Abstract
Purpose
Anti-neutrophil cytoplasmic autoantibody-associated vasculitis (AAV) is predominantly a disease of the elderly, and the incidence increases with age. However, there are few data focusing on the clinical features in elderly onset AAV, especially in very elderly onset AAV in China. The aim of this study was to explore whether elderly onset AAV shows any specific clinical features and outcomes in Chinese patients.
Methods
We performed a retrospective study in Xiangya Hospital, a mixed tertiary medical center in south China. A total of 177 patients presenting with AAV were included between January 1, 2010 and December 31, 2017. Patients were divided into younger group (age < 65 years) and older group (age ≥ 65 years) which was sub-divided into elderly group (age 65–74 years) and very elderly group (age ≥ 75 years). And their medical records were analyzed by retrospective review.
Results
We found patients in the very elderly group had more chest and cardiovascular involvement (P = 0.033 and P = 0.017). Older AAV patients had less renal involvement and lower serum C4 level (P = 0.013 and P = 0.003). Very elderly AAV patients had lower platelet counts. Patients in the younger group had a higher level of BVAS among three groups (P < 0.05 younger group vs. very elderly group; P < 0.05 younger group vs. elderly group). There were no significant difference in the proportion of ESRD patients among the three groups (P = 0.473). Patients in the very elderly group had the poorest patient survival (P = 0.002).
Conclusion
Older AAV patients had less renal involvement, lower serum C4 level and BVAS. The very elderly group got the most chest and cardiovascular involvement and had lower platelet counts. Older age is associated with higher mortality in AAV patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Anti-neutrophil cytoplasmic antibody (ANCA)-associated vasculitis (AAV) is an autoimmune disease that mainly affects small vessel polyangiitis. It is the most common type of rapidly progressive glomerulonephritis [1], which might progress to Chronic kidney disease (CKD), even to end-stage renal disease (ESRD) or death, and carries huge financial burden on health care systems [2, 3]. AAV can be divided into three major categories, including granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA) [4]. MPA was the dominant form of AAV in China [5], which is in contrast with many Caucasian populations. AAV occurs at any age but usually occurs to adults, and the incidence increases with age [6]. The prognosis of AAV has dramatically improved with the introduction of effective immunosuppressive treatment. However, there is a dilemma exists in clinical practice concerning how to control active disease of elderly patients with AAV effectively with fewer adverse events. On one hand, increasing age is associated with poor outcomes in AAV patients [7]. Previous reports have demonstrated that the proportion of elderly patients is increasing and elderly patients are more likely to develop complications of treatment and have a higher mortality rate than younger patients [8, 9]. On the other hand, several studies suggested that elderly patients with immunosuppressive treatment were equally likely to respond as younger patients and showed improved survival when compared with untreated patients [10].
To elucidate this issue, we retrospectively compared the demographic factors, laboratory data, pathological characteristics and outcomes in younger and older patients with AAV at a tertiary medical center in China.
Methods
Patients
Patients were recruited from the departments of nephrology, rheumatology and immunology, and respiratory, Xiangya Hospital, a mixed tertiary hospital. All patients newly diagnosed with AAV between January 1, 2010 and December 31, 2017 were recruited.
Inclusion criteria
A definite clinical diagnosis of GPA or MPA according to the European Medicines Agency algorithm was required during the study period [11]. The diagnosis was retrieved in the original medical records and confirmed by two independent investigators. All patients met the criteria of Chapel Hill Consensus Conferences Nomenclature of Vasculitis proposed in 2012 [4].
Exclusion criteria
Patients with secondary vasculitis were excluded. All EGPA were excluded because they were not usually referred to Xiangya Hospital and thus, their incidence would be underestimated. Those patients whose were positive for serum circulating anti-GBM antibodies were also excluded [11].
Definitions and groups
We defined younger adults as the patients aged < 65 years, older adults as those aged ≥ 65 years. And older group was sub-divided into elderly group (age 65–74 years) and very elderly group (age ≥ 75 years). Organ system involvement was considered only if the manifestations were due to AAV [12].
