 12, 32].
Measurement of the volume of the brain infarcted area
After the cylinder procedure, the animals were euthanized and the brains were quickly removed from the skulls and sectioned in a coronal plane at 2 mm thickness using a rat brain matrix (Insight LTDA, Ribeirão Preto, SP, Brazil). The slices were immersed for 30 min in 2 % TTC at 37 °C followed by overnight fixation in 4 % paraformaldehyde. The infarct volume was calculated by the formula: volume = measurement of infarct area × slice thickness (2 mm). The brain slices were analyzed by the software Image J. The results are expressed in mm3.
Dysfunctional mitochondria measurement
Tissue samples (30 mg) from the side of the lesion of parietal cortex, located between the lesion and the cerebral longitudinal fissure (a piece measuring approximately 8 mm × 6.2 mm) was dissected after rat transcardial perfusion with saline in accordance with recent studies by our group [11, 12]. This region was chosen because it has characteristics similar to the penumbra area [11, 12, 32]; therefore, it was designated as the penumbra area. The samples were dissociated in 0.1 M phosphate-buffered solution (PBS), pH 7.4, containing 0.1 mg/ml of collagenase IV. After the dissociation, the samples were decanted for 15 min and an aliquot of supernatant was collected and incubated with MitoTrackerTM Green FM and Red FM dyes (100 nM each). MitotrackerTM green provides an estimation of mitochondrial quantity and mass, and red provides a measure of the mitochondrial potential. Taken together, these data (higher mitochondrial mass and lower potential) indicate mitochondria dysfunction [33]. The emission of fluorescence was measured by a band pass green (FL-1; 530 nm/30) and red (FL-3; 670 nm long pass) using CellQuest Pro software (Becton Dickinson, Franklin Lakes, NJ, USA) and data from 10,000 events were acquired. All flow cytometric analyses were performed using Flow Jo software 7.6.3 (Treestar, Ashland, OR).
Statistics
An unpaired Student’s t test was used to compare radioactivity measurements between IN and IP [3H] GUO groups. Purine levels evaluated by HPLC in brain structures, blood samples, and CSF were analyzed by a one-way ANOVA followed by Bonferroni’s post-test. Kruskal Wallis test followed by Dunn’s post-test was used to analyze the neuroprotective effects of different administration schedules of IN GUO treatment on sensorimotor activity and on brain infarct volume, comparing each different treatment protocol with IS. Dysfunctional mitochondrial cell data were analyzed by one-way ANOVA followed by a Bonferroni’s post-test. Post-test statistical powers were calculated after each analysis of neuroprotective effects and are shown in the Supplementary Material. Correlations were analyzed by a Pearson’s correlation analysis. Differences were considered significant at p ≤ 0.05 probability.
Results
Pharmacokinetic analysis following IN [3H] GUO solution administration
Radioactivity detection
Radioactivity was detected in all investigated brain structures (i.e., olfactory bulb, parietal cortex, hippocampus, and cerebellum) with the olfactory bulb presenting higher radioactivity levels (Fig. 1). The dose curve indicated that IN [3H] GUO exposure was increased in brain structures by increasing the GUO amount administered (Fig. 1a), pointing to a dose-dependent profile. Saturation was achieved with the dose of 30 mg/ml IN [3H] GUO solution. Regarding the time curve, no significant difference was observed in radioactivity content from 5 to 180 min after IN [3H] GUO solution administration (Fig. 1b).
Brain structures. a Dose curve of IN [3H] GUO administration. Radioactivity detected 15 min after administration of 0.05 ml per nostril. b Time curve. Radioactivity detected after administration of 30 mg/ml of IN [3H] GUO solution, 0.05 ml per nostril. Each point represents the mean ± SE. N = 6 animals per group
Similar to brain structures, the dose curve indicated a dose-dependent profile of [3H] GUO after IN [3H] GUO solution administration in blood plasma (Fig. 2a). In contrast to brain structures, no saturation level was reached even in the higher doses administered (Fig. 2a), and higher radioactivity levels were observed over time (Fig. 2b).