Data collection
All data were collected retrospectively from the medical records. One of our investigators contacted each patient or their families were via phone to determine their status by December 2018. The following characteristics were collected at presentation: each patient’s age, gender, symptoms and signs, time interval from first symptoms to date of diagnosis, laboratory data. The activity of disease was measured by Birmingham Vasculitis Activity Score (BVAS) [12].
Detection of ANCA
Indirect immunofluorescence (IIF) was used to test cytoplasmic ANCA (c-ANCA) and perinuclear ANCA (p-ANCA) were tested. ANCA against proteinase 3 (PR3-ANCA) and myeloperoxidase (MPO-ANCA) were tested using antigen-specific ELISA. Standard ELISA (Inova Diagnostics, San Diego, USA) and IIF assay (Euroimmun, Lübeck, Germany) were carried out according to the manufacturer’s instructions.
Renal histology
For light microscopy, renal biopsies were fixed and embedded in paraffin. Paraffin sections were stained with hematoxylin and eosin, periodic acid-schiff, Masson trichrome and methenamine silver. Direct immune fluorescence was used to test immunoglobulins and complement components. Electron microscopy were also performed for each sample. Two renal pathologists scored the renal specimens independently according to the classification system of ANCA-associated glomerulonephritis proposed by Berden et al. for glomerular lesions [13], and Chen et al. for tubulointerstitial lesions [14]. In brief, each glomerulus was scored separately. The presence of glomerular lesions was calculated as the percentage of the total number of glomeruli in a biopsy: ≥ 50% normal glomeruli for focal class, ≥ 50% glomeruli with cellular crescents for crescentic class, ≥ 50% globally sclerotic glomeruli for sclerotic class and the left for mixed class. Interstitial and tubular lesions were semi quantitatively scored on the basis of the percentage of interstitial fibrosis and tubular atrophy: score 0 for absent, 1 for 1–20%, 2 for 21–50%, and 3 for > 50%.
Treatment
All patients were treated with induction therapy and maintenance therapy described previously [15, 16]. Induction therapy included standard dose oral glucocorticoids (prednisolone, starting at a dosage of 1 mg/kg daily for 4–6 weeks, tapered over a period of 3–6 months to 12.5–15 mg) and cyclophosphamide (CTX) that was administered by intravenous 0.5–1.0 g/m2 every month. For those over 65 years old or those with renal insufficiency, twenty-five percent dose reduction of CTX was made. CTX was temporarily stopped for those who developed leukocytopenia or thrombocytopenia. Some patients with severe kidney injury or pulmonary hemorrhage received intravenous pulse methylprednisolone (5–10 mg/kg/day) for 3 days before the standard induction therapy, and some of these patients received plasma exchanges additionally. After the 3–6 months’ induction, patients were converted to azathioprine (AZA) or mycophenolate mofetil or intravenous CTX every 3 months for maintenance therapy. And a low-dose oral prednisolone was continued.
Ethical issues
The protocol was approved by the Ethic Committee of Xiangya Hospital. Informed consent was obtained from all participants included in the study.
Statistical analysis
All data were analyzed using the statistical software Graphpad Prism, version 7. Baseline characteristics are presented as means and standard deviations (SDs) or median with interquartile range for continuous variables and percentages for categorical variables. The Fisher’s exact test for categorical data and one-way analysis of variance or the Mann–Whitney test for numerical data were used to examine for differences between groups. Kaplan–Meier curves and log-rank tests were used to analyze patient survival and renal survival. P values < 0.05 were considered significant.
Results
General characteristics
A total of 177 patients were included in the study. The demographic and clinical characteristics of the patients are shown in Table 1. There were 93 patients < 65 years old and 84 patients ≥ 65 years old. And 25 of the 84 older patients were in the very elderly group. One hundred and fifty-nine patients were classified as MPA, and 18 patients as GPA, MPO/p-ANCA positivity was seen in 89% and PR3/c-ANCA positivity in 11%. The gender of patients and classification of vasculitis were equally distributed among the three groups. The median course of disease of overall patients was 64 days, and there was no difference among the three groups.