Blood plasma. a Dose curve of IN [3H] GUO administration. Radioactivity detected 15 min after administration of 0.05 ml per nostril. b Time curve. Radioactivity detected after administration of 30 mg/ml of IN [3H] GUO solution, 0.05 ml per nostril. Each point represents the mean ± SE. N = 6 animals per group. *P < 0.05 compared to the naïve group
HPLC measurements
No significant difference in GUO levels analyzed by HPLC was observed in any brain structure between naïve rats and rats that received IN [3H] GUO solution of each different tested conditions (concentration and time curves; Supplementary Tables 1 and 2). Only XAN and UA profiles showed statistically significant differences at specific conditions; a significant increase in XAN level in the olfactory bulb, 15 min after 7.5 mg/ml of IN [H3] GUO solution (Supplementary Table 1), and an increase in UA level in the parietal cortex, 60 min following 30 mg/ml of IN [H3] GUO solution administration (Supplementary Table 2).
We observed that only ADO plasma levels were significantly increased 15 min after animals received 15 to 60 mg/ml of IN [3H] GUO solution (Supplementary Table 3A). This selectivity of the increase in ADO levels was confirmed in the time curve (Supplementary Table 3B). A significant decrease in XAN levels was observed from 60 to 180 min following 30 mg/ml of IN [3H] GUO solution (Supplementary Table 3B). Blood plasma GUO and HYP levels were not possible to be detected due to its value not reaching the HPLC inferior detection limits (data not shown). This inability seems to be related specifically to the use of TFA 7 % in purines extraction protocol, as GUO plasma levels could be observed using different extraction compounds [7, 16, 25, 26]. Notably, we chose TFA 7 % based on a pilot experiment which we tested different chemicals to homogenize brain tissue and blood samples to obtain the highest radioactivity extraction derived from [3H] GUO (TCA 10 %, TFA 7 %, ACN, methanol, perchloric acid; data not shown).
Comparison between IN and IP [3H] GUO solution administration
Five minutes after administration of 30 mg/ml IP (0.1 ml) and IN (0.05 ml per nostril) [3H] GUO solution, the radioactivity was detected in brain structures (Fig. 3a). The radioactivity levels detected in the olfactory bulb were higher compared to other brain structures after IN but not IP administration. The radioactivity levels in the parietal cortex, hippocampus, and cerebellum were significantly higher after IP than IN administration.
Comparison of injection routes for [3H] GUO solution administration. The radioactivity in: a different brain structures and b the CSF and blood plasma, five minutes after IN (0.05 ml per nostril) or IP (0.1 ml) 30 mg/ml [3H] GUO administration. Data are expressed as the mean ± SE. N = 6 (brain structures and plasma) or 3–4 (CSF) animals per group. *P < 0.05 compared to IN groups
HPLC analyses confirmed no significant change in endogenous purine levels in brain structures after IN [3H] GUO solution administration, while IP [3H] GUO solution administration caused a small number of significant increases, i.e., UA in the olfactory bulb, INO in the hippocampus, and GUO and INO in the cerebellum (Supplementary Table 4).
CSF was collected from six animals of each naïve, IN, and IP GUO groups; however, only four, three, and three CSF samples were obtained without blood contamination, respectively. The radioactivity levels in the CSF were not significantly different between the two administrations (Fig. 3b), while in blood plasma it was significantly higher after IP than IN administration. In both protocols, the radioactivity levels in blood plasma were significantly higher than in the CSF. Significantly higher ADO levels were observed in blood plasma 5 min after IP, but not IN [3H] GUO solution injection compared to naïve rats. The concentrations of other analyzed purines showed no significant differences between the groups in blood plasma (Table 1). In contrast, IN [3H] GUO solution administration significantly increased the levels of GUO, XAN, UA, INO, and HYP in the CSF, especially GUO, INO, and HYP levels that were 2.5, 2.1, and 4.5 times compared to naïve animals. The concentrations of other analyzed purines in the CSF showed no significant differences between the groups (Table 1).