Patients in the very elderly group had chest and cardiovascular involvement significantly more often compare to the other two groups (P = 0.033 and P = 0.017). The younger group seemed to have more renal involvement among three groups (P = 0.027). The elderly group got the most neurological involvement (P = 0.046). A similar frequency of general, cutaneous, mucous, ENT and abdominal involvement was found in all three groups. In addition, patients in the younger group had a higher level of BVAS among three groups (P < 0.05 younger group vs. very elderly group; P < 0.05 younger group vs. elderly group). The most common comorbidities of patients were hypertension, heart disease, lung disease and diabetes. And the very elderly group got the most often heart disease, the elderly had the most lung disease. (Supplemental Table 1).
Laboratory data showed significantly lower platelet counts in the very elderly AAV patients (P < 0.05 very elderly group vs younger group; P < 0.05 very elderly group vs. elderly group). The younger AAV patients had the highest C4 level (P < 0.05 younger group vs. very elderly group; P < 0.05 younger group vs. elderly group). There was no significant difference in other laboratory tests among the groups, including p-ANCA/c-ANCA positivity.
Renal biopsy
Renal biopsies were performed in 62 patients (35%) (9 in elderly group and 53 in younger group) and none of the patients from the very elderly group performed this operation. The pathological characteristics of renal biopsies were shown in Table 2.
According to Berden et al. classification system of ANCA-associated glomerulonephritis, for elderly patients, 4 (44%) were sclerotic class, 2 (22%) were crescentic class, 3 (33%) were mixed class, and none were focal class. For younger patients, the sclerotic class, crescentic class, focal class and mixed class were 8 (15%), 5 (9%), 20 (38%) and 20 (38%), respectively. According to Chen et al. tubulointerstitial lesions classification, all patients who performed renal biopsies present with tubulointerstitial injury. The tubulointerstitial injury score range from 1 to 3 were 5 (56%) vs 30 (57%), 3 (33%) vs 17 (32%) and 1 (11%) vs 6 (11%) in elderly and younger group. There was no difference in glomerular lesions and tubulointerstitial injury between elderly and younger patients.
Survival
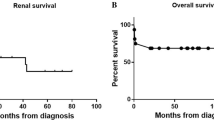
Overall, a total of 16 patients were lost during follow-up. At the end of the observation period, 48% (12 out of 25 patients) of the very elderly patients, 25% (15 out of 59 patients) of the elderly patients and 18% (17 out of 93 patients) of the younger patients died.
The patient survival of the patients is shown in Fig. 1. Patients in the younger group had superior patient survival, whereas patients in the very elderly group had the poorest patient survival (P = 0.002). Regarding kidney survival, no significant difference was found among the three groups (Fig. 2).
Discussion
In this retrospective cohort, we described and compared the clinical characteristics and survival of young and old patients with AAV. The ratio of MPA to GPA was 9:1 in this study. MPO-ANCA/p-ANCA positivity was seen in 81% AAV patients. Chen et al. reported that MPA was striking preponderance in China, constituting about 80% of the patients with AAV [17]. The constitution of AAV in our cohort is in line with their report.
We found that older AAV patients had similar clinical features compared with younger AAV patients, but showed an increased frequency of chest and cardiovascular and neurological involvement, and had lower BVAS. It is worth mentioning that there was no difference in serum MPO/p-ANCA or PR3/c-ANCA between older and younger patients, which was inconsistent with the results of the previous study [8, 18]. The discrepancy might be mainly due to that MPA is more prevalent in both younger and older patients in our cohort.