Evaluation of the neuroprotective potential of IN GUO administration
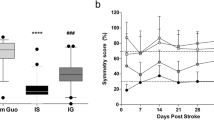
All animals presented a symmetry rate of approximately 90 % in the cylinder test before surgery (data not shown). Ischemic insult reduced the symmetry to approximately 25 %. IN GUO treatments improved the symmetry rate (Fig. 4, Supplementary Table 5).
Performance in the cylinder test 48 h after ischemia. Symmetry score of rats receiving IN treatment of saline (IS, N = 21) or GUO through a protocol starting immediately (IG 0 h, N = 16), 1 h (GUO 1 h, N = 9) or 3 h (GUO 3 h, N = 19) after ischemia induction. The symmetry score index and the schedule of administration for each treatment are described in material and methods. # P < 0.0001 compared to IS, IG 0 h, IG 1 h, IG 3 h groups; *P < 0.05 compared to IS group; **P < 0.001 compared to IS group. Data are expressed as the mean ± SE
Brain TTC staining indicated that permanent focal ischemia induced a lesion in the cerebral cortex of the left hemispher measured at 48 h after surgery (Fig. 5). IN GUO administration decreased the infarct volume only when the treatment started immediately after ischemia induction (IG 0 h; Fig. 5a-b, Supplementary Table 6). No statistical correlation between the symmetry score and the infarct volume was found (Pearson’s R 2 = 0.016, P = 0.41; Fig. 5c).
Parameters of brain infarct measured 48 h after cerebral ischemia. a Volume of brain infarct of rats receiving treatment with saline (IS, N = 14) or GUO starting immediately (GUO 0 h, N = 16), 1 h (GUO 1 h, N = 9) or 3 h (GUO 3 h, N = 12) following ischemia induction. b Representative images of brain TTC staining of experimental groups. c Correlation (IS and GUO 0H groups) between cortex infarct volume and forelimb function (symmetry score) measured 48 h after ischemia, Pearson’s R 2 = 0.016, P = 0.41. *P < 0.05 compared to IS group
We further evaluated functional mitochondrial integrity in cortical penumbra area of animals that received IN GUO treatment starting 3 h after ischemia onset since this experimental group presents a more interesting therapeutic time window compared to the others. The volume and morphological complexity analyses together with the Mitotracker™ incorporation (mass and potential mitochondrial measurement) through flow cytometry indicated that permanent focal ischemia induced injury to neural cells in the penumbra area of the parietal cortex of the ipsilateral, but not of the contralateral hemisphere. Notably, IN GUO treatment starting 3 h after ischemic insult (IG 3 h) significantly reduced mitochondrial dysfunction when compared to the IS group (Fig. 6a, Supplementary Table 7). We observed a statistical correlation between functional behavior recovery and mitochondrial dysfunction in the penumbra area (Pearson’s R 2 = 0.39, P = 0.006; Fig. 6b).
Dysfunctional mitochondria in the penumbra zone (contralateral and ipsilateral sides) measured 48 h after ischemia induction: a percentage of dysfunctional mitochondria in the penumbra area from rats of SHAM (N = 5 animals), IS (N = 7 animals), and IG 3 h (N = 7 animals). The description of each experimental group is detailed in material and methods. c Correlation between infarct volume and forelimb function (symmetry score; Pearson’s R 2 = 0.39, P = 0.006)
Histological analysis of the nasal septum was performed to verify the integrity of the mucosa after IN GUO treatment (IG 0 h group). No histological alteration was observed (Supplementary Figure 1).
Discussion
In the present work, we conducted pharmacokinetic evaluation of GUO IN administration to determine when, how, and where GUO could reach the brain. We observed a dose-dependent and saturable pattern of GUO exposure in brain structures. Although, to our knowledge, this was the first time that IN GUO administration was investigated, the delivery of nucleoside analogs to the CNS has been demonstrated by several works through IN administration in rodents [34, 35]. Indeed, nucleoside transporters were found in the nasal epithelia, pointing out that the uptake of GUO by their specific transporters can facilitate its delivery to the brain [36]. The pathway by which GUO applied to the nostril reaches the CNS seems to be reached as fast as only 5 min post-injection. This result is in accordance with other studies, which demonstrated that different drugs could reach maximal CNS concentrations immediately after administration [37, 38]. No significant difference was observed in GUO endogenous levels in the brain structures following IN [3H] GUO solution administration in any condition tested in this work. These results could be expected as GUO exposure on each brain structure was lower than the variability of total endogenous purines among naïve animals.
In blood plasma, IN [3H] GUO administration increased ADO levels 15 min after injection of 15–60 mg/ml IN GUO. Previously, we reported that chronic oral GUO treatment was also able to increase ADO plasma levels [7]. Some works in the literature have focused attention on the interplay of extracellular ADO and GUO levels. An experimentally based hypothesis is that GUO caused an increase in extracellular ADO levels by competing with nucleoside transporter [19, 20]. In fact, some of GUO’s neuroprotective effects, but not all, are ADO receptor dependent [18–22, 39].
Interestingly, radioactivity amounts were higher in brain structures following IP than IN [3H] GUO solution administration. As expected, significantly, more radioactivity amount was detected in the blood plasma after IP compared with IN [3H] GUO administration; however, the same levels of radioactivity were detected in CSF. Taken together, these data support the hypotheses that GUO reaches CSF after IN administration by a pathway, at least partially, not involving systemic circulation and that brain structures take up purines directly from blood after IP administration. CSF purines analysis indicated that GUO levels were significantly increased after IN [3H] GUO administration. Moreover, GUO direct metabolites, i.e., XAN and UA, as well as INO and HYP, which concentrations can be influenced by GUO, are also significantly increased after IN [3H] GUO administration, demonstrating a fast delivery pathway to the CNS. CSF GUO levels increased after IP [3H] GUO administration but did not reach a statistically significant difference. Except for ADO, no purine levels showed a significant difference compared to endogenous levels in CSF after IP [3H] GUO administration. The increase of CSF ADO levels may be associated with the increased blood plasma ADO levels after IP [3H] GUO injection. Together, these data reinforced the idea that the CSF may be a major source of distribution to the brain following IN administration while the purine levels after IP administration reflect blood levels. This hypothesis is reinforced by works of Jiang’s group [19, 20] that showed, using a mixture of unlabeled and labeled [3H] GUO (40 times more [3H] GUO than was used here), that GUO is promptly and markedly metabolic breakdown after systemic administration reflecting in an increase of GUO metabolites in the brain [25, 26].
As we demonstrated that an IN route can be an efficient method for the delivery of GUO to the CNS, we further evaluated the IN GUO treatment neuroprotective potential in a brain ischemia model. Stroke, which mainly causes ischemic events, is the third cause of death worldwide and the main cause of chronic, severe adult disability. The current therapy can restore cerebral blood flow within a narrow time window to prevent damage to the “penumbra” area, which surrounds the infarct core [40]. In order to increase the therapeutic time window, neuroprotection is an alternative or adjunct approach to thrombolysis, targeting the cerebral parenchyma in the acute ischemic phase [41].
The neuroprotective effects of the nucleoside GUO have been demonstrated after systemic administration in ischemia models by our and other groups [11–15]. We recently showed, using the same permanent focal cerebral ischemia model used in the present work, that systemic GUO treatment started immediately after ischemia induction improved functional recovery of behavioral impairment, simultaneously preventing brain oxidative stress, modulating glutamatergic parameters, attenuating changes in the inflammatory system, thus decreasing neuronal degeneration in the penumbra area [11, 12]. Additionally, other groups demonstrated that GUO treatment starting before a transient focal cerebral ischemia induction (middle cerebral arteria occlusion model [MCAO]) decreased brain infarct volume and improved neurological deficits, acting directly in the CNS [13, 15].