A major finding of our study is that age is a strong predictor of death in AAV. Kaplan–Meier analyses showed significantly lower overall survival rates in the older AAV patients. The very elderly AAV patient had the highest mortality, with nearly 48% patient dead. This data is consistent with that obtained by other investigators [7]. There are some possible explanations for this phenomenon. First, we found chest and cardiovascular involvement increases with age in AAV patients and it might contribute to the high mortality in elderly onset AAV. Second, in line with previous reports [18, 19], the strength of immunosuppressive therapy was weaker in older patients than that in younger patients. When came to comorbidities, the very elderly group got the most often heart disease, the elderly had the most lung disease. However, multivariable cox regression model analysis demonstrated that these comorbidities were not independent risk factors of patients’ mortality.
What’s more, in our study, laboratory data showed significantly lower platelet counts in very elderly AAV patients. That might be one possible reason for the poor outcome of this group. Xu et al. reported that increased platelet count is associated with active and reversible renal lesions in MPO-ANCA AAV and higher renal recovery rate [20]. Our finding that the very elderly group who had the lowest platelet counts got the poorest survival is in accordance with their report.
When come to complement system, it is recognized to play a prominent role in the pathogenesis of glomerular diseases [21, 22], Recent cumulative evidence implicates that the activation of the complement system is important for the development of AAV [23]. Low serum complement C3 level is associated with severe AAV and can predict poor renal outcome at diagnosis [24, 25]. However, in our study, we found that serum C4 levels but not C3 was higher in the younger AAV patients. When use multivariable cox regression model to further analyze these variables, we found that C4 levels were not associated with patient survival. This result was interesting and the relationship between C4 and AAV required further investigation.
In this study, we found no difference in renal histology between elder group and younger group. However, only 35% patient had renal biopsy results, and the number of renal biopsy patients in the elderly group was extremely small. And none of those very elderly patients who aged over 75 performed renal biopsy. Thus, sampling bias could not be excluded.
Previous studies suggested that older AAV patients have more severe renal involvement and poorer renal outcomes [8, 18, 26]. It should be noted that in contrast to the previous study, no significantly difference was found in the proportion of AAV patients that progression into ESRD among three groups. The reason for this discrepancy is unclear, which may partly relate to the high mortality of the older AAV patients for some older patients died before they progressed into ESRD.
When use multivariable cox regression model to further analyze these variables, we found that platelet counts, chest and cardiovascular involvement were independently associated with a higher risk of mortality (see Supplemental Table 2).
There are several limitations in our study such as the retrospective design itself. On the other hand, due to the restrictions of single cohort, the sample size of the study was small. Furthermore, as mentioned above, only about 35% patients performed renal biopsy, which might lead to some bias. Lastly, selection biases based on the basis of the disease severity couldn’t be avoided since treatment were not protocol-driven for the limitation of retrospective design itself. And we cannot exclude the possibility completely that different treatment may have had minor variable effects on the various outcomes evaluated in our study.
Conclusion
This study documents the characteristic of older patients with AAV and outcome. The very elderly group had lower platelet counts and got the most chest and cardiovascular involvement. Older AAV patients had less renal involvement, lower serum C4 level and BVAS. Older age is associated with higher mortality in AAV patients.
Availability of data and material
Not applicable.