The main goal of the present work was to explore the neuroprotective potential of GUO through an alternative administration route, i.e., the IN pathway. In addition to being a non-invasive method, the advantage of the IN route is to be a direct pathway for endogenous drugs to be delivered to the CNS, decreasing the influence of systemic metabolism and the blood brain barrier, as we observed for GUO in our pharmacokinetics data. Moreover, the IN route presents alternative pathways to deliver drugs to the CNS that does not involve blood vessels, which are compromised in stroke [27, 28]. Remarkably, IN GUO treatment that was initiated immediately after ischemia onset prevented behavior impairment and decreased brain infarct volume with a dose almost seven times lower than the effective dose for IP administration [11, 12]. This effective result of IN compared to systemic administration was also observed for other neuroprotective drugs against ischemia damage [29, 30] .
Although the exact GUO mechanism of action is still not fully clear, GUO seems to counteract different steps following the ischemia cascade events [11, 12]. Thus, we tested different therapeutic schedules of treatment, increasing the time of the first dose administered after ischemia induction. We observed that IN GUO treatment starting 1 or 3 h after ischemia induction were efficient in preventing functional behavior impairment induced by ischemia but had no effect on brain infarct volume, evaluated by the TTC technique. Interestingly, no statistical correlation between these two parameters was observed. In this way, it is important to consider that TTC methodology relies on the degree of dehydrogenase enzymes and cofactors functionality, but the tissue that stains positively is not necessarily health. Together, these results suggest that GUO may be acting in a different damaged region. The area between the pale-ischemic core and the red-colored healthy tissue represents the penumbra zone where brain tissue is damaged but not yet dead, thus comprising the transition zone between the core and the repairable zone that is the anatomical target of protective intervention [42, 43]. In agreement with the idea of neuroprotection action in the penumbra zone, we observed that IN GUO treatment starting 3 h after the insult statistically decreased the number of events containing dysfunctional mitochondria in the penumbra area. To reinforce this idea, we detected a statistical correlation between the mitochondrial status in the penumbra area and the behavioral performance. Our data are in agreement with our previous work, which reported a correlation between oxidative stress parameters in the penumbra area (but not infarct volume) and functional recovery of animals submitted to ischemia treated with systemic GUO [12]. However, the wide time window for therapy with GUO seems to be an outstanding outcome particular to the IN route, as systemic GUO injection was efficient only when administered before or immediately after ischemia onset [11–15].
In summary, we showed in the present work that the IN route is an efficient route to promptly deliver the neuroprotective nucleoside GUO to the CNS. Moreover, we demonstrated that IN GUO prevented behavioral injury in a much lower dose and a wider therapeutic time window compared to systemic administration, an effect related to improvement in tissue viability in the penumbra area. As the search for an effective neuroprotective treatment that can be started later after ischemia onset is currently one of the most challenging goals to treat stroke, we believe that our present data support that IN GUO may be a promise strategy to treat stroke. We expect that our present results will stimulate other groups to explore the neuroprotective potential of IN GUO treatment.
References
Schmidt AP, Lara DR, Souza DO (2007) Proposal of a guanine-based purinergic system in the mammalian central nervous system. Pharmacol Ther 116(3):401–416. doi:10.1016/j.pharmthera.2007.07.004
Frizzo ME, Antunes Soares FA, Dall’Onder LP, Lara DR, Swanson RA, Souza DO (2003) Extracellular conversion of guanine-based purines to guanosine specifically enhances astrocyte glutamate uptake. Brain Res 972(1-2):84–89
Frizzo ME, Lara DR, Dahm KC, Prokopiuk AS, Swanson RA, Souza DO (2001) Activation of glutamate uptake by guanosine in primary astrocyte cultures. Neuroreport 12(4):879–881
Tasca CI, Santos TG, Tavares RG, Battastini AM, Rocha JB, Souza DO (2004) Guanine derivatives modulate L-glutamate uptake into rat brain synaptic vesicles. Neurochem Int 44(6):423–431
Lai TW, Zhang S, Wang YT (2014) Excitotoxicity and stroke: identifying novel targets for neuroprotection. Prog Neurobiol 115:157–188. doi:10.1016/j.pneurobio.2013.11.006
Lipton SA (2007) Pathologically activated therapeutics for neuroprotection. Nat Rev Neurosci 8(10):803–808. doi:10.1038/nrn2229
Ganzella M, de Oliveira ED, Comassetto DD, Cechetti F, Cereser VH Jr, Moreira JD, Hansel G, Almeida RF, Ramos DB, Figueredo YN, Souza DG, Oses JP, Worm PV, Achaval M, Netto CA, Souza DO (2012) Effects of chronic guanosine treatment on hippocampal damage and cognitive impairment of rats submitted to chronic cerebral hypoperfusion. Neurol Sci 33(5):985–997. doi:10.1007/s10072-011-0872-1
Schmidt AP, Avila TT, Souza DO (2005) Intracerebroventricular guanine-based purines protect against seizures induced by quinolinic acid in mice. Neurochem Res 30(1):69–73
Lara DR, Schmidt AP, Frizzo ME, Burgos JS, Ramirez G, Souza DO (2001) Effect of orally administered guanosine on seizures and death induced by glutamatergic agents. Brain Res 912(2):176–180
Schmidt AP, Paniz L, Schallenberger C, Bohmer AE, Wofchuk ST, Elisabetsky E, Portela LV, Souza DO (2010) Guanosine prevents thermal hyperalgesia in a rat model of peripheral mononeuropathy. Journal Pain 11(2):131–141. doi:10.1016/j.jpain.2009.06.010
Hansel G, Tonon AC, Guella FL, Pettenuzzo LF, Duarte T, Duarte MM, Oses JP, Achaval M, Souza DO (2014) Guanosine Protects Against Cortical Focal Ischemia. Involvement of Inflammatory Response. Mol Neurobiol. doi:10.1007/s12035-014-8978-0
Hansel G, Ramos DB, Delgado CA, Souza DG, Almeida RF, Portela LV, Quincozes-Santos A, Souza DO (2014) The potential therapeutic effect of guanosine after cortical focal ischemia in rats. PLoS One 9(2), e90693. doi:10.1371/journal.pone.0090693
Connell BJ, Di Iorio P, Sayeed I, Ballerini P, Saleh MC, Giuliani P, Saleh TM, Rathbone MP, Su C, Jiang S (2013) Guanosine protects against reperfusion injury in rat brains after ischemic stroke. J Neurosci Res 91(2):262–272. doi:10.1002/jnr.23156
Rathbone MP, Saleh TM, Connell BJ, Chang R, Su C, Worley B, Kim M, Jiang S (2011) Systemic administration of guanosine promotes functional and histological improvement following an ischemic stroke in rats. Brain Res 1407:79–89. doi:10.1016/j.brainres.2011.06.027
Chang R, Algird A, Bau C, Rathbone MP, Jiang S (2008) Neuroprotective effects of guanosine on stroke models in vitro and in vivo. Neurosci Lett 431(2):101–105. doi:10.1016/j.neulet.2007.11.072
Paniz LG, Calcagnotto ME, Pandolfo P, Machado DG, Santos GF, Hansel G, Almeida RF, Bruch RS, Brum LM, Torres FV, de Assis AM, Rico EP, Souza DO (2014) Neuroprotective effects of guanosine administration on behavioral, brain activity, neurochemical and redox parameters in a rat model of chronic hepatic encephalopathy. Metab Brain Dis 29(3):645–654. doi:10.1007/s11011-014-9548-x