References
Wu T, Peng J, Meng T, Liu Q, Ao X, Lin W, Yin H, Chen J, Pu J, Peng Z, Peng W, Li X, Xiao X, Zhou Q, Zhong Y, Xiao P (2019) Clinicopathological features and prognostic analysis of 49 cases with crescentic glomerulonephritis. Exp Ther Med 18:3984–3990
Peng Z, Wang J, Yuan Q, Xiao X, Xu H, Xie Y, Wang W, Huang L, Zhong Y, Ao X, Zhang L, Zhao M, Tao L, Zhou Q, CSs group (2017) Clinical features and CKD-related quality of life in patients with CKD G3a and CKD G3b in China: results from the Chinese Cohort Study of Chronic Kidney Disease (C-STRIDE). BMC Nephrol 18:311
Yuan Q, Wang J, Peng Z, Zhou Q, Xiao X, Xie Y, Wang W, Huang L, Tang W, Sun D, Zhang L, Wang F, Zhao MH, Tao L, He K, Xu H, CSs group (2019) Neutrophil-to-lymphocyte ratio and incident end-stage renal disease in Chinese patients with chronic kidney disease: results from the Chinese Cohort Study of Chronic Kidney Disease (C-STRIDE). J Transl Med 17:86
Jennette JC, Falk RJ, Bacon PA, Basu N, Cid MC, Ferrario F, Flores-Suarez LF, Gross WL, Guillevin L, Hagen EC, Hoffman GS, Jayne DR, Kallenberg CG, Lamprecht P, Langford CA, Luqmani RA, Mahr AD, Matteson EL, Merkel PA, Ozen S, Pusey CD, Rasmussen N, Rees AJ, Scott DG, Specks U, Stone JH, Takahashi K, Watts RA (2013) 2012 revised international Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum 65:1–11
Li ZY, Ma TT, Chen M, Zhao MH (2016) The prevalence and management of anti-neutrophil cytoplasmic antibody-associated vasculitis in China. Kidney Dis (Basel) 1:216–223
Hamour SM, Salama AD (2011) ANCA comes of age-but with caveats. Kidney Int 79:699–701
Flossmann O, Berden A, de Groot K, Hagen C, Harper L, Heijl C, Hoglund P, Jayne D, Luqmani R, Mahr A, Mukhtyar C, Pusey C, Rasmussen N, Stegeman C, Walsh M, Westman K, G. European Vasculitis Study (2011) Long-term patient survival in ANCA-associated vasculitis. Ann Rheum Dis 70:488–494
Harper L, Savage CO (2005) ANCA-associated renal vasculitis at the end of the twentieth century—a disease of older patients. Rheumatology (Oxford) 44:495–501
Ntatsaki E, Watts RA, Scott DG (2010) Epidemiology of ANCA-associated vasculitis. Rheum Dis Clin N Am 36:447–461
McGovern D, Williams SP, Parsons K, Farrah TE, Gallacher PJ, Miller-Hodges E, Kluth DC, Hunter RW, Dhaun N (2019) Long-term outcomes in elderly patients with ANCA-associated vasculitis. Rheumatology 59:1076–1083
Watts R, Lane S, Hanslik T, Hauser T, Hellmich B, Koldingsnes W, Mahr A, Segelmark M, Cohen-Tervaert JW, Scott D (2007) Development and validation of a consensus methodology for the classification of the ANCA-associated vasculitides and polyarteritis nodosa for epidemiological studies. Ann Rheum Dis 66:222–227
Mukhtyar C, Lee R, Brown D, Carruthers D, Dasgupta B, Dubey S, Flossmann O, Hall C, Hollywood J, Jayne D, Jones R, Lanyon P, Muir A, Scott D, Young L, Luqmani RA (2009) Modification and validation of the Birmingham Vasculitis Activity Score (version 3). Ann Rheum Dis 68:1827–1832
Berden AE, Ferrario F, Hagen EC, Jayne DR, Jennette JC, Joh K, Neumann I, Noel LH, Pusey CD, Waldherr R, Bruijn JA, Bajema IM (2010) Histopathologic classification of ANCA-associated glomerulonephritis. J Am Soc Nephrol 21:1628–1636
Chen YX, Xu J, Pan XX, Shen PY, Li X, Ren H, Chen XN, Ni LY, Zhang W, Chen N (2017) Histopathological classification and renal outcome in patients with antineutrophil cytoplasmic antibodies-associated renal vasculitis: a study of 186 patients and metaanalysis. J Rheumatol 44:304–313
Chang DY, Li ZY, Chen M, Zhao MH (2019) Myeloperoxidase-ANCA-positive granulomatosis with polyangiitis is a distinct subset of ANCA-associated vasculitis: a retrospective analysis of 455 patients from a single center in China. Semin Arthritis Rheum 48:701–706