Traversa U, Bombi G, Di Iorio P, Ciccarelli R, Werstiuk ES, Rathbone MP (2002) Specific [(3)H]-guanosine binding sites in rat brain membranes. Br J Pharmacol 135(4):969–976. doi:10.1038/sj.bjp.0704542
Dal-Cim T, Ludka FK, Martins WC, Reginato C, Parada E, Egea J, Lopez MG, Tasca CI (2013) Guanosine controls inflammatory pathways to afford neuroprotection of hippocampal slices under oxygen and glucose deprivation conditions. J Neurochem 126(4):437–450. doi:10.1111/jnc.12324
Jackson EK, Cheng D, Jackson TC, Verrier JD, Gillespie DG (2013) Extracellular guanosine regulates extracellular adenosine levels. Am J Physiol Cell Physiol 304(5):C406–C421. doi:10.1152/ajpcell.00212.2012
Jackson EK, Mi Z (2014) The guanosine-adenosine interaction exists in vivo. J Pharmacol Exp Ther 350(3):719–726. doi:10.1124/jpet.114.216978
Dal-Cim T, Molz S, Egea J, Parada E, Romero A, Budni J, Martin de Saavedra MD, del Barrio L, Tasca CI, Lopez MG (2012) Guanosine protects human neuroblastoma SH-SY5Y cells against mitochondrial oxidative stress by inducing heme oxigenase-1 via PI3K/Akt/GSK-3beta pathway. Neurochem Int 61(3):397–404. doi:10.1016/j.neuint.2012.05.021
Di Iorio P, Kleywegt S, Ciccarelli R, Traversa U, Andrew CM, Crocker CE, Werstiuk ES, Rathbone MP (2002) Mechanisms of apoptosis induced by purine nucleosides in astrocytes. Glia 38(3):179–190. doi:10.1002/glia.10055
Ipata PL, Camici M, Micheli V, Tozz MG (2011) Metabolic network of nucleosides in the brain. Curr Top Med Chem 11(8):909–922
Micheli V, Camici M, Tozzi MG, Ipata PL, Sestini S, Bertelli M, Pompucci G (2011) Neurological disorders of purine and pyrimidine metabolism. Curr Top Med Chem 11(8):923–947
Giuliani P, Ballerini P, Ciccarelli R, Buccella S, Romano S, D’Alimonte I, Poli A, Beraudi A, Pena E, Jiang S, Rathbone MP, Caciagli F, Di Iorio P (2012) Tissue distribution and metabolism of guanosine in rats following intraperitoneal injection. J Biol Regul Homeost Agents 26(1):51–65
Jiang S, Fischione G, Giuliani P, Romano S, Caciagli F, Di Iorio P (2008) Metabolism and distribution of guanosine given intraperitoneally: implications for spinal cord injury. Nucleosides Nucleotides Nucleic Acids 27(6):673–680. doi:10.1080/15257770802143962
Djupesland PG, Messina JC, Mahmoud RA (2014) The nasal approach to delivering treatment for brain diseases: an anatomic, physiologic, and delivery technology overview. Ther Deliv 5(6):709–733. doi:10.4155/tde.14.41
Lochhead JJ, Thorne RG (2012) Intranasal delivery of biologics to the central nervous system. Adv Drug Deliv Rev 64(7):614–628. doi:10.1016/j.addr.2011.11.002
Yu YP, Xu QQ, Zhang Q, Zhang WP, Zhang LH, Wei EQ (2005) Intranasal recombinant human erythropoietin protects rats against focal cerebral ischemia. Neurosci Lett 387(1):5–10. doi:10.1016/j.neulet.2005.07.008
Fletcher L, Kohli S, Sprague SM, Scranton RA, Lipton SA, Parra A, Jimenez DF, Digicaylioglu M (2009) Intranasal delivery of erythropoietin plus insulin-like growth factor-I for acute neuroprotection in stroke. Laboratory investigation. J Neurosurg 111(1):164–170. doi:10.3171/2009.2.JNS081199
Lee M, Bikram M, Oh S, Bull DA, Kim SW (2004) Sp1-dependent regulation of the RTP801 promoter and its application to hypoxia-inducible VEGF plasmid for ischemic disease. Pharm Res 21(5):736–741
de Vasconcelos Dos Santos A, da Costa RJ, Diaz Paredes B, Moraes L, Jasmin G-GA, Mendez-Otero R (2010) Therapeutic window for treatment of cortical ischemia with bone marrow-derived cells in rats. Brain Res 1306:149–158. doi:10.1016/j.brainres.2009.09.094
Tal MC, Sasai M, Lee HK, Yordy B, Shadel GS, Iwasaki A (2009) Absence of autophagy results in reactive oxygen species-dependent amplification of RLR signaling. Proc Natl Acad Sci U S A 106(8):2770–2775. doi:10.1073/pnas.0807694106
Chavanpatil MD, Vavia PR (2004) The influence of absorption enhancers on nasal absorption of acyclovir. Eur J Pharm Biopharm 57(3):483–487. doi:10.1016/j.ejpb.2004.01.001
Yang Z, Huang Y, Gan G, Sawchuk RJ (2005) Microdialysis evaluation of the brain distribution of stavudine following intranasal and intravenous administration to rats. J Pharm Sci 94(7):1577–1588. doi:10.1002/jps.20334
Genter MB, Krishan M, Augustine LM, Cherrington NJ (2010) Drug transporter expression and localization in rat nasal respiratory and olfactory mucosa and olfactory bulb. Drug Metab Dispos 38(10):1644–1647. doi:10.1124/dmd.110.034611
Falcone JA, Salameh TS, Yi X, Cordy BJ, Mortell WG, Kabanov AV, Banks WA (2014) Intranasal administration as a route for drug delivery to the brain: evidence for a unique pathway for albumin. J Pharmacol Exp Ther 351(1):54–60. doi:10.1124/jpet.114.216705
Dhuria SV, Hanson LR, Frey WH 2nd (2009) Intranasal drug targeting of hypocretin-1 (orexin-A) to the central nervous system. J Pharm Sci 98(7):2501–2515. doi:10.1002/jps.21604
Schmidt AP, Bohmer AE, Schallenberger C, Antunes C, Tavares RG, Wofchuk ST, Elisabetsky E, Souza DO (2010) Mechanisms involved in the antinociception induced by systemic administration of guanosine in mice. Br J Pharmacol 159(6):1247–1263. doi:10.1111/j.1476-5381.2009.00597.x
Balami JS, Hadley G, Sutherland BA, Karbalai H, Buchan AM (2013) The exact science of stroke thrombolysis and the quiet art of patient selection. Brain 136(Pt 12):3528–3553. doi:10.1093/brain/awt201
Moretti A, Ferrari F, Villa RF (2015) Neuroprotection for ischaemic stroke: current status and challenges. Pharmacol Ther 146:23–34. doi:10.1016/j.pharmthera.2014.09.003
Kramer M, Dang J, Baertling F, Denecke B, Clarner T, Kirsch C, Beyer C, Kipp M (2010) TTC staining of damaged brain areas after MCA occlusion in the rat does not constrict quantitative gene and protein analyses. J Neurosci Methods 187(1):84–89. doi:10.1016/j.jneumeth.2009.12.020
Lo EH (2008) A new penumbra: transitioning from injury into repair after stroke. Nat Med 14(5):497–500. doi:10.1038/nm1735
Acknowledgments
This work was supported by the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES), Fundação de Amparo à Pesquisa do Estado do Rio Grande do Sul (FAPERGS), Financiadora de Estudos e Projetos (FINEP) - IBN.Net 01.06.0842-00, and Instituto Nacional de Ciência e Tecnologia para Excitotoxicidade e Neuroproteção (INCTEN).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Authors’ contributions
Author contributions: D.B.R., G.C.M., S.O.L., D.O.S., and M.G. designed research; D.B.R., G.C.M., G.B.M.R., G.H.D., R.F.A., L.F.P., G.H., A.C.M.H., S.O.L., and M.G. performed research; L.F.P., A.C.M.H., D.O.S. and M.G. contributed new reagents/analytic tools; D.B.R., G.C.M., G.B.M.R., R.F.A., L.F.P., G.H., A.C.M.H., S.O.L., D.O.S., and M.G. analyzed data; and D.B.R., G.C.M., S.O.L., D.O.S., and M.G. wrote the paper.
Additional information
Denise Barbosa Ramos and Gabriel Cardozo Muller contributed equally as first authors.
Rights and permissions
About this article
Cite this article
Ramos, D.B., Muller, G.C., Rocha, G.B.M. et al. Intranasal guanosine administration presents a wide therapeutic time window to reduce brain damage induced by permanent ischemia in rats. Purinergic Signalling 12, 149–159 (2016). https://doi.org/10.1007/s11302-015-9489-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-015-9489-9