Huang L, Zhong Y, Ooi JD, Zhou YO, Zuo X, Luo H, Chen JB, Wu T, Yang Y, Meng T, Xiao Z, Lin W, Ao X, Xiao X, Zhou Q, Xiao P (2019) The effect of pulse methylprednisolone induction therapy in Chinese patients with dialysis-dependent MPO-ANCA associated vasculitis. Int Immunopharmacol 76:105883
Chen M, Yu F, Zhang Y, Zhao MH (2005) Clinical [corrected] and pathological characteristics of Chinese patients with antineutrophil cytoplasmic autoantibody associated systemic vasculitides: a study of 426 patients from a single centre. Postgrad Med J 81:723–727
Chen M, Yu F, Zhang Y, Zhao MH (2008) Antineutrophil cytoplasmic autoantibody-associated vasculitis in older patients. Medicine (Baltimore) 87:203–209
Titeca-Beauport D, Francois A, Lobbedez T, Guerrot D, Launay D, Vrigneaud L, Daroux M, Lebas C, Bienvenu B, Hachulla E, Diouf M, Choukroun G (2018) Early predictors of one-year mortality in patients over 65 presenting with ANCA-associated renal vasculitis: a retrospective, multicentre study. BMC Nephrol 19:317
Xu PC, Chen T, Wu SJ, Yang X, Gao S, Hu SY, Wei L, Yan TK (2019) Pathological severity determines the renal recovery for anti-myeloperoxidase antibody-associated vasculitis requiring dialysis at disease onset: a retrospective study. BMC Nephrol 20:287
Tan Y, Zhao MH (2018) Complement in glomerular diseases. Nephrology (Carlton) 23(Suppl 4):11–15
Hu X, Feng J, Zhou Q, Luo L, Meng T, Zhong Y, Tang W, Deng S, Li X (2019) Respiratory syncytial virus exacerbates kidney damages in IgA nephropathy mice via the C5a–C5aR1 axis orchestrating Th17 cell responses. Front Cell Infect Microbiol 9:151
Chen M, Jayne DRW, Zhao MH (2017) Complement in ANCA-associated vasculitis: mechanisms and implications for management. Nat Rev Nephrol 13:359–367
Choi H, Kim Y, Jung SM, Song JJ, Park YB, Lee SW (2019) Low serum complement 3 level is associated with severe ANCA-associated vasculitis at diagnosis. Clin Exp Nephrol 23:223–230
Manenti L, Vaglio A, Gnappi E, Maggiore U, Allegri L, Allinovi M, Urban ML, Delsante M, Galetti M, Nicastro M, Pilato FP, Buzio C (2015) Association of serum C3 concentration and histologic signs of thrombotic microangiopathy with outcomes among patients with ANCA-associated renal vasculitis. Clin J Am Soc Nephrol 10:2143–2151
Sato S, Yashiro M, Matsuoka N, Asano T, Kobayashi H, Watanabe H, Migita K (2018) Clinical features and outcomes in patients with elderly-onset anti-neutrophil cytoplasmic antibody-associated vasculitis. Geriatr Gerontol Int 18:1453–1457
Funding
This work was supported by the National Natural Science Foundation of China (81800641), the Natural Science Foundation of Hunan Province (2018JJ3853, 2018JJ3818), the Project of Health Commission of Hunan province (C2019184), and Chinese Society of Nephrology (18020010780).
Author information
Authors and Affiliations
Contributions
TM, YZ, JBC and YOZ designed the study, analyzed the data and wrote the manuscript. TM, XXZ, HL, TW, YQY, RT, XA, XCX, QLZ and PX contributed to patient enrollment and follow-up. WL and ZX analyzed the pathological data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics review committee of Xiangya Hospital Central South University (reference no. 201403061). All patients provided written informed consent to participate in the study. Patients consent for publication.
Consent for publication
Written informed consent for publication was obtained from all participants.
Code availability
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Meng, T., Zhong, Y., Chen, J. et al. Clinical features and outcomes of anti-neutrophil cytoplasmic autoantibody-associated vasculitis in Chinese elderly and very elderly patients. Int Urol Nephrol 53, 1875–1881 (2021). https://doi.org/10.1007/s11255-021-02786-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-021-02786-